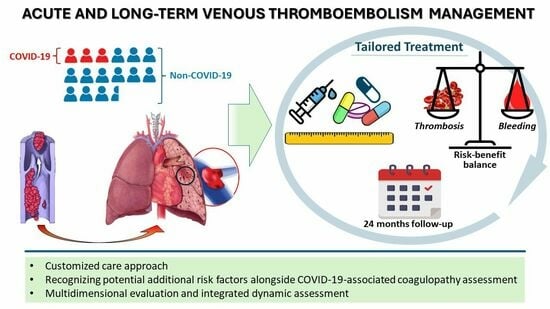
Venous Thromboembolism Management throughout the COVID-19 Era: Addressing Acute and Long-Term Challenges
Abstract
:1. Introduction
2. Materials and Methods
Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Giorgio, K.; Walker, R.F.; MacLehose, R.F.; Adrianzen-Herrera, D.; Wang, W.; Alonso, A.; Zakai, N.A.; Lutsey, P.L. Venous thromboembolism mortality and trends in older US adults, 2011–2019. Am. J. Hematol. 2023, 98, 1364–1373. [Google Scholar] [CrossRef]
- Baldwin, M.J.; Moore, H.M.; Rudarakanchana, N.; Gohel, M.; Davies, A.H. Post-thrombotic syndrome: A clinical review. J. Thromb. Haemost. 2013, 11, 795–805. [Google Scholar] [CrossRef]
- Mangwani, J.; Roberts, V.; Shannak, O.; Divall, P.; Srinivasan, A.; Dias, J. Epidemiology and Diagnosis of Post-Thrombotic Syndrome: Qualitative Synthesis with a Systematic Review. J. Clin. Med. 2023, 12, 5896. [Google Scholar] [CrossRef]
- Valerio, L.; Mavromanoli, A.C.; Barco, S.; Abele, C.; Becker, D.; Bruch, L.; Ewert, R.; Faehling, M.; Fistera, D.; Gerhardt, F.; et al. Chronic thromboembolic pulmonary hypertension and impairment after pulmonary embolism: The FOCUS study. Eur. Heart J. 2022, 43, 3387–3398. [Google Scholar] [CrossRef]
- Ende-Verhaar, Y.M.; Cannegieter, S.C.; Vonk Noordegraaf, A.; Delcroix, M.; Pruszczyk, P.; Mairuhu, A.T.; Huisman, M.V.; Klok, F.A. Incidence of chronic thromboembolic pulmonary hypertension after acute pulmonary embolism: A contemporary view of the published literature. Eur. Respir. J. 2017, 49, 1601792. [Google Scholar] [CrossRef]
- Fauche, A.; Presles, E.; Sanchez, O.; Jais, X.; Le Mao, R.; Robin, P.; Pernod, G.; Bertoletti, L.; Jego, P.; Parent, F.; et al. Frequency and predictors for chronic thromboembolic pulmonary hypertension after a first unprovoked pulmonary embolism: Results from PADIS studies. J. Thromb. Haemost. 2022, 20, 2850–2861. [Google Scholar] [CrossRef] [PubMed]
- Estrada, R.A.; Auger, W.R.; Sahay, S. Chronic Thromboembolic Pulmonary Hypertension. JAMA 2024, 331, 972–973. [Google Scholar] [CrossRef] [PubMed]
- Humbert, M.; Kovacs, G.; Hoeper, M.M.; Badagliacca, R.; Berger, R.M.F.; Brida, M.; Carlsen, J.; Coats, A.J.S.; Escribano-Subias, P.; Ferrari, P.; et al. 2022 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension. Eur. Heart J. 2022, 43, 3618–3731. [Google Scholar] [CrossRef] [PubMed]
- Yuriditsky, E.; Horowitz, J.M.; Lau, J.F. Chronic thromboembolic pulmonary hypertension and the post-pulmonary embolism (PE) syndrome. Vasc. Med. 2023, 28, 348–360. [Google Scholar] [CrossRef] [PubMed]
- Connors, J.M.; Levy, J.H. Thromboinflammation and the hypercoagulability of COVID-19. J. Thromb. Haemost. 2020, 18, 1559–1561. [Google Scholar] [CrossRef] [PubMed]
- Iba, T.; Levy, J.H.; Connors, J.M.; Warkentin, T.E.; Thachil, J.; Levi, M. The unique characteristics of COVID-19 coagulopathy. Crit. Care 2020, 24, 360. [Google Scholar] [CrossRef]
- Wu, M.A.; Fossali, T.; Pandolfi, L.; Carsana, L.; Ottolina, D.; Frangipane, V.; Rech, R.; Tosoni, A.; Lopez, G.; Agarossi, A.; et al. Hypoalbuminemia in COVID-19: Assessing the hypothesis for underlying pulmonary capillary leakage. J. Intern. Med. 2021, 289, 861–872. [Google Scholar] [CrossRef]
- Boccatonda, A.; Campello, E.; Simion, C.; Simioni, P. Long-term hypercoagulability, endotheliopathy and inflammation following acute SARS-CoV-2 infection. Expert. Rev. Hematol. 2023, 16, 1035–1048. [Google Scholar] [CrossRef] [PubMed]
- Roncon, L.; Zuin, M.; Barco, S.; Valerio, L.; Zuliani, G.; Zonzin, P.; Konstantinides, S.V. Incidence of acute pulmonary embolism in COVID-19 patients: Systematic review and meta-analysis. Eur. J. Intern. Med. 2020, 82, 29–37. [Google Scholar] [CrossRef] [PubMed]
- Kollias, A.; Kyriakoulis, K.G.; Lagou, S.; Kontopantelis, E.; Stergiou, G.S.; Syrigos, K. Venous thromboembolism in COVID-19: A systematic review and meta-analysis. Vasc. Med. 2021, 26, 415–425. [Google Scholar] [CrossRef] [PubMed]
- Tudoran, C.; Velimirovici, D.E.; Berceanu-Vaduva, D.M.; Rada, M.; Voita-Mekeres, F.; Tudoran, M. Increased Susceptibility for Thromboembolic Events versus High Bleeding Risk Associated with COVID-19. Microorganisms 2022, 10, 1738. [Google Scholar] [CrossRef] [PubMed]
- Wichmann, D.; Sperhake, J.P.; Lutgehetmann, M.; Steurer, S.; Edler, C.; Heinemann, A.; Heinrich, F.; Mushumba, H.; Kniep, I.; Schroder, A.S.; et al. Autopsy Findings and Venous Thromboembolism in Patients With COVID-19: A Prospective Cohort Study. Ann. Intern. Med. 2020, 173, 268–277. [Google Scholar] [CrossRef] [PubMed]
- Voigtlaender, M.; Edler, C.; Gerling, M.; Schadler, J.; Ondruschka, B.; Schroder, A.S.; Sperhake, J.; Ehrhardt, S.; Wang, L.; Haddad, M.; et al. Thromboembolic events in deceased patients with proven SARS-CoV-2 infection: Frequency, characteristics and risk factors. Thromb. Res. 2022, 218, 171–176. [Google Scholar] [CrossRef] [PubMed]
- Konstantinides, S.V.; Meyer, G.; Becattini, C.; Bueno, H.; Geersing, G.J.; Harjola, V.P.; Huisman, M.V.; Humbert, M.; Jennings, C.S.; Jimenez, D.; et al. 2019 ESC Guidelines for the diagnosis and management of acute pulmonary embolism developed in collaboration with the European Respiratory Society (ERS). Eur. Heart J. 2020, 41, 543–603. [Google Scholar] [CrossRef]
- Ortel, T.L.; Neumann, I.; Ageno, W.; Beyth, R.; Clark, N.P.; Cuker, A.; Hutten, B.A.; Jaff, M.R.; Manja, V.; Schulman, S.; et al. American Society of Hematology 2020 guidelines for management of venous thromboembolism: Treatment of deep vein thrombosis and pulmonary embolism. Blood Adv. 2020, 4, 4693–4738. [Google Scholar] [CrossRef]
- Stevens, S.M.; Woller, S.C.; Kreuziger, L.B.; Bounameaux, H.; Doerschug, K.; Geersing, G.J.; Huisman, M.V.; Kearon, C.; King, C.S.; Knighton, A.J.; et al. Antithrombotic Therapy for VTE Disease: Second Update of the CHEST Guideline and Expert Panel Report. Chest 2021, 160, e545–e608. [Google Scholar] [CrossRef] [PubMed]
- Stevens, S.M.; Woller, S.C.; Baumann Kreuziger, L.; Doerschug, K.; Geersing, G.J.; Klok, F.A.; King, C.S.; Murin, S.; Vintch, J.R.E.; Wells, P.S.; et al. Antithrombotic Therapy for VTE Disease: Compendium and Review of CHEST Guidelines 2012–2021. Chest 2024. [Google Scholar] [CrossRef] [PubMed]
- Wu, M.A.; Del Giovane, C.; Colombo, R.; Dolci, G.; Arquati, M.; Vicini, R.; Russo, U.; Ruggiero, D.; Coluccio, V.; Taino, A.; et al. Low-molecular-weight heparin for the prevention of clinical worsening in severe non-critically ill COVID-19 patients: A joint analysis of two randomized controlled trials. Intern. Emerg. Med. 2024, 19, 71–79. [Google Scholar] [CrossRef]
- Schulman, S.; Kearon, C. Definition of major bleeding in clinical investigations of antihemostatic medicinal products in non-surgical patients. J. Thromb. Haemost. 2005, 3, 692–694. [Google Scholar] [CrossRef]
- Bhoelan, S.; Codreanu, C.; Tichelaar, V.; Borjas Howard, J.; Meijer, K. Exploring heterogeneity in reported venous thromboembolism risk in COVID-19 and comparison to other viral pneumonias: A systematic review and meta-regression. Res. Pract. Thromb. Haemost. 2023, 7, 102146. [Google Scholar] [CrossRef]
- Barnes, G.D.; Burnett, A.; Allen, A.; Ansell, J.; Blumenstein, M.; Clark, N.P.; Crowther, M.; Dager, W.E.; Deitelzweig, S.B.; Ellsworth, S.; et al. Thromboembolic prevention and anticoagulant therapy during the COVID-19 pandemic: Updated clinical guidance from the anticoagulation forum. J. Thromb. Thrombolysis 2022, 54, 197–210. [Google Scholar] [CrossRef] [PubMed]
- Filippi, L.; Turcato, G.; Milan, M.; Barbar, S.; Miozzo, E.; Zaboli, A.; Tonello, D.; Milazzo, D.; Marchetti, M.; Cuppini, S.; et al. Long term follow-up of a multicentre cohort of COVID-19 patients with pulmonary embolism: Anticoagulation management and outcomes. Thromb. Res. 2023, 229, 73–76. [Google Scholar] [CrossRef]
- Demelo-Rodriguez, P.; Alonso-Beato, R.; Jara-Palomares, L.; Galeano-Valle, F.; Bura-Riviere, A.; Visona, A.; Francisco, I.; Vidal, G.; Lopez-Ruiz, A.; Monreal, M.; et al. COVID-19-associated venous thromboembolism: Risk of recurrence and major bleeding. Res. Pract. Thromb. Haemost. 2023, 7, 102206. [Google Scholar] [CrossRef]
- Thachil, J. The versatile heparin in COVID-19. J. Thromb. Haemost. 2020, 18, 1020–1022. [Google Scholar] [CrossRef]



| Whole Cohort (n = 157) | VTE Associated with COVID-19 (n = 30) | VTE Unrelated to COVID-19 (n = 127) | p | ||
|---|---|---|---|---|---|
| Age—years | 69.92 (±14.16) | 66.46 (±13.57) | 70.73 (±14.2) | 0.138 | |
| Male sex—n (%) | 78 (49.7%) | 17 (56.7%) | 61 (48%) | 0.423 | |
| Current smoker—n (%) | 21 (13.4%) | 4 (13.3%) | 17 (13.4%) | >0.999 | |
| Comorbidities—n (%) | |||||
| Hypertension | 85 (54.1%) | 17 (56.7%) | 68 (53.5%) | 0.839 | |
| Diabetes | 22 (14%) | 2 (6.67%) | 20 (12.7%) | 0.253 | |
| Myocardial infarction | 10 (6.4%) | 1 (3.3%) | 9 (7.1%) | 0.688 | |
| Previous VTE episode | 23 (14.6%) | 1 (3.3%) | 22 (17.3%) | 0.080 | |
| Pulmonary hypertension | 1 (0.6%) | 0 | 1 (0.8%) | >0.999 | |
| Chronic Cor pulmonale | 0 | 0 | 0 | >0.999 | |
| Transient ischemic attack | 5 (3.2%) | 0 | 5 (3.9%) | 0.584 | |
| Atrial fibrillation | 6 (3.8%) | 0 | 6 (4.7%) | 0.596 | |
| COPD | 16 (10.2%) | 3 (10%) | 13 (10.2%) | >0.999 | |
| Asthma | 5 (3.2%) | 0 | 5 (3.9%) | 0.584 | |
| Interstitial lung disease | 2 (1.3%) | 0 | 2 (1.6%) | >0.999 | |
| Peptic ulcer | 3 (1.9%) | 1 (3.3%) | 2 (1.6%) | 0.473 | |
| Chronic kidney disease | 11 (7%) | 0 | 11 (8.7%) | 0.125 | |
| Dialysis | 0 | 0 | 0 | >0.999 | |
| Anemia | 9 (5.7%) | 0 | 9 (7.1%) | 0.208 | |
| Recent transfusion | 1 (0.6%) | 0 | 1 (0.8%) | >0.999 | |
| Chronic transfusions | 0 | 0 | 0 | >0.999 | |
| Inflammatory Bowel Disease | 6 (3.8%) | 1 (3.3%) | 5 (3.9%) | 0.839 | |
| Cancer | 35 (22.3%) | 4 (13.3%) | 31 (24.4%) | 0.229 | |
| Antineoplastic treatment | 14 (8.9%) | 1 (3.3%) | 13 (10.2%) | 0.309 | |
| Red Blood Cell Disorder * | 4 (2.5%) | 0 | 4 (3.2%) | >0.999 | |
| Neuropsychiatric disorder ** | 16 (10.2%) | 5 (16.7%) | 11 (8.7%) | 0.192 | |
| Whole Cohort (n = 157) | VTE Associated with COVID-19 (n = 30) | VTE Unrelated to COVID-19 (n = 127) | p | ||
|---|---|---|---|---|---|
| SBP—mmHg | 134 (±22) | 138 (±13) | 133 (±24) | 0.202 | |
| DBP—mmHg | 76 (±12) | 79 (±9) | 76 (±13) | 0.345 | |
| Heart rate—bpm | 93 (±61) | 93 (±21) | 94 (±66) | 0.970 | |
| Respiratory rate—bpm | 24 (±7) | 28 (±7) | 22 (±6) | 0.006 | |
| SO2—% | 94 (±6) | 92 (±6) | 95 (±6) | 0.031 | |
| rGENEVA—n (%) ¶ | 0.581 | ||||
| Low risk (0–3) | 45 (29.03%) | 11 (36.7%) | 34 (27.2%) | ||
| Intermediate risk (4–10) | 91 (58.71%) | 16 (53.3%) | 75 (60%) | ||
| High risk (≥11) | 19 (12.26%) | 3 (10%) | 16 (12.8%) | ||
| sPESI—n (%) † | >0.999 | ||||
| Low risk | 69 (45.1%) | 13 (46.4%) | 56 (44.8%) | ||
| High risk | 84 (54.9%) | 15 (53.6%) | 69 (55.2%) | ||
| PE—n (%) # | 126 (80.3%) | 29 (96.7%) | 97 (76.4%) | 0.01 | |
| Massive PE | 36 (28.6%) | 5 (17.2%) | 31 (32%) | ||
| Lobar PE | 39 (31%) | 9 (31%) | 30 (30.9%) | ||
| Segmental PE | 46 (36.6%) | 13 (44.8%) | 33 (34%) | ||
| Subsegmental PE | 4 (3.2%) | 2 (6.9%) | 2 (2.1%) | ||
| DVT—n (%) | 58 (36.9%) | 1 (3.4%) | 57 (44.9%) | <0.001 | |
| Lower limbs | 47 (81%) | 0 | 47 (82.5%) | ||
| Other DVT * | 11 (19%) | 1 (100%) | 10 (17.5%) | ||
| PE with DVT—n (%) | 28 (17.8%) | 0 | 28 (22%) | 0.002 | |
| Pulmonary hypertension signs at TTE—n (%) § | 17 (18.1%) | 1 (6.67%) | 16 (20.2%) | 0.289 | |
| Whole Cohort (n= 157) | VTE Associated with COVID-19 (n=30) | VTE Unrelated to COVID-19 (n = 127) | p | |
|---|---|---|---|---|
| Hb—g/dL | 13.7 (±9.1) | 13.3 (±1.7) | 13.9 (±10.2) | 0.760 |
| Hct—% | 38.2 (±6.5) | 39.3 (±5.1) | 37.9 (±6.8) | 0.346 |
| WBC—cell/mm3 | 9469 (±3720) | 9782 (±2998) | 9384 (±3900) | 0.605 |
| Platelets—cell/mm3 | 241,712 (±90,878) | 264,600 (±76,704) | 235,793 (±93,582) | 0.122 |
| INR | 1.17 (±0.16) | 1.16 (±0.13) | 1.17 (±0.17) | 0.866 |
| aPTT ratio | 0.97 (±0.11) | 0.99 (±0.13) | 0.96 (±0.11) | 0.224 |
| D-dimer—ng/mL | 9518 (±14,866) | 8622 (±11,378) | 9943 (±16,335) | 0.701 |
| CRP—mg/L | 67.6 (±94.2) | 86.7 (±102.5) | 62.6 (±91.8) | 0.230 |
| Creatinine—mg/dL | 1.02 (±0.5) | 0.94 (±0.46) | 1.05 (±0.52) | 0.300 |
| ALT—U/I | 29.8 (±41.9) | 29.2 (±13.9) | 29.9 (±46.7) | 0.931 |
| Bilirubin—mg/dL | 1.03 (±0.4) | 0.96 (±0.1) | 1.05 (±0.4) | 0.099 |
| CK—U/I | 315 (±1986) | 301 (±670) | 318.64 (±2231) | 0.968 |
| LDH—U/I | 284 (±96) | 322 (±110) | 274 (±90) | 0.044 |
| hs-TnT—ng/L | 38.8 (±77.6) | 17.2 (±16) | 44 (±85.4) | 0.232 |
| NTpro-BNP—ng/L | 1317 (±2283) | 264 (±303) | 1503 (±2436) | 0.401 |
| Whole Cohort (n = 157) | VTE Associated with COVID-19 (n = 30) | VTE Unrelated to COVID-19 (n = 127) | p | |
|---|---|---|---|---|
| First treatment | ||||
| LMWH—n (%) | 130 (79.62%) | 29 (96.7%) | 101 (79.53%) | 0.158 |
| Fondaparinux—n (%) | 15 (9.55%) | 1 (3.3%) | 14 (11.02%) | |
| UFH—n (%) | 4 (3.82%) | 0 | 4 (3.15%) | |
| DOAC—n (%) | 8 (5.09%) | 0 | 8 (4.72%) | |
| Treatment after first outpatient visit | 0.623 * | |||
| LMWH—n (%) | 21 (13.37%) | 4 (13.33%) | 17 (13.38%) | |
| Fondaparinux—n (%) | 11 (7%) | 1 (3.3%) | 10 (7.87%) | |
| UFH—n (%) | 0 | 0 | 0 | |
| DOAC—n (%) | 123 (78.34%) | 25 (83.33%) | 98 (77.16%) | |
| Warfarin—n (%) | 2 (1.27%) | 0 | 2 (1.57%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wu, M.A.; Taino, A.; Facchinetti, P.; Rossi, V.; Ruggiero, D.; Berra, S.; Blanda, G.; Flor, N.; Cogliati, C.; Colombo, R. Venous Thromboembolism Management throughout the COVID-19 Era: Addressing Acute and Long-Term Challenges. J. Clin. Med. 2024, 13, 1825. https://doi.org/10.3390/jcm13061825
Wu MA, Taino A, Facchinetti P, Rossi V, Ruggiero D, Berra S, Blanda G, Flor N, Cogliati C, Colombo R. Venous Thromboembolism Management throughout the COVID-19 Era: Addressing Acute and Long-Term Challenges. Journal of Clinical Medicine. 2024; 13(6):1825. https://doi.org/10.3390/jcm13061825
Chicago/Turabian StyleWu, Maddalena Alessandra, Alba Taino, Pietro Facchinetti, Valentina Rossi, Diego Ruggiero, Silvia Berra, Giulia Blanda, Nicola Flor, Chiara Cogliati, and Riccardo Colombo. 2024. "Venous Thromboembolism Management throughout the COVID-19 Era: Addressing Acute and Long-Term Challenges" Journal of Clinical Medicine 13, no. 6: 1825. https://doi.org/10.3390/jcm13061825
APA StyleWu, M. A., Taino, A., Facchinetti, P., Rossi, V., Ruggiero, D., Berra, S., Blanda, G., Flor, N., Cogliati, C., & Colombo, R. (2024). Venous Thromboembolism Management throughout the COVID-19 Era: Addressing Acute and Long-Term Challenges. Journal of Clinical Medicine, 13(6), 1825. https://doi.org/10.3390/jcm13061825