Transjugular Intrahepatic Portosystemic Shunt as a Bridge to Abdominal Surgery in Cirrhosis
Abstract
:1. Introduction
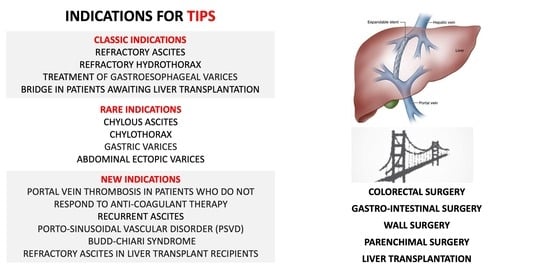
Indication for TIPS
- Refractory ascites and/or refractory hydrothorax;
- Treatment of gastroesophageal varices as secondary prophylaxis of variceal bleeding or as rescue therapy for uncontrolled bleeding;
- Bridge in patients awaiting liver transplantation, particularly in patients with portal hypertension complications. No significative difference was reported in the recent literature on the post-transplant outcome, comparing patients with TIPS and no TIPS, regarding postoperative complications, transfusion requirement, length of stay, and re-transplantation rate [27].
- Chylous ascites and chylothorax;
- Gastric varices;
- Abdominal ectopic varices.
- Portal vein thrombosis in patients who do not respond to anti-coagulant therapy and as an attempt in patients with an extension of the thrombosis that contraindicates liver transplantation;
- Recurrent ascites;
- Vascular disorders such as Porto-sinusoidal Vascular Disorder (PSVD) and Budd–Chiari Syndrome;
- Refractory ascites in liver transplant recipients. This complication occurred in 5–7% of patients. The use of post-liver transplant TIPS was reported in a large series by Saad et al. [28], including 39 cases of refractory ascites and variceal bleeding after transplant. In this series, the PSPG of 10 mmHg after TIPS placement. Bianco et al. [29] presented three cases of refractory ascites after transplant in patients without chronic disease recurrence. In all cases, refractory ascites were resolved after TIPS placement.
2. Colorectal Surgery
3. Upper-Gastrointestinal Surgery
4. Wall Surgery
5. Parenchymal Surgery
6. TIPS as a Bridge to Liver Transplantation
7. Discussion and Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- del Olmo, J.A.; Flor-Lorente, B.; Flor-Civera, B.; Rodriguez, F.; Serra, M.A.; Escudero, A.; Lledó, S.; Rodrigo, J.M. Risk factors for nonhepatic surgery in patients with cirrhosis. World J. Surg. 2003, 27, 647–652. [Google Scholar] [CrossRef]
- Fagiuoli, S.; Bruno, R.; Debernardi Venon, W.; Schepis, F.; Vizzutti, F.; Toniutto, P.; Senzolo, M.; Caraceni, P.; Salerno, F.; Angeli, P.; et al. Consensus conference on TIPS management: Techniques, indications, contraindications. Dig. Liver Dis. 2017, 49, 121–137. [Google Scholar] [CrossRef]
- Jain, D.; Mahmood, E.; V-Bandres, M.; Feyssa, E. Preoperative elective transjugular intrahepatic portosystemic shunt for cirrhotic patients undergoing abdominal surgery. Ann. Gastroenterol. 2018, 31, 330–337. [Google Scholar] [CrossRef]
- Tabchouri, N.; Barbier, L.; Menahem, B.; Perarnau, J.M.; Muscari, F.; Fares, N.; D’Alteroche, L.; Valette, P.J.; Dumortier, J.; Alves, A.; et al. Original Study: Transjugular Intrahepatic Portosystemic Shunt as a Bridge to Abdominal Surgery in Cirrhotic Patients. J. Gastrointest. Surg. 2019, 23, 2383–2390. [Google Scholar] [CrossRef]
- Reverter, E.; Cirera, I.; Albillos, A.; Debernardi-Venon, W.; Abraldes, J.G.; Llop, E.; Flores, A.; Martínez-Palli, G.; Blasi, A.; Martínez, J.; et al. The prognostic role of hepatic venous pressure gradient in cirrhotic patients undergoing elective extrahepatic surgery. J. Hepatol. 2019, 71, 942–950. [Google Scholar] [CrossRef]
- Patel, P.; Irani, M.; Graviss, E.A.; Nguyen, D.T.; Quigley, E.M.M.; Victor, D.W., III. Impact of pre-operative transjugular intrahepatic portosystemic shunt on post-operative outcomes following non-transplant surgeries in patients with decompensated cirrhosis. Transl. Gastroenterol. Hepatol. 2023, 8, 9. [Google Scholar] [CrossRef]
- Piecha, F.; Vonderlin, J.; Frühhaber, F.; Graß, J.K.; Ozga, A.K.; Harberts, A.; Benten, D.; Hübener, P.; Reeh, M.; Riedel, C.; et al. Preoperative TIPS and in-hospital mortality in patients with cirrhosis undergoing surgery. JHEP Rep. 2023, 6, 100914. [Google Scholar] [CrossRef]
- da Saltini, D.; Indulti, F.; Guasconi, T.; Bianchini, M.; Cuffari, B.; Caporali, C.; Casari, F.; Prampolini, F.; Senzolo, M.; Colecchia, A.; et al. Transjugular Intrahepatic Portosystemic Shunt: Devices Evolution, Technical Tips and Future Perspectives. J. Clin. Med. 2023, 12, 6758. [Google Scholar] [CrossRef]
- Vinet, E.; Perreault, P.; Bouchard, L.; Bernard, D.; Wassef, R.; Richard, C.; Létourneau, R.; Pomier-Layrargues, G. Transjugular intrahepatic portosystemic shunt before abdominal surgery in cirrhotic patients: A retrospective, comparative study. Can. J. Gastroenterol. 2006, 20, 401–404. [Google Scholar] [CrossRef]
- Goel, A.; Khanna, A.; Mehrzad, H.; Bach, S.; Karkhanis, S.; Kamran, U.; Morgan, J.; Rajoriya, N.; Tripathi, D. Portal decompression with transjugular intrahepatic portosystemic shunt prior to nonhepatic surgery: A single-center case series. Eur. J. Gastroenterol. Hepatol. 2021, 33, e254–e259. [Google Scholar] [CrossRef]
- Kapeleris, A.P.P.; Venkatachalapathy, S. TIPSS as a bridge to extrahepatic abdominal surgery: A case report. Oxf. Med. Case Rep. 2022, 2022, 129–131. [Google Scholar] [CrossRef]
- Azoulay, D.; Buabse, F.; Damiano, I.; Smail, A.; Ichai, P.; Dannaoui, M.; Castaing, D.; Bismuth, H. Neoadjuvant transjugular intrahepatic portosystemic shunt: A solution for extrahepatic abdominal operation in cirrhotic patients with severe portal hypertension. J. Am. Coll. Surg. 2001, 193, 46–51. [Google Scholar] [CrossRef]
- Schlenker, C.; Johnson, S.; Trotter, J.F. Preoperative transjugular intrahepatic portosystemic shunt (TIPS) for cirrhotic patients undergoing abdominal and pelvic surgeries. Surg. Endosc. 2009, 23, 1594–1598. [Google Scholar] [CrossRef]
- Gil, A.; Martínez-Regueira, F.; Hernández-Lizoain, J.L.; Pardo, F.; Olea, J.M.; Bastarrika, G.; Cienfuegos, J.A.; Bilbao, J.I. The role of transjugular intrahepatic portosystemic shunt prior to abdominal tumoral surgery in cirrhotic patients with portal hypertension. Eur. J. Surg. Oncol. 2004, 30, 46–52. [Google Scholar] [CrossRef]
- Masood, I.; Saleem, A.; Malik, K.; Rashidi, L.; Kathuria, M. TIPS to the rescue: Preoperative Transjugular Intrahepatic Portosystemic Shunt (TIPS) placement in a patient with caput medusae and colon cancer. Radiol. Case Rep. 2020, 15, 1423–1427. [Google Scholar] [CrossRef]
- Fares, N.; Robic, M.A.; Péron, J.M.; Muscari, F.; Otal, P.; Suc, B.; Vinel, J.P.; Bureau, C. Transjugular intrahepatic portosystemic shunt placement before abdominal intervention in cirrhotic patients with portal hypertension: Lessons from a pilot study. Eur. J. Gastroenterol. Hepatol. 2018, 30, 21–26. [Google Scholar] [CrossRef]
- Schmitz, A.; Haste, P.; Johnson, M.S. Transjugular Intrahepatic Portosystemic Shunt (TIPS) Creation Prior to Abdominal Operation: A Retrospective Analysis. J. Gastrointest. Surg. 2020, 24, 2228–2232. [Google Scholar] [CrossRef]
- de Andres Olabarria, U.; Ugarte Sierra, S.; Maniega Alba, R.; Alberdi San Roman, I.; Ibáñez Aguirre, F.J. Laparoscopic myotomy after transjugular intrahepatic portosystemic shunt placement and embolization of gastroesophageal varices in patients with achalasia and cirrhosis. Cir. Española 2017, 95, 296–297. [Google Scholar] [CrossRef]
- Becq, A.; Ozenne, V.; Plessier, A.; Valleur, P.; Dray, X. Transjugular intrahepatic portosystemic shunt as bridge-to-surgery in refractory gastric antral vascular ectasia. World J. Gastroenterol. 2015, 21, 5749–5750. [Google Scholar] [CrossRef]
- Chang, J.; Höfer, P.; Böhling, N.; Lingohr, P.; Manekeller, S.; Kalff, J.C.; Dohmen, J.; Kaczmarek, D.J.; Jansen, C.; Meyer, C.; et al. Preoperative TIPS prevents the development of postoperative acute-on-chronic liver failure in patients with high CLIF-C AD score. JHEP Rep. 2022, 4, 100442. [Google Scholar] [CrossRef]
- Aryan, M.; McPhail, J.; Ravi, S.; Harris, P.; Allamneni, C.; Shoreibah, M. Perioperative Transjugular Intrahepatic Portosystemic Shunt Is Associated With Decreased Postoperative Complications in Decompensated Cirrhotics Undergoing Abdominal Surgery. Am. Surg. 2022, 88, 1613–1620. [Google Scholar] [CrossRef]
- Telem, D.A.; Schiano, T.; Divino, C.M. Complicated hernia presentation in patients with advanced cirrhosis and refractory ascites: Management and outcome. Surgery 2010, 148, 538–543. [Google Scholar] [CrossRef]
- Jabbar, S.A.; Jamieson, N.B.; Morris, A.J.; Oien, K.A.; Duthie, F.; McKay, C.J.; Carter, C.R.; Dickson, E.J. A Glasgow Tipple-transjugular intrahepatic portosystemic shunt insertion prior to Whipple resection. J. Surg. Case Rep. 2016, 2016, rjw089. [Google Scholar] [CrossRef]
- Grübel, P.; Pratt, D.S.; Elhelw, T. Transjugular intrahepatic portosystemic shunt for portal decompression before abdominal and retroperitoneal surgery in patients with severe portal hypertension. J. Clin. Gastroenterol. 2002, 34, 489–490. [Google Scholar] [CrossRef]
- Lapenna, L.; Di Cola, S.; Gazda, J.; De Felice, I.; Gioia, S.; Merli, M. New Indications for TIPSs: What Do We Know So Far? J. Clin. Exp. Hepatol. 2023, 13, 794–803. [Google Scholar] [CrossRef]
- Rajesh, S.; George, T.; Philips, C.A.; Ahamed, R.; Kumbar, S.; Mohan, N.; Mohanan, M.; Augustine, P. Transjugular intrahepatic portosystemic shunt in cirrhosis: An exhaustive critical update. World J. Gastroenterol. 2020, 26, 5561–5596. [Google Scholar] [CrossRef]
- Di Cola, S.; Lapenna, L.; Gazda, J.; Fonte, S.; Cusi, G.; Esposito, S.; Mattana, M.; Merli, M. Role of Transjugular Intrahepatic Portosystemic Shunt in the Liver Transplant Setting. J. Clin. Med. 2024, 13, 600. [Google Scholar] [CrossRef]
- Saad, W.E.; Darwish, W.M.; Davies, M.G.; Waldman, D.L. Transjugular intrahepatic portosystemic shunts in liver transplant recipients for management of refractory ascites: Clinical outcome. J. Vasc. Interv. Radiol. 2010, 21, 218–223. [Google Scholar] [CrossRef]
- Bianco, G.; Pascale, M.M.; Frongillo, F.; Nure, E.; Agnes, S.; Spoletini, G. Transjugular portosystemic shunt for early-onset refractory ascites after liver transplantation. Hepatobiliary Pancreat. Dis. Int. 2021, 20, 90–93. [Google Scholar] [CrossRef]
- Patel, R.K.; Chandel, K.; Tripathy, T.P.; Mukund, A. Complications of transjugular intrahepatic portosystemic shunt (TIPS) in the era of the stent graft—What the interventionists need to know? Eur. J. Radiol. 2021, 144, 109986. [Google Scholar] [CrossRef]
- Nardelli, S.; Riggio, O.; Marra, F.; Gioia, S.; Saltini, D.; Bellafante, D.; Adotti, V.; Guasconi, T.; Ridola, L.; Rosi, M.; et al. Episodic overt hepatic encephalopathy after transjugular intrahepatic portosystemic shunt does not increase mortality in patients with cirrhosis. J. Hepatol. 2023, 80, 596–602. [Google Scholar] [CrossRef]
- Abbas, N.; Fallowfield, J.; Patch, D.; Stanley, A.J.; Mookerjee, R.; Tsochatzis, E.; Leithead, J.A.; Hayes, P.; Chauhan, A.; Sharma, V.; et al. Guidance document: Risk assessment of patients with cirrhosis prior to elective non-hepatic surgery. Frontline Gastroenterol. 2023, 14, 359–370. [Google Scholar] [CrossRef]
- Menahem, B.; Lubrano, J.; Desjouis, A.; Lepennec, V.; Lebreton, G.; Alves, A. Transjugular intrahepatic portosystemic shunt placement increases feasibility of colorectal surgery in cirrhotic patients with severe portal hypertension. Dig. Liver Dis. 2015, 47, 81–84. [Google Scholar] [CrossRef]
- Lai, Q.; Spoletini, G.; Pinheiro, R.S.; Melandro, F.; Guglielmo, N.; Lerut, J. From portal to splanchnic venous thrombosis: What surgeons should bear in mind. World J. Hepatol. 2014, 6, 549–558. [Google Scholar] [CrossRef]
- Ghinolfi, D.; Melandro, F.; Torri, F.; Martinelli, C.; Cappello, V.; Babboni, S.; Silvestrini, B.; De Simone, P.; Basta, G.; Del Turco, S. Extended criteria grafts and emerging therapeutics strategy in liver transplantation. The unstable balance between damage and repair. Transplant. Rev. 2021, 35, 100639. [Google Scholar] [CrossRef]
- Sellers, C.M.; Nezami, N.; Schilsky, M.L.; Kim, H.S. Transjugular intrahepatic portosystemic shunt as a bridge to liver transplant: Current state and future directions. Transplant. Rev. 2019, 33, 64–71. [Google Scholar] [CrossRef]
- Mumtaz, K.; Metwally, S.; Modi, R.M.; Patel, N.; Tumin, D.; Michaels, A.J.; Hanje, J.; El-Hinnawi, A.; Hayes, D., Jr.; Black, S.M. Impact of transjugular intrahepatic porto-systemic shunt on post liver transplantation outcomes: Study based on the United Network for Organ Sharing database. World J. Hepatol. 2017, 9, 99–105. [Google Scholar] [CrossRef]
- Guerrini, G.P.; Pleguezuelo, M.; Maimone, S.; Calvaruso, V.; Xirouchakis, E.; Patch, D.; Rolando, N.; Davidson, B.; Rolles, K.; Burroughs, A. Impact of tips preliver transplantation for the outcome posttransplantation. Am. J. Transplant. 2009, 9, 192–200. [Google Scholar] [CrossRef]
- Levi Sandri, G.B.; Lai, Q.; Lucatelli, P.; Melandro, F.; Guglielmo, N.; Mennini, G.; Berloco, P.B.; Fanelli, F.; Salvatori, F.M.; Rossi, M. Transjugular intrahepatic portosystemic shunt for a wait list patient is not a contraindication for orthotopic liver transplant outcomes. Exp. Clin. Transplant. 2013, 11, 426–428. [Google Scholar] [CrossRef]
- Barbier, L.; Hardwigsen, J.; Borentain, P.; Biance, N.; Daghfous, A.; Louis, G.; Botta-Fridlund, D.; Le Treut, Y.P. Impact of transjugular intrahepatic portosystemic shunting on liver transplantation: 12-year single-center experience. Clin. Res. Hepatol. Gastroenterol. 2014, 38, 155–163. [Google Scholar] [CrossRef]
- Manzano-Nunez, R.; Jimenez-Masip, A.; Chica-Yanten, J.; Ibn-Abdelouahab, A.; Sartelli, M.; de’Angelis, N.; Moore, E.E.; García, A.F. Unlocking the potential of TIPS placement as a bridge to elective and emergency surgery in cirrhotic patients: A meta-analysis and future directions for endovascular resuscitation in acute care surgery. World J. Emerg. Surg. 2023, 18, 30. [Google Scholar] [CrossRef]
- Lahat, E.; Lim, C.; Bhangui, P.; Fuentes, L.; Osseis, M.; Moussallem, T.; Salloum, C.; Azoulay, D. Transjugular intrahepatic portosystemic shunt as a bridge to non-hepatic surgery in cirrhotic patients with severe portal hypertension: A systematic review. HPB 2018, 20, 101–109. [Google Scholar] [CrossRef]
- Philip, M.; Thornburg, B. Preoperative Transjugular Intrahepatic Portosystemic Shunt Placement for Extrahepatic Abdominal Surgery. Semin. Interv. Radiol. 2018, 35, 203–205. [Google Scholar] [CrossRef]

| Study | Stage of Cirrhosis | Number of Cases | Surgical Procedure | Time between TIPS Placement and Surgery | Major Complications |
|---|---|---|---|---|---|
| Colorectal surgery | |||||
| Vinet, Canada, 2006 [9] | NR | 10 TIPS group NO TIPS group | Colon resection | NR | NR |
| Tabchouri, France, 2019 [4] | CTP A,B,C | 30 TIPS group 38 NO TIPS group | Colon resection | Median 40 days | No perioperative major complications (90-day mortality: 1 in TIPS group, 4 in NO TIPS group) |
| Goel, UK, 2020 [10] | CTP A | 15 | Colectomy | 38 days | NR |
| Kepeleris, UK, 2022 [11] | CTP A:1 CTP B: 1 | 2 | Colon resection | NR | NR |
| Azulay, France, 2001 [12] | CTP A and B | 2 | Colon resection | NR | Death of one patient |
| Schlenker, US, 2009 [13] | CTP A and B | 1 | Colon resection | Median 13 days | Ascites; wound infection treated with drainage and antibiotics |
| Gil, Spain, 2004 [14] | CTP B7 | 1 | Right hemicolectomy | 30 days | Right cardiac insufficiency, encephalopathy |
| Masood, US, 2020 [15] | NR | 1 | Laparoscopic right hemicolectomy | 60 days | No perioperative major complications |
| Fares, France, 2018 [16] | CTP A-B | 6 | Colon resection | NR | Ascites and wound infection |
| Upper-Gastrointestinal Surgery | |||||
| Schmitz, US, 2020 [17] | CTP A | 8 | Sleeve gastrectomy (6), gastrectomy (1), esophagectomy (1) | Mean 38, 7 days | No perioperative major complications |
| Vinet, Canada, 2006 [9] | NR | 5 TIPS group 1 NO TIPS group | Gastrectomy | NR | NR |
| Schlenker, US, 2009 [13] | CTP A | 1 | Gastrectomy | Mean 13 days | No perioperative major complications |
| Gil, Spain, 2004 [14] | CTP A5 | 1 | Subtotal gastrectomy | 45 days | No perioperative major complications |
| de Andres, Spain, 2020 [18] | CTP class A | 1 | Laparoscopic Heller myotomy + dor fundoplication | 42 days | No perioperative major complications |
| Becq, France, 2015 [19] | NR | 1 | Antrectomy | 90 days | No perioperative major complications |
| Fares, France, 2018 [16] | CTP A-B | 3 | Gastric or duodenum resection | NR | NR |
| Wall surgery | |||||
| Chang, Germany 2022 [20] | CTP A or B | 11 | Hernia repair | Mean 6 months | Ascites, HE, ACLF, infections, blood transfusions |
| Aryan, UK, 2022 [21] | NR | 21 TIPS group 13 NO TIPS group | Hernia repair | median 8 days | Rate of ascites, HE, infections, AKI higher in NO TIPS group |
| Fares, France, 2018 [16] | CTP B-C | 5 | Hernia repair | Median 24 days | No major complications |
| Telem, US 2010 [22] | NR | 6 | Hernia repair | One day | No major complications |
| Parenchymal Surgery | |||||
| Vinet, Canada, 2006 [9] | NR | 2 TIPS group 3 NO TIPS group | Pancreatoduodenectomy nephrectomy | NR | Ascites, HE, infections: no significative reduction in TIPS group |
| Jabbar, UK, 2016 [23] | NR | 1 | Pancreatoduodenectomy | NR | No major complications |
| Gil, Spain, 2004 [14] | CTP A 6 | 1 | Pancreatoduodenectomy | 14 days | No major complications |
| Azulay, France, 2001 [12] | CTP A 6 | 1 | Kidney resection | NR | No major complications |
| Schlenker, US, 2009 [13] | CTP A | 1 | Nephrectomy | Mean 13 days | No major complications |
| Grubel, US, 2002 [24] | CTP C | 1 | Nephrectomy | 56 days | No major complications |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Melandro, F.; Parisse, S.; Ginanni Corradini, S.; Cardinale, V.; Ferri, F.; Merli, M.; Alvaro, D.; Pugliese, F.; Rossi, M.; Mennini, G.; et al. Transjugular Intrahepatic Portosystemic Shunt as a Bridge to Abdominal Surgery in Cirrhosis. J. Clin. Med. 2024, 13, 2213. https://doi.org/10.3390/jcm13082213
Melandro F, Parisse S, Ginanni Corradini S, Cardinale V, Ferri F, Merli M, Alvaro D, Pugliese F, Rossi M, Mennini G, et al. Transjugular Intrahepatic Portosystemic Shunt as a Bridge to Abdominal Surgery in Cirrhosis. Journal of Clinical Medicine. 2024; 13(8):2213. https://doi.org/10.3390/jcm13082213
Chicago/Turabian StyleMelandro, Fabio, Simona Parisse, Stefano Ginanni Corradini, Vincenzo Cardinale, Flaminia Ferri, Manuela Merli, Domenico Alvaro, Francesco Pugliese, Massimo Rossi, Gianluca Mennini, and et al. 2024. "Transjugular Intrahepatic Portosystemic Shunt as a Bridge to Abdominal Surgery in Cirrhosis" Journal of Clinical Medicine 13, no. 8: 2213. https://doi.org/10.3390/jcm13082213
APA StyleMelandro, F., Parisse, S., Ginanni Corradini, S., Cardinale, V., Ferri, F., Merli, M., Alvaro, D., Pugliese, F., Rossi, M., Mennini, G., & Lai, Q. (2024). Transjugular Intrahepatic Portosystemic Shunt as a Bridge to Abdominal Surgery in Cirrhosis. Journal of Clinical Medicine, 13(8), 2213. https://doi.org/10.3390/jcm13082213