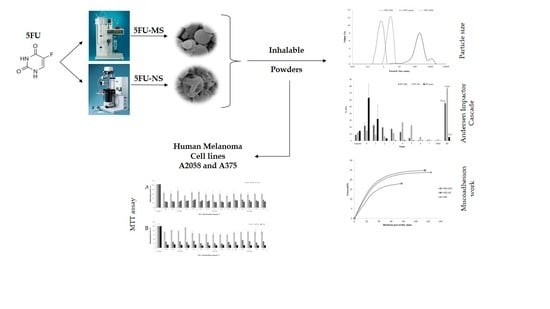
An Inhalable Powder Formulation Based on Micro- and Nanoparticles Containing 5-Fluorouracil for the Treatment of Metastatic Melanoma
Abstract
:1. Introduction
2. Results
2.1. Dry Powders: Preparation and Physicochemical Characterization
2.2. Morphological Analysis
2.3. Fourier Transformed Infrared Spectroscopy (FTIR)
2.4. In Vitro Aerodynamic Performance
2.5. In Vitro Drug Release Assay
2.6. Study of Mucoadhesive Properties In Vitro
2.6.1. Mucoadhesive Performance
2.6.2. Mucin Adsorption Capacity
2.6.3. Washability Test
2.7. Mitochondrial Activity Evaluation (MTT Assay)
3. Discussions
4. Materials and Methods
4.1. Materials
4.2. Production of Dry Powders for Lung Delivery
4.3. Physicochemical Characterization of Dry Powders
4.3.1. Mean Particle Size and Aerodynamic Diameter
4.3.2. Drug Content
4.3.3. Morphological Analysis
4.3.4. Fourier Transformed Infrared Spectroscopy (FTIR)
4.3.5. In Vitro Aerodynamic Performance
4.3.6. In Vitro Drug Release Studies
4.4. Study of Mucoadhesive Properties In Vitro
4.4.1. Mucoadhesive Performance
4.4.2. Adsorption of Mucin
4.4.3. Washability Assay
4.5. Mitochondrial Activity Evaluation (MTT Assay)
4.6. Statistical Analysis
5. Conclusions
Supplementary Materials
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Melanoma Institute Australia 2017. Available online: https://www.melanoma.org.au/understanding-melanoma/stages-of-melanoma (accessed on 13 March 2017).
- Bhatia, S.; Tykodi, S.S.; Thompson, J.A. Treatment of Metastatic Melanoma: An Overview. Oncology 2009, 23, 488–496. [Google Scholar] [PubMed]
- Instituto Nacional de Câncer. Available online: http://www2.inca.gov.br/wps/wcm/connect/tiposdecancer/site/home/pele_melanoma/definicao+ (accessed on 17 July 2017).
- Wolff, K.; Johnson, R. Fitzpatrick’s Color Atlas and Synopsis of Clinical Dermatology, 6th ed.; McGraw Hill: New York, NY, USA, 2009; ISBN 978-0-07-163342-0. [Google Scholar]
- Yang, S.; Haluska, F.G. Treatment of melanoma with 5-Fluorouracil or dacarbazine in vitro sensitizes cells to antigen-specific CTL Lysis through perforin/granzyme- and Fas-mediated pathways. J. Immunol. 2004, 172, 4599–4608. [Google Scholar] [CrossRef] [PubMed]
- Garbe, C.; Peris, K.; Hauschild, A.; Saiag, P.; Middleton, M.; Spatz, A.; Grob, J.-J.; Malvehy, J.; Newton-Bishop, J.; Stratigos, A.; et al. Diagnosis and treatment of melanoma: European consensus-based interdisciplinary guideline. Eur. J. Cancer 2010, 46, 270–283. [Google Scholar] [CrossRef] [PubMed]
- Singh, B.N.; Singh, R.B.; Singh, J. Effects of ionization and penetration enhancers on the transdermal delivery of 5-fluorouracil through excised human stratum corneum. Int. J. Pharm. 2005, 298, 98–107. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Lin, J.; Zhang, X.; Liu, Q.; Xu, Q.; Tan, R.X.; Guo, Z. 5-Fluorouracil-cisplatin adducts with potential antitumor activity. J. Inorg. Biochem. 2003, 94, 186–192. [Google Scholar] [CrossRef]
- Gudasi, K.B.; Vadavi, R.S.; Shelke, N.B.; Sairam, M.; Aminahbavi, T.M. Synthesis and characterization of novel polyorganophosphazenes substituted with 4-methoxybenzylamine and 4-methoxyphenethylamine for in vitro release of indomethacin and 5-fluorouracil. React. Funct. Polym. 2006, 66, 1149–1157. [Google Scholar] [CrossRef]
- Rejinold, N.S.; Muthunarayanan, M.; Chennazhi, K.P.; Nair, S.V.; Jayakumar, R. 5-fluorouracil loaded fibrinogen nanoparticles for cancer drug delivery applications. Int. J. Biol. Macromol. 2011, 48, 98–105. [Google Scholar] [CrossRef] [PubMed]
- Malet-Martino, M.; Martino, R. Clinical Studies of Three Oral Prodrugs of 5-Fluorouracil (Capecitabine, UFT, S-1): A Review. Oncologist 2002, 7, 288–323. [Google Scholar] [CrossRef] [PubMed]
- Grem, J.L. 5-Fluorouracil: Forty-plus and still ticking. A review of its preclinical and clinical development. Investig. New Drugs 2000, 18, 299–313. [Google Scholar] [CrossRef]
- Longley, D.B.; Harkin, D.P.; Johnston, P.G. 5-fluorouracil: Mechanisms of action and clinical strategies. Nat. Rev. Cancer 2003, 3, 330–338. [Google Scholar] [CrossRef] [PubMed]
- Senft, D.; Berking, C.; Graf, S.A.; Kammerbauer, C.; Ruzicka, T.; Besch, R. Selective induction of cell death in melanoma cell lines through targeting of Mcl-1 and A1. PLoS ONE 2012, 7, e30821. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shenoy, V.S.; Gude, R.P.; Murthy, R.S.R. In vitro anticancer evaluation of 5-fluorouracil lipid nanoparticles using B16F10 melanoma cell lines. Int. Nano Lett. 2013, 36, 3–9. [Google Scholar] [CrossRef]
- Di Paolo, A.; Danesi, R.; Falcone, A.; Cionini, L.; Vannozzi, F.; Masi, G. Relationship between 5-fluorouracil disposition, toxicity and dihydropyrimidine dehydrogenase activity in cancer patients. Ann. Oncol. 2001, 12, 1301–1306. [Google Scholar] [CrossRef] [PubMed]
- Thomas, A.M.; Kapanen, A.I.; Hare, J.I.; Ramsay, E.; Edwards, K.; Karlsson, G.; Bally, M.B. Development of a liposomal nanoparticle formulation of 5-fluorouracil for parenteral administration: Formulation design, pharmacokinetics and efficacy. J. Control. Release 2011, 150, 212–219. [Google Scholar] [CrossRef] [PubMed]
- Kaiser, N.; Kimpfler, A.; Massing, U.; Burger, A.M.; Fiebig, H.H.; Brandl, M.; Schubert, R. 5-Fluorouracil in vesicular phospholipid gels for anticancer treatment: Entrapment and release properties. Int. J. Pharm. 2003, 256, 123–131. [Google Scholar] [CrossRef]
- Lamprecht, A.; Yamamoto, H.; Takeuchi, H.; Kawashima, Y. Microsphere design for the colonic delivery of 5-fluorouracil. J. Control. Release 2003, 90, 313–322. [Google Scholar] [CrossRef]
- Huang, L.; Sui, W.; Wang, Y.; Jiao, Q. Preparation of chitosan/chondroitin sulfate complex microcapsules and application in controlled release of 5-fluorouracil. Carbohydr. Polym. 2010, 80, 168–173. [Google Scholar] [CrossRef]
- Lu, F.; Lei, L.; Shen, Y.Y.; Hou, J.W.; Chen, W.L.; Li, Y.G.; Guo, S.R. Effects of amphiphilic PCL–PEG–PCL copolymer addition on 5-fluorouracil release from biodegradable PCL films for stent application. Int. J. Pharm. 2011, 419, 77–84. [Google Scholar] [CrossRef] [PubMed]
- Zhang, C.; Li, G.; Wang, Y.; Gui, F.; Zhang, J.; Huang, Q. Preparation and characterization of 5-fluorouracil-loaded PLLA–PEG/PEG nanoparticles by a novel supercritical CO2 technique. Int. J. Pharm. 2012, 436, 272–281. [Google Scholar] [CrossRef] [PubMed]
- Peters, G.J.; Lankelma, J.; Kok, R.M.; Noordhuis, P.; van Groeningen, C.J.; van der Wilt, C.L.; Meyer, S.; Pinedo, H.M. Prolonged retention of high concentrations of 5-fluorouracil in human and murine tumors as compared with plasma. Cancer Chemother. Pharmacol. 1993, 31, 269–276. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, F.; Fukuse, T.; Wada, H.; Fukushima, M. The history, mechanism and clinical use of oral 5-fluorouracil derivative chemotherapeutic agents. Curr. Pharm. Biotechnol. 2000, 1, 137–164. [Google Scholar] [CrossRef] [PubMed]
- Shah, N.D.; Shah, V.V.; Chivate, N.D. Pulmonary Drug Delivery: A Promising Approach. J. Appl. Pharm. Sci. 2012, 2, 33–37. [Google Scholar]
- Al-Qadi, S.; Grenha, A.; Carrion-Recio, D.; Seijo, B.; Remunan-Lopez, C. Microencapsulated chitosan nanoparticles for pulmonary protein delivery: In vivo evaluation of insulin-loaded formulations. J. Control. Release 2012, 157, 383–390. [Google Scholar] [CrossRef] [PubMed]
- Beck-Broichsitter, M.; Schweiger, C.; Schmehl, T.; Gessler, T.; Seeger, W.; Kissel, T. Characterization of novel spray-dried polymeric particles for controlled pulmonary drug delivery. J. Control. Release 2012, 158, 329–335. [Google Scholar] [CrossRef] [PubMed]
- Nangrejo, M.; Ahmad, Z.; Stride, E.; Edirisinghe, M. Preparation of Polymeric and Ceramic Porous Capsules by a Novel Electrohydrodynamic Process. Pharm. Dev. Technol. 2008, 13, 425–432. [Google Scholar] [CrossRef] [PubMed]
- Zhang, C.; Yao, Z.-C.; Ding, Q.; Choi, J.J.; Ahmad, Z.; Chang, M.-W.; Li, J.-S. Tri-Needle Coaxial Electrospray Engineering of Magnetic Polymer Yolk−Shell Particles Possessing Dual-Imaging Modality, Multiagent Compartments, and Trigger Release Potential. ACS Appl. Mater. Interfaces 2017, 9, 21485–21495. [Google Scholar] [CrossRef] [PubMed]
- Raseck, M.; Ahmad, Z.; Cross, R.B.M.; Gil, J.H.; Wilton-Ely, J.D.E.T.; Miller, P.W. Facile Preparation of Drug-Loaded Tristearin Encapsulated Superparamagnetic Iron Oxide Nanoparticles using Coaxial Electrospray Processing. Mol. Pharm. 2017, 14, 2010–2023. [Google Scholar]
- Ungaro, F.; d’Angelo, I.; Coletta, C.; d’Emmanuele, D.V.; Sorrentino, R.; Perfetto, B.; Tufano, M.A.; Miro, A.; La Rotonda, M.I.; Quaglia, F. Dry powders based on PLGA nanoparticles for pulmonary delivery of antibiotics: Modulation of encapsulation efficiency, release rate and lung deposition pattern by hydrophilic polymers. J. Control. Release 2012, 157, 149–159. [Google Scholar] [CrossRef] [PubMed]
- Seville, P.C.; Li, H.; Learoyd, T.P. Spray-Dried Powders for Pulmonary Drug Delivery. Crit. Rev. Ther. Drug Carr. Syst. 2007, 24, 307–360. [Google Scholar] [CrossRef]
- Chow, A.H.; Tong, H.H.; Chattopadhyay, P.; Shekunov, B.Y. Particle engineering for pulmonary drug delivery. Pharm. Res. 2007, 24, 411–437. [Google Scholar] [CrossRef] [PubMed]
- Dutta, R.C. Drug carriers in pharmaceutical design: Promises and progress. Curr. Pharm. Des. 2007, 13, 761–769. [Google Scholar] [CrossRef] [PubMed]
- Baghirov, H.; Karaman, D.; Viitala, T.; Duchanoy, A.; Lou, Y.; Mamaeva, V.; Pryazhnikov, E.; Khiroug, L.; Davies, C.L.; Sahlgren, C.; et al. Feasibility Study of the Permeability and Uptake of Mesoporous Silica Nanoparticles across the Blood-Brain Barrier. PLoS ONE 2016. [Google Scholar] [CrossRef] [PubMed]
- Volpi, N.; Maccari, F. Electrophoretic approaches to the analysis of complex polysaccharides. J. Chromatogr. B Anal. Technol. Biomed. 2006, 834, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Lee, E.S.; Park, K.H.; Kang, D.; Park, I.S.; Min, H.Y.; Lee, D.H.; Kim, S.; Kim, J.H.; Na, K. Protein complexed with chondroitin sulfate in poly (lactide-co-glycolide) microspheres. Biomaterials 2007, 28, 2754–2762. [Google Scholar] [CrossRef] [PubMed]
- Zou, X.H.; Jiang, Y.Z.; Zhang, G.R.; Jin, H.M.; Nguyen, T.M.; Ouyang, H.W. Specific interactions between human fibroblasts and particular chondroitin sulfate molecules for wound healing. Acta Biomater. 2009, 5, 1588–1595. [Google Scholar] [CrossRef] [PubMed]
- Uchida, S.; Itaka, K.; Chen, Q.; Osada, K.; Miyata, K.; Ishii, T.; Harada-Shiba, M.; Kataoka, K. Combination of chondroitin sulfate and polyplex micelles from Poly(ethylene glycol)-poly{N′-[N-(2-aminoethyl)-2-aminoethyl]aspartamide} block copolymer for prolonged in vivo gene transfection with reduced toxicity. J. Control. Release 2011, 155, 296–302. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.S.; Imai, T.; Suenaga, A.; Otagiri, M. Molecular-weight-dependent pharmacokinetics and cytotoxic properties of cisplatin complexes prepared with chondroitin sulfate A and C. Int. J. Pharm. 2002, 240, 23–31. [Google Scholar] [CrossRef]
- De Mariscal, P.; Bell, D.A. Fiber-based fat mimics methylcellulose gums. In Handbook of Fat Replacers; Roller, S., Jones, S.A., Eds.; CRC Press: Boca Raton, FL, USA, 1996; pp. 145–159. [Google Scholar]
- Alpar, H.O.; Somavarapu, S.; Atuah, K.N.; Bramwell, V.W. Biodegradable mucoadhesive particulates for nasal and pulmonary antigen and DNA delivery. Adv. Drug Deliv. Rev. 2005, 57, 411–430. [Google Scholar] [CrossRef] [PubMed]
- Banerji, B.; Pramanik, S.K.; Mandal, S.; Maiti, N.C.; Chaudhuri, K. Synthesis, characterization and cytotoxicity study of magnetic (Fe3O4) nanoparticles and their drug conjugate. RSC Adv. 2012, 2, 2493–2497. [Google Scholar] [CrossRef]
- Lee, S.-T.; Mi, F.-L.; Shen, Y.-J.; Shyu, S.-S. Equilibrium and kinetic studies of copper (II) ion uptake by chitosan-tripolyphosphate chelating resin. Polymer 2001, 42, 1879–1892. [Google Scholar] [CrossRef]
- Foot, M.; Mulholland, M. Classification of chondroitin sulfate A, chondroitin sulfate C, glucosamine hydrochloride and glucosamine 6 sulfate using chemometric techniques. J. Pharm. Biomed. Anal. 2005, 38, 397–407. [Google Scholar] [CrossRef] [PubMed]
- Meenach, S.A.; Anderson, K.W.; Hilt, Z.; McGarry, R.C.; Mansour, H.M. Characterization and aerosol dispersion performance of advanced spray-dried chemotherapeutic PEGylated phospholipid particles for dry powder inhalation delivery in lung cancer. Eur. J. Pharm. Sci. 2013, 49, 699–711. [Google Scholar] [CrossRef] [PubMed]
- Carvalho, T.C.; Peters, J.I.; Williams, R.O., III. Influence of particle size on regional lung deposition—What evidence is there? Int. J. Pharm. 2011, 406, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Anton, N.; Arpagaus, C.; Belleteix, F.; Vandamme, T.F. Nanoparticles by spray drying using innovative new technology: The Buchi nano spray dryer B-90. J. Control. Release 2010, 147, 304–310. [Google Scholar] [CrossRef] [PubMed]
- Schafroth, N.; Arpagaus, C.; Jadhav, U.Y.; Makne, S.; Douroumis, D. Nano and microparticle engineering of water insoluble drugs using a novel spray-drying process. Colloids Surf. B Biointerfaces 2012, 90, 8–15. [Google Scholar] [CrossRef] [PubMed]
- Foster, T.P.; Laetherman, M.W. Powder characteristics of proteins spray-dried from different spray-dryers. Drug Dev. Ind. Pharm. 1995, 21, 1705–1723. [Google Scholar] [CrossRef]
- Maa, Y.F.; Costantino, H.R.; Nguyen, P.A.; Hsu, C.C. The effect of operating and formulation variables on the morphology of spray-dried protein particles. Pharm. Dev. Technol. 1997, 2, 213–223. [Google Scholar] [CrossRef] [PubMed]
- Walton, D.E.; Mumford, C.J. Spray dried productsð characterization of particle morphology. Trans. IChemE 1999, 77, 21–37. [Google Scholar] [CrossRef]
- Raffin, R.P.; Colome, L.M.; Haas, S.E.; Jornada, D.S.; Pohlmann, A.R.; Guterres, S.S. Development of HPMC and Eudragit S100 blended microparticles containing sodium pantoprazole. Pharmazie 2007, 62, 361–364. [Google Scholar] [PubMed]
- Brannon-Peppas, L.; Peppas, N.A. Dynamic and equilibrium swelling behaviour of pH-sensitive hydrogels containing 2-hydroxyethyl methacrylate. Biomaterials 1990, 11, 635–644. [Google Scholar] [CrossRef]
- McCarron, P.A.; Donnelly, R.F.; Zawislak, A.; Woolfson, A.D.; Price, J.H.; Mcclelland, R. Evaluation of a water-soluble bioadhesive patch for photodynamic therapy of vulval lesions. Int. J. Pharm. 2005, 293, 11–23. [Google Scholar] [CrossRef] [PubMed]
- Bruschi, M.L. Strategies to Modify the Drug Release from Pharmaceutical Systems; Woodhead Publishing: Cambridge, UK, 2015; p. 208. [Google Scholar]
- Newman, S.P.; Sutton, D.J.; Segarra, R.; Lamarca, R.; De Miquel, G. Lung deposition of aclidinium bromide from Genuair, a multidose dry powder inhaler. Respiration 2009, 78, 322–328. [Google Scholar] [CrossRef] [PubMed]
- Chrystyn, H. Is total particle dose more important than particle distribution? Respir. Med. 1997, 91 (Suppl. A), 17–19. [Google Scholar] [CrossRef]
- Brand, P.; Meyer, T.; Weuthen, T.; Timmer, W.; Berkel, E.; Wallenstein, G.; Scheuch, G. Lung deposition of radiolabeled tiotropium in healthy subjects and patients with chronic obstructive pulmonary disease. J. Clin. Pharmacol. 2007, 47, 1335–1341. [Google Scholar] [CrossRef] [PubMed]
- Kurmi, B.D.; Kayat, J.; Gajbhiye, V.; Tekade, R.K.; Jain, N.K. Micro- and nanocarrier-mediated lung targeting. Expert Opin. Drug Deliv. 2010, 7, 781–794. [Google Scholar] [CrossRef] [PubMed]
- Geller, D.E.; Weers, J.; Heuerding, S. Development of an inhaled dry-powder formulation of tobramycin using PulmoSphere technology. J. Aerosol Med. Pulm. Drug Deliv. 2011, 24, 175–182. [Google Scholar] [CrossRef] [PubMed]
- Longest, P.W.; Tian, G.; Li, X.; Son, Y.J.; Hindle, M. Performance of combination drug and hygroscopic excipient submicrometer particles from a softmist inhaler in a characteristic model of the airways. Ann. Biomed. Eng. 2012, 40, 2596–2610. [Google Scholar] [CrossRef] [PubMed]
- Son, Y.J.; Worth, L.P.; Hindle, M. Aerosolization characteristics of dry powder inhaler formulations for the excipient enhanced growth (EEG) application: Effect of spray drying process conditions on aerosol performance. Int. J. Pharm. 2013, 443, 137–145. [Google Scholar] [CrossRef] [PubMed]
- Jaques, P.A.; Kim, C.S. Measurement of total lung deposition of inhaled ultrafine particles in healthy men and women. Inhal. Toxicol. 2000, 12, 715–731. [Google Scholar] [PubMed]
- Patton, J.S.; Byron, P.R. Inhaling medicines: Delivering drugs to the body through the lungs. Nat. Rev. Drug Discov. 2007, 6, 67–74. [Google Scholar] [CrossRef] [PubMed]
- Servaty, R.; Schiller, J.; Binder, H.; Arnold, K. Hydration of polymeric components of cartilage—An infrared spectroscopic study on hyaluronic acid and chondroitin sulfate. Int. J. Biol. Macromol. 2001, 28, 121–127. [Google Scholar] [CrossRef]
- Esko, J.D.; Selleck, S.B. Order out of chaos: Assembly of ligand binding sites in heparan sulfate. Annu. Rev. Biochem. 2002, 71, 435–471. [Google Scholar] [CrossRef] [PubMed]
- Sandri, G.; Rossi, S.; Ferrari, F.; Bonferoni, M.C.; Muzzarelli, C.; Caramella, C. Assessment of chitosan derivatives as buccal and vaginal penetration enhancers. Eur. J. Pharm. 2004, 21, 351–359. [Google Scholar] [CrossRef]
- Frank, L.A.; Sandri, G.; D’Autilia, F.; Contri, R.V.; Bonferoni, M.C.; Caramella, C.; Frank, A.G.; Pohlmann, A.R.; Guterres, S.S. Chitosan gel containing polymeric nanocapsules: A new formulation for vaginal drug delivery. Int. J. Nanomed. 2014, 9, 3151–3161. [Google Scholar]
- Andrews, G.P.; Laverty, T.P.; Jones, D.S. Mucoadhesive polymeric platforms for controlled drug delivery. Eur. J. Pharm. Biopharm. 2009, 71, 505–518. [Google Scholar] [CrossRef] [PubMed]
- Carvalho, F.C.; Barbi, M.S.; Sarmento, V.H.; Chiavacci, L.A.; Netto, F.M.; Gremiao, M.P. Surfactant systems for nasal zidovudine delivery: Structural, rheological and mucoadhesive properties. J. Pharm. Pharmacol. 2010, 62, 430–439. [Google Scholar] [CrossRef] [PubMed]
- Antonow, M.B.; Asbahr, A.C.C.; Raddatz, P.; Beckenkamp, A.; Buffon, A.; Guterres, S.S.; Pohlmann, A.R. Liquid formulation containing doxorubicin-loaded lipid-core nanocapsules: Cytotoxicity in human breast cancer cell line and in vitro uptake mechanism. Mater. Sci. Eng. C 2017, 76, 374–382. [Google Scholar] [CrossRef] [PubMed]
- Frank, L.A.; Chaves, P.S.; D’Amore, C.M.; Contri, R.V.; Frank, A.G.; Beck, R.C.R.; Pohlmann, A.R.; Buffon, A.; Guterres, S.S. The use of chitosan as cationic coating or gel vehicle for polymeric nanocapsules: Increasing penetration and adhesion of imiquimod in vaginal tissue. Eur. J. Pharm. Biopharm. 2017, 114, 202–212. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, C.P.; Prado, W.A.; Lavayen, V.; Büttenbender, S.L.; Beckenkamp, A.; Martins, B.S.; Lüdtke, D.S.; Campo, L.F.; Rodembusch, F.S.; Buffon, A.; et al. Bromelain-Functionalized Multiple-Wall Lipid-Core Nanocapsules: Formulation, Chemical Structure and Antiproliferative Effect Against Human Breast Cancer Cells (MCF-7). Pharm. Res. 2017, 34, 438–452. [Google Scholar] [CrossRef] [PubMed]
- United States Pharmacopeial Convention. United States Pharmacopeia (USP), 29th ed.; United States Pharmacopeial Convention: Rockville, MD, USA, 2006. [Google Scholar]
- Learoyd, T.P.; Burrows, J.L.; French, E.; Seville, P.C. Chitosan-based spray-dried respirable powders for sustained delivery of terbutaline sulfate. Eur. J. Pharm. Biopharm. 2008, 68, 224–234. [Google Scholar] [CrossRef] [PubMed]
- U.S. Department of Health and Human Services Food and Drug Administration. Guidance for Industry—Validation of Analytical Procedures: Methodology; ICH-Q2B; International Commission on Harmonisation (ICH): Geneva, Switzerland, 1996. Available online: https://www.fda.gov/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/ucm265700.htm (accessed on 26 January 2018).
- Bonferoni, M.C.; Rossi, S.; Ferrari, F.; Caramella, C. A modified Franz diffusion cell for simultaneous assessment of drug release and washability of mucoadhesive gels. Pharm. Dev. Technol. 1999, 4, 45–53. [Google Scholar] [CrossRef] [PubMed]
- Rossi, S.; Bonferoni, M.C.; Ferrari, F.; Caramella, C. Drug release and washability of mucoadhesive gels based on sodium carboxymethylcellulose and polyacrylic acid. Pharm. Dev. Technol. 1999, 4, 55–63. [Google Scholar] [CrossRef] [PubMed]
- Amaral-Machado, L.; Xavier-Júnior, F.H.; Rutckeviski, R.; Morais, A.R.V.; Alencar, E.N.; Dantas, T.R.F.; Cruz, A.K.M.; Genre, J.; Silva-Junior, A.A.; Pedrosa, M.F.F.; et al. New Trends on Antineoplastic Therapy Research: Bullfrog (Rana catesbeiana Shaw) Oil Nanostructured Systems. Molecules 2016, 21, 585. [Google Scholar] [CrossRef] [PubMed]









| ED (%) | FPF (%) | RF (%) | DPF (µg of 5FU) | |
|---|---|---|---|---|
| 5FU-NS | 92.02 ± 0.06 | 44.60 ± 0.24 | 76.84 ± 0.07 | 5201.73 ± 11.81 |
| 5FU-MS | 94.14 ± 0.72 | 33.84 ± 0.58 | 55.12 ± 2.98 | 2198.40 ± 57.19 |
| 5FU pure | 92.39 ± 4.46 | 2.78 ± 1.73 | 5.14 ± 0.55 | 591.97 ± 368.57 |
| sLangmuir Isotherm | Freundlich Isotherm | ||||||
|---|---|---|---|---|---|---|---|
| Q0 | Q0b | RL | r | K | n | r | |
| 5FU-MS | 100.00 | 200.00 | 1 | 0.994 | 41.59 | 3.33 | 0.531 |
| MS-AD | 83.33 | * | 1 | 0.931 | 26.30 | 1.77 | 0.990 |
| MS-AM | 142.86 | 2.17 | >1 | 0.803 | 4.23 | 1.47 | 0.902 |
| Component | 5FU-MS * | 5FU-NS * | MS-AD * | MS-AM * |
|---|---|---|---|---|
| 5FU | 0.1 | 0.1 | - | 0.1 |
| Chondroitin Sulfate | 0.05 | 0.05 | 0.05 | 0.05 |
| Sodium Deoxycholate | 0.02 | 0.02 | 0.02 | 0.02 |
| Methocel F4M | 0.3 | - | 0.3 | - |
| H2O | 100 | 98 | 100 | 100 |
| Acetone | - | 2 | - | - |
| Mini Spray-Dryer B-290 1 | Nano Spray-Dryer B-90 1 | ||
|---|---|---|---|
| Parameter 2 | Condition * | Parameter 2 | Condition * |
| Spray mesh (µm) | 7 | Spray mesh (µm) | 4 |
| Q-Flow | 60 | Airflow (L·min−1) | 120 |
| Inlet (°C) | 130 | Inlet (°C) | 50 |
| Outlet (°C) | 70 | Outlet (°C) | 40 |
| Aspirator (%) | 100 | CAP (°C) | 62 |
| Pump (%) | 20 | Mode * | Open |
| Nozzle Cleaner | 1 | ||
| Mode * | Open | ||
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zatta, K.C.; Frank, L.A.; Reolon, L.A.; Amaral-Machado, L.; Egito, E.S.T.; Gremião, M.P.D.; Pohlmann, A.R.; Guterres, S.S. An Inhalable Powder Formulation Based on Micro- and Nanoparticles Containing 5-Fluorouracil for the Treatment of Metastatic Melanoma. Nanomaterials 2018, 8, 75. https://doi.org/10.3390/nano8020075
Zatta KC, Frank LA, Reolon LA, Amaral-Machado L, Egito EST, Gremião MPD, Pohlmann AR, Guterres SS. An Inhalable Powder Formulation Based on Micro- and Nanoparticles Containing 5-Fluorouracil for the Treatment of Metastatic Melanoma. Nanomaterials. 2018; 8(2):75. https://doi.org/10.3390/nano8020075
Chicago/Turabian StyleZatta, Kelly Cristine, Luiza A. Frank, Luciano Antonio Reolon, Lucas Amaral-Machado, Eryvaldo S. T. Egito, Maria Palmira Daflon Gremião, Adriana Raffin Pohlmann, and Silvia S. Guterres. 2018. "An Inhalable Powder Formulation Based on Micro- and Nanoparticles Containing 5-Fluorouracil for the Treatment of Metastatic Melanoma" Nanomaterials 8, no. 2: 75. https://doi.org/10.3390/nano8020075
APA StyleZatta, K. C., Frank, L. A., Reolon, L. A., Amaral-Machado, L., Egito, E. S. T., Gremião, M. P. D., Pohlmann, A. R., & Guterres, S. S. (2018). An Inhalable Powder Formulation Based on Micro- and Nanoparticles Containing 5-Fluorouracil for the Treatment of Metastatic Melanoma. Nanomaterials, 8(2), 75. https://doi.org/10.3390/nano8020075