Rare Source of Embolism in a Young Patient: Case Report and Literature Review
Abstract
:1. Introduction
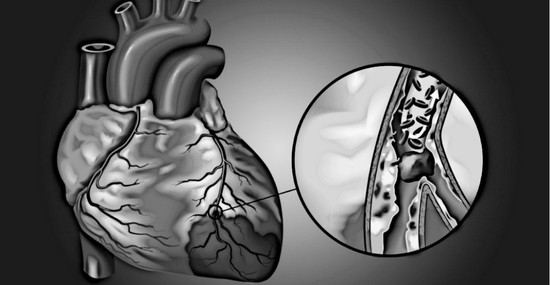
2. Case Report
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Boekholdt, S.M.; Kramer, M.H. Arterial thrombosis and the role of thrombophilia. Semin. Thromb. Hemost. 2007, 33, 588–596. [Google Scholar] [CrossRef] [PubMed]
- Segev, A.; Ellis, M.H.; Segev, F.; Friedman, Z.; Reshef, T.; Sparkes, J.D.; Tetro, J.; Pauzner, H.; David, D. High prevalence of thrombophilia among young patients with myocardial infarction and few conventional risk factors. Int. J. Cardiol. 2005, 98, 421–424. [Google Scholar] [CrossRef] [PubMed]
- Zasada, W.; Bobrowska, B.; Plens, K.; Dziewierz, A.; Siudak, Z.; Surdacki, A.; Dudek, D.; Bartuś, S. Acute myocardial infarction in young patients. Kardiol. Pol. 2021, 79, 1093–1098. [Google Scholar] [CrossRef] [PubMed]
- Shibata, T.; Kawakami, S.; Noguchi, T.; Tanaka, T.; Asaumi, Y.; Kanaya, T.; Nagai, T.; Nakao, K.; Fujino, M.; Nagatsuka, K.; et al. Prevalence, clinical features, and prognosis of acute myocardial infarction attributable to coronary artery embolism. Circulation 2015, 132, 241–250. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gulati, R.; Behfar, A.; Narula, J.; Kanwar, A.; Lerman, A.; Cooper, L.; Singh, M. Acute Myocardial Infarction in Young Individuals. Mayo Clin. Proc. 2020, 95, 136–156. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Prizel, K.R.; Hutchins, G.M.; Bulkley, B.H. Coronary artery embolism and myocardial infarction. Ann. Intern. Med. 1978, 88, 155–161. [Google Scholar] [CrossRef]
- Kanwar, S.M.; Noheria, A.; DeSimone, C.V.; Rabinstein, A.A.; Asirvatham, S.J. Coincidental impact of transcatheter patent foramen ovale closure on migraine with and without aura—A comprehensive meta-analysis. Clin. Trials Regul. Sci. Cardiol. 2016, 15, 7–13. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kleber, F.X.; Hauschild, T.; Schulz, A.; Winkelmann, A.; Bruch, L. Epidemiology of myocardial infarction caused by presumed paradoxical embolism via a patent foramen ovale. Circ. J. 2017, 81, 1484–1489. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, W.; Yu, Z.; Li, S.; Wagatsuma, K.; Du, B.; Yang, P. Concomitant acute myocardial infarction and acute pulmonary embolism caused by paradoxical embolism: A case report. BMC Cardiovasc. Disord. 2021, 21, 313. [Google Scholar] [CrossRef] [PubMed]





Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vachalcová, M.; Jankajová, M.; Jakubová, M.; Sieradzka, K.A.; Porubän, T.; Valočik, G.; Šafár, P.; Ondušová, D.; Petruš, J.; Schusterová, I. Rare Source of Embolism in a Young Patient: Case Report and Literature Review. J. Clin. Med. 2022, 11, 2038. https://doi.org/10.3390/jcm11072038
Vachalcová M, Jankajová M, Jakubová M, Sieradzka KA, Porubän T, Valočik G, Šafár P, Ondušová D, Petruš J, Schusterová I. Rare Source of Embolism in a Young Patient: Case Report and Literature Review. Journal of Clinical Medicine. 2022; 11(7):2038. https://doi.org/10.3390/jcm11072038
Chicago/Turabian StyleVachalcová, Marianna, Monika Jankajová, Marta Jakubová, Karolina Angela Sieradzka, Tibor Porubän, Gabriel Valočik, Peter Šafár, Daniela Ondušová, Ján Petruš, and Ingrid Schusterová. 2022. "Rare Source of Embolism in a Young Patient: Case Report and Literature Review" Journal of Clinical Medicine 11, no. 7: 2038. https://doi.org/10.3390/jcm11072038
APA StyleVachalcová, M., Jankajová, M., Jakubová, M., Sieradzka, K. A., Porubän, T., Valočik, G., Šafár, P., Ondušová, D., Petruš, J., & Schusterová, I. (2022). Rare Source of Embolism in a Young Patient: Case Report and Literature Review. Journal of Clinical Medicine, 11(7), 2038. https://doi.org/10.3390/jcm11072038