Knowledge, Attitudes and Practices of Flu Vaccination in Hemodialysis Patients
Abstract
:1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Neovius, M.; Jacobson, S.H.; Eriksson, J.K.; Elinder, C.G.; Hylander, B. Mortality in chronic kidney disease and renal replacement therapy: A population-based cohort study. BMJ Open 2014, 4, 1–9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ortiz, A.; Covic, A.; Fliser, D.; Fouque, D.; Goldsmith, D.; Kanbay, M.; Mallamaci, F.; Massy, Z.A.; Rossignol, P.; Vanholder, R.; et al. Epidemiology, contributors to, and clinical trials of mortality risk in chronic kidney failure. Lancet 2014, 383, 1831–1843. [Google Scholar] [CrossRef]
- Pesanti, E.L. Immunologic defects and vaccination in patients with chronic renal failure. Infect. Dis. Clin. N. Am. 2001, 15, 813–832. [Google Scholar] [CrossRef]
- Grzegorzewska, A.E. Prophylactic vaccinations in chronic kidney disease. Hum. Vaccines Immunother. 2015, 11, 2599–2605. [Google Scholar] [CrossRef] [Green Version]
- Kato, S.; Chmielewski, M.; Honda, H.; Pecoits-Filho, R.; Matsuo, S.; Yuzawa, Y.; Tranaeus, A.; Stenvinkel, P.; Lindholm, B. Aspects of immune dysfunction in end-stage renal disease. Clin. J. Am. Soc. Nephrol. 2008, 3, 1526–1533. [Google Scholar] [CrossRef] [Green Version]
- Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO 2012 Clinical Practice Guideline for the Evaluation and Management of Chronic Kidney Disease. Kidney Int. Suppl. 2013, 3, 1–150. [Google Scholar]
- Grzegorzewska, A.E. Hepatitis B vaccination in chronic kidney disease: Review of evidence in non-dialyzed patients. Hepat. Mon. 2012, 12, e7359. [Google Scholar] [CrossRef] [Green Version]
- Grzegorzewska, A.E. Hepatitis B vaccination in chronic kidney disease patients: A call for novel vaccines. Expert Rev. Vaccines 2014, 13, 1317–1326. [Google Scholar] [CrossRef]
- Mathew, R.; Mason, D.; Kennedy, J.S. Vaccination issues in patients with chronic kidney disease. Expert Rev. Vaccines 2014, 13, 285–298. [Google Scholar] [CrossRef]
- Durlik, M.; Ciancira, J.; Rutkowski, B. Zalecenia postępowania profilaktycznego i leczniczego w zakażeniach wirusami zapalenia wątroby typu B i C u pacjentów z przewlekłymi chorobami nerek. Nefrologia Dializoterapia Polska 2007, 11, 141–145. [Google Scholar]
- Sarnak, M.J.; Jaber, B.L. Pulmonary infectious mortality among patients with end-stage renal disease. Chest 2001, 120, 1883–1887. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sarnak, M.J.; Jaber, B.L. Mortality caused by sepsis in patients with end-stage renal disease compared with the general population. Kidney Int. 2000, 58, 1758–1764. [Google Scholar] [CrossRef] [PubMed]
- Dalrymple, L.S.; Go, A.S. Epidemiology of Acute Infections among Patients with Chronic Kidney Disease. Clin. J. Am. Soc. Nephrol. 2008, 3, 1487–1493. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Centers for Disease Control and Prevention. Prevention of pneumococcal disease: Recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm. Rep. 1997, 46, 1–24. [Google Scholar]
- Fiore, A.E.; Shay, D.K.; Haber, P.; Iskander, J.K.; Uyeki, T.M.; Mootrey, G.; Bresee, J.S.; Cox, N.J. Prevention and control of influenza: Recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm. Rep. 2007, 56, 1–54. [Google Scholar]
- Naqvi, S.B.; Collins, A.J. Infectious Complications in Chronic Kidney Disease. Adv. Chronic Kidney Dis. 2006, 13, 199–204. [Google Scholar] [CrossRef]
- DaRoza, G.; Loewen, A.; Djurdjev, O.; Love, J.; Kempston, C.; Burnett, S.; Kiaii, M.; Taylor, P.A.; Levin, A. Stage of chronic kidney disease predicts seroconversion after hepatitis B immunization: Earlier is better. Am. J. Kidney Dis. 2003, 42, 1184–1192. [Google Scholar] [CrossRef]
- Gilbertson, D.T.; Unruh, M.; McBean, A.M.; Kausz, A.T.; Snyder, J.J.; Collins, A.J. Influenza vaccine delivery and effectiveness in end-stage renal disease. Kidney Int. 2003, 63, 738–743. [Google Scholar] [CrossRef] [Green Version]
- Wang, I.K.; Lin, C.L.; Lin, P.C.; Liang, C.C.; Liu, Y.L.; Chang, C.T.; Yen, T.H.; Morisky, D.E.; Huang, C.C.; Sung, F.C. Effectiveness of influenza vaccination in patients with end-stage renal disease receiving hemodialysis: A population-based study. Vaccine 2012, 31, 718–724. [Google Scholar] [CrossRef]
- Bond, T.C.; Spaulding, A.C.; Krisher, J.; McClellan, W. Mortality of dialysis patients according to influenza and pneumococcal vaccination status. Am. J. Kidney Dis. 2012, 60, 959–965. [Google Scholar] [CrossRef]
- Bertoldo, G.; Annalisa, Pesce, A.; Pepe, A.; Concetta Paola Pelullo, C.P.; Di Giuseppe, G.D. Seasonal influenza: Knowledge, attitude and vaccine uptake among adults with chronicconditions in Italy. PLoS ONE 2019, 14, e0215978. [Google Scholar] [CrossRef] [Green Version]
- Luz, P.M.; Johnson, R.E.; Brown, H.E. Workplace availability, risk group and perceived barriers predictive of 2016–17 influenza vaccine uptake in the United States: A cross-sectional study. Vaccine 2017, 35, 5890–5896. [Google Scholar] [CrossRef] [PubMed]
- Casalino, E.; Ghazali, A.; Bouzid, D.; Antoniol, S.; Pereira, L.; Kenway, P.; Choquet, C. Patient’s behaviors and missed opportunities for vaccination against seasonal epidemic influenza and evaluation of their impact on patient’s influenza vaccine uptake. PLoS ONE 2018, 13, e0193029. [Google Scholar] [CrossRef] [Green Version]
- Jorgensen, P.; Mereckiene, J.; Cotter, S.; Johansen, K.; Tsolova, S.; Brown, C. How close are countries of the WHO European Region to achieving the goal of vaccinating 75% of key risk groups against influenza? Results from national surveys on seasonal influenza vaccination programmes, 2008/2009 to 2014/2015. Vaccine 2018, 36, 442–452. [Google Scholar] [CrossRef] [PubMed]
- Giese, C.; Mereckiene, J.; Danis, K.; O’Donnell, J.; O’Flanagan, D.; Cotter, S. Low vaccination coverage for seasonal influenza and pneumococcal disease among adults at-risk and health care workers in Ireland, 2013: The key role of GPs in recommending vaccination. Vaccine 2016, 34, 3657–3662. [Google Scholar] [CrossRef] [PubMed]
- Bodeker, B.; Remschmidt, C.; Schmich, P.; Wichmann, O. Why are older adults and individuals with underlying chronic diseases in Germany not vaccinated against flu? A population-based study. BMC Public Health 2015, 15, 618. [Google Scholar] [CrossRef] [Green Version]
- Garthwaite, E.; Reddy, V.; Douthwaite, S.; Lines, S.; Tyerman, K.; Eccles, J. Clinical practice guideline management of blood borne viruses within the haemodialysis unit. BMC Nephrol. 2019, 20, 388. [Google Scholar] [CrossRef]
- Kliś, A. Vaccinations in patients with chronic disease disease. Nephrol. Forum 2019, 12, 133–139. [Google Scholar]
- Malhi, G.; Rumman, A.; Thanabalan, R.; Croitoru, K.; Silverberg, M.S.; Steinhart, H.A.; Nguyen, G.C. Vaccination in Inflammatory Bowel Disease Patients: Attitudes, Knowledge, and Uptake. J. Crohn’s Colitis 2015, 9, 439–444. [Google Scholar] [CrossRef] [Green Version]
- Nitsch-Osuch, A.; Gołębiak, I.; Wyszkowska, D.; Rosińska, R.; Kargul, L.; Szuba, B.; Brydak, L.B. Influenza Vaccination Coverage Among Polish Patients with Chronic Diseases. Adv. Exp. Med. Biol. 2017, 10, 968. [Google Scholar]
- Bohlke, K.; Davis, R.L.; Marcy, S.M.; Braun, M.M.; DeStefano, F.; Black, S.B.; Mullooly, J.P.; Thompson, R.S. Risk of anaphylaxis after vaccination of children and adolescents. Pediatrics 2003, 112, 815–820. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hui-Chen, L.; Hui-Fen, C.; Shu-Chen, H.; Chun-Yuh, Y. Association of Influenza Vaccination and Reduced Risk of Stroke Hospitalization among the Elderly: A Population-Based Case-Control. Int. J. Environ. Res. Public Health 2014, 11, 3639–3649. [Google Scholar]
- Lindsberg, P.; Grau, A.J. Inflammation and infections as risk factors for ischemic stroke. Stroke 2003, 34, 2518–2532. [Google Scholar] [CrossRef] [PubMed]
- Grau, A.J.; Fischer, B.; Barth, C.; Ling, P.; Lichy, C.; Buggle, F. Influenza vaccination is associated with a reduced risk of stroke. Stroke 2005, 36, 1501–1506. [Google Scholar] [CrossRef] [Green Version]
- Lee, K.R.; Bae, J.H.; Hwang, I.C.; Kim, K.K.; Suh, H.S.; Ko, K.D. Effect of Influenza Vaccination on Riskof Stroke: A Systematic Review and Meta-Analysis. Neuroepidemiology 2017, 48, 103–110. [Google Scholar] [CrossRef] [Green Version]
- Siriwardena, A.N.; Gwini, S.M.; Coupland, C.A.C. Influenza vaccination, pneumococcal vaccination and risk of acute myocardial infarction: Matched case–control study. Can. Med. Assoc. J. 2010, 15, 182. [Google Scholar] [CrossRef] [Green Version]
- Olatunbosuna, O.D.; Esterhuizenb, T.M.; Wiysongec, C.S. A cross sectional survey to evaluate knowledge, attitudes and practices regarding seasonal influenza and influenza vaccination among diabetics in Pretoria, South Africa. Vaccine 2017, 35, 6375–6386. [Google Scholar] [CrossRef]
- Tan, E.K.; Lim, L.H.; Teoh, Y.L.; Ong, G.; Bock, H.L. Influenza and seasonal influenza vaccination among diabetics in Singapore: Knowledge, attitudes and practices. Singapore Med. J. 2010, 51, 623–630. [Google Scholar]
- Ogólnopolski Program Zwalczania Grypy—National Program for Combating Influenza. Available online: http://opzg.pl (accessed on 18 November 2020).
- Dower, J.; Donald, M.; Begum, N.; Vlack, S.; Ozolins, I. Patterns and determinants of influenza and pneumococcal immunisation among adults with chronic disease living in Queensland, Australia. Vaccine 2011, 29, 3031–3037. [Google Scholar] [CrossRef]
| Variables | CDC (No = 103) | SDC (No = 90) | p |
|---|---|---|---|
| Age y. ± SD | 64.48 ± 14.64 | 62.54 ± 14.11 | 0.354 |
| Female (1) No (%) | 53 (51) | 37 (41) | 0.385 * |
| Basic education (1) No (%) | 30 (29) | 30 (33) | 0.648 * |
| High school education (1) No (%) | 51 (50) | 53 (59) | 0.476 * |
| Higher education (1) No (%) | 22 (21) | 9 (10) | 0.067 * |
| Weight kg ± SD | 75.41 ± 18.11 | 80.27 ± 16.87 | 0.059 |
| BMI kg/m² ± SD | 27.42 ± 5.78 | 28.37 ± 6.19 | 0.271 |
| Diabetes (1) No (%) | 30 (29) | 37 (41) | 0.226 * |
| Combined comorbidity (1) No (%) | 32 (31) | 46 (51) | 0.066 * |
| Variables | Patients Regularly Vaccinated against Influenza—One a Year (No = 87) | Patients Irregularly or Not Vaccinated against Influenza (No = 106) | p |
|---|---|---|---|
| Age y. ± SD | 64.09 ± 14.06 | 62.94 ± 14.83 | 0.601 |
| Female No (%) | 31 (30.1) | 59 (55.7) | 0.09 * |
| Basic education No (%) | 32(36.8) | 28(26.4) | 0.31 * |
| High school education No (%) | 46 (52.9) | 58 (54.7) | 0.89 * |
| Higher education No (%) | 9 (10.3) | 20 (18.9) | 0.15 * |
| Weight kg ± SD | 75.03 ± 18.88 | 82.66 ± 21.03 | 0.291 |
| Diabetes No (%) | 32 (36.8) | 35 (33) | 0.70 * |
| Combined comorbidity No (%) | 45 (51.7) | 34 (32) | 0.08 * |
| HD vintage m ± SD | 57.96 ± 53.50 | 49.72 ± 56.85 | 0.550 |
| Patients from SDC No (%) | 67 (77) | 23 (21.7) | <0.01 * |
| Vaccination concerns and obstacles | |||
| Patient did not know that they should be vaccinated against influenza No (%) | 0 (0) | 24 (22.6) | <0.01 * |
| Patient was afraid of vaccine side effects No (%) | 0 (0) | 31 (29.2) | <0.01 * |
| Patient thinks that vaccination takes too much time No (%) | 0 (0) | 4 (3.8) | 0.07 * |
| Patient thinks that the vaccine is too expensive No (%) | 0 (0) | 6 (5.7) | <0.05 * |
| Patient thinks that influenza vaccinations are ineffective No (%) | 1 (1.1) | 28 (26.4) | <0.01 * |
| Patients with any concerns and obstacles No (%) | 1 (1.1) | 96 (90.6) | <0.01 * |
| Who or what is a reliable source of information for patient about vaccinations? | |||
| Nephrologist No (%) | 72 (82.8) | 74 (70) | 0.44 * |
| Family doctor No (%) | 36 (41.4) | 60 (56.6) | 0.22 * |
| Medical press No (%) | 2 (2.2) | 14 (13.2) | <0.05 * |
| Daily or popular press No (%) | 0 (0) | 6 (5.7) | <0.05 * |
| Family or friends No (%) | 2 (2.2) | 6 (5.7) | 0.26 * |
| Vaccination websites No (%) | 0 (0) | 6 (5.7) | <0.05 * |
| Patients who believe vaccination is effective No (%) | 76 (87.4) | 33 (31.1) | <0.01 * |
| Patients vaccinated in the past No (%) | 65 (74.7) | 30 (28.3) | <0.01 * |
| Variables | OR | 95% CI | p | Estimate |
|---|---|---|---|---|
| Age (y.) | 0.994 | 0.975–1.014 | 0.579 | −0.006 |
| Female (1) | 0.441 | 0.246–0.790 | 0.006 | −0.819 |
| Basic education (1) | 1.621 | 0.878–2.993 | 0.123 | 0.483 |
| High school education (1) | 0.929 | 0.526–1.640 | 0.798 | −0.074 |
| Higher education (1) | 0.496 | 0.213–1.154 | 0.104 | −0.701 |
| Weight (kg) | 1.024 | 1.008–1.040 | 0.004 | 0.023 |
| Diabetes (1) | 1.180 | 0.651–2.139 | 0.585 | 0.166 |
| Combined comorbidity (1) | 2.269 | 1.263–4.076 | 0.006 | 0.819 |
| HD vintage (m) | 0.997 | 0.992–1.003 | 0.304 | −0.003 |
| Vaccination concerns and obstacles | ||||
| Patient did not know that they should be vaccinated against influenza (1) | 0.000 | 0.000–0.244 | 0.997 | −20.262 |
| Patient was afraid of vaccine side effects (1) | 0.000 | 0.000 | 0.996 | −20.351 |
| Patient thinks that vaccination takes too much time (1) | 0.000 | 0.000 | 0.997 | −18.044 |
| Patient thinks that the vaccine is too expensive (1) | 0.000 | 0.000 | 0.997 | −19.064 |
| Patient thinks that influenza vaccinations are ineffective (1) | 0.032 | 0.004–0.244 | 0.001 | −3.430 |
| Patients with any concerns and obstacles (1) | 0.001 | 0.000–0.010 | 0.000 | −6.716 |
| Who or what is a reliable source of information for patient about vaccinations? | ||||
| Nephrologist (1) | 2.076 | 1.037–4.154 | 0.0391 | 0.730 |
| Family doctor (1) | 0.541 | 0.305–0.961 | 0.0361 | −0.614 |
| Medical press (1) | 0.155 | 0.034 | 0.015 | −1.867 |
| Daily or popular press (1) | 0.000 | 0.000 | 0.997 | −19.064 |
| Family or friends (1) | 0.392 | 0.077–1.994 | 0.259 | −0.936 |
| Vaccination websites (1) | 0.000 | 0.000 | 0.997 | −19.064 |
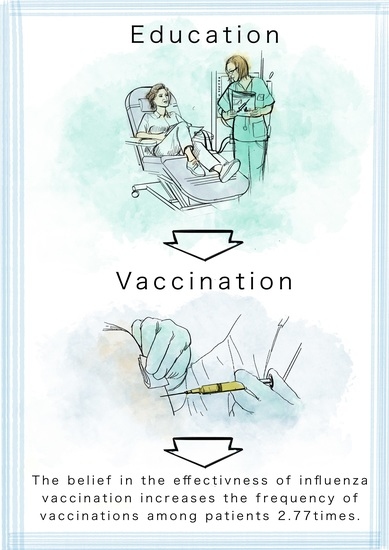
| Patients who believe vaccination effective (1) | 15.284 | 7.189–32.492 | 0.000 | 2.727 |
| Patients vaccinated in the past (1) | 7.485 | 3.938–14.225 | 0.000 | 2.013 |
| Variables | adj. OR | 95% CI | p | Estimate | LR * (p) |
|---|---|---|---|---|---|
| Patients who believe vaccination are effective (1) | 9.863 | 4.357–22.326 | 0.000 | 2.289 | <0.01 |
| Vaccinated in the past (1) | 5.179 | 2.367–11.332 | 0.000 | 1.645 | <0.01 |
| Combined comorbidity (1) | 2.448 | 1.127–5.318 | 0.024 | 0.895 | <0.01 |
| Female (1) | 0.408 | 0.189–0.882 | 0.023 | −0.896 | <0.05 |
| Variables | Group A Vaccination Effective (No = 109) | Group B Vaccination Ineffective (No = 84) | p |
|---|---|---|---|
| Age y. ± SD | 63.1 ± 14.6 | 64.2 ± 14.2 | 0.61 |
| Female No (%) | 45 (41.2) | 45 (53.5) | 0.308 * |
| Basic education No (%) | 33 (30.5) | 27 (32.1) | 0.840 * |
| High school education No (%) | 64 (58.7) | 40 (47.6) | 0.398 * |
| Higher education No (%) | 12 (11) | 17 (20.3) | 0.127 * |
| Weight kg ±SD | 80.1 ± 21 | 76.3 ± 18.9 | 0.19 |
| Diabetes No (%) | 40 (36.7) | 25 (29.8) | 0.47 * |
| Combined comorbidity No (%) | 79 (72) | 53 (63) | 0.55 * |
| HD vintage m ± SD | 56.2 ± 61.2 | 51.7 ± 46.1 | 0.58 |
| Patients from SDC No (%) | 69 (63.3) | 21 (25) | <0.01 * |
| Vaccination concerns and obstacles | |||
| Patient did not know that they should be vaccinated against influenza No (%) | 9 (8.3) | 15 (17.9) | 0.08 * |
| Patient was afraid of vaccine side effects No (%) | 10 (9.2) | 21 (25) | <0.05 * |
| Patient thinks that vaccination takes too much time No (%) | 1 (0.9) | 3 (3.6) | 0.21 * |
| Patient thinks that the vaccine is too expensive No (%) | 2 (1.8) | 4 (4.8) | 0.26 * |
| Patients with any concerns and obstacles No (%) | 29 (26.6) | 68 (8.9) | <0.01 * |
| Who or what is a reliable source of information for patient about vaccinations? | |||
| Nephrologist No (%) | 89 (81.7) | 57 (67.9) | 0.41 * |
| Family doctor No (%) | 48 (44) | 48 (57.1) | 0.29 * |
| Medical press No (%) | 7 (6.4) | 9 (10.7) | 0.32 * |
| Daily or popular press No (%) | 2 (1.8) | 4 (4.8) | 0.26 * |
| Family or friends No (%) | 2 (1.8) | 6 (7.1) | 0.08 * |
| Vaccination websites No (%) | 1 (0.9) | 5 (6) | 0.053 * |
| Patients regularly vaccinated against influenza—one a year No (%) | 76 (70) | 11 (13) | <0.01 * |
| Patients vaccinated in the past No (%) | 74 (67.9) | 21 (25) | <0.01 * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gawryś, A.; Gołębiowski, T.; Zielińska, D.; Augustyniak-Bartosik, H.; Kuriata-Kordek, M.; Szenborn, L.; Krajewska, M. Knowledge, Attitudes and Practices of Flu Vaccination in Hemodialysis Patients. Vaccines 2021, 9, 77. https://doi.org/10.3390/vaccines9020077
Gawryś A, Gołębiowski T, Zielińska D, Augustyniak-Bartosik H, Kuriata-Kordek M, Szenborn L, Krajewska M. Knowledge, Attitudes and Practices of Flu Vaccination in Hemodialysis Patients. Vaccines. 2021; 9(2):77. https://doi.org/10.3390/vaccines9020077
Chicago/Turabian StyleGawryś, Ada, Tomasz Gołębiowski, Dorota Zielińska, Hanna Augustyniak-Bartosik, Magdalena Kuriata-Kordek, Leszek Szenborn, and Magdalena Krajewska. 2021. "Knowledge, Attitudes and Practices of Flu Vaccination in Hemodialysis Patients" Vaccines 9, no. 2: 77. https://doi.org/10.3390/vaccines9020077
APA StyleGawryś, A., Gołębiowski, T., Zielińska, D., Augustyniak-Bartosik, H., Kuriata-Kordek, M., Szenborn, L., & Krajewska, M. (2021). Knowledge, Attitudes and Practices of Flu Vaccination in Hemodialysis Patients. Vaccines, 9(2), 77. https://doi.org/10.3390/vaccines9020077