Critical Review of Lipid-Based Nanoparticles as Carriers of Neuroprotective Drugs and Extracts
Abstract
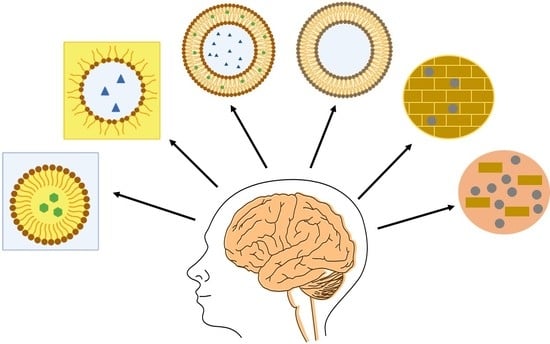
:1. Introduction
2. Gastrointestinal Absorption of Nanoparticles
3. Blood-Brain Barrier
4. Delivery Routes for Neuroprotective Drugs
4.1. Intracerebroventricular Delivery Route of Lipid-Based Nanoparticles
4.2. Intravenous and Intramuscular Administration of Lipid-Based Nanoparticles
4.3. Intranasal Delivery of Lipid-Based Nanoparticles
5. Lipid-Based Nanoencapsulation Techniques
5.1. Encapsulation by Nanoemulsions

5.1.1. Oil
5.1.2. Surfactant
5.1.3. Cosurfactant
5.2. Encapsulation by Nanoliposomes/Nanophytosomes
- Unilamellar vesicles (ULV), which contain one single lipidic bilayer and can be a small unilamellar vesicle (SUV, when less than 100 nm) or a large unilamellar vesicle (LUV);
- Multilamellar vesicles, composed of multiple concentric bilayers;
- Multivesicular vesicles (MVV), which are composed of many small nonconcentric vesicles encapsulated within a single lipid bilayer;
- Double bilayer vesicle (DBV), consisting of two bilayer membranes.
5.2.1. Phospholipids
5.2.2. Active Compound
5.2.3. Solvents
5.2.4. Stoichiometric Ratio of Active Compound to Phospholipid
5.2.5. Other Factors Affecting Phytosome Production
5.3. Encapsulation by Nanostructured Lipid Carriers
5.3.1. Lipids
5.3.2. Surfactants
6. Comparison of Lipid-Based Nanoparticles with Other Types of Nanoparticles for Brain-Delivery
7. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Feigin, V.L.; Vos, T.; Nichols, E.; Owolabi, M.O.; Carroll, W.M.; Dichgans, M.; Deuschl, G.; Parmar, P.; Brainin, M.; Murray, C. The global burden of neurological disorders: Translating evidence into policy. Lancet Neurol. 2020, 19, 255–265. [Google Scholar] [CrossRef]
- Copeland, C.; Stabenfeldt, S.E. Leveraging the dynamic blood–brain barrier for central nervous system nanoparticle-based drug delivery applications. Curr. Opin. Biomed. Eng. 2020, 14, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Assadpour, E.; Jafari, S.M. Chapter One—An overview of lipid-based nanostructures for encapsulation of food ingredients. In Lipid-Based Nanostructures for Food Encapsulation Purposes; Jafari, S.M., Ed.; Academic Press: Cambridge, MA, USA, 2019; pp. 1–34. ISBN 978-0-12-815673-5. [Google Scholar]
- Jafari, S.M. Nanoencapsulation Technologies for the Food and Nutraceutical Industries; Jafari, S.M., Ed.; Academic Press: London, UK, 2016; ISBN 978-0-12-809436-5. [Google Scholar]
- Quintanilla-Carvajal, M.X.; Camacho-Díaz, B.H.; Meraz-Torres, L.S.; Chanona-Pérez, J.J.; Alamilla-Beltrán, L.; Jimenéz-Aparicio, A.; Gutiérrez-López, G.F. Nanoencapsulation: A new trend in food engineering processing. Food Eng. Rev. 2010, 2, 39–50. [Google Scholar] [CrossRef]
- Uskokovic, V. Nanomaterials and Nanotechnologies: Approaching the Crest of this Big Wave. Curr. Nanosci. 2008, 4, 119–129. [Google Scholar] [CrossRef] [Green Version]
- Li, Z.; Jiang, H.; Xu, C.; Gu, L. A review: Using nanoparticles to enhance absorption and bioavailability of phenolic phytochemicals. Food Hydrocoll. 2015, 43, 153–164. [Google Scholar] [CrossRef]
- Ghorbanzade, T.; Jafari, S.M.; Akhavan, S.; Hadavi, R. Nano-encapsulation of fish oil in nano-liposomes and its application in fortification of yogurt. Food Chem. 2017, 216, 146–152. [Google Scholar] [CrossRef] [PubMed]
- Bayraktar, O.; Erdoğan, İ.; Köse, M.D.; Kalmaz, G. Chapter 17—Nanocarriers for Plant-Derived Natural Compounds. In Nanostructures for Antimicrobial Therapy; Ficai, A., Grumezescu, A.M., Eds.; Elsevier: Amsterdam, The Netherlands, 2017; pp. 395–412. ISBN 978-0-323-46152-8. [Google Scholar]
- Rezaei, A.; Fathi, M.; Jafari, S.M. Nanoencapsulation of hydrophobic and low-soluble food bioactive compounds within different nanocarriers. Food Hydrocoll. 2019, 88, 146–162. [Google Scholar] [CrossRef]
- Rostamabadi, H.; Falsafi, S.R.; Jafari, S.M. Nanoencapsulation of carotenoids within lipid-based nanocarriers. J. Control. Release 2019, 298, 38–67. [Google Scholar] [CrossRef] [PubMed]
- Akhavan, S.; Assadpour, E.; Katouzian, I.; Jafari, S.M. Lipid nano scale cargos for the protection and delivery of food bioactive ingredients and nutraceuticals. Trends Food Sci. Technol. 2018, 74, 132–146. [Google Scholar] [CrossRef]
- Katouzian, I.; Faridi Esfanjani, A.; Jafari, S.M.; Akhavan, S. Formulation and application of a new generation of lipid nano-carriers for the food bioactive ingredients. Trends Food Sci. Technol. 2017, 68, 14–25. [Google Scholar] [CrossRef]
- Kalepu, S.; Manthina, M.; Padavala, V. Oral lipid-based drug delivery systems—An overview. Acta Pharm. Sin. B 2013, 3, 361–372. [Google Scholar] [CrossRef] [Green Version]
- Thummel, K.E.; Kunze, K.L.; Shen, D.D. Enzyme-catalyzed processes of first-pass hepatic and intestinal drug extraction. Adv. Drug Deliv. Rev. 1997, 27, 99–127. [Google Scholar] [CrossRef]
- Liu, W.; Hou, Y.; Jin, Y.; Wang, Y.; Xu, X.; Han, J. Research progress on liposomes: Application in food, digestion behavior and absorption mechanism. Trends Food Sci. Technol. 2020, 104, 177–189. [Google Scholar] [CrossRef]
- Salentinig, S. Supramolecular structures in lipid digestion and implications for functional food delivery. Curr. Opin. Colloid Interface Sci. 2019, 39, 190–201. [Google Scholar] [CrossRef] [Green Version]
- Chakraborty, S.; Shukla, D.; Mishra, B.; Singh, S. Lipid—An emerging platform for oral delivery of drugs with poor bioavailability. Eur. J. Pharm. Biopharm. 2009, 73, 1–15. [Google Scholar] [CrossRef]
- Iwanaga, K.; Ono, S.; Narioka, K.; Kakemi, M.; Morimoto, K.; Yamashita, S.; Namba, Y.; Naoto, O. Application of surface-coated liposomes for oral delivery of peptide: Effects of coating the liposome’s surface on the GI transit of insulin. J. Pharm. Sci. 1999, 88, 248–252. [Google Scholar] [CrossRef] [PubMed]
- Liu, W.; Ye, A.; Liu, C.; Liu, W.; Singh, H. Structure and integrity of liposomes prepared from milk- or soybean-derived phospholipids during in vitro digestion. Food Res. Int. 2012, 48, 499–506. [Google Scholar] [CrossRef]
- Liu, W.; Liu, J.; Li, T.; Liu, C.; Liu, W. Improved physical and in vitro digestion stability of a polyelectrolyte delivery system based on layer-by-layer self-assembly alginate-chitosan-coated nanoliposomes. J. Agric. Food Chem. 2013, 61, 4133–4144. [Google Scholar] [CrossRef]
- Ding, S.; Khan, A.I.; Cai, X.; Song, Y.; Lyu, Z.; Du, D.; Dutta, P.; Lin, Y. Overcoming blood–brain barrier transport: Advances in nanoparticle-based drug delivery strategies. Mater. Today 2020, 37, 112–125. [Google Scholar] [CrossRef] [PubMed]
- Bhowmik, A.; Khan, R.; Ghosh, M.K. Blood brain barrier: A challenge for effectual therapy of brain tumors. BioMed Res. Int. 2015, 2015. [Google Scholar] [CrossRef] [Green Version]
- Sánchez-Navarro, M.; Giralt, E.; Teixidó, M. Blood–brain barrier peptide shuttles. Curr. Opin. Chem. Biol. 2017, 38, 134–140. [Google Scholar] [CrossRef]
- Pinheiro, R.G.R.; Granja, A.; Loureiro, J.A.; Pereira, M.C.; Pinheiro, M.; Neves, A.R.; Reis, S. Quercetin lipid nanoparticles functionalized with transferrin for Alzheimer’s disease. Eur. J. Pharm. Sci. 2020, 148, 105314. [Google Scholar] [CrossRef] [PubMed]
- Pandit, R.; Chen, L.; Götz, J. The blood-brain barrier: Physiology and strategies for drug delivery. Adv. Drug Deliv. Rev. 2019. [Google Scholar] [CrossRef] [PubMed]
- Harilal, S.; Jose, J.; Parambi, D.G.T.; Kumar, R.; Unnikrishnan, M.K.; Uddin, M.S.; Mathew, G.E.; Pratap, R.; Marathakam, A.; Mathew, B. Revisiting the blood-brain barrier: A hard nut to crack in the transportation of drug molecules. Brain Res. Bull. 2020, 160, 121–140. [Google Scholar] [CrossRef]
- Chen, Y.; Liu, L. Modern methods for delivery of drugs across the blood-brain barrier. Adv. Drug Deliv. Rev. 2012, 64, 640–665. [Google Scholar] [CrossRef]
- Almutairi, M.M.A.; Gong, C.; Xu, Y.G.; Chang, Y.; Shi, H. Factors controlling permeability of the blood-brain barrier. Cell. Mol. Life Sci. 2016, 73, 57–77. [Google Scholar] [CrossRef]
- Sweeney, M.; Sagare, A.; Zlokovic, B. Blood–brain barrier breakdown in Alzheimer disease and other neurodegenerative disorders. Nat. Rev. Neurol. 2018, 14, 133–150. [Google Scholar] [CrossRef]
- Fresta, M.; Puglisi, G.; Di Giacomo, C.; Russo, A. Liposomes as in-vivo carriers for citicoline: Effects on rat cerebral post-ischaemic reperfusion. J. Pharm. Pharmacol. 1994, 46, 974–981. [Google Scholar] [CrossRef]
- Phachonpai, W.; Wattanathorn, J.; Muchimapura, S.; Tong-Un, T.; Preechagoon, D. Neuroprotective effect of quercetin encapsulated liposomes: A novel therapeutic strategy against Alzheimer’s disease. Am. J. Appl. Sci. 2010, 7, 480–485. [Google Scholar] [CrossRef] [Green Version]
- Mori, N.; Kurokouchi, A.; Osonoe, K.; Saitoh, H.; Ariga, K.; Suzuki, K.; Iwata, Y. Liposome-entrapped phenytoin locally suppresses amygdaloid epileptogenic focus created by db-cAMP/EDTA in rats. Brain Res. 1995, 703, 184–190. [Google Scholar] [CrossRef]
- Purkayastha, J.; Ghosh, J. Phytosomes: The novel drug delivery system for phytomedicine. New Age Herbals Resour. Qual. Pharmacogn. 2018, 455–464. [Google Scholar] [CrossRef]
- Emami, J.; Yousefian, H.; Sadeghi, H. Targeted nanostructured lipid carrier for brain delivery of artemisinin: Design, preparation, characterization, optimization and cell toxicity. J. Pharm. Pharm. Sci. 2018, 21, 225s–241s. [Google Scholar] [CrossRef] [PubMed]
- Wong, H.L.; Bendayan, R.; Rauth, A.M.; Li, Y.; Wu, X.Y. Chemotherapy with anticancer drugs encapsulated in solid lipid nanoparticles. Adv. Drug Deliv. Rev. 2007, 59, 491–504. [Google Scholar] [CrossRef] [PubMed]
- Hu, Y.; Gaillard, P.J.; de Lange, E.C.M.; Hammarlund-Udenaes, M. Targeted brain delivery of methotrexate by glutathione PEGylated liposomes: How can the formulation make a difference? Eur. J. Pharm. Biopharm. 2019, 139, 197–204. [Google Scholar] [CrossRef] [Green Version]
- Chen, Z.L.; Huang, M.; Wang, X.R.; Fu, J.; Han, M.; Shen, Y.Q.; Xia, Z.; Gao, J.Q. Transferrin-modified liposome promotes α-mangostin to penetrate the blood-brain barrier. Nanomed. Nanotechnol. Biol. Med. 2016, 12, 421–430. [Google Scholar] [CrossRef]
- Anderson, G.D.; Saneto, R.P. Current oral and non-oral routes of antiepileptic drug delivery. Adv. Drug Deliv. Rev. 2012, 64, 911–918. [Google Scholar] [CrossRef] [PubMed]
- Fisher, R.S.; Ho, J. Potential New Methods for Antiepileptic Drug Delivery. CNS Drugs 2002, 16, 579–593. [Google Scholar] [CrossRef]
- Glascock, J.J.; Osman, E.Y.; Coady, T.H.; Rose, F.F.; Shababi, M.; Lorson, C.L. Delivery of therapeutic agents through intracerebroventricular (ICV) and intravenous (IV) injection in mice. J. Vis. Exp. 2011, 56, e2968. [Google Scholar] [CrossRef]
- Bourganis, V.; Kammona, O.; Alexopoulos, A.; Kiparissides, C. Recent advances in carrier mediated nose-to-brain delivery of pharmaceutics. Eur. J. Pharm. Biopharm. 2018, 128, 337–362. [Google Scholar] [CrossRef]
- Rungta, R.L.; Choi, H.B.; Lin, P.J.; Ko, R.W.; Ashby, D.; Nair, J.; Manoharan, M.; Cullis, P.R.; MacVicar, B.A. Lipid nanoparticle delivery of siRNA to silence neuronal gene expression in the brain. Mol. Ther. Nucleic Acids 2013. [Google Scholar] [CrossRef]
- Ma, F.; Yang, L.; Sun, Z.; Chen, J.; Rui, X.; Glass, Z.; Xu, Q. Neurotransmitter-derived lipidoids (NT-lipidoids) for enhanced brain delivery through intravenous injection. Sci. Adv. 2020, 6, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Graverini, G.; Piazzini, V.; Landucci, E.; Pantano, D.; Nardiello, P.; Casamenti, F.; Pellegrini-Giampietro, D.E.; Bilia, A.R.; Bergonzi, M.C. Solid lipid nanoparticles for delivery of andrographolide across the blood-brain barrier: In vitro and in vivo evaluation. Coll. Surf. B Biointerfaces 2018, 161, 302–313. [Google Scholar] [CrossRef]
- Kakkar, V.; Mishra, A.K.; Chuttani, K.; Kaur, I.P. Proof of concept studies to confirm the delivery of curcumin loaded solid lipid nanoparticles (C-SLNs) to brain. Int. J. Pharm. 2013, 448, 354–359. [Google Scholar] [CrossRef] [PubMed]
- Koshkina, N.V.; Gilbert, B.E.; Waldrep, J.C.; Seryshev, A.; Knight, V. Distribution of camptothecin after delivery as a liposome aerosol or following intramuscular injection in mice. Cancer Chemother. Pharmacol. 1999, 44, 187–192. [Google Scholar] [CrossRef]
- Ahmed, A.E.; Jacob, S.; Giovanella, B.C.; Kozielski, A.J.; Stehlin, J.S.J.; Liehr, J.G. Influence of route of administration on [3 H]-camptothecin distribution and tumor uptake in CASE-bearing nude mice: Whole-body autoradiographic studies. Cancer Chemother. Pharmacol. 1996, 39, 122–130. [Google Scholar] [CrossRef]
- Wang, L.; Zhao, X.; Du, J.; Liu, M.; Feng, J.; Hu, K. Improved brain delivery of pueraria flavones via intranasal administration of borneol-modified solid lipid nanoparticles. Nanomedicine 2019, 14, 2105–2119. [Google Scholar] [CrossRef] [PubMed]
- Montes, C.; Villaseñor, M.J.; Ríos, Á. Analytical control of nanodelivery lipid-based systems for encapsulation of nutraceuticals: Achievements and challenges. Trends Food Sci. Technol. 2019, 90, 47–62. [Google Scholar] [CrossRef]
- Benita, S.; Levy, M.Y. Submicron emulsions as colloidal drug carriers for intravenous administration: Comprehensive physicochemical characterization. J. Pharm. Sci. 1993, 82, 1069–1079. [Google Scholar] [CrossRef] [PubMed]
- Mahdi Jafari, S.; He, Y.; Bhandari, B. Nano-emulsion production by sonication and microfluidization—A comparison. Int. J. Food Prop. 2006, 9, 475–485. [Google Scholar] [CrossRef]
- McClements, D.J. Edible nanoemulsions: Fabrication, properties, and functional performance. Soft Matter 2011, 7, 2297–2316. [Google Scholar] [CrossRef] [Green Version]
- Tadros, T.; Izquierdo, P.; Esquena, J.; Solans, C. Formation and stability of nano-emulsions. Adv. Colloid Interface Sci. 2004, 108–109, 303–318. [Google Scholar] [CrossRef] [PubMed]
- Sivakumar, M.; Tang, S.Y.; Tan, K.W. Cavitation technology—A greener processing technique for the generation of pharmaceutical nanoemulsions. Ultrason. Sonochem. 2014, 21, 2069–2083. [Google Scholar] [CrossRef]
- Nirale, P.; Paul, A.; Yadav, K.S. Nanoemulsions for targeting the neurodegenerative diseases: Alzheimer’s, Parkinson’s and Prion’s. Life Sci. 2020, 245, 117394. [Google Scholar] [CrossRef] [PubMed]
- Walker, R.; Decker, E.A.; McClements, D.J. Development of food-grade nanoemulsions and emulsions for delivery of omega-3 fatty acids: Opportunities and obstacles in the food industry. Food Funct. 2015, 6, 42–55. [Google Scholar] [CrossRef] [Green Version]
- Franco, M.K.K.D.; de Araújo, D.R.; de Paula, E.; Cavalcanti, L.; Yokaichiya, F. X-ray Scattering Techniques Applied in the Development of Drug Delivery Systems. In X-ray Scattering; Intech: Rijeka, Croatia, 2017. [Google Scholar] [CrossRef] [Green Version]
- Qadir, A.; Faiyazuddin, M.D.; Talib Hussain, M.D.; Alshammari, T.M.; Shakeel, F. Critical steps and energetics involved in a successful development of a stable nanoemulsion. J. Mol. Liq. 2016, 214, 7–18. [Google Scholar] [CrossRef]
- Teo, A.; Lee, S.J.; Goh, K.K.T.; Wolber, F.M. Kinetic stability and cellular uptake of lutein in WPI-stabilised nanoemulsions and emulsions prepared by emulsification and solvent evaporation method. Food Chem. 2017, 221, 1269–1276. [Google Scholar] [CrossRef] [PubMed]
- Vishwanathan, R.; Wilson, T.A.; Nicolosi, R.J. Bioavailability of a nanoemulsion of lutein is greater than a lutein supplement. Nano Biomed. Eng. 2009, 1, 38–49. [Google Scholar] [CrossRef] [Green Version]
- Harwansh, R.K.; Deshmukh, R.; Rahman, M.A. Nanoemulsion: Promising nanocarrier system for delivery of herbal bioactives. J. Drug Deliv. Sci. Technol. 2019, 51, 224–233. [Google Scholar] [CrossRef]
- Arora, A.; Kumar, S.; Ali, J.; Baboota, S. Intranasal Delivery of Tetrabenazine Nanoemulsion via Olfactory Region for Better Treatment of Hyperkinetic Movement Associated with Huntington’s Disease: Pharmacokinetic and Brain Delivery Study; Elsevier: Dublin, Ireland, 2020; Volume 230, ISBN 9818529286. [Google Scholar]
- Dordević, S.M.; Cekić, N.D.; Savić, M.M.; Isailović, T.M.; Randelović, D.V.; Marković, B.D.; Savić, S.R.; Stamenić, T.T.; Daniels, R.; Savić, S.D. Parenteral nanoemulsions as promising carriers for brain delivery of risperidone: Design, characterization and in vivo pharmacokinetic evaluation. Int. J. Pharm. 2015, 493, 40–54. [Google Scholar] [CrossRef] [Green Version]
- Singh, Y.; Meher, J.G.; Raval, K.; Khan, F.A.; Chaurasia, M.; Jain, N.K.; Chourasia, M.K. Nanoemulsion: Concepts, development and applications in drug delivery. J. Control. Release 2017, 252, 28–49. [Google Scholar] [CrossRef]
- Haider, M.F.; Khan, S.; Gaba, B.; Alam, T.; Baboota, S.; Ali, J.; Ali, A. Optimization of rivastigmine nanoemulsion for enhanced brain delivery: In-vivo and toxicity evaluation. J. Mol. Liq. 2018, 255, 384–396. [Google Scholar] [CrossRef]
- Shu, G.; Khalid, N.; Chen, Z.; Neves, M.A.; Barrow, C.J.; Nakajima, M. Formulation and characterization of astaxanthin-enriched nanoemulsions stabilized using ginseng saponins as natural emulsifiers. Food Chem. 2018, 255, 67–74. [Google Scholar] [CrossRef]
- Khalid, N.; Shu, G.; Holland, B.J.; Kobayashi, I.; Nakajima, M.; Barrow, C.J. Formulation and characterization of O/W nanoemulsions encapsulating high concentration of astaxanthin. Food Res. Int. 2017, 102, 364–371. [Google Scholar] [CrossRef]
- Weigel, F.; Weiss, J.; Decker, E.A.; McClements, D.J. Lutein-enriched emulsion-based delivery systems: Influence of emulsifiers and antioxidants on physical and chemical stability. Food Chem. 2018, 242, 395–403. [Google Scholar] [CrossRef]
- Frede, K.; Henze, A.; Khalil, M.; Baldermann, S.; Schweigert, F.J.; Rawel, H. Stability and cellular uptake of lutein-loaded emulsions. J. Funct. Foods 2014, 8, 118–127. [Google Scholar] [CrossRef]
- Shofia, S.I.; Jayakumar, K.; Mukherjee, A.; Chandrasekaran, N. Efficiency of brown seaweed (Sargassum longifolium) polysaccharides encapsulated in nanoemulsion and nanostructured lipid carrier against colon cancer cell lines HCT 116. RSC Adv. 2018, 8, 15973–15984. [Google Scholar] [CrossRef] [Green Version]
- Hussein, J.; El-Bana, M.; Refaat, E.; El-Naggar, M.E. Synthesis of carvacrol-based nanoemulsion for treating neurodegenerative disorders in experimental diabetes. J. Funct. Foods 2017, 37, 441–448. [Google Scholar] [CrossRef]
- Colombo, M.; Figueiró, F.; de Fraga Dias, A.; Teixeira, H.F.; Battastini, A.M.O.; Koester, L.S. Kaempferol-loaded mucoadhesive nanoemulsion for intranasal administration reduces glioma growth in vitro. Int. J. Pharm. 2018, 543, 214–223. [Google Scholar] [CrossRef]
- Zhao, C.; Wei, L.; Yin, B.; Liu, F.; Li, J.; Liu, X.; Wang, J.; Wang, Y. Encapsulation of lycopene within oil-in-water nanoemulsions using lactoferrin: Impact of carrier oils on physicochemical stability and bioaccessibility. Int. J. Biol. Macromol. 2020, 153, 912–920. [Google Scholar] [CrossRef]
- Md, S.; Gan, S.Y.; Haw, Y.H.; Ho, C.L.; Wong, S.; Choudhury, H. In vitro neuroprotective effects of naringenin nanoemulsion against $β$-amyloid toxicity through the regulation of amyloidogenesis and tau phosphorylation. Int. J. Biol. Macromol. 2018, 118, 1211–1219. [Google Scholar] [CrossRef] [PubMed]
- Sharma, S.; Rabbani, S.A.; Narang, J.K.; Hyder Pottoo, F.; Ali, J.; Kumar, S.; Baboota, S. Role of rutin nanoemulsion in ameliorating oxidative stress: Pharmacokinetic and pharmacodynamics studies. Chem. Phys. Lipids 2020, 228, 104890. [Google Scholar] [CrossRef]
- Yadav, S.; Gandham, S.K.; Panicucci, R.; Amiji, M.M. Intranasal Brain Delivery of Cationic Nanoemulsion-Encapsulated Tnfα Sirna in Prevention of Experimental Neuroin-Flammation; Elsevier: Amsterdam, The Netherlands, 2016; Volume 12, ISBN 6173733137. [Google Scholar]
- Ahmad, N.; Ahmad, R.; Alam, M.A.; Samim, M.; Iqbal, Z.; Ahmad, F.J. Quantification and evaluation of thymoquinone loaded mucoadhesive nanoemulsion for treatment of cerebral ischemia. Int. J. Biol. Macromol. 2016, 88, 320–332. [Google Scholar] [CrossRef] [PubMed]
- Kumbhar, S.A.; Kokare, C.R.; Shrivastava, B.; Gorain, B.; Choudhury, H. Preparation, characterization, and optimization of asenapine maleate mucoadhesive nanoemulsion using Box-Behnken design: In vitro and in vivo studies for brain targeting. Int. J. Pharm. 2020, 586, 119499. [Google Scholar] [CrossRef]
- Desai, J.; Thakkar, H. Enhanced oral bioavailability and brain uptake of Darunavir using lipid nanoemulsion formulation. Coll. Surf. B Biointerfaces 2019, 175, 143–149. [Google Scholar] [CrossRef]
- Mallick, A.; Gupta, A.; Hussain, A.; Aparajay, P.; Singh, S.; Singh, S.K.; Dev, A. Intranasal delivery of gabapentin loaded optimized nanoemulsion for augmented permeation. J. Drug Deliv. Sci. Technol. 2020, 56, 101606. [Google Scholar] [CrossRef]
- Prabhakar, K.; Afzal, S.M.; Surender, G.; Kishan, V. Tween 80 containing lipid nanoemulsions for delivery of indinavir to brain. Acta Pharm. Sin. B 2013, 3, 345–353. [Google Scholar] [CrossRef] [Green Version]
- Iqbal, R.; Ahmed, S.; Jain, G.K.; Vohora, D. Design and development of letrozole nanoemulsion: A comparative evaluation of brain targeted nanoemulsion with free letrozole against status epilepticus and neurodegeneration in mice. Int. J. Pharm. 2019, 565, 20–32. [Google Scholar] [CrossRef] [PubMed]
- Đorđević, S.M.; Santrač, A.; Cekić, N.D.; Marković, B.D.; Divović, B.; Ilić, T.M.; Savić, M.M.; Savić, S.D. Parenteral nanoemulsions of risperidone for enhanced brain delivery in acute psychosis: Physicochemical and in vivo performances. Int. J. Pharm. 2017, 533, 421–430. [Google Scholar] [CrossRef]
- Kumar, M.; Misra, A.; Babbar, A.K.; Mishra, A.K.; Mishra, P.; Pathak, K. Intranasal nanoemulsion based brain targeting drug delivery system of risperidone. Int. J. Pharm. 2008, 358, 285–291. [Google Scholar] [CrossRef] [PubMed]
- Vyas, T.K.; Shahiwala, A.; Amiji, M.M. Improved oral bioavailability and brain transport of Saquinavir upon administration in novel nanoemulsion formulations. Int. J. Pharm. 2008, 347, 93–101. [Google Scholar] [CrossRef] [Green Version]
- Patel, R.J.; Parikh, R.H. Intranasal delivery of topiramate nanoemulsion: Pharmacodynamic, pharmacokinetic and brain uptake studies. Int. J. Pharm. 2020, 585, 119486. [Google Scholar] [CrossRef]
- Tan, S.F.; Masoumi, H.R.F.; Karjiban, R.A.; Stanslas, J.; Kirby, B.P.; Basri, M.; Basri, H. Bin Ultrasonic emulsification of parenteral valproic acid-loaded nanoemulsion with response surface methodology and evaluation of its stability. Ultrason. Sonochem. 2016, 29, 299–308. [Google Scholar] [CrossRef]
- Mozafari, M.R.; Reed, C.J.; Rostron, C.; Kocum, C.; Piskin, E. Construction of stable anionic liposome-plasmid particles using the heating method: A preliminary investigation. Cell. Mol. Biol. Lett. 2002, 7, 923–927. [Google Scholar]
- Briuglia, M.L.; Rotella, C.; McFarlane, A.; Lamprou, D.A. Influence of cholesterol on liposome stability and on in vitro drug release. Drug Deliv. Transl. Res. 2015, 5, 231–242. [Google Scholar] [CrossRef] [Green Version]
- Jafari, S.M. Chapter 1—An Introduction to Nanoencapsulation Techniques for the Food Bioactive Ingredients. In Nanoencapsulation of Food Bioactive Ingredients; Jafari, S.M., Ed.; Academic Press: Cambridge, MA, USA, 2017; pp. 1–62. ISBN 978-0-12-809740-3. [Google Scholar]
- Mozafari, M.R.; Khosravi-Darani, K.; Borazan, G.G.; Cui, J.; Pardakhty, A.; Yurdugul, S. Encapsulation of food ingredients using nanoliposome technology. Int. J. Food Prop. 2008, 11, 833–844. [Google Scholar] [CrossRef]
- Liu, W.; Ye, A.; Liu, W.; Liu, C.; Han, J.; Singh, H. Behaviour of liposomes loaded with bovine serum albumin during in vitro digestion. Food Chem. 2015, 175, 16–24. [Google Scholar] [CrossRef]
- Campardelli, R.; Espirito Santo, I.; Albuquerque, E.C.; De Melo, S.V.; Della Porta, G.; Reverchon, E. Efficient encapsulation of proteins in submicro liposomes using a supercritical fluid assisted continuous process. J. Supercrit. Fluids 2016, 107, 163–169. [Google Scholar] [CrossRef]
- Gülseren, İ.; Guri, A.; Corredig, M. Encapsulation of Tea Polyphenols in Nanoliposomes Prepared with Milk Phospholipids and Their Effect on the Viability of HT-29 Human Carcinoma Cells. Food Dig. 2012, 3, 36–45. [Google Scholar] [CrossRef]
- Chen, Y.; Xia, G.; Zhao, Z.; Xue, F.; Gu, Y.; Chen, C.; Zhang, Y. 7,8-Dihydroxyflavone nano-liposomes decorated by crosslinked and glycosylated lactoferrin: Storage stability, antioxidant activity, in vitro release, gastrointestinal digestion and transport in Caco-2 cell monolayers. J. Funct. Foods 2020, 65, 103742. [Google Scholar] [CrossRef]
- Hassane Hamadou, A.; Huang, W.C.; Xue, C.; Mao, X. Comparison of β-carotene loaded marine and egg phospholipids nanoliposomes. J. Food Eng. 2020, 283, 110055. [Google Scholar] [CrossRef]
- Aliakbari, F.; Shabani, A.A.; Bardania, H.; Mohammad-Beigi, H.; Tayaranian Marvian, A.; Dehghani Esmatabad, F.; Vafaei, A.A.; Shojaosadati, S.A.; Saboury, A.A.; Christiansen, G.; et al. Formulation and anti-neurotoxic activity of baicalein-incorporating neutral nanoliposome. Coll. Surf. B Biointerfaces 2018, 161, 578–587. [Google Scholar] [CrossRef]
- Zhao, Y.Z.; Lin, M.; Lin, Q.; Yang, W.; Yu, X.C.; Tian, F.R.; Mao, K.L.; Yang, J.J.; Lu, C.T.; Wong, H.L. Intranasal delivery of bFGF with nanoliposomes enhances in vivo neuroprotection and neural injury recovery in a rodent stroke model. J. Control. Release 2016, 224, 165–175. [Google Scholar] [CrossRef]
- Hasan, M.; Belhaj, N.; Benachour, H.; Barberi-Heyob, M.; Kahn, C.J.F.; Jabbari, E.; Linder, M.; Arab-Tehrany, E. Liposome encapsulation of curcumin: Physico-chemical characterizations and effects on MCF7 cancer cell proliferation. Int. J. Pharm. 2014, 461, 519–528. [Google Scholar] [CrossRef]
- Lazar, A.N.; Mourtas, S.; Youssef, I.; Parizot, C.; Dauphin, A.; Delatour, B.; Antimisiaris, S.G.; Duyckaerts, C. Curcumin-conjugated nanoliposomes with high affinity for Aβ deposits: Possible applications to Alzheimer disease. Nanomed. Nanotechnol. Biol. Med. 2013, 9, 712–721. [Google Scholar] [CrossRef] [PubMed]
- Mourtas, S.; Lazar, A.N.; Markoutsa, E.; Duyckaerts, C.; Antimisiaris, S.G. Multifunctional nanoliposomes with curcumin-lipid derivative and brain targeting functionality with potential applications for Alzheimer disease. Eur. J. Med. Chem. 2014, 80, 175–183. [Google Scholar] [CrossRef] [PubMed]
- Jaafar-Maalej, C.; Diab, R.; Andrieu, V.; Elaissari, A.; Fessi, H. Ethanol injection method for hydrophilic and lipophilic drug-loaded liposome preparation. J. Liposome Res. 2010, 20, 228–243. [Google Scholar] [CrossRef] [PubMed]
- Rasti, B.; Jinap, S.; Mozafari, M.R.; Abd-Manap, M.Y. Optimization on preparation condition of polyunsaturated fatty acids nanoliposome prepared by Mozafari method. J. Liposome Res. 2014, 24, 99–105. [Google Scholar] [CrossRef]
- Mufamadi, M.S.; Choonara, Y.E.; Kumar, P.; Modi, G.; Naidoo, D.; Van Vuuren, S.; Ndesendo, V.M.K.; Toit, L.C.D.; Iyuke, S.E.; Pillay, V. Ligand-functionalized nanoliposomes for targeted delivery of galantamine. Int. J. Pharm. 2013, 448, 267–281. [Google Scholar] [CrossRef]
- Jiao, Y.; Li, D.; Liu, C.; Chang, Y.; Song, J.; Xiao, Y. Polypeptide-decorated nanoliposomes as novel delivery systems for lutein. RSC Adv. 2018, 8, 31372–31381. [Google Scholar] [CrossRef] [Green Version]
- Markoutsa, E.; Pampalakis, G.; Niarakis, A.; Romero, I.A.; Weksler, B.; Couraud, P.O.; Antimisiaris, S.G. Uptake and permeability studies of BBB-targeting immunoliposomes using the hCMEC/D3 cell line. Eur. J. Pharm. Biopharm. 2011, 77, 265–274. [Google Scholar] [CrossRef]
- Kuo, Y.C.; Chen, I.Y.; Rajesh, R. Use of functionalized liposomes loaded with antioxidants to permeate the blood–brain barrier and inhibit $β$-amyloid-induced neurodegeneration in the brain. J. Taiwan Inst. Chem. Eng. 2018, 87, 1–14. [Google Scholar] [CrossRef]
- Saesoo, S.; Bunthot, S.; Sajomsang, W.; Gonil, P.; Phunpee, S.; Songkhum, P.; Laohhasurayotin, K.; Wutikhun, T.; Yata, T.; Ruktanonchai, U.R.; et al. Phospholipid-chitosan hybrid nanoliposomes promoting cell entry for drug delivery against cervical cancer. J. Coll. Interface Sci. 2016, 480, 240–248. [Google Scholar] [CrossRef] [PubMed]
- Salem, H.F.; Ahmed, S.M.; Hassaballah, A.E.; Omar, M.M. Targeting brain cells with glutathione-modulated nanoliposomes: In vitro and in vivo study. Drug Des. Dev. Ther. 2015, 9, 3705–3727. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Praveen, A.; Aqil, M.; Imam, S.S.; Ahad, A.; Moolakkadath, T.; Ahmad, F.J. Lamotrigine encapsulated intra-nasal nanoliposome formulation for epilepsy treatment: Formulation design, characterization and nasal toxicity study. Coll. Surf. B Biointerfaces 2019, 174, 553–562. [Google Scholar] [CrossRef]
- Saffari, P.M.; Alijanpour, S.; Takzaree, N.; Sahebgharani, M.; Etemad-Moghadam, S.; Noorbakhsh, F.; Partoazar, A. Metformin loaded phosphatidylserine nanoliposomes improve memory deficit and reduce neuroinflammation in streptozotocin-induced Alzheimer’s disease model. Life Sci. 2020, 255, 117861. [Google Scholar] [CrossRef]
- Re, F.; Cambianica, I.; Sesana, S.; Salvati, E.; Cagnotto, A.; Salmona, M.; Couraud, P.O.; Moghimi, S.M.; Masserini, M.; Sancini, G. Functionalization with ApoE-derived peptides enhances the interaction with brain capillary endothelial cells of nanoliposomes binding amyloid-beta peptide. J. Biotechnol. 2011, 156, 341–346. [Google Scholar] [CrossRef]
- Upadhyay, P.; Trivedi, J.; Pundarikakshudu, K.; Sheth, N. Direct and enhanced delivery of nanoliposomes of anti schizophrenic agent to the brain through nasal route. Saudi Pharm. J. 2017, 25, 346–358. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kizelsztein, P.; Ovadia, H.; Garbuzenko, O.; Sigal, A.; Barenholz, Y. Pegylated nanoliposomes remote-loaded with the antioxidant tempamine ameliorate experimental autoimmune encephalomyelitis. J. Neuroimmunol. 2009, 213, 20–25. [Google Scholar] [CrossRef]
- Mahtab, A.; Rizwanullah, M.; Pandey, S.; Leekha, A.; Rabbani, S.A.; Verma, A.K.; Aqil, M.; Talegaonkar, S. Quality by design driven development and optimization of teriflunomide loaded nanoliposomes for treatment of rheumatoid arthritis: An in vitro and in vivo assessments. J. Drug Deliv. Sci. Technol. 2019, 51, 383–396. [Google Scholar] [CrossRef]
- Ghanbarzadeh, B.; Babazadeh, A.; Hamishehkar, H. Nano-phytosome as a potential food-grade delivery system. Food Biosci. 2016, 15, 126–135. [Google Scholar] [CrossRef]
- Saraf, S.; Khan, J.; Alexander, A.; Ajazuddin; Saraf, S. Recent advances and future prospects of phyto-phospholipid complexation technique for improving pharmacokinetic profile of plant actives. J. Control. Release 2013, 168, 50–60. [Google Scholar] [CrossRef]
- Semalty, A.; Semalty, M.; Rawat, M.S.M.; Franceschi, F. Supramolecular phospholipids-polyphenolics interactions: The PHYTOSOME ® strategy to improve the bioavailability of phytochemicals. Fitoterapia 2010, 81, 306–314. [Google Scholar] [CrossRef]
- Lu, M.; Qiu, Q.; Luo, X.; Liu, X.; Sun, J.; Wang, C.; Lin, X.; Deng, Y.; Song, Y. Phyto-phospholipid complexes (phytosomes): A novel strategy to improve the bioavailability of active constituents. Asian J. Pharm. Sci. 2019, 14, 265–274. [Google Scholar] [CrossRef] [PubMed]
- Babazadeh, A.; Jafari, S.M.; Shi, B. Encapsulation of food ingredients by nanophytosomes. In Lipid-Based Nanostructures for Food Encapsulation Purposes; Jafari, S.M., Ed.; Academic Press: Cambridge, MA, USA, 2019; Volume 2, pp. 405–443. [Google Scholar]
- Karpuz, M.; Gunay, M.S.; Ozer, Y.A. Liposomes and phytosomes for phytoconstituents. In Advances and Avenues in the Development of Novel Carriers for Bioactives and Biological Agents; Singh, M.R., Singh, D., Kanwar, J., Chauhan, N.S., Eds.; Academic Press: Cambridge, MA, USA, 2020; pp. 525–553. [Google Scholar]
- Ting, Y.; Jiang, Y.; Ho, C.T.; Huang, Q. Common delivery systems for enhancing in vivo bioavailability and biological efficacy of nutraceuticals. J. Funct. Foods 2014, 7, 112–128. [Google Scholar] [CrossRef]
- Gnananath, K.; Nataraj, K.S.; Rao, B.G. Phospholipid complex technique for superior bioavailability of phytoconstituents. Adv. Pharm. Bull. 2017, 7, 35–42. [Google Scholar] [CrossRef] [Green Version]
- Froiio, F.; Gagliardi, A.; Fresta, M.; Cosco, D.; Paolino, D. Phytosomes as Useful Drug Delivery Systems for Cosmeceutical Application. In Novel Drug Delivery Systems for Phytoconstituents; Gupta, M., Chauhan, D.N., Vikas, S., Nagendra, S.C., Eds.; CRC Press: Boca Raton, FL, USA, 2019; pp. 105–119. ISBN 9781138481374. [Google Scholar]
- Caesar, L.K.; Cech, N.B.; Kubanek, J.; Linington, R.; Luesch, H. Synergy and antagonism in natural product extracts: When 1 + 1 does not equal 2. Nat. Prod. Rep. 2019, 36, 845–936. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Harborne, J.B. Biochemical Plant Ecology. In Plant Biochemistry; Elsevier: Amsterdam, The Netherlands, 1997; pp. 503–516. [Google Scholar]
- Seremet, O.C.; Olaru, O.T.; Gutu, C.M.; Nitulescu, G.M.; Ilie, M.; Negres, S.; Zbarcea, C.E.; Purdel, C.N.; Spandidos, D.A.; Tsatsakis, A.M.; et al. Toxicity of plant extracts containing pyrrolizidine alkaloids using alternative invertebrate models. Mol. Med. Rep. 2018, 17, 7757–7763. [Google Scholar] [CrossRef]
- Bolarinwa, I.F.; Oke, M.O.; Olaniyan, S.A.; Ajala, A.S. A Review of Cyanogenic Glycosides in Edible Plants. In Toxicology—New Aspects to This Scientific Conundrum; Larramendy, M.L., Soloneski, S., Eds.; Interchopen: London, UK, 2016; pp. 179–191. [Google Scholar]
- Höllerhage, M.; Rösler, T.W.; Berjas, M.; Luo, R.; Tran, K.; Richards, K.M.; Sabaa-Srur, A.U.; Maia, J.G.S.; de Moraes, M.R.; Godoy, H.T.; et al. Neurotoxicity of dietary supplements from Annonaceae species. Int. J. Toxicol. 2015, 34, 543–550. [Google Scholar] [CrossRef] [Green Version]
- Liang, Q.; Chow, A.H.L.; Wang, Y.; Tong, H.H.Y.; Zheng, Y. Removal of toxic aristolochic acid components from Aristolochia plants by supercritical fluid extraction. Sep. Purif. Technol. 2010, 72, 269–274. [Google Scholar] [CrossRef]
- Yang, H.-Y.; Chen, P.-C.; Wang, J.-D. Chinese herbs containing aristolochic acid associated with renal failure and urothelial carcinoma: A review from epidemiologic observations to causal inference. BioMed Res. Int. 2014, 2014, 1–9. [Google Scholar] [CrossRef] [Green Version]
- Schulzová, V.; Hajšlová, J.; Botek, P.; Peroutka, R. Furanocoumarins in vegetables: Influence of farming system and other factors on levels of toxicants. J. Sci. Food Agric. 2007, 87, 2763–2767. [Google Scholar] [CrossRef]
- Bruni, R.; Barreca, D.; Protti, M.; Brighenti, V.; Righetti, L.; Anceschi, L.; Mercolini, L.; Benvenuti, S.; Gattuso, G.; Pellati, F. Botanical sources, chemistry, analysis, and biological activity of furanocoumarins of pharmaceutical interest. Molecules 2019, 24, 2163. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Roberts, D.M.; Gallapatthy, G.; Dunuwille, A.; Chan, B.S.; Roberts, D. Pharmacological treatment of cardiac glycoside poisoning. Br. J. Clin. Pharmacol. 2015, 81, 488–495. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tan, Q.; Liu, S.; Chen, X.; Wu, M.; Wang, H.; Yin, H.; He, D.; Xiong, H.; Zhang, J. Design and evaluation of a novel evodiamine-phospholipid complex for improved oral bioavailability. AAPS PharmSciTech 2012, 13, 534–547. [Google Scholar] [CrossRef] [Green Version]
- Yue, P.F.; Yuan, H.L.; Li, X.Y.; Yang, M.; Zhu, W.F. Process optimization, characterization and evaluation in vivo of oxymatrine-phospholipid complex. Int. J. Pharm. 2010, 387, 139–146. [Google Scholar] [CrossRef] [PubMed]
- Freag, M.S.; Saleh, W.M.; Abdallah, O.Y. Self-assembled phospholipid-based phytosomal nanocarriers as promising platforms for improving oral bioavailability of the anticancer celastrol. Int. J. Pharm. 2018, 535, 18–26. [Google Scholar] [CrossRef] [PubMed]
- Maiti, K.; Mukherjee, K.; Murugan, V.; Saha, B.P.; Mukherjee, P.K. Enhancing bioavailability and hepatoprotective activity of andrographolide from Andrographis paniculata, a well-known medicinal food, through its herbosome. J. Sci. Food Agric. 2010, 90, 43–51. [Google Scholar] [CrossRef]
- Yue, P.F.; Yuan, H.L.; Xie, H.; Xiao, X.H.; Yang, M.; Liao, M.X.; Zhu, W.F.; Cai, P.L. Preparation, characterization, and bioavailability of ursodeoxycholic acid-phospholipid complex in vivo. Drug Dev. Ind. Pharm. 2008, 34, 708–718. [Google Scholar] [CrossRef] [PubMed]
- Semalty, A.; Tanwar, Y.S. Nimesulide-phosphatidylcholine complex for improvement of solubility and dissolution. Am. J. Drug Discov. Dev. 2013, 3, 225–234. [Google Scholar] [CrossRef] [Green Version]
- Pathan, R.A.; Bhandari, U.; Javed, S.; Nag, T.C. Anti-apoptotic potential of gymnemic acid phospholipid complex pretreatment in Wistar rats with experimental cardiomyopathy. Indian J. Exp. Biol. 2012, 50, 117–127. [Google Scholar] [PubMed]
- Singh, D.; Rawat, M.S.M.; Semalty, A.; Semalty, M. Emodin-phospholipid complex: A potential of herbal drug in the novel drug delivery system. J. Therm. Anal. Calorim. 2012, 108, 289–298. [Google Scholar] [CrossRef]
- Feng, C.; Yahan, G.; Zhi, Y.; Qineng, P. Enhanced Oral Bioavailability of Oleanolic Acid in Rats with Phospholipid Complex. Lett. Drug Des. Discov. 2012, 9, 505–512. [Google Scholar] [CrossRef]
- Pu, Y.; Zhang, X.; Zhang, Q.; Wang, B.; Chen, Y.; Zang, C.; Wang, Y.; Dong, T.T.X.; Zhang, T. 20(S)-Protopanaxadiol phospholipid complex: Process optimization, characterization, in vitro dissolution and molecular docking studies. Molecules 2016, 21, 1396. [Google Scholar] [CrossRef] [Green Version]
- Yu, F.; Li, Y.; Chen, Q.; He, Y.; Wang, H.; Yang, L.; Guo, S.; Meng, Z.; Cui, J.; Xue, M.; et al. Monodisperse microparticles loaded with the self-assembled berberine-phospholipid complex-based phytosomes for improving oral bioavailability and enhancing hypoglycemic efficiency. Eur. J. Pharm. Biopharm. 2016, 103, 136–148. [Google Scholar] [CrossRef]
- Pathan, R.A.; Bhandari, U. Preparation and characterization of embelin–phospholipid complex as effective drug delivery tool. J. Incl. Phenom. Macrocycl. Chem. 2011, 69, 139–147. [Google Scholar] [CrossRef]
- Semalty, A.; Semalty, M.; Singh, D.; Rawat, M.S.M. Phyto-phospholipid complex of catechin in value added herbal drug delivery. J. Incl. Phenom. Macrocycl. Chem. 2012, 73, 377–386. [Google Scholar] [CrossRef]
- Telange, D.R.; Patil, A.T.; Pethe, A.M.; Fegade, H.; Anand, S.; Dave, V.S. Formulation and characterization of an apigenin-phospholipid phytosome (APLC) for improved solubility, in vivo bioavailability, and antioxidant potential. Eur. J. Pharm. Sci. 2017, 108, 36–49. [Google Scholar] [CrossRef] [Green Version]
- Mancini, S.; Nardo, L.; Gregori, M.; Ribeiro, I.; Mantegazza, F.; Delerue-Matos, C.; Masserini, M.; Grosso, C. Functionalized liposomes and phytosomes loading Annona muricata L. aqueous extract: Potential nanoshuttles for brain-delivery of phenolic compounds. Phytomedicine 2018, 42, 233–244. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Abd El-Fattah, A.I.; Fathy, M.M.; Ali, Z.Y.; El-Garawany, A.E.R.A.; Mohamed, E.K. Enhanced therapeutic benefit of quercetin-loaded phytosome nanoparticles in ovariectomized rats. Chem. Biol. Interact. 2017, 271, 30–38. [Google Scholar] [CrossRef]
- Saoji, S.D.; Raut, N.A.; Dhore, P.W.; Borkar, C.D.; Popielarczyk, M.; Dave, V.S. Preparation and evaluation of phospholipid-based complex of standardized Centella extract (SCE) for the enhanced delivery of phytoconstituents. AAPS J. 2016, 18, 102–114. [Google Scholar] [CrossRef] [PubMed]
- Direito, R.; Reis, C.; Roque, L.; Gonçalves, M.; Sanches-Silva, A.; Gaspar, M.M.; Pinto, R.; Rocha, J.; Sepodes, B.; Bronze, M.R.; et al. Phytosomes with persimmon (Diospyros kaki l.) extract: Preparation and preliminary demonstration of in vivo tolerability. Pharmaceutics 2019, 11, 296. [Google Scholar] [CrossRef] [Green Version]
- Nazari, M.; Ghanbarzadeh, B.; Samadi Kafil, H.; Zeinali, M.; Hamishehkar, H. Garlic essential oil nanophytosomes as a natural food preservative: Its application in yogurt as food model. Coll. Interface Sci. Commun. 2019, 30, 100176. [Google Scholar] [CrossRef]
- El-Gazayerly, O.N.; Makhlouf, A.I.A.; Soelm, A.M.A.; Mohmoud, M.A. Antioxidant and hepatoprotective effects of silymarin phytosomes compared to milk thistle extract in CCl4 induced hepatotoxicity in rats. J. Microencapsul. 2014, 31, 23–30. [Google Scholar] [CrossRef] [PubMed]
- Babazadeh, A.; Ghanbarzadeh, B.; Hamishehkar, H. Phosphatidylcholine-rutin complex as a potential nanocarrier for food applications. J. Funct. Foods 2017, 33, 134–141. [Google Scholar] [CrossRef]
- Vankudri, R.; Habbu, P.; Hiremath, M.; Patil, B.S.; Savant, C. Preparation and therapeutic evaluation of rutin-phospholipid complex for antidiabetic activity. J. Appl. Pharm. Sci. 2016, 6, 90–101. [Google Scholar] [CrossRef] [Green Version]
- Hooresfand, Z.; Ghanbarzadeh, S.; Hamishehkar, H. Preparation and characterization of rutin-loaded nanophytosomes. Pharm. Sci. 2015, 21, 145–151. [Google Scholar] [CrossRef] [Green Version]
- Maiti, K.; Mukherjee, K.; Gantait, A.; Saha, B.P.; Mukherjee, P.K. Curcumin-phospholipid complex: Preparation, therapeutic evaluation and pharmacokinetic study in rats. Int. J. Pharm. 2007, 330, 155–163. [Google Scholar] [CrossRef] [PubMed]
- Tung, B.T.; Hai, N.T.; Son, P.K. Hepatoprotective effect of Phytosome Curcumin against paracetamol-induced liver toxicity in mice. Brazil. J. Pharm. Sci. 2017, 53, 1–13. [Google Scholar] [CrossRef] [Green Version]
- Li, Y.; Yang, D.J.; Chen, S.L.; Chen, S.B.; Chan, A.S.C. Process parameters and morphology in puerarin, phospholipids and their complex microparticles generation by supercritical antisolvent precipitation. Int. J. Pharm. 2008, 359, 35–45. [Google Scholar] [CrossRef] [PubMed]
- Xia, F.; Hu, D.; Jin, H.; Zhao, Y.; Liang, J. Preparation of lutein proliposomes by supercritical anti-solvent technique. Food Hydrocoll. 2012, 26, 456–463. [Google Scholar] [CrossRef]
- Zhao, L.; Temelli, F.; Curtis, J.M.; Chen, L. Encapsulation of lutein in liposomes using supercritical carbon dioxide. Food Res. Int. 2017, 100, 168–179. [Google Scholar] [CrossRef]
- Kalita, B.; Patwary, B.N. Formulation and in vitro evaluation of hesperidin-phospholipid complex and its antioxidant potential. Curr. Drug Ther. 2020, 15, 28–36. [Google Scholar] [CrossRef]
- Jain, S.; Dhanotiya, C.; Malviya, N. Physicochemical characterization and determination of free radical scavenging activity of rutin-phospholipid complex. Int. J. Pharm. Sci. Res. 2012, 3, 909–913. [Google Scholar]
- Matias, D.; Roque, L.; Simões, M.d.F.; Diaz-Lanza, A.; Rijo, P.; Reis, C.P. Plectranthus madagascariensis phytosomes: Formulation optimization. J. Biomed. Biopharm. Res. 2015, 12, 223–231. [Google Scholar] [CrossRef]
- Saoji, S.D.; Dave, V.S.; Dhore, P.W.; Bobde, Y.S.; Mack, C.; Gupta, D.; Raut, N.A. The role of phospholipid as a solubility- and permeability-enhancing excipient for the improved delivery of the bioactive phytoconstituents of Bacopa monnieri. Eur. J. Pharm. Sci. 2017, 108, 23–35. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rasaie, S.; Ghanbarzadeh, S.; Mohammadi, M.; Hamishehkar, H. Nano phytosomes of quercetin: A promising formulation for fortification of food products with antioxidants. Pharm. Sci. 2014, 20, 96–101. [Google Scholar]
- Lim, A.W.; Ng, P.Y.; Chieng, N.; Ng, S.F. Moringa oleifera leaf extract–loaded phytophospholipid complex for potential application as wound dressing. J. Drug Deliv. Sci. Technol. 2019, 54, 101329. [Google Scholar] [CrossRef]
- Kim, S.M.; Jung, J.I.; Chai, C.; Imm, J.Y. Characteristics and glucose uptake promoting effect of chrysin-loaded phytosomes prepared with different phospholipid matrices. Nutrients 2019, 11. [Google Scholar] [CrossRef] [Green Version]
- Singh, D.; SM Rawat, M.; Semalty, A.; Semalty, M. Rutin-phospholipid complex: An innovative technique in novel drug delivery system- NDDS. Curr. Drug Deliv. 2012, 9, 305–314. [Google Scholar] [CrossRef] [PubMed]
- Maryana, W.; Rachmawati, H.; Mudhakir, D. Formation of phytosome containing silymarin using thin layer-hydration technique aimed for oral delivery. Mater. Today Proc. 2016, 3, 855–866. [Google Scholar] [CrossRef]
- He, H.; Yao, J.; Zhang, Y.; Chen, Y.; Wang, K.; Lee, R.J.; Yu, B.; Zhang, X. Solid lipid nanoparticles as a drug delivery system to across the blood-brain barrier. Biochem. Biophys. Res. Commun. 2019, 519, 385–390. [Google Scholar] [CrossRef]
- Svetlichny, G.; Kulkamp-Guerreiro, I.C.; Cunha, S.L.; Silva, F.E.K.; Bueno, K.; Pohlmann, A.R.; Fuentefria, A.M.; Guterres, S.S. Solid lipid nanoparticles containing copaiba oil and allantoin: Development and role of nanoencapsulation on the antifungal activity. Pharmazie 2015, 70, 155–164. [Google Scholar] [CrossRef]
- Fang, C.-L.; Al-Suwayeh, S.A.; Fang, J.-Y. Nanostructured lipid carriers (NLCs) for drug delivery and targeting. Recent Pat. Nanotechnol. 2012, 7, 41–55. [Google Scholar] [CrossRef]
- De Carvalho, S.M.; Noronha, C.M.; Floriani, C.L.; Lino, R.C.; Rocha, G.; Bellettini, I.C.; Ogliari, P.J.; Barreto, P.L.M. Optimization of α-tocopherol loaded solid lipid nanoparticles by central composite design. Ind. Crops Prod. 2013, 49, 278–285. [Google Scholar] [CrossRef]
- Salvi, V.R.; Pawar, P. Nanostructured lipid carriers (NLC) system: A novel drug targeting carrier. J. Drug Deliv. Sci. Technol. 2019, 51, 255–267. [Google Scholar] [CrossRef]
- Beloqui, A.; Solinís, M.Á.; Rodríguez-Gascón, A.; Almeida, A.J.; Préat, V. Nanostructured lipid carriers: Promising drug delivery systems for future clinics. Nanomed. Nanotechnol. Biol. Med. 2016, 12, 143–161. [Google Scholar] [CrossRef] [PubMed]
- Gordillo-Galeano, A.; Mora-Huertas, C.E. Solid Lipid Nanoparticles and Nanostructured Lipid Carriers: A Review Emphasizing on Particle Structure and Drug Re-Lease; Elsevier B.V.: Amterdam, The Netherlands, 2018; Volume 133, ISBN 5713165000. [Google Scholar]
- Tapeinos, C.; Battaglini, M.; Ciofani, G. Advances in the design of solid lipid nanoparticles and nanostructured lipid carriers for targeting brain diseases. J. Control. Release 2017, 264, 306–332. [Google Scholar] [CrossRef]
- Khosa, A.; Reddi, S.; Saha, R.N. Nanostructured lipid carriers for site-specific drug delivery. Biomed. Pharmacother. 2018, 103, 598–613. [Google Scholar] [CrossRef] [PubMed]
- Yasir, M.; Sara, U.V.S. Solid lipid nanoparticles for nose to brain delivery of haloperidol: In vitro drug release and pharmacokinetics evaluation. Acta Pharm. Sin. B 2014, 4, 454–463. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Abdel Hady, M.; Sayed, O.M.; Akl, M.A. Brain uptake and accumulation of new levofloxacin-doxycycline combination through the use of solid lipid nanoparticles: Formulation; Optimization and in-vivo evaluation. Coll. Surf. B Biointerfaces 2020, 193, 111076. [Google Scholar] [CrossRef] [PubMed]
- Devkar, T.B.; Tekade, A.R.; Khandelwal, K.R. Surface engineered nanostructured lipid carriers for efficient nose to brain delivery of ondansetron HCl using Delonix regia gum as a natural mucoadhesive polymer. Coll. Surf. B Biointerfaces 2014, 122, 143–150. [Google Scholar] [CrossRef]
- Tamjidi, F.; Shahedi, M.; Varshosaz, J.; Nasirpour, A. Design and Characterization of Astaxanthin-Loaded Nanostructured Lipid Carriers; Elsevier B.V.: Amterdam, The Netherlands, 2014; Volume 26, ISBN 8415683111. [Google Scholar]
- Lacatusu, I.; Mitrea, E.; Badea, N.; Stan, R.; Oprea, O.; Meghea, A. Lipid nanoparticles based on omega-3 fatty acids as effective carriers for lutein delivery. Preparation and in vitro characterization studies. J. Funct. Foods 2013, 5, 1260–1269. [Google Scholar] [CrossRef]
- Nasirizadeh, S.; Malaekeh-Nikouei, B. Solid lipid nanoparticles and nanostructured lipid carriers in oral cancer drug delivery. J. Drug Deliv. Sci. Technol. 2020, 55, 101458. [Google Scholar] [CrossRef]
- Martins, S.; Tho, I.; Reimold, I.; Fricker, G.; Souto, E.; Ferreira, D.; Brandl, M. Brain delivery of camptothecin by means of solid lipid nanoparticles: Formulation design, in vitro and in vivo studies. Int. J. Pharm. 2012, 439, 49–62. [Google Scholar] [CrossRef] [PubMed]
- Salem, L.H.; El-Feky, G.S.; Fahmy, R.H.; El Gazayerly, O.N.; Abdelbary, A. Coated lipidic nanoparticles as a new strategy for enhancing nose-to-brain delivery of a hydrophilic drug molecule. J. Pharm. Sci. 2020, 109, 2237–2251. [Google Scholar] [CrossRef]
- Rassu, G.; Soddu, E.; Posadino, A.M.; Pintus, G.; Sarmento, B.; Giunchedi, P.; Gavini, E. Nose-to-brain delivery of BACE1 siRNA loaded in solid lipid nanoparticles for Alzheimer’s therapy. Coll. Surf. B Biointerfaces 2017, 152, 296–301. [Google Scholar] [CrossRef] [PubMed]
- Madan, J.; Pandey, R.S.; Jain, V.; Katare, O.P.; Chandra, R.; Katyal, A. Poly (ethylene)-glycol conjugated solid lipid nanoparticles of noscapine improve biological half-life, brain delivery and efficacy in glioblastoma cells. Nanomed. Nanotechnol. Biol. Med. 2013, 9, 492–503. [Google Scholar] [CrossRef]
- Jose, S.; Anju, S.S.; Cinu, T.A.; Aleykutty, N.A.; Thomas, S.; Souto, E.B. In vivo pharmacokinetics and biodistribution of resveratrol-loaded solid lipid nanoparticles for brain delivery. Int. J. Pharm. 2014, 474, 6–13. [Google Scholar] [CrossRef]
- Venishetty, V.K.; Samala, R.; Komuravelli, R.; Kuncha, M.; Sistla, R.; Diwan, P.V. β-Hydroxybutyric acid grafted solid lipid nanoparticles: A novel strategy to improve drug delivery to brain. Nanomed. Nanotechnol. Biol. Med. 2013, 9, 388–397. [Google Scholar] [CrossRef]
- Arduino, I.; Depalo, N.; Re, F.; Dal Magro, R.; Panniello, A.; Margiotta, N.; Fanizza, E.; Lopalco, A.; Laquintana, V.; Cutrignelli, A.; et al. PEGylated solid lipid nanoparticles for brain delivery of lipophilic kiteplatin Pt(IV) prodrugs: An in vitro study. Int. J. Pharm. 2020, 583, 119351. [Google Scholar] [CrossRef]
- Wu, Y.; Song, X.; Kebebe, D.; Li, X.; Xue, Z.; Li, J.; Du, S.; Pi, J.; Liu, Z. Brain targeting of Baicalin and Salvianolic acid B combination by OX26 functionalized nanostructured lipid carriers. Int. J. Pharm. 2019, 571, 118754. [Google Scholar] [CrossRef] [PubMed]
- Rajput, A.P.; Butani, S.B. Resveratrol anchored nanostructured lipid carrier loaded in situ gel via nasal route: Formulation, optimization and in vivo characterization. J. Drug Deliv. Sci. Technol. 2019, 51, 214–223. [Google Scholar] [CrossRef]
- Singh, S.K.; Hidau, M.K.; Gautam, S.; Gupta, K.; Singh, K.P.; Singh, S.K.; Singh, S. Glycol chitosan functionalized asenapine nanostructured lipid carriers for targeted brain delivery: Pharmacokinetic and teratogenic assessment. Int. J. Biol. Macromol. 2018, 108, 1092–1100. [Google Scholar] [CrossRef] [PubMed]
- Khan, N.; Shah, F.A.; Rana, I.; Ansari, M.M.; Din, F.U.; Rizvi, S.Z.H.; Aman, W.; Lee, G.Y.; Lee, E.S.; Kim, J.K.; et al. Nanostructured lipid carriers-mediated brain delivery of carbamazepine for improved in vivo anticonvulsant and anxiolytic activity. Int. J. Pharm. 2020, 577, 119033. [Google Scholar] [CrossRef]
- Pokharkar, V.; Patil-Gadhe, A.; Palla, P. Efavirenz loaded nanostructured lipid carrier engineered for brain targeting through intranasal route: In-vivo pharmacokinetic and toxicity study. Biomed. Pharmacother. 2017, 94, 150–164. [Google Scholar] [CrossRef]
- Garg, B.; Beg, S.; Kumar, R.; Katare, O.P.; Singh, B. Nanostructured lipidic carriers of lopinavir for effective management of HIV-associated neurocognitive disorder. J. Drug Deliv. Sci. Technol. 2019, 53, 101220. [Google Scholar] [CrossRef]
- Jazuli, I.; Annu; Nabi, B.; Moolakkadath, T.; Alam, T.; Baboota, S.; Ali, J. Optimization of nanostructured lipid carriers of lurasidone hydrochloride using Box-Behnken design for brain targeting: In vitro and in vivo studies. J. Pharm. Sci. 2019, 108, 3082–3090. [Google Scholar] [CrossRef]
- Wavikar, P.; Pai, R.; Vavia, P. Nose to brain delivery of rivastigmine by in situ gelling cationic nanostructured lipid carriers: Enhanced brain distribution and pharmacodynamics. J. Pharm. Sci. 2017, 106, 3613–3622. [Google Scholar] [CrossRef] [PubMed]
- Kumar, S.; Dilbaghi, N.; Saharan, R.; Bhanjana, G. Nanotechnology as emerging tool for enhancing solubility of poorly water-soluble Drugs. Bionanoscience 2012, 2, 227–250. [Google Scholar] [CrossRef]
- Poovi, G.; Damodharan, N. Lipid nanoparticles: A challenging approach for oral delivery of BCS Class-II drugs. Futur. J. Pharm. Sci. 2018, 4, 191–205. [Google Scholar] [CrossRef]
- Saraiva, C.; Praça, C.; Ferreira, R.; Santos, T.; Ferreira, L.; Bernardino, L. Nanoparticle-mediated brain drug delivery: Overcoming blood-brain barrier to treat neurodegenerative diseases. J. Control. Release 2016, 235, 34–47. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Attama, A.A.; Momoh, M.A.; Builders, P.F. Chapter 5-Lipid nanoparticulate drug delivery systems: A revolution in dosage form design and development. In Recent Advances in Novel Drug Carrier Systems; InTech: Rijeka, Croatia, 2012; pp. 107–140. [Google Scholar]





| Compounds/Extracts | Oil | Surfactant: Cosurfactant | Oil: Surfactant Ratio v/v | T | Oil Phase | Aqueous Phase | Ultrasound | Rotation | Time | Analysis | Ref |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Seaweed extract | |||||||||||
| Sargassum longifolium (Turner) C.Agardh | Orange oil | Span 80: Pluronic L81 | 10:1 | Room T | Oil, Span 80 | Deionized water, Pluronic L81 | Probe sonicator, 30 s on; 10 s off; 40% amp, 140 W, 30 min | Yes, 30 min | 24 h | DLS, SEM, TEM, FTIR, UV-Vis, in vitro drug release, cytotoxicity | [71] |
| Natural compounds | |||||||||||
| Astaxanthin | Soybean oil | Ginseng saponins | 0.08–1.2% w/w surfactant, distilled water | 8000 rpm | 5 min | DLS, UV-Vis | [67] | ||||
| Astaxanthin | Soybean oil | Modified lecithin or sodium caseinate | Oil, drug | Distilled water, 2.0% w/w surfactant | 10,000 rpm | 5 min | DLS, laser diffraction, UV-Vis, in vitro intestinal digestion, CLSM | [68] | |||
| Carvacrol | n-hexane | Tween 80 | Oil, drug | Deionized water, surfactant | 20 kHz, 100 W, 1 h | 1 h | 2 h | TEM, DLS, in vivo studies, ELISA, HPLC | [72] | ||
| Kaempferol | 16% w/w MCT | 1% w/w Polysorbate 80 | Oil, 0.1% drug, 5% w/w lecithin | Distilled water, surfactant | 9500 rpm | 1 min | PCS, TEM, viscometry, refractometry, HPLC, DPPH, ex vivo diffusion, in vivo studies | [73] | |||
| Lutein | 10% corn oil (w/w) | 50 °C | Oil, ethyl acetate, drug | Distilled water, 2% whey protein isolate | 20 min | DLS, TEM, HPLC, in vitro cytotoxicity, cellular uptake | [60] | ||||
| Lutein | 10 g soybean oil, 0.67 g Xangold 15% oil, 12 drops vitamin E oil | 8 g Phospholipon 85G | 60 °C | Oils, surfactant, drug | Natural spring water | 35 min | DLS, HPLC-DAD | [61] | |||
| Lutein | Corn oil | Quillaja saponin, Tween 80, WPI or sodium caseinate | Oil, drug | 0.25% surfactant, aqueous buffer solution, 10 mM phosphate, pH 7 | 10,000 rpm | 2 min | Colorimeter, DLS | [69] | |||
| Lutein | EtOh/ MCT oil 50/50, v/v | Lecithin, β-lactoglobulin, Biozate 1 or Tween 20 | Oil, drug, antioxidant, lecithin | β-lactoglobulin, Biozate 1 or Tween 20 in water | 5 min 70% max power | 500 rpm | 10 min | Laser diffraction, UV-Vis, HPLC, cytotoxicity, cellular uptake | [70] | ||
| Lycopene | Sesame, linseed, walnut oil | Oil, drug | Deionized water, lactoferrin | 10,000 rpm | 3 min | DLS, TEM, UV-Vis, in vitro digestion | [74] | ||||
| Naringenin | Capryol 90 | Tween 20: EtOH | Oil, drug, surfactant | Distilled water | Continuous | > 1 h | PCS, TEM, ROS activity, in vitro studies | [75] | |||
| Rutin | Sefsol 218: Tocopheryl polyethylene glycol 1000 succinate | Solutol HS15: Transcutol P | 1:9; 1:8; 1:7; 1:6; 1:5; 1:4; 1:3.5; 1:3; 3:7; 1:2; 4:6; 5:5; 6:4; 7:3; 8:2; 9:1 | Oil, drug, surfactant | Double distilled water | Continuous | TEM, HPLC, DLS, in vitro drug release, in vivo studies | [76] | |||
| siRNA | Flaxseed oil | Tween 80 | DOTAP dissolved in EtOH, siRNA, oil | Water, Lipoid E80®, surfactant | 10 min 22% amplitude 50% duty cycle | 6000 rpm | 2 min | DLS, TEM, EMSA, CLSM, FCM, in vitro gene silencing, in vivo studies | [77] | ||
| Thymoquinone | Oleic acid | Tween 20: carbitol (0:3; 1:3; 2:3; 3:3; 3:2; 3:1; 3:0) | 1:9; 2:8; 3:7; 4:6; 5:5; 6:4; 7:3; 8:2; 9:1 | Oil, drug, surfactants | Purified water | Continuous | DLS, DPPH, FTIR, refractometry, in vitro drug release, ex vivo permeability, in vivo studies, UPLC-PDA | [78] | |||
| Synthetic compounds | |||||||||||
| Asenapine maleate | Capmul PG-8 | Kolliphore RH40:Transcutol HP (3:1; 2:1; 1:1; 1:2; 1:3) | 1:9; 2:8; 3:7; 4:6; 5:5; 6:4; 7:3; 8:2; 9:1 | Oil, drug, surfactant | Double distilled water | Continuous | DLS, TEM, viscometry, in vitro drug release, in vivo studies, HPLC | [79] | |||
| Darunavir | Soybean oil | Tween 80 (0.5; 0.75; 1; 1.25; 1.5% w/v) | 55–60 °C | 8% w/v oil, surfactant, drug | Distilled water, 1.2% egg lecithin | 8000 rpm | 20 min | DLS, UV-Vis, conductivity, TEM, in vitro drug release, in vivo studies | [80] | ||
| Gabapentin | Capmul MCM | Tween 80: PEG-400 | 1:9; 2:8; 3:7; 4:6; 5:5; 6:4 | Oil, surfactants, drug | Double distilled water, 0.3% oleic acid, 2.25% glycerol | 70% amplitude | 10 min | UV-Vis, FTIR, DLS, TEM, viscometry, in vitro diffusion, ex vivo permeation | [81] | ||
| Indinavir | 10% w/v soybean oil | 0.2, 0.6, 1% w/v Tween 80 | 70 °C | Oil, surfactant, 0.25% w/v α-tocopherol, 1.2% w/v egg PC | 750 W, 20 min at 50% amplitude | 15,000 rpm | 3 min | DLS, in vitro drug release, HPLC, FLM, in vivo studies | [82] | ||
| Letrozole | Triacetin | Tween 80:PEG-400 1:1; 2:1; 3:1; 4:1 | 1:9; 1:8; 1:7; 1:6; 1:5; 2:8; 1:3.5; 1:3; 3:7; 1:2; 4:6; 5:5; 6:4; 7:3; 8:2; 9:1 | Oil, drug, surfactant | 14.66% cosurfactant, 48% distilled water | Yes | UV-Vis, DLS, TEM, in vitro drug release, ex vivo permeation, DSC, in vivo studies | [83] | |||
| Risperidone | MCT: soybean oil (4:1 w/w) | 2% w/w Polysorbate 80, Kolliphor® P 188 or Solutol® HS 15 | 25 or 50 °C | 20% Oil, 2% emulsifier (lecithin), 0.05% antioxidant (BHT). 2% benzyl alcohol | Surfactants dissolved in 0.01M PBS pH 9 or double distilled water | 10,000 rpm | 3 min | PCS, laser diffraction, viscometry, conductivity, AFM, DSC, FTIR, in vivo studies | [64] | ||
| Risperidone (follow-up study) | MCT: soybean oil (4:1 w/w) | 2% w/w Polysorbate 80 | 50 °C | 20% Oil, 2% emulsifier (lecithin), 0.05% antioxidant (BHT). 2% benzyl alcohol | Double-distilled water, Polysorbate 80, sodium oleate, glycerol | 10,000 rpm | 3 min | PCS, laser diffraction, DLS, viscometry, conductivity, in vivo studies | [84] | ||
| Risperidone | Capmul MCM | Tween 80: (transcutol: propylene glycol (1:1 w/w)) | 35 °C | 8% oil, 29.33% surfactant, drug | 0.5, 0.7% Carbopol 934 | Continuous | UV-Vis, PCS, in vivo studies | [85] | |||
| Rivastigmine hydrochloride | Capmul MCM | Tween 80:Transcutol P (1:1; 1:2; 2:1; 3:1; 4:1; 5:1) | 1:9; 1:8; 1:7; 1:6; 1:5; 2:8; 1:3.5; 1:3; 3:7; 1:2; 4:6; 5:5; 6:4; 7:3; 8:2; 9:1 | Oil, drug, surfactant | Distilled water | Continuous | HPLC, UV-Vis, DLS, TEM, in vitro drug release, in vivo studies | [66] | |||
| Saquinavir | Flaxseed or safflower oil | Egg PC: deoxycholic acid | 60 °C | Oil, drug, ethanol | 10 min, 21% amplitude | Continuous | DLS, TEM, in vivo studies | [86] | |||
| Tetrabenazine | Capmul MCM | Tween 80: Transcutol P 1:0; 1:1; 1:2; 1:3; 2:1; 3:1; 4:1 v/v | 1:9; 1:8; 1:7; 1:6; 1:5; 1:4; 3:7; 1:2; 4:6; 5:5; 6:4; 7:3; 8:2; 9:1 | 25 °C | Oil, drug, surfactant | HPLC-grade water | High speed | HPLC, UV-Vis, DLS, refractometry, ex vivo nasal permeation, in vivo studies | [63] | ||
| Topiramate | Capmul MCM C8 | 2:1 Tween 20:Carbitol | Oil, surfactant, drug | Water | 100 rpm | 30 min | DLS, TEM, in vivo studies | [87] | |||
| Valproic acid | MCT: safflower seed oil (1:3 w/w) | Tween 80 | 60 °C | Oil, drug, 1% w/w lecithin | 24 kHz, 240 W | Yes | 15 min | DLS, TEM | [88] |
| Compound | PP | Solvent | Molar Ratio (E: PP) | T | Chol | Ultrasound | Rotation | Time | Rehydration Film | Analysis | Ref |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Natural compounds | |||||||||||
| 7,8-dihydroxy-flavone | Soybean PC | Absolute EtOH | 1:40, 1:30, 1:15, 1:10, 1:5 w/w | 25 °C | 5:1 PC:Chol | 40 kHz, 5 min, 10 s on/off | Yes | 30 min | PBS pH 7.4 | DLS, UPLC, TEM, FTIR, DSC, DPPH, in vitro drug release | [96] |
| β-carotene | Marine PP or egg PC | 5 mL absolute EtOH | 0.01, 0.02, 0.03, 0.04 g to 1g PP | 55 °C | 9 min 240 W 8 s on/off | Yes | 60 min | 100 mL PBS pH 7.4 | DLS, TEM, DSC, UV-Vis | [97] | |
| Baicalein | DPPC | Chloroform for DPPC, MetOH for baicalein | 1:3 1:5 1:10 | 37 °C | 15% Chol, 10% PEG2000 PE | 30 s | 150 rpm | 2 h | PBS pH 7.4 | TEM, DLS, UV-Vis, HPLC, DSC, DPPH, CLSM, cellular uptake | [98] |
| Basic fibroblast growth factor | Hydrogenated soy PC | 1 mL Poloxamer 188-grafted heparin copolymer 5% w/v | 5 °C | 110 W, 20 s | 2500 rpm | 5 h | Double distilled water | TEM, DLS, viscometry, ELISA, UV-Vis, in vivo studies | [99] | ||
| Curcumin | Soy, rapeseed, salmon lecithin | 48.5 mL distilled water | 10 mg curcumin to 1.5 g lecithin | 40 kHz 40% full power, 120 s, 1 s on/off | Yes | 5 h | DLS, HPLC, TEM, in vitro anticancer activity evaluation | [100] | |||
| Curcumin | DPPC | Chloroform: MetOH (2:1 v/v) | 1:5 | 45 °C | 2:1 PP:Chol | Yes | PBS pH 7.4 | DLS, FCM, in vivo studies, brain cell studies | [101] | ||
| Curcumin | DSPC | Chloroform: MetOH (2:1 v/v) | (0.375–0.75):2:1 E:PP:Chol | 60 °C | Yes | Yes | Yes | 1 h | PBS pH7.4 or FITC-dextran | DLS, post mortem brain tests, cellular uptake | [102] |
| Cytarabine | Lipoid E80 | EtOH | Room T | Yes | 700 rpm | 15 min | PCS, HPLC, TEM, in vitro drug release, stability and cell uptake, CLSM | [103] | |||
| Docosa-hexaenoic, eicosa-pentaenoic acid (2:3) w/w | Soybean PP | Deionized water and glycerol (2% v/v) | 0.4:2 | 30 °C | 20 kHz 120 W (10, 15, 20 min) | 600, 800, 1000 rpm | 30, 45, 60 min | DLS, GC | [104] | ||
| Galantamine | DSPC, DSPE | Chloroform: MetOH (9:1 v/v) | 65 °C | Yes | Probe sonicator | 60 rpm | 30 s | PBS pH 7.4 or 5% w/v dextrose | FTIR, UV-Vis, DSC, DLS, TEM, in vitro drug release | [105] | |
| Lutein | Lecithin | Absolute ethanol | 1:10:40:10 lutein, chol, Tween 80, lecithin | 50 °C | Yes | 30 min | HPLC, DLS, TEM, FTIR, in vitro drug release, antioxidant activity | [106] | |||
| OX-26 or IgG | PC, DSPC | 37 °C for PC, 53 °C for DSPC | 20:10:0.8: (0.002–0.02) DSPC:Chol:DSPE-PEG2000:DSPE-PEG2000-Biotin | Probe sonication | 1 h | Excess solution of biotin-OX-26 or biotin-IgG | ELISA, DLS, cellular uptake, TEM, CLSM | [107] | |||
| Quercetin, rosmarinic acid | PA, DPPC, DHDP | MeOH for quercetin, chloroform for PP, PBS for RA | 25 °C | 5:4:1 DPPC:Chol:DHDP | 46 kHz | 50 min | 1 mL aqueous solution containing RA | HPLC, ELISA, DLS, SEM, TEM, XPS, in vivo studies | [108] | ||
| Synthetic compounds | |||||||||||
| Beclometha-sone dipropionate | Lipoid E80 | EtOH | Room T | Yes | 700 rpm | 15 min | PCS, HPLC, TEM, in vitro drug release, stability and cell uptake, CLSM | [103] | |||
| Cisplatin | Soy PC | Silver nitrate for cisplatin, chloroform: diethyl ether (3:1 v/v) for PP | (9:1:1.5 mg) PC, PE-PEG, QCS-modified PP | 25 °C | Yes | 5 mL PBS pH 7.4 and aqueous cisplatin (100 μg/ 1 mg lipid) | AAS, AFM, DLS, in vitro drug release, cellular uptake | [109] | |||
| Flucytosine | Soybean PC | Chloroform: MetOH 3:2 v/v | 1:1:1:(0, 0.25, 0.5 or 0.75) PC: Chol: Span 65: Glutathione | Ultrasonic bath 30 min | 90 rpm | 1 h | 15 mL aqueous solution of flucytosine in PBS pH 7.4 | UV-VIS, DLS, TEM, in vitro drug release, cellular uptake, in vivo studies | [110] | ||
| Lamotrigine | Lipoid 90G | Chloroform: MetOH (2:1 v/v) | Various | 35 °C | Yes | Yes | Yes | 1 h | Tween 80, nasal saline buffer pH 6.5 | PCS, UV-Vis, TEM, DSC, XRD, in vitro drug release, CLSM | [111] |
| Metmorfin Hydrochloride | PS | Pure EtOH | 50 °C | 2 min mild frequency | 800 rpm | Distilled water | DLS, TEM, UV-Vis, in vivo studies | [112] | |||
| Phosphatidic acid, cardiolipin | Bovine brain sphingomyelin | Chloroform: MetOH (2:1 v/v) | 5% either extract | 55 °C | 1:1 molar ratio Chol:PP mixed with 2.5% mal-PEG-PE | 3 h | PBS | DLS, CLSM, cellular uptake | [113] | ||
| Quetiapin fumarate | Egg PC | 10 mL MetOH: chloroform 2:1 | 1:1; 1:2; 1:3 | 37 ºC | 1:1; 1:2; 1:3 Chol:PC | 2 min 80% amplitude | 90 rpm | 2 h | 10 mL nasal saline buffer pH 6.8 | FTIR, SEM, TEM, DLS, ex vivo drug diffusion, in vitro drug release, in vivo studies | [114] |
| Tempamine | Egg PC or HSPC | Tert-butanol for lipids, 70% EtOH for drug | 54:41:5 PP:Chol: 2000PEG-DSPE | 60 ºC for HPSC, room T for egg PC | 250 mM ammonium sulfate | EPR, in vivo studies | [115] | ||||
| Teriflunomide | Lipoid S100 | 10 mL chloroform: MetOH(95:5 v/v) | 5, 7.5 or 10 mg drug to 75, 100 or 125 mg PP | Yes | 70% amplitude 2–5 min | Yes | PBS pH 7.4 | DLS, TEM, SEM, DSC, PXRD, UV-Vis, in vitro drug release, in vivo studies | [116] | ||
| Extracts/Compounds | PP | Solvent | Molar Ratio (E: PP) | T | Chol | Ultrasound | Rotation | Time | Rehydration Film | Analysis | References |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Plant extracts | |||||||||||
| Annona muricata L. aqueous extract | PC | 3 mL THF | 1:4 | 75 °C | 32.5% | 15 min | Yes | 4 h | PBS | DLS, HPLC-DAD, FLS, MAO-A inhibition | [150] |
| Moringa oleifera Lam. aqueous extract | Soy lecithin | 10 mL DCM | Various | Room T | Yes | 60% amplitude for 15 min, 15 s on/30 s off | Yes | 3 h | 10 mL n-hexane | DLS, LC-MS, TEM | [169] |
| Persimmon | PC | 20 mL EtOH | 1:1; 1:2 | 25 °C | 300 rpm | 2 h | 40 mL 2% acetic acid solution | HPLC, DPPH, DLS, Folin-ciocalteu, UV-Vis, UHPLC-DAD, in vivo studies | [153] | ||
| Plectranthus madagasca-riensis (Pers.) Benth.acetonic extract | PC | 20 mL acetone, DCM or EtOH | 1:1 | 50 °C | 0, 2.5 or 5% | Yes | 1, 2 or 4 h | 40 mL reverse osmosis water | HPLC-DAD, SEM, DLS | [166] | |
| Standardized Bacopa monnieri (L.) Wettst. extract | Phospholipon ®90H | 40 mL EtOH | 1:0.5; 1:1; 1:1.75; 1:2.5; 1:3 | 40, 44, 50, 56, 60 °C | Continuous at rehydration | 1, 1.4, 2, 2.6, 3 h | n-hexane | HPLC, Phm, SEM, DLS, FTIR, DSC, TGA, PXRD, in vitro drug release, ex vivo permeation, in vivo studies | [167] | ||
| Standardized Centella asiatica extract | Phospholipon ®90H | 40 mL EtOH | 1:0.5; 1:1.01; 1:1.75; 1:2.49; 1:3 | 40, 44, 50 56, 60 °C | Continuous at rehydration | 1; 1,4; 2; 2,6; 3 h | n-hexane | HPLC, Phm, SEM, PCS, FTIR, DSC, PXRD, in vitro drug release, in vivo studies | [152] | ||
| Natural compounds | |||||||||||
| Apigenin | Phospholipon 90H (Hydrogenated soy PC) | 1,4-dioxane: MetOH (14:6) | 1:1; 1:2; 1:3 | 40, 50, 60 °C | 2 h | 100 mL n-hexane | UV-Vis, DLS, DSC, FTIR, H-NMR, PXRD, in vitro drug release, in vivo studies | [149] | |||
| Catechin | PC | DCM | 1:1 | 3 h | 30 mL n-hexane | UV-Vis, SEM, FTIR, DSC, PXRD, H-NMR, DPPH | [148] | ||||
| Celastrol | Soy PC | Anhydrous EtOH | 1:1; 1:2; 1:3 | 40 °C | Brief (2 min) | 100 rpm | 3 h | 6 mL deionized water | UV-Vis, FTIR, DSC, PXRD, DLS, TEM, in vitro drug release, in vivo studies | [138] | |
| Chrysin | Soy or egg PC | 12.5 mL THF | 1:2; 1:3 | 40 °C | Yes | 4 h | 12 mL distilled water | DLS, HPLC, AFM, FTIR, XRD, SEM, in vitro drug release | [170] | ||
| Curcumin | Hydrogenated soy PC | 20 mL DCM | 1:1 | ≤60 °C | 2 h | 10 mL n-hexane | HPLC, DSC, HPTLC, in vivo studies | [159] | |||
| Curcumin | PC | 30 mL DCM | 1:1; 1:2; 1:4 | 40 °C | Yes | 2 h | 50 mL n-hexane | SEM, TEM, HPLC, DSC, H-NMR, FTIR, PCS, in vivo studies | [160] | ||
| Embelin | Phospholipon ®90H | 250 mL EtOH | 1:0.5; 1:1; 1:2; 1:3 | ≤60 °C | 2 h | UHPLC, UV-Vis, DSC, FTIR, PXRD, H-NMR, in vitro drug release | [147] | ||||
| Hesperidin | Soy lecithin | 40 mL DCM | 1:0.5; 1:1; 1:2; 1:3 | ≤60 °C | 2 h | UV-Vis, DSC, SEM, in vitro drug release | [164] | ||||
| Quercetin | PC | MetOH: Chloroform (1:1 v/v) | 1:2 | 45 °C | 2:0.2 PC:Chol | Probe sonicator for 5 min | 80 rpm | Glucose 50% solution | TEM, DLS, UV-Vis, DPPH | [151] | |
| Rutin | PC | Absolute EtOH | 1:1; 1:2; 1:3 | 45 °C | 30 min | 5 mL distilled water | DLS, SEM, UV-Vis, FRAP, FTIR, HPLC | [156] | |||
| Rutin | Soy PC | MetOH: Chloroform (1:4) | 1:1; 1:2; 1:4 | 45 °C | Yes | Distilled water | DLS, DSC, FTIR, UV-Vis | [158] | |||
| Rutin | PC | 20 mL DCM | 1:1 | 45–50°C | 100 mL n-hexane | HPLC, FTIR, DSC, PXRD, SEM, DPPH, in vitro drug release | [171] | ||||
| Silymarin | Soy and egg yolk lecithin | 100 mL MetOH | 1:0.25; 1:0.5; 1:1; 1:2 | Room T | Yes | 300 mL petroleum ether | SEM, TEM, H-NMR, DSC, FTIR, HPLC, in vivo studies | [155] | |||
| Silymarin | Soy PC | 20 mL absolute EtOH | 1:5; 1:10; 1:15 | 25 °C | 4min, 5 s on/off, 60% amplitude | 180 rpm | 2 h | PBS, pH 7.4 | UV-Vis, FTIR, DSC, TEM, DLS | [172] |
| Compound | Lipids | Solvent | T | Oil Phase | Aqueous Phase | Ultrasound | Rotation | Time | Analysis | Ref |
|---|---|---|---|---|---|---|---|---|---|---|
| Natural compounds | ||||||||||
| Andrographolide | Compritol 888 ATO | 5 mL acetone for lipids | 50 °C oil phase, 75 °C aqueous phase | Drug, lipids, fluorescein isothiocyanate | 30 mL water, Brij 78 | Continuous | DLS, TEM, DSC, HPLC-DAD, HPLC-FLD, in vitro drug release, in vivostudies | [45] | ||
| BACE1 siRNA | 200 mg Witepsol E 85 solid triglycerides | 2 mL DCM for lipids | Room T | Drug, lipids, RVG-9R (to increase intracellular pathway), 10 mL polyvinyl alcohol (2% w/v) | Chitosan (1% w/v), water containing 1% v/v acetic acid and PVA (2% w/v) | 30 s 70% amplitude | Yes | DLS, SEM, FMPR | [190] | |
| Camptothecin | 5 or 15% Cetyl palmitate, Dynasan 114 or Witepsol E85 | 5–10 °C above lipid melting point | Drug, lipid | Water, 0.8 or 2% surfactant (Polysorbate 20, 40, 60 and 80) | Yes | PCS, DSC, HPLC, in vitro drug release, in vivo studies | [188] | |||
| Curcumin | Compritol 888 ATO (7.27%) | 82–85 °C | Lipid | Water, polysorbate 80 (45.45%), soy lecithin (0.58%), drug | 5000 rpm | 1.5h | CLSM, in vivo studies | [46] | ||
| Lutein | Fish oil, corn oil | 85 °C | Fish oil, glycerol stearate, carnauba wax, corn oil, drug | Water, 4% surfactant mixture of Tween 80/ lecithin/ block copolymer | 25,000 rpm | 10 min | DLS, TEM, UV-Vis, DSC, antioxidant activity, in vitro drug release | [186] | ||
| Noscapine | Stearic acid (0.70 mM), egg PC (0.14 mM) | 70 °C | Drug, lipids, sodium glycocholate (0.69 mM) | Distilled water (111.10 mM) | Yes | DLS, TEM, AFM, UV-Vis, FTIR, DSC, PXRD, in vitro drug release, in vivo studies | [191] | |||
| Resveratrol | Compritol 888 ATO | EtOH: Chloroform (20:80% v/v) | Drug, 5 mL lipids | 20 mL aqueous solution 3% w/v Tween 80 or 2.5% Tween 80 and 0.5% w/v polyvinyl alcohol | Probe sonicator | 15,000 rpm | DLS, FTIR, XRD, SEM, UV-Vis, in vitro drug release, in vivo studies | [192] | ||
| Synthetic compounds | ||||||||||
| Docetaxel | Soy lecithin, monostearin | 3 mL chloroform | 10 mg drug, 40 mg lecithin, 100 mg monostearin, 40 mg vitamin E | 10 mL deionized water, 150 mg tween 80 | 15 min | 11,000 rpm 3 min | 3 h with stirring | XPS, PCS, HPLC, PXRD, in vitro drug release, cytotoxicity, in vivo studies | [193] | |
| Haloperidol | Glyceryl monostearate, Compritol ATO 888, precirol ATO 5, stearic acid or palmitic acid | 2.5 mL chloroform: EtOH 1:1 v/v | 43.75–50 mg Drug, 87.5–100 mg lipid | 22.5 mL aqueous solution of Tween 80 (1.5–1.625% w/v) | 5 min 100% amplitude | 3000 rpm | 30 min | PCS, TEM, UV-Vis, XRD, DSC, HPLC, in vitro drug release, in vivo studies | [182] | |
| Levofloxacin-Doxycycline | Compritol 888 ATO 2.5–4.5%, stearic acid 1–2% | Drug, lipids, 1.75–2.5% Span 60 (emulsifier) | Distilled water, 0.5% Pluronic F127 (emulsifier) | 10 cycles 1 min on/off | 24,000 rpm | DLS, in vitro drug release, UV-Vis, TEM, FTIR, DSC, CLSM, ex vivonasal permeation, HPLC, in vivo studies | [183] | |||
| Lipophilic Kiteplatin Pt(IV) Prodrugs (SMF 111, 196, 200, 144) | Cetyl palmitate (lipid matrix), 16:0 PEG-2-PE (surface-modifier) | 1 mL chloroform | 65 °C | Drug, lipids | 3 mL ultrapure water, Tween 80 3% p/V (surface modifier) | Probe-tip 0.27 W | Gently stirred | 15 min | H-NMR, AAS, in vitro drug release, FLM, UV-Vis, DLS, TEM | [194] |
| Compounds/ Extracts | Lipids | Solvent | T | Oil Phase | Aqueous Phase | Ultrasound | Rotation | Time | Analysis | Ref |
|---|---|---|---|---|---|---|---|---|---|---|
| Seaweed extract | ||||||||||
| Sargassum longifolium (Turner) C.Agardh | Lecithin, stearic acid, orange oil | EtOH: acetone (40:60 v/v) | 72–75 °C | Lipids | 1% w/v Poloxamer 188 | Yes | DLS, SEM, TEM, FTIR, UV-Vis, in vitro drug release, cytotoxicity | [71] | ||
| Natural compounds | ||||||||||
| Astaxanthin | Glyceryl behenate as solid lipid, oleic acid as liquid lipid | PBS for Tween 80 | 78 °C | Lipids, drug, lecithin | Tween 80, PBS | 15 min at 25 °C; 4 min 2 s on/ off | 2000 rpm | 3 min | PCS, UV-Vis, XRD, DSC | [185] |
| Baicalin, Salvianolic acid B | Lecithin, Compritol 888 ATO | EtOH for drug and lecithin, chloroform for compritol 888 ATO, mPEG-MAL, mPEG-OH and MCT 812 | 75 °C | Drug, lipids, mPEG-MAL, mPEG-OH, MCT 812 | Myrj 52 dissolved in deionized water | Yes | 2 h | PCS, HPLC, in vitro drug release, UPLC, in vivo studies | [195] | |
| Resveratrol | Cetyl palmitate, Capmul MCM | 5 °C above solid lipid melting point | Drug, lipids, Acrysol K150 | Distilled water, Poloxamer 188, Tween 80 | Probe 2 min 30% amplitude, 3s on, 2 off | Yes | 2 min | DLS, HPLC, TEM, DSC, FTIR, in vivo studies | [196] | |
| Synthetic compounds | ||||||||||
| Almotriptan maleate | Compritol 888 ATO, Precirol ATO 5 or stearic acid as solid lipid, Labrafil M2125CS as liquid lipid | 77 °C | Drug, lipids | Water, Tween 80: (Lauroglycol, Labrasol or Transcutol) 2:1 (3.5% w/v) | 15 min | Yes | 10 min | PCS, UV-Vis, DSC, in vitro drug release, ex vivo drug permeation, in vivo studies | [189] | |
| Asenapine | Glyceryl monostearate (800 mg), oleic acid (160 mg) | 70 °C | 80 mg drug, lipids | 50 mL aqueous solution 1.5% w/v Tween 80 | 5 min 60% amplitude, on/off 0.5 s | 16,000 rpm | DLS, HPLC, DSC, XRD, FTIR, TEM, AFM, in vitro drug release, in vivo studies | [197] | ||
| Carbamazepine | Trilaurin, oleic acid | DMSO for drug | 70 °C | Drug, lipids, surfactants (Tween 80, Span 80 and Poloxamer 188) | Deionized water | 800 rpm | 30 min | DLS, UV-Vis, TEM, DSC, PXRD, FTIR, HPLC, invitro drug release, in vivo studies | [198] | |
| Efavirenz | Precirol ATO 5, Captex P 500 (8:2; 7:3) | 66 °C | Drug, lipids | Deionized water, MYS-25 (1; 2% w/v) | 30 s on, 5 off, 75 or 90% amplitude | 4 min | HPLC, DLS, TEM, FTIR, DSC, PXRD, in vitro drug release, in vivo studies | [199] | ||
| Lopinavir | Compritol 888, oleic acid (60:40 to 80:20) | 80 °C | Drug, lipids | Water, Tween 80 | 50% amplitude 5 min | 1200 rpm | 15 min | DLS, UV-Vis, in vitro drug release, TEM, in vivo studies | [200] | |
| Lurasidone hydrochloride | Gelot 64, Capryol 90 | EtOH: acetone 1:1 | Drug, lipids | Distilled water, Tween 80, Transcutol P | Probe 6 min | Continuous | 2 h | PCS, UV-Vis, TEM, SEM, DSC, HPLC, in vitro drug release, in vivo studies | [201] | |
| Ondansetron hydrochloride | Glyceryl monostearate, Capryol 90, soy lecithin | 85 °C | Drug, glyceryl monostearate, capryol 90 | Poloxamer 188, soy lecithin, water | 1500 rpm | 10 min | DLS, UV-Vis, in vitro drug release, ex vivo permeation, SEM, DSC, XRD, in vivo studies | [184] | ||
| Rivastigmine | Glyceryl monostearate, Capmul MCM C8 3:2 | 1 mL EtOH | 70 °C | Drug, lipids, 0.1% stearylamine, lecithin | Double distilled water, Tween 80 | 180 W, 2 min, 4 s pulses, 3 s off | Yes | 2 h | UV-Vis, HPLC, in vivo studies | [202] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fernandes, F.; Dias-Teixeira, M.; Delerue-Matos, C.; Grosso, C. Critical Review of Lipid-Based Nanoparticles as Carriers of Neuroprotective Drugs and Extracts. Nanomaterials 2021, 11, 563. https://doi.org/10.3390/nano11030563
Fernandes F, Dias-Teixeira M, Delerue-Matos C, Grosso C. Critical Review of Lipid-Based Nanoparticles as Carriers of Neuroprotective Drugs and Extracts. Nanomaterials. 2021; 11(3):563. https://doi.org/10.3390/nano11030563
Chicago/Turabian StyleFernandes, Filipe, Mónica Dias-Teixeira, Cristina Delerue-Matos, and Clara Grosso. 2021. "Critical Review of Lipid-Based Nanoparticles as Carriers of Neuroprotective Drugs and Extracts" Nanomaterials 11, no. 3: 563. https://doi.org/10.3390/nano11030563
APA StyleFernandes, F., Dias-Teixeira, M., Delerue-Matos, C., & Grosso, C. (2021). Critical Review of Lipid-Based Nanoparticles as Carriers of Neuroprotective Drugs and Extracts. Nanomaterials, 11(3), 563. https://doi.org/10.3390/nano11030563