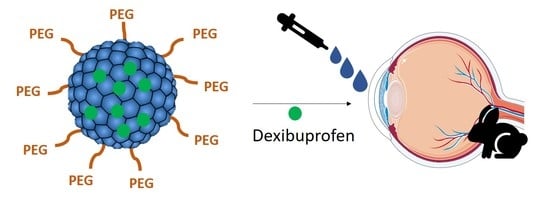
Dexibuprofen Biodegradable Nanoparticles: One Step Closer towards a Better Ocular Interaction Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Preparation of Polymeric Nanoparticles
2.2. Characterization of Formulations
2.2.1. Particle Size, Zeta Potential and Polydispersity (PI)
2.2.2. Entrapment Efficiency (EE)
2.2.3. Transmission Electron Microscopy
2.2.4. Interaction Studies
2.3. In Vitro Release Study
2.4. Sterilization Using Gamma Radiation
2.5. In Vitro Ocular Irritation Assay: HET-CAM
2.6. In Vivo Ocular Irritation Assay
2.7. In Vitro Customized Corneal Membrane Model and Interactions Study
2.7.1. Langmuir Monolayers
2.7.2. Preparation of Fluorescent Labeled LUVs
2.7.3. Interaction of DXI NPs with Model Membranes
2.8. Prevention of In Vivo Ocular Inflammation
2.9. Ex Vivo Ocular Permeation
3. Results and Discussion
3.1. Characterization of the Nanocarriers
3.2. DXI NPs Characterization Studies
3.3. Sterilization Using Gamma Radiation
3.4. In Vitro Drug Release
3.5. Ocular Tolerance
3.6. In Vitro Interactions with a Customized Corneal Membrane Model
3.6.1. π-A Isotherm Analysis
3.6.2. Membrane Dipole Potential Changes
3.7. Ocular Inflammation
3.8. Ex Vivo Permeation Assay
4. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Rainsford, K.D. Ibuprofen: Pharmacology, efficacy and safety. Inflammopharmacology 2009, 17, 275–342. [Google Scholar] [CrossRef] [PubMed]
- Kaehler, S.T.; Phleps, W.; Hesse, E. Dexibuprofen: Pharmacology, therapeutic uses and safety. Inflammopharmacology 2003, 11, 371–383. [Google Scholar] [CrossRef] [PubMed]
- Bucolo, C.; Puglisi, G. Enhanced Ocular Anti-Inflammatory Activity of Ibuprofen Carried by an Eudragit RS100 ® Nanoparticle Suspension. Opthalmic 2002, 34, 319–323. [Google Scholar] [CrossRef] [PubMed]
- Ariza-Sáenz, M.; Espina, M.; Bolaños, N.; Calpena, A.C.; Gomara, M.J.; Haro, I.; García, M.L. Penetration of polymeric nanoparticles loaded with an HIV-1 inhibitor peptide derived from GB virus C in a vaginal mucosa model. Eur. J. Pharm. Biopharm. 2017, 120, 98–106. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Suk, J.S.; Xu, Q.; Kim, N.; Hanes, J.; Ensign, L.M.; Sciences, H.; Sciences, M. PEGylation as a strategy for improving nanoparticle-based drug and gene delivery. Adv. Drug Deliv. Rev. 2016, 99, 28–51. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ledezma, D.K.; Balakrishnan, P.B.; Cano-mejia, J.; Sweeney, E.E.; Hadley, M.; Bollard, C.M.; Villagra, A. Indocyanine Green-Nexturastat A-PLGA Nanoparticles Combine Photothermal and Epigenetic Therapy for Melanoma. Nanomaterials 2020, 10, 161. [Google Scholar] [CrossRef] [Green Version]
- Locatelli, E.; Franchini, M.C. Biodegradable PLGA-b-PEG polymeric nanoparticles: Synthesis, properties, and nanomedical applications as drug delivery system. J. Nanoparticle Res. 2012, 14, 1–17. [Google Scholar] [CrossRef]
- Dorati, R.; DeTrizio, A.; Spalla, M.; Migliavacca, R.; Pagani, L.; Pisani, S.; Chiesa, E.; Conti, B.; Modena, T.; Genta, I. Gentamicin Sulfate PEG-PLGA/PLGA-H nanoparticles: Screening design and antimicrobial effect evaluation toward clinic bacterial isolates. Nanomaterials 2018, 8, 37. [Google Scholar] [CrossRef] [Green Version]
- EMA/CHMP. Information for the package leaflet regarding polysorbates used as excipients in medicinal products for human use. Eur. Med. Agency Comm. Med. Prod. Hum. Use 2017, 44, 1–42. [Google Scholar]
- Sánchez-López, E.; Ettcheto, M.; Egea, M.A.; Espina, M.; Calpena, A.C.; Folch, J.; Camins, A.; García, M.L. New potential strategies for Alzheimer’s disease prevention: Pegylated biodegradable dexibuprofen nanospheres administration to APPswe/PS1dE9. Nanomed. Nanotechnol. Biol. Med. 2017, 13, 1171–1182. [Google Scholar] [CrossRef]
- Sánchez-López, E.; Egea, M.A.; Cano, A.; Espina, M.; Calpena, A.C.; Ettcheto, M.; Camins, A.; Souto, E.B.; Silva, A.M.; García, M.L. PEGylated PLGA nanospheres optimized by design of experiments for ocular administration of dexibuprofen– in vitro, ex vivo and in vivo characterization. Colloids Surf. B Biointerfaces 2016, 145, 241–250. [Google Scholar] [CrossRef] [Green Version]
- Cano, A.; Ettcheto, M.; Espina, M.; Auladell, C.; Calpena, A.C.; Folch, J.; Barenys, M.; Sánchez-López, E.; Camins, A.; García, M.L. Epigallocatechin-3-gallate loaded PEGylated-PLGA nanoparticles: A new anti-seizure strategy for temporal lobe epilepsy. Nanomed. Nanotechnol. Biol. Med. 2018, 14, 1073–1085. [Google Scholar] [CrossRef] [PubMed]
- Carvajal-Vidal, P.; Fábrega, M.J.; Espina, M.; Calpena, A.C.; García, M.L. Development of Halobetasol-loaded nanostructured lipid carrier for dermal administration: Optimization, physicochemical and biopharmaceutical behavior, and therapeutic efficacy. Nanomed. Nanotechnol. Biol. Med. 2019, 20, 102026. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez-Mira, E.; Nikolic, S.; Calpena, A.C.; Egea, M.A.; Souto, E.B.; García, M.L. Improved and safe transcorneal delivery of flurbiprofen by NLC and NLC-based hydrogels. J. Pharm. Sci. 2012, 101, 707–725. [Google Scholar] [CrossRef] [PubMed]
- Ramos, G.R.; García, M.L.; Espina, M.; Coca, A.P.; Calpena, A.C. Influence of freeze-drying and γ -irradiation in preclinical studies of flurbiprofen polymeric nanoparticles for ocular delivery using d-(+)-trehalose and polyethylene glycol. Int. J. Nanomed. 2016, 11, 4093–4106. [Google Scholar] [CrossRef] [Green Version]
- Yeo, Y.; Ito, T.; Bellas, E.; Highley, C.B.; Marini, R.; Kohane, D.S. In situ cross-linkable hyaluronan hydrogels containing polymeric nanoparticles for preventing postsurgical adhesions. Ann. Surg. 2007, 245, 819–824. [Google Scholar] [CrossRef] [PubMed]
- Invittox-Protocol. Ergatt/Frame data bank of in vitro techniques in toxicology. Toxicol. Vitro 1990, 4, 707–710. [Google Scholar] [CrossRef]
- Jírová, D.; Kejlová, K.; Janoušek, S.; Bendová, H.; Malý, M.; Kolářová, H.; Dvořáková, M. Eye irritation hazard of chemicals and formulations assessed by methods in vitro. Neuroendocrinol. Lett. 2014, 35, 133–140. [Google Scholar]
- Vasconcelos, A.; Vega, E.; Pérez, Y.; Gómara, M.J.; García, M.L.; Haro, I. Conjugation of cell-penetrating peptides with poly(lactic-co-glycolic acid)-polyethylene glycol nanoparticles improves ocular drug delivery. Int. J. Nanomedicine 2015, 10, 609–631. [Google Scholar]
- Sánchez-López, E.; Egea, M.A.; Davis, B.M.; Guo, L.; Espina, M.; Silva, A.M.; Calpena, A.C.; Souto, E.M.B.; Ravindran, N.; Ettcheto, M.; et al. Memantine-Loaded PEGylated Biodegradable Nanoparticles for the Treatment of Glaucoma. Small 2018, 14, 1–12. [Google Scholar] [CrossRef]
- Keller, H.; Worch, R.; Schwille, P. Model membrane systems. In Protein-Ligand Interactions: Methods and Applications. Methods in Molecular Biology; Springer-Science+Business Media: Berlin/Heidelberg, Germany, 2013; pp. 417–437. [Google Scholar]
- Davies, J.T.; Rideal, E.K. Interfacial Phenomena; Academic Press: New York, NY, USA, 1963. [Google Scholar]
- Maget-Dana, R. The monolayer technique: A potent tool for studying the interfacial properties of antimicrobial and membrane-lytic peptides and their interactions with lipid membranes. BBA Biomembr. 1999, 1462, 109–140. [Google Scholar] [CrossRef] [Green Version]
- Vitovic, P.; Subjakova, V.; Hianik, T. The physical properties of lipid monolayers and bilayers containing calixarenes sensitive to cytochrome c. Gen. Physiol. Biophys. 2013, 32, 189–200. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Clarke, R.J. Effect of lipid structure on the dipole potential of phosphatidylcholine bilayers. Biochim. Biophys. Acta Biomembr. 1997, 1327, 269–278. [Google Scholar] [CrossRef] [Green Version]
- Ortiz, A.; Girona, V. Interaction of the GBV-C E2-derived peptide, P6-2VIR576, with anionic phospholipid membranes. Colloids Surf. A 2017, 532, 483–492. [Google Scholar] [CrossRef]
- Cladera, J.; O’Shea, P. Intramembrane molecular dipoles affect the membrane insertion and folding of a model amphiphilic peptide. Biophys. J. 1998, 74, 2434–2442. [Google Scholar] [CrossRef] [Green Version]
- Starke-Peterkovic, T.; Turner, N.; Vitha, M.F.; Waller, M.P.; Hibbs, D.E.; Clarke, R.J. Cholesterol effect on the dipole potential of lipid membranes. Biophys. J. 2006, 90, 4060–4070. [Google Scholar] [CrossRef] [Green Version]
- Gonzalez-Pizarro, R.; Carvajal-Vidal, P.; Halbault Bellowa, L.; Calpena, A.C.; Espina, M.; García, M.L. In-situ forming gels containing fluorometholone-loaded polymeric nanoparticles for ocular inflammatory conditions. Colloids Surf. B Biointerfaces 2019, 175, 365–374. [Google Scholar] [CrossRef]
- Gómez-Segura, L.; Parra, A.; Calpena-Campmany, A.C.; Gimeno, Á.; de Aranda, I.G.; Boix-Montañes, A. Ex vivo permeation of carprofen vehiculated by PLGA nanoparticles through porcine mucous membranes and ophthalmic tissues. Nanomaterials 2020, 10, 355. [Google Scholar] [CrossRef] [Green Version]
- Ozturk, K.; Caban, S.; Kozlu, S.; Kadayifci, E.; Yerlikaya, F.; Capan, Y. The influence of technological parameters on the physicochemical properties of blank PLGA nanoparticles. Pharmazie 2010, 65, 665–669. [Google Scholar]
- Gómara, M.J.; Sánchez-Merino, V.; Paús, A.; Merino-Mansilla, A.; Gatell, J.M.; Yuste, E.; Haro, I. Definition of an 18-mer Synthetic Peptide Derived from the GB virus C E1 Protein as a New HIV-1 Entry Inhibitor. Biochim. Biophys. Acta Gen. Subj. 2016, 1860, 1139–1148. [Google Scholar] [CrossRef]
- Dongol, M.; El-Denglawey, A.; Abd El Sadek, M.S.; Yahia, I.S. Thermal annealing effect on the structural and the optical properties of Nano CdTe films. Optik (Stuttg) 2015, 126, 1352–1357. [Google Scholar] [CrossRef]
- Jäger, A.; Jäger, E.; Giacomelli, F.C.; Nallet, F.; Steinhart, M.; Putaux, J.L.; Konefał, R.; Spěváček, J.; Ulbrich, K.; Štěpánek, P. Structural changes on polymeric nanoparticles induced by hydrophobic drug entrapment. Colloids Surf. A Physicochem. Eng. Asp. 2018, 538, 238–249. [Google Scholar] [CrossRef]
- Dillen, K.; Vandervoort, J.; Van Den Mooter, G.; Verheyden, L.; Ludwig, A. Factorial design, physicochemical characterisation and activity of ciprofloxacin-PLGA nanoparticles. Int. J. Pharm. 2004, 275, 171–187. [Google Scholar] [CrossRef] [PubMed]
- Ramos, G.R.; Calpena, A.C.; Egea, M.A.; Espina, M.; García, M.L. Freeze drying optimization of polymeric nanoparticles for ocular flurbiprofen delivery: Effect of protectant agents and critical process parameters on long-term stability. Drug Dev. Ind. Pharm. 2017, 43, 637–651. [Google Scholar] [CrossRef] [PubMed]
- Fernández, J.A.; Santos, R.G.; Estévez, G.F. Cinética de liberación de cefalexiana desde un biomaterial compuesto por HAP-200/POVIAC/CaCO 3. An. Real Acad. Nac. Farm. 2009, 75, 345–363. [Google Scholar]
- Ahnfelt, E.; Sjögren, E.; Hansson, P.; Lennernäs, H. In Vitro Release Mechanisms of Doxorubicin From a Clinical Bead Drug-Delivery System. J. Pharm. Sci. 2016, 105, 3387–3398. [Google Scholar] [CrossRef] [Green Version]
- Wang, Q.; Shen, M.; Li, W.; Li, W.; Zhang, F. Controlled-release of fluazinam from biodegradable PLGA-based microspheres. J. Environ. Sci. Heal. Part B Pestic. Food Contam. Agric. Wastes 2019, 54, 810–816. [Google Scholar] [CrossRef]
- Vega, E.; Egea, M.A.; Garduño-Ramírez, M.L.; García, M.L.; Sánchez, E.; Espina, M.; Calpena, A.C. Flurbiprofen PLGA-PEG nanospheres: Role of hydroxy-β-cyclodextrin on ex vivo human skin permeation and in vivo topical anti-inflammatory efficacy. Colloids Surf. B Biointerfaces 2013, 110, 339–346. [Google Scholar] [CrossRef]
- Marsh, D. Lateral pressure in membranes. Biochim. Biophys. Acta Rev. Biomembr. 1996, 1286, 183–223. [Google Scholar] [CrossRef]
- Tsumoto, K.; Matsuo, H.; Tomita, M.; Yoshimura, T. Efficient formation of giant liposomes through the gentle hydration of phosphatidylcholine films doped with sugar. Colloids Surf. B Biointerfaces 2009, 68, 98–105. [Google Scholar] [CrossRef]
- Wnętrzak, A.; Makyła-Juzak, K.; Chachaj-Brekiesz, A.; Lipiec, E.; Romeu, N.V.; Dynarowicz-Latka, P. Cyclosporin A distribution in cholesterol-sphingomyelin artificial membranes modeled as Langmuir monolayers. Colloids Surf. B Biointerfaces 2018, 166, 286–294. [Google Scholar] [CrossRef] [PubMed]
- Przykaza, K.; Woźniak, K.; Jurak, M.; Wiącek, A.E.; Mroczka, R. Properties of the Langmuir and Langmuir–Blodgett monolayers of cholesterol-cyclosporine A on water and polymer support. Adsorption 2019, 25, 923–936. [Google Scholar] [CrossRef] [Green Version]
- Broniatowski, M.; Flasiński, M.; Ziȩba, K.; Miśkowiec, P. Langmuir monolayer studies of the interaction of monoamphiphilic pentacyclic triterpenes with anionic mitochondrial and bacterial membrane phospholipids - Searching for the most active terpene. Biochim. Biophys. Acta Biomembr. 2014, 1838, 2460–2472. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gross, E.; Bedlack, R.S.; Loew, L.M. Dual-wavelength ratiometric fluorescence measurement of the membrane dipole potential. Biophys. J. 1994, 67, 208–216. [Google Scholar] [CrossRef] [Green Version]
- Cladera, J.; O’Shea, J.; Hadgraft, C.V. Influence of molecular dipoles on human skin permeability: Use of 6-ketocholestanol to enhance the transdermal delivery of bacitracin. J. Pharm. Sci. 2013, 92, 1018–1027. [Google Scholar] [CrossRef]
- Alakoskela, J.M.I.; Söderlund, T.; Holopainen, J.M.; Kinnunen, P.K.J. Dipole potential and head-group spacing are determinants for the membrane partitioning of pregnanolone. Mol. Pharmacol. 2004, 66, 161–168. [Google Scholar] [CrossRef] [Green Version]
- Araújo, J.; Gonzalez, E.; Egea, M.A.; Garcia, M.L.; Souto, E.B. Nanomedicines for ocular NSAIDs: Safety on drug delivery. Nanomedicine 2009, 5, 394–401. [Google Scholar] [CrossRef]
- Xu, Q.; Ensign, L.M.; Boylan, N.J.; Schön, A.; Gong, X.; Yang, J.C.; Lamb, N.W.; Cai, S.; Yu, T.; Freire, E.; et al. Impact of surface polyethylene glycol (PEG) density on biodegradable nanoparticle transport in mucus ex vivo and distribution in vivo. ACS Nano. 2015, 9, 9217–9227. [Google Scholar] [CrossRef] [Green Version]
- Leonardi, A.; Bucolo, C.; Romano, G.L.; Platania, C.B.; Drago, F.; Puglisi, G.; Pignatello, R. Influence of different surfactants on the technological properties and in vivo ocular tolerability of lipid nanoparticles. Int. J. Pharm. 2014, 470, 133–140. [Google Scholar] [CrossRef]
- Pignatello, R.; Bucolo, C.; Ferrara, P.; Maltese, A.; Puleo, A.; Puglisi, G. Eudragit RS100 nanosuspensions for the ophthalmic controlled delivery of ibuprofen. Eur. J. Pharm. Sci. 2002, 16, 53–61. [Google Scholar] [CrossRef]
- Liu, Z.; Zhang, X.; Wu, H.; Li, J.; Shu, L.; Liu, R.; Li, L.; Li, N. Preparation and evaluation of solid lipid nanoparticles of baicalin for ocular drug delivery system in vitro and in vivo. Drug Dev. Ind. Pharm. 2011, 37, 475–481. [Google Scholar] [CrossRef] [PubMed]
- Giannavola, C.; Bucolo, C.; Maltese, A.; Paolino, D.; Vandelli, M.A.; Puglisi, G.; Lee, V.H.; Fresta, M. Influence of preparation conditions on acyclovir-loaded poly-D,L-lactic acid nanospheres and effect of PEG coating on ocular drug bioavailability. Pharm. Res. 2003, 20, 584–590. [Google Scholar] [CrossRef] [PubMed]
- Lynch, C.; Kondiah, P.P.D.; Choonara, Y.E.; du Toit, L.C.; Ally, N.; Pillay, V. Advances in biodegradable nano-sized polymer-based ocular drug delivery. Polymers 2019, 11, 1371. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vega, E.; Egea, M.A.; Valls, O.; Espina, M.; Garcia, M.L. Flurbiprofen loaded biodegradable nanoparticles for ophthalmic administration. J. Pharm. Sci. 2006, 95, 2393–2405. [Google Scholar] [CrossRef] [PubMed]











| Formulation Number | Polymer Used | Surfactant | Average Size (nm) | Polydispersity Index (PI) | Zeta Potential (ZP, mV) | EE (%) |
|---|---|---|---|---|---|---|
| 1 | PLGA 503 H | PVA | 234.1 ± 0.5 | 0.081 ± 0.009 | −12.2 ± 1.3 | 93.4 |
| 2 | Tween80® | 146.0 ± 0.6 | 0.054 ± 0.008 | −25.2 ± 0.6 | 87.5 | |
| 3 | Lutrol | 159.5 ± 0.8 | 0.058 ± 0.021 | −26.0 ± 0.1 | 85.1 | |
| 4 | PLGA-5% | PVA | 167.1 ± 1.1 | 0.080 ± 0.012 | −11.8 ± 0.9 | 95.0 |
| 5 | Tween80® | 138.4 ± 1.3 | 0.072 ± 0.015 | −14.1 ± 1.1 | 91.5 | |
| 6 | Lutrol | 154.2 ± 1.9 | 0.063 ± 0.015 | −18.7 ± 1.4 | 93.8 | |
| 7 | PLGA 10% | PVA | 140.9 ± 1.0 | 0.055 ± 0.023 | −16.7 ± 0.7 | 99.0 |
| 8 | Tween80® | 119.2 ± 1.0 | 0.074 ± 0.008 | −21.2 ± 0.6 | 99.2 | |
| 9 | Lutrol | 120.7 ± 0.8 | 0.071 ± 0.008 | −23.1 ± 1.8 | 91.5 | |
| 10 | PLGA 15% | PVA | 156.4 ± 0.8 | 0.078 ± 0.008 | −16.2 ± 0.7 | 92.2 |
| 11 | Tween80® | 143.0 ± 0.5 | 0.062 ± 0.006 | −21.4 ± 0.8 | 93.4 | |
| 12 | Lutrol | 155.2 ± 1.1 | 0.076 ± 0.012 | −22.5 ± 0.5 | 94.0 |
| Formulation Number | Polymer Used | Surfactant | Average Size Ratio | Polydispersity Index Ratio | Zeta Potential Ratio | EE Ratio |
|---|---|---|---|---|---|---|
| 1 | PLGA 503 H | PVA | 1.00 | 0.61 | 0.97 | 1.00 |
| 2 | Tween80® | 1.01 | 1.23 | 0.97 | 1.01 | |
| 3 | Lutrol | 1.00 | 1.00 | 1.00 | 1.02 | |
| 4 | PLGA-5% | PVA | 1.01 | 1.03 | 1.14 | 0.98 |
| 5 | Tween80® | 1.00 | 0.92 | 1.05 | 1.01 | |
| 6 | Lutrol | 1.01 | 1.07 | 0.97 | 0.95 | |
| 7 | PLGA 10% | PVA | 0.98 | 1.00 | 1.03 | 0.98 |
| 8 | Tween80® | 0.99 | 0.94 | 1.01 | 0.98 | |
| 9 | Lutrol | 0.99 | 1.21 | 0.99 | 0.99 | |
| 10 | PLGA 15% | PVA | 0.99 | 1.28 | 1.02 | 1.04 |
| 11 | Tween80® | 1.02 | 1.06 | 1.03 | 1.01 | |
| 12 | Lutrol | 1.00 | 1.01 | 0.94 | 1.02 |
| Formulation Number | Polymer Used | Surfactant | Bmax (%) | Kd (min) |
|---|---|---|---|---|
| 1 | PLGA 503 H | PVA | 50.6 ± 2.3 | 210.6 ± 24.3 |
| 2 | Tween80® | 46.9 ± 1.6 | 89.6 ± 10.1 | |
| 3 | Lutrol | 48.7 ± 1.4 | 79.7 ± 7.9 | |
| 4 | PLGA-5% | PVA | 33.5 ± 2.8 | 149.2 ± 35.2 |
| 5 | Tween80® | 40.4 ± 1.1 | 84.5 ± 7.6 | |
| 6 | Lutrol | 41.6 ± 0.5 | 79.9 ± 3.4 | |
| 7 | PLGA 10% | PVA | 38.5 ± 0.5 | 78.1 ± 3.9 |
| 8 | Tween80® | 43.0 ± 1.8 | 72.1 ± 10.9 | |
| 9 | Lutrol | 45.1 ± 1.4 | 77.1 ± 8.5 | |
| 10 | PLGA 15% | PVA | 41.4 ± 1.1 | 59.8 ± 6.0 |
| 11 | Tween80® | 44.6 ± 1.0 | 79.4 ± 6.3 | |
| 12 | Lutrol | 58.3 ± 1.5 | 113.6 ± 9.2 |
| Monolayer Composition | A/cm2 at 32 mN·m−1 | /mN·m−1 at 32 mN m−1 | πc/mN·m−1 | /mN·m−1 |
|---|---|---|---|---|
| ACMM | 169.47 | 44.87 | 47.07 | 76.57 |
| ACMM + PLGA-DXI-PVA-NPs | 185.50 | 29.35 | 51.00 | 84.83 |
| ACMM + PLGA-DXI-PEG 5%-PVA-NPs | 194.17 | 39.89 | 47.72 | 76.77 |
| ACMM + PLGA-DXI-PEG 10%-PVA-NPs | 184.36 | 50.19 | 47.14 | 93.17 |
| ACMM + PLGA-DXI-PEG 15%-PVA-NPs | 197.36 | 60.17 | 45.45 | 96.46 |
| ACMM + PLGA-DXI-TWEEN-NPs | 234.10 | 28.16 | 46.98 | 45.88 |
| ACMM + PLGA-DXI-PEG 5%-Tween-NPs | 238.04 | 21.58 | 47.55 | 52.07 |
| ACMM + PLGA-DXI-PEG 10%- Tween -NPs | 223.49 | 23.52 | 48.02 | 66.36 |
| ACMM + PLGA-DXI-PEG 15%- Tween -NPs | 247.55 | 29.16 | 46.24 | 39.12 |
| ACMM + PLGA-DXI-Lutrol-NPs | 178.19 | 52.24 | 46.00 | 63.94 |
| ACMM + PLGA-DXI-PEG 5%- Lutrol -NPs | 186.69 | 47.55 | 47.30 | 96.83 |
| ACMM + PLGA-DXI-PEG 10%- Lutrol-NPs | 178.75 | 48.04 | 47.70 | 94.78 |
| ACMM + PLGA-DXI-PEG 15%- Lutrol -NPs | 180.36 | 40.82 | 46.56 | 63.94 |
| DXI NPs | Bmax | Kd | R2 |
|---|---|---|---|
| PLGA-PVA | 0.55 ± 0.01 | 39.95 ± 3.58 | 0.996 |
| PEG 5%-PVA | 0.68 ± 0.01 | 10.93 ± 1.07 | 0.998 |
| PEG 10%-PVA | 0.72 ± 0.02 | 46.98 ± 3.85 | 0.997 |
| PEG 15%-PVA | 0.65 ± 0.02 | 18.97 ± 2.03 | 0.993 |
| PLGA-Tween | 0.59 ± 0.00 | 27.52 ± 7.37 | 0.960 |
| PEG 5%-Tween | 0.70 ± 0.01 | 5.48 ± 0.62 | 0.999 |
| PEG 10%-Tween | 0.59 ± 0.02 | 16.17 ± 2.69 | 0.984 |
| PEG 15%-Tween | 0.62 ± 0.02 | 8.86 ± 1.95 | 0.976 |
| PLGA-Lutrol | 0.71 ± 0.03 | 57.49 ± 7.08 | 0.993 |
| PEG 5%-Lutrol | 0.66 ± 0.00 | 17.82 ± 0.35 | 0.999 |
| PEG 10%-Lutrol | 0.65 ± 0.03 | 53.43 ± 7.17 | 0.993 |
| PEG 15%-Lutrol | 0.61 ± 0.05 | 10.9 6 ± 0.39 | 0.993 |
| Corneal Permeation | |||
| Formulation | Best Fit | Pharmacokinetic Parameters | |
| PLGA Lutrol | Korsmeyer-Peppas | K: 0.814 ± 0.075 | n: 0.33 ± 0.02 |
| PLGA 5% Lutrol | Korsmeyer-Peppas | K: 1.45 ± 0.34 | n: 0.40 ± 0.04 |
| PLGA 10% Tween | Hyperbola | Kd: 38.01 ± 3.64 min | B max: 19.8% ± 0.4904% |
| PLGA 15% Lutrol | Hyperbola | Kd: 46.02 ± 4.15 min | B max 27.98% ± 0.7002% |
| Scleral Permeation | |||
| Formulation | Best Fit | Pharmacokinetic Parameters | |
| PLGA Lutrol | Korsmeyer-Peppas | K: 7.29 ± 0.58 | N: 0.14 ± 0.16 |
| PLGA 5% Lutrol | Hyperbola | Kd: 90.92 ± 8.80 min | Bmax: 24.64% ± 0.85% |
| PLGA 10% Tween | Hyperbola | Kd: 24.26 ± 3.90 min | Bmax: 21.57% ± 0.75% |
| PLGA 15% Lutrol | Hyperbola | Kd: 19.23 ± 2.59 min | Bmax: 23.05% ± 0.61% |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sánchez-López, E.; Esteruelas, G.; Ortiz, A.; Espina, M.; Prat, J.; Muñoz, M.; Cano, A.; Calpena, A.C.; Ettcheto, M.; Camins, A.; et al. Dexibuprofen Biodegradable Nanoparticles: One Step Closer towards a Better Ocular Interaction Study. Nanomaterials 2020, 10, 720. https://doi.org/10.3390/nano10040720
Sánchez-López E, Esteruelas G, Ortiz A, Espina M, Prat J, Muñoz M, Cano A, Calpena AC, Ettcheto M, Camins A, et al. Dexibuprofen Biodegradable Nanoparticles: One Step Closer towards a Better Ocular Interaction Study. Nanomaterials. 2020; 10(4):720. https://doi.org/10.3390/nano10040720
Chicago/Turabian StyleSánchez-López, Elena, Gerard Esteruelas, Alba Ortiz, Marta Espina, Josefina Prat, Montserrat Muñoz, Amanda Cano, Ana Cristina Calpena, Miren Ettcheto, Antoni Camins, and et al. 2020. "Dexibuprofen Biodegradable Nanoparticles: One Step Closer towards a Better Ocular Interaction Study" Nanomaterials 10, no. 4: 720. https://doi.org/10.3390/nano10040720
APA StyleSánchez-López, E., Esteruelas, G., Ortiz, A., Espina, M., Prat, J., Muñoz, M., Cano, A., Calpena, A. C., Ettcheto, M., Camins, A., Alsafi, Z., Souto, E. B., García, M. L., & Pujol, M. (2020). Dexibuprofen Biodegradable Nanoparticles: One Step Closer towards a Better Ocular Interaction Study. Nanomaterials, 10(4), 720. https://doi.org/10.3390/nano10040720