High-Risk Obesity Phenotypes: Target for Multimorbidity Prevention at the ROFEMI Study
Abstract
:1. Answer the Study Importance Questions
2. Introduction
3. Materials and Methods
3.1. Patient Classification and Data Collection
- BMI: Healthy weight—BMI 18.5 kg/m2 to 24.9 kg/m2; Overweight—BMI 25 kg/m2 to 29.9 kg/m2; Obese—BMI 30 kg/m2 to 34.9 kg/m2; Very obese—BMI 35 kg/m2 or higher.
- WC: For men, low risk—less than 94 cm; high risk—94–102 cm; very high risk—greater than 102 cm. For women, low risk—less than 80 cm; high risk—80–88 cm; very high risk—greater than 88 cm.
3.2. Statistical Analysis
4. Results
4.1. BMI-WC Classification (Nice Guidelines)
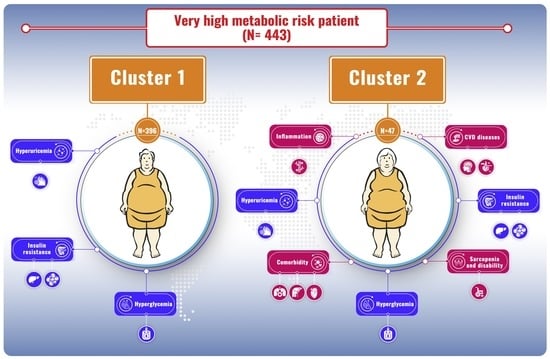
4.2. Clusters of Very High-Risk Patients
5. Discussion
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO. Obesity and Overweight. 9 June 2021. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 22 April 2022).
- Dai, H.; Alsalhe, T.A.; Chalghaf, N.; Riccò, M.; Bragazzi, N.L.; Wu, J. The global burden of disease attributable to high body mass index in 195 countries and territories, 1990–2017: An analysis of the Global Burden of Disease Study. PLoS Med. 2020, 17, e1003198. [Google Scholar] [CrossRef] [PubMed]
- Agborsangaya, C.B.; Ngwakongnwi, E.; Lahtinen, M.; Cooke, T.; Johnson, J.A. Multimorbidity prevalence in the general population: The role of obesity in chronic disease clustering. BMC Public Health 2013, 13, 1161. [Google Scholar] [CrossRef] [PubMed]
- Heymsfield, S.B.; Wadden, T.A. Mechanisms, pathophysiology, and management of obesity. N. Engl. J. Med. 2017, 376, 254–266. [Google Scholar] [CrossRef] [PubMed]
- Kivimäki, M.; Kuosma, E.; Ferrie, J.E.; Luukkonen, R.; Nyberg, S.T.; Alfredsson, L.; Batty, G.D.; Brunner, E.J.; Fransson, E.; Goldberg, M.; et al. Overweight, obesity, and risk of cardiometabolic multimorbidity: Pooled analysis of individual-level data for 120 813 adults from 16 cohort studies from the USA and Europe. Lancet Public Health 2017, 2, e277–e285. [Google Scholar] [CrossRef]
- Blüher, M. Obesity: Global epidemiology and pathogenesis. Nat. Rev. Endocrinol. 2019, 15, 288–298. [Google Scholar] [CrossRef] [PubMed]
- Woolcott, O.O.; Bergman, R.N. Relative fat mass (RFM) as a new estimator of whole-body fat percentage—A cross-sectional study in American adult individuals. Sci. Rep. 2018, 8, 10980. [Google Scholar] [CrossRef]
- Fu, J.; Hofker, M.; Wijmenga, C. Apple or pear: Size and shape matter. Cell Metab. 2015, 21, 507–508. [Google Scholar] [CrossRef]
- Visscher, T.L.S.; Heitmann, B.L.; Rissanen, A.; Lahti-Koski, M.; Lissner, L. A break in the obesity epidemic? Explained by biases or misinterpretation of the data? Int. J. Obes. 2015, 39, 189–198. [Google Scholar] [CrossRef]
- Chen, L.K.; Woo, J.; Assantachai, P.; Auyeung, T.W.; Chou, M.Y.; Iijima, K.; Jang, H.C.; Kang, L.; Kim, M.; Kim, S.; et al. Asian Working Group for Sarcopenia: 2019 Consensus Update on Sarcopenia Diagnosis and Treatment. J. Am. Med. Dir. Assoc. 2020, 21, 300–307.e2. [Google Scholar] [CrossRef]
- Charlson, M.E.; Pompei, P.; Ales, K.L.; MacKenzie, C.R. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chronic. Dis. 1987, 40, 373–383. [Google Scholar] [CrossRef]
- Gómez, J.C.; Lorido, J.A.; Huelgas, R.G.; Vidal, M.S.; Tembra, M.S.; Aguilar, J.V.; Voces, I.M.; Pérez, E.F.; Rodríguez, J.F.; Muñoz, J.E. Prevalence of obesity according to Edmonton staging in the Internal Medicine consultations. Results of the OBEMI study. Rev. Clin. Esp. 2017, 217, 71–78. [Google Scholar] [CrossRef] [PubMed]
- Hameed, E.K. TyG index a promising biomarker for glycemic control in type 2 Diabetes Mellitus. Diabetes Metab. Syndr. 2019, 13, 560–563. [Google Scholar] [CrossRef] [PubMed]
- Okugawa, Y.; Toiyama, Y.; Yamamoto, A.; Shigemori, T.; Ide, S.; Kitajima, T.; Fujikawa, H.; Yasuda, H.; Hiro, J.; Yoshiyama, S.; et al. Lymphocyte-C-reactive Protein Ratio as Promising New Marker for Predicting Surgical and Oncological Outcomes in Colorectal Cancer. Ann. Surg. 2020, 272, 342–351. [Google Scholar] [CrossRef]
- Çınar, T.; Çağdaş, M.; Rencüzoğulları, İ.; Karakoyun, S.; Karabağ, Y.; Yesin, M.; Sadioğlu Çağdaş, Ö.; Tanboğa, H.İ. Prognostic efficacy of C-reactive protein/albumin ratio in ST elevation myocardial infarction. Scand. Cardiovasc. J. 2019, 53, 83–90. [Google Scholar] [CrossRef] [PubMed]
- Obesity: Identification, Assessment and Management. 2021. Available online: https://www.guidelines.co.uk/public-health/nice-obesity-guideline/252547.article (accessed on 15 January 2022).
- Altman, N.S. An introduction to kernel and nearest-neighbor nonparametric regression. Am. Stat. 1992, 46, 175–185. [Google Scholar] [CrossRef]
- Ding, X.; Wang, X.; Wu, J.; Zhang, M.; Cui, M. Triglyceride-glucose index and the incidence of atherosclerotic cardiovascular diseases: A meta-analysis of cohort studies. Cardiovasc. Diabetol. 2021, 20, 76. [Google Scholar] [CrossRef] [PubMed]
- Kalkhoff, R.K.; Hartz, A.H.; Rupley, D.; Kissebah, A.H.; Kelber, S. Relationship of body fat distribution to blood pressure, carbohydrate tolerance, and plasma lipids in healthy obese women. J. Lab. Clin. Med. 1983, 102, 621–627. [Google Scholar]
- Kissebah, A.H.; Vydelingum, N.; Murray, R.; Evans, D.J.; Hartz, A.J.; Kalkhoff, R.K.; Adams, P.W. Relation of body fat distribution to metabolic complications of obesity. J. Clin. Endocrinol. Metab. 1982, 54, 254–260. [Google Scholar] [CrossRef]
- Krotkiewski, M.; Björntorp, P.; Sjöström, L.; Smith, U. Impact of obesity on metabolism in men and women. Importance of regional adipose tissue distribution. J. Clin. Investig. 1983, 72, 1150–1162. [Google Scholar] [CrossRef]
- Ross, R.; Neeland, I.J.; Yamashita, S.; Shai, I.; Seidell, J.; Magni, P.; Santos, R.D.; Arsenault, B.; Cuevas, A.; Hu, F.B.; et al. Waist circumference as a vital sign in clinical practice: A Consensus Statement from the IAS and ICCR Working Group on Visceral Obesity. Nat. Rev. Endocrinol. 2020, 16, 177–189. [Google Scholar] [CrossRef]
- Cerhan, J.R.; Moore, S.C.; Jacobs, E.J.; Kitahara, C.M.; Rosenberg, P.S.; Adami, H.O.; Ebbert, J.O.; English, D.R.; Gapstur, S.M.; Giles, G.G.; et al. A pooled analysis of waist circumference and mortality in 650,000 adults. Mayo Clin. Proc. 2014, 89, 335–345. [Google Scholar] [CrossRef] [PubMed]
- de Hollander, E.L.; Bemelmans, W.J.; Boshuizen, H.C.; Friedrich, N.; Wallaschofski, H.; Guallar-Castillón, P.; Walter, S.; Zillikens, M.C.; Rosengren, A.; Lissner, L.; et al. The association between waist circumference and risk of mortality considering body mass index in 65- to 74-year-olds: A meta-analysis of 29 cohorts involving more than 58,000 elderly persons. Int. J. Epidemiol. 2012, 41, 805–817. [Google Scholar] [CrossRef] [PubMed]
- Christiansen, M.R.; Ureña, M.G.; Borisevich, D.; Grarup, N.; Martínez, J.A.; Oppert, J.M.; Sørensen, T.I.; Hansen, T.; Blaak, E.E.; Kilpeläinen, T.O. Abdominal and gluteofemoral fat depots show opposing associations with postprandial lipemia. Am. J. Clin. Nutr. 2021, 114, 1467–1475. [Google Scholar] [CrossRef] [PubMed]
- Janssen, I.; Katzmarzyk, P.T.; Ross, R. Body mass index is inversely related to mortality in older people after adjustment for waist circumference. J. Am. Geriatr. Soc. 2005, 53, 2112–2118. [Google Scholar] [CrossRef]
- Iwabu, M.; Okada-Iwabu, M.; Yamauchi, T.; Kadowaki, T. Adiponectin/AdipoR research and its implications for lifestyle-related diseases. Front. Cardiovasc. Med. 2019, 6, 116. [Google Scholar] [CrossRef]
- Cypess, A.M. Reassessing Human Adipose Tissue. N. Engl. J. Med. 2022, 386, 768–779. [Google Scholar] [CrossRef]
- Larabee, C.M.; Neely, O.C.; Domingos, A.I. Obesity: A neuroimmunometabolic perspective. Nat. Rev. Endocrinol. 2020, 16, 30–43. [Google Scholar] [CrossRef]
- Ridker, P.M. A Test in Context: High-Sensitivity C-Reactive Protein. J. Am. Coll. Cardiol. 2016, 67, 712–723. [Google Scholar] [CrossRef]
- Karanfil, M.; Gayretli, Y.K. The association of aortic elasticity properties with novel inflammatory marker CRP/albumin ratio. Clin. Exp. Hypertens. 2021, 43, 780–787. [Google Scholar] [CrossRef]
- Iseda, N.; Itoh, S.; Yoshizumi, T.; Tomiyama, T.; Morinaga, A.; Shimagaki, T.; Mori, M. Lymphocyte-to-C-reactive protein ratio as a prognostic factor for hepatocellular carcinoma. Int. J. Clin. Oncol. 2021, 26, 1890–1900. [Google Scholar] [CrossRef]
- Kelesoglu, S.; Yilmaz, Y.; Elcık, D.; Kalay, N. Systemic immune inflammation index: A novel predictor for coronary collateral circulation. Perfusion 2021, 7, 2676591211014822. [Google Scholar] [CrossRef] [PubMed]
- He, Y.; Hara, H.; Núñez, G. Mechanism and Regulation of NLRP3 Inflammasome Activation. Trends Biochem Sci. 2016, 41, 1012–1021. [Google Scholar] [CrossRef] [PubMed]
- Hughes, M.M.; O’Neill, L.A. Metabolic regulation of nlrp 3. Immunol. Rev. 2018, 281, 88–98. [Google Scholar] [CrossRef] [PubMed]
- Antonioli, L.; Moriconi, D.; Masi, S.; Bottazzo, D.; Pellegrini, C.; Fornai, M.; Anselmino, M.; Ferrannini, E.; Blandizzi, C.; Taddei, S.; et al. Differential Impact of Weight Loss and Glycemic Control on Inflammasome Signaling. Obesity (Silver Spring) 2020, 28, 609–615. [Google Scholar] [CrossRef]



| Variable (Absolute Number (Percentage)) | Group 1 n = 3 | Group 2 n = 27 | Group 3 n = 44 | Group 4 n = 462 | p |
|---|---|---|---|---|---|
| Sex (women) | 3 (100) | 26 (96.3) | 29 (65.9) | 216 (46.7) | 0.0001 |
| Smoker | 0 | 0 | 9 (20.4) | 72 (15.6) | 0.09 |
| Education level | 0.14 | ||||
| Illiterate | 0 | 1 (3.7) | 2 (4.8) | 33 (7.3) | |
| Primary | 0 | 14 (5.8) | 27 (64.3) | 190 (41.9) | |
| Secondary | 2 (66.7) | 7 (25.9) | 10 (23.8) | 170 (37.5) | |
| University | 1 (33.3) | 5 (18.5) | 3 (7.14) | 60 (13.2) | |
| Employed | 1 (33.3) | 10 (37.04) | 16 (36.4) | 177 (38.4) | 0.99 |
| Origin (Urban) | 2 (66.7) | 18 (66.7) | 30 (68.2) | 349 (75.5) | 0.5 |
| Physical activity | 2 (66.7) | 8 (29.6) | 9 (20.4) | 157 (33.9) | 0.17 |
| HBP | 0 | 13 (48.1) | 36 (81.8) | 331 (71.6) | 0.0008 |
| T2DM | 0 | 5 (18.5) | 17 (38.6) | 199 (43.1) | 0.03 |
| Dyslipidemia | 0 | 12 (44.4) | 29 (65.9) | 313 (43.1) | 0.007 |
| Hyperuricemia | 0 | 1 (3.7) | 1 (2.27) | 102 (22.2) | 0.001 |
| HFpEF | 0 | 3 (11.1) | 6 (13.6) | 69 (14.9) | 0.85 |
| HFrEF | 0 | 0 | 1 (2.3) | 19 (4.1) | 0.85 |
| CAD | 0 | 2 (7.4) | 6 (13.6) | 42 (9.1) | 0.7 |
| Stroke | 0 | 0 | 5 (11.3) | 35 (7.6) | 0.3 |
| Gastroesophageal reflux disease | 1 (33.3) | 8 (29.6) | 7 (15.9) | 67 (14.5) | 0.15 |
| COPD/Asthma | 0 | 2 (7.4) | 5 (11.4) | 48 (10.4) | 0.88 |
| Cancer | 1 (33.3) | 0 | 0 | 13 (2.8) | 0.004 |
| Arthrosis | 1 (33.3) | 7 (25.9) | 21 (47.7) | 141 (30.5) | 0.11 |
| Depression | 0 | 6 (22.2) | 11 (25) | 98 (21.3) | 0.76 |
| Disability | |||||
| Moderate | 0 | 2 (7.4) | 11 (25) | 93 (20.3) | 0.35 |
| Severe | 0 | 1 (3.7) | 5 (11.4) | 42 (9.15) | 0.35 |
| Previous treatment | |||||
| Glucocorticoids | 0 | 2 (7.4) | 3 (6.8) | 28 (6.1) | 0.9 |
| Metformin | 0 | 3 (11.1) | 14 (31.8) | 156 (33.9) | 0.05 |
| Sulfonylureas | 0 | 1 (3.7) | 3 (6.8) | 9 (1.9) | 0.2 |
| DPP-4 inhibitors | 0 | 1 (3.7) | 3 (6.8) | 38 (8.3) | 0.78 |
| GLP-1 RA | 0 | 1 (3.7) | 5 (11.4) | 78 (16.9) | 0.19 |
| SGLT2 inhibitors | 0 | 3 (11.1) | 6 (13.6) | 79 (17.2) | 0.6 |
| Insulin | 0 | 2 (7.4) | 10 (22.7) | 54 (11.7) | 0.13 |
| Statins | 0 | 9 (33.3) | 26 (59.1) | 259 (56.3) | 0.02 |
| IBP | 1 (33.3) | 13 (48.15) | 31 (70.4) | 231 (50.2) | 0.06 |
| Antihypertensives | 0 | 14 (51.8) | 33 (75) | 325 (70.8) | 0.007 |
| NSAIDs | 0 | 6 (22.2) | 11 (25) | 65 (14.2) | 0.15 |
| Antidepressants | 0 | 6 (22.2) | 15 (34.1) | 104 (22.6) | 0.27 |
| Variable (Median/Interquartile Range) | Group 1 n= 3 | Group 2 n = 27 | Group 3 n = 44 | Group 4 n = 462 | p |
|---|---|---|---|---|---|
| Age (years) | 62 (26) | 59 (22.5) | 65 (22.2) | 62 (22) | 0.17 |
| Weight (Kg) | 64 (21) | 78 (8.8) | 81 (9.6) | 97 (21.9) | 0.0000 |
| BMI (Kg/m2) | 26.6 (7.2) | 31.9 (2.7) | 31.2 (3.7) | 34.7 (6.9) | 0.0000 |
| WC (cm) | 81 (10.5) | 90 (5) | 100 (9.2) | 112 (13.5) | 0.0000 |
| Charlson | 0 (3) | 0 (1) | 1 (2) | 1 (3) | 0.009 |
| FPG (mg/dL) | 89 (7.5) | 97 (18.5) | 101 (28) | 104 (32) | 0.04 |
| HbA1c (%) | 5.3 (0.5) | 5.7 (0.87) | 6 (0.8) | 5.9 (1.3) | 0.1 |
| eGFR (ml/min/1.73 m2) | 66.9 (41.9) | 87.6 (24.3) | 85.6 (33.6) | 84.1 (36) | 0.28 |
| Uric acid (mg/dL) | 2.8 (0.15) | 4.65 (1.85) | 5.18 (2.01) | 5.8 (2.5) | 0.000 |
| hsCRP (mg/dL) | 1.6 (1.3) | 3 (7.9) | 2 (3) | 3 (5.5) | 0.57 |
| LDL-c (mg/dL) | 96.4 (45.5) | 107 (44) | 109 (61) | 97 (52) | 0.85 |
| HDL-c (mg/dL) | 57 (4.5) | 53 (15) | 49.5 (22) | 46 (16) | 0.0002 |
| Triglycerides (mg/dL) | 113 (74.5) | 102 (60) | 119.5 (72) | 136 (86) | 0.009 |
| TyG index | 9.1 (0.7) | 9.3 (0.7) | 9.5 (0.9) | 9.6 (0.7) | 0.008 |
| AST (U/L) | 46 (21) | 23 (19.5) | 20 (15.7) | 22 (17) | 0.63 |
| ALT (U/L) | 30 (15.5) | 24 (17.5) | 20 (12) | 21 (12.7) | 0.85 |
| GGT (U/L) | 72 (47) | 24 (34) | 28.5 (48.5) | 32 (31) | 0.07 |
| ALP (U/L) | 83 (27.5) | 75.5 (38.7) | 83 (52) | 79 (35) | 0.48 |
| Hemoglobin (g/dL) | 13.8 (0.1) | 13.6 (1.45) | 13.6 (2.4) | 14 (2.3) | 0.016 |
| Leukocytes (×109/L) | 6.9 (1.15) | 7.5 (2.5) | 6.34 (3.1) | 7.4 (2.8) | 0.06 |
| Lymphocytes (×109/L) | 2.5 (0.6) | 2.31 (0.93) | 1.96 (1.18) | 2.13 (1.1) | 0.49 |
| Platelets (×109/L) | 256 (110.5) | 224 (132) | 228 (75.2) | 237 (97) | 0.66 |
| Albumin (g/dL) | 4.2 (0.3) | 4.1 (0.45) | 4.2 (0.5) | 4.3 (0.5) | 0.26 |
| UACR (mg/g) | 7.5 (4.5) | 11.2 (10.7) | 11.1 (20.6) | 9.4 (19.4) | 0.9 |
| Drugs number | 2 (1) | 4.5 (4.7) | 8 (4) | 7 (6.25) | 0.004 |
| Variable | Cluster 1 n = 396 | Cluster 2 n = 47 | p |
|---|---|---|---|
| Origin (Urban) | 299 (74.9) | 36 (76.6) | 0.8 |
| Age (years) | 61 (21) | 77 (16) | 0.00 |
| Sex (women) | 185 (46.4) | 27 (57.4) | 0.15 |
| SARC-F (>4) | 72 (16) | 37 (78.7) | 0.00 |
| HBP | 275 (68.9) | 42 (89.4) | 0.003 |
| T2DM | 169 (42.4) | 25 (53.2) | 0.15 |
| Dyslipidemia | 265 (66.4) | 34 (72.3) | 0.41 |
| Hyperuricemia | 75 (18) | 19 (40.4) | 0.0006 |
| HF | 57 (14.3) | 27 (57.4) | 0.0001 |
| CAD | 27 (6.7) | 10 (21.3) | 0.0006 |
| Stroke | 22 (5.5) | 12 (25.5) | 0.00 |
| GERD | 53 (13.3) | 10 (21.3) | 0.13 |
| COPD/Asthma | 43 (10.8) | 5 (10.6) | 0.97 |
| Cancer | 8 (2) | 5 (10.6) | 0.0009 |
| Arthrosis | 109 (27.3) | 29 (61.7) | 0.0001 |
| Depression | 78 (19.5) | 17 (36.2) | 0.008 |
| Disability | |||
| Moderate | 77 (19.3) | 12 (25.5) | 0.000 |
| Severe | 12 (3.01) | 30 (63.8) | 0.000 |
| Comorbidities Charlson Index | |||
| Mild (0–1) | 316 (79.2) | 4 (8.5) | 0.000 |
| Moderate (2) | 64 (16) | 18 (38.3) | 0.000 |
| Severe (≥3) | 19 (4.8) | 25 (53.2) | 0.000 |
| BMI (kg/m2) | 34.7 (6.6) | 34.5 (8.89) | 0.46 |
| WC (cm) | 112 (13.9) | 116.3 (15.7) | 0.02 |
| FPG (mg/dL) | 104 (32) | 106.5 (37) | 0.79 |
| eGFR (mil/min/1.73 m2) | 86.1 (30.4) | 52.1 (42.4) | 0.000 |
| Uric acid (mg/dL) | 5.8 (2.2) | 7.4 (3.3) | 0.00 |
| hsCRP (mg/dL) | 2.1 (4.5) | 5.8 (4.1) | 0.008 |
| HDL-Chol (mg/dL) | 46 (15) | 48 (16) | 0.63 |
| LDL-Chol (mg/dL) | 97 (51) | 93 (67.5) | 0.9 |
| Triglycerides (mg/dL) | 136 (87) | 134.3 (72) | 0.95 |
| HbA1c (%) | 5.9 (1.2) | 6.3 (2) | 0.05 |
| AST (U/L) | 23 (17) | 15.5 (12.2) | 0.001 |
| ALT (U/L) | 21 (12) | 18 (7.5) | 0.01 |
| GGT (U/L) | 31 (31) | 35 (36.5) | 0.11 |
| ALP (U/L) | 79 (35) | 79.5 (37.5) | 0.3 |
| Hemoglobin (g/dL) | 14.1 (2.3) | 13 (2.2) | 0.000 |
| Leukocytes (×109/L) | 7.4 (2.7) | 8.3 (3.2) | 0.007 |
| Lymphocytes (×109/L) | 2.2 (1) | 1.9 (1.7) | 0.33 |
| Platelets (×109/L) | 237 (95) | 257 (115) | 0.97 |
| Albumin (mg/dL) | 4.3 (0.5) | 3.9 (0.7) | 0.000 |
| UACR (mg/g) | 9 (17.8) | 15 (38.2) | 0.17 |
| TyG index | 4.1 (0.3) | 4.1 (0.3) | 0.91 |
| C-reactive Protein/Albumin ratio (CAR) | 0.5 (1.1) | 1.3 (3.4) | 0.01 |
| Lymphocyte to CRP ratio (LCR) | 0.925 (1.86) | 0.52 (0.9) | 0.002 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Carretero-Gómez, J.; Pérez-Martínez, P.; Seguí-Ripoll, J.M.; Carrasco-Sánchez, F.J.; Lois Martínez, N.; Fernández Pérez, E.; Pérez Hernández, O.; García Ordoñez, M.Á.; Martín González, C.; Vigueras-Pérez, J.F.; et al. High-Risk Obesity Phenotypes: Target for Multimorbidity Prevention at the ROFEMI Study. J. Clin. Med. 2022, 11, 4644. https://doi.org/10.3390/jcm11164644
Carretero-Gómez J, Pérez-Martínez P, Seguí-Ripoll JM, Carrasco-Sánchez FJ, Lois Martínez N, Fernández Pérez E, Pérez Hernández O, García Ordoñez MÁ, Martín González C, Vigueras-Pérez JF, et al. High-Risk Obesity Phenotypes: Target for Multimorbidity Prevention at the ROFEMI Study. Journal of Clinical Medicine. 2022; 11(16):4644. https://doi.org/10.3390/jcm11164644
Chicago/Turabian StyleCarretero-Gómez, Juana, Pablo Pérez-Martínez, José Miguel Seguí-Ripoll, Francisco Javier Carrasco-Sánchez, Nagore Lois Martínez, Esther Fernández Pérez, Onán Pérez Hernández, Miguel Ángel García Ordoñez, Candelaria Martín González, Juan Francisco Vigueras-Pérez, and et al. 2022. "High-Risk Obesity Phenotypes: Target for Multimorbidity Prevention at the ROFEMI Study" Journal of Clinical Medicine 11, no. 16: 4644. https://doi.org/10.3390/jcm11164644
APA StyleCarretero-Gómez, J., Pérez-Martínez, P., Seguí-Ripoll, J. M., Carrasco-Sánchez, F. J., Lois Martínez, N., Fernández Pérez, E., Pérez Hernández, O., García Ordoñez, M. Á., Martín González, C., Vigueras-Pérez, J. F., Puchades, F., Blasco Avaria, M. C., Pérez Soto, M. I., Ena, J., Arévalo-Lorido, J. C., & on behalf of Diabetes, Obesity and Nutrition Working Group of Spanish Society of Internal Medicine. (2022). High-Risk Obesity Phenotypes: Target for Multimorbidity Prevention at the ROFEMI Study. Journal of Clinical Medicine, 11(16), 4644. https://doi.org/10.3390/jcm11164644