Development of a Point-of-Care System Based on White Light Reflectance Spectroscopy: Application in CRP Determination
Abstract
:1. Introduction
2. Materials and Methods
2.1. Materials
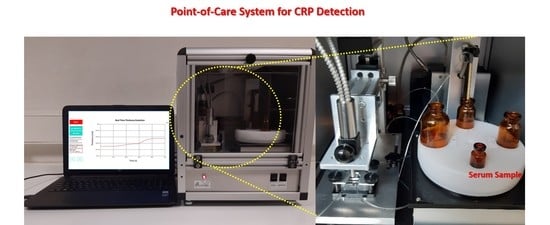
2.2. Instrumentation
2.3. Chip Biofunctionalization and Assay Protocol
3. Results
3.1. Assay Development and Optimization
3.2. Sample Dilution Effect on CRP Assay
3.3. Analytical Evaluation
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Peisajovich, A.; Marnell, L.; Mold, C.; Du Clos, T.W. C-reactive protein at the interface between innate immunity and inflammation. Exp. Rev. Clin. Immunol. 2008, 4, 379–390. [Google Scholar] [CrossRef]
- Ansar, W.; Ghosh, S. C-reactive protein and the biology of disease. Immunol. Res. 2013, 56, 131–142. [Google Scholar] [CrossRef]
- Pfäfflin, A.; Schleicher, E. Inflammation markers in point-of-care testing (POCT). Anal. Bioanal. Chem. 2008, 393, 1473–1480. [Google Scholar] [CrossRef]
- Grondman, I.; Pirvu, A.; Riza, A.; Ioana, M.; Netea, G.M. Biomarkers of inflammation and the etiology of sepsis. Biochem. Soc. Trans. 2020, 48, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Tsao, Y.-T.; Tsai, Y.-H.; Liao, W.-T.; Shen, C.-J.; Shen, C.-F.; Cheng, C.-M. Differential markers of bacterial and viral infections in children for point-of-care testing. Trends Mol. Med. 2020, 26, 1118–1132. [Google Scholar] [CrossRef] [PubMed]
- Prucha, M.; Bellingan, G.; Zazula, R. Sepsis biomarkers. Clin. Chim. Acta 2015, 440, 97–103. [Google Scholar] [CrossRef] [PubMed]
- Teggert, A.; Datta, H.; Ali, Z. Biomarkers for Point-of-Care Diagnosis of Sepsis. Micromachines 2020, 11, 286. [Google Scholar] [CrossRef] [Green Version]
- Hofer, N.; Zacharias, E.; Müller, W.; Resch, B. An update on the use of C-reactive protein in early-onset neonatal sepsis: Current insights and new Tasks. Neonatology 2012, 102, 25–36. [Google Scholar] [CrossRef] [PubMed]
- Landry, A.; Docherty, P.; Ouellette, S.; Cartier, L.J. Causes and outcomes of markedly elevated C-reactive protein levels. Can. Fam. Physician 2017, 63, 316–323. [Google Scholar]
- Boncler, M.; Wu, Y.; Watala, C. The multiple faces of C-reactive protein—Physiological and pathophysiological implications in cardiovascular disease. Molecules 2019, 24, 2062. [Google Scholar] [CrossRef] [Green Version]
- Algarra, M.; Gomes, D.; Esteves da Silva, J.C.G. Current analytical strategies for C-reactive protein quantification in blood. Clin. Chim. Acta 2013, 415, 1–9. [Google Scholar] [CrossRef]
- Vashist, S.K.; Venkatesh, A.G.; Marion Schneider, E.; Beaudoin, C.; Luppa, P.B.; Luong, J.H.T. Bioanalytical advances in assays for C-reactive protein. Biotechnol. Adv. 2016, 34, 272–290. [Google Scholar] [CrossRef] [PubMed]
- Komoriya, T.; Inoue, N.; Yoshimune, K.; Ogawa, M.; Moriyama, M.; Kohno, H. Use of a highly sensitive latex reagent with amino acid spacer for determination of C-reactive protein concentration in a variety of liver diseases. J. Biosci. Bioeng. 2012, 114, 560–563. [Google Scholar] [CrossRef] [PubMed]
- Vashist, S.K.; Czilwik, G.; van Oordt, T.; von Stetten, F.; Zengerle, R.; Marion Schneider, E.; Luong, J.H.T. One-step kinetics-based immunoassay for the highly sensitive detection of C-reactive protein in less than 30 min. Anal. Biochem. 2014, 456, 32–37. [Google Scholar] [CrossRef]
- Yang, S.F.; Gao, B.Z.; Tsai, H.Y.; Fuh, C.B. Detection of c-reactive protein based on a magnetic immunoassay by using functional magnetic and fluorescent nanoparticles in microplates. Analyst 2014, 139, 5576–5581. [Google Scholar] [CrossRef]
- Shiesh, S.-C.; Chou, T.-C.; Lin, X.-Z.; Kao, P.-C. Determination of C-reactive protein with an ultra-sensitivity immunochemiluminometric assay. J. Immunol. Method 2006, 311, 87–95. [Google Scholar] [CrossRef] [PubMed]
- Ouyang, Μ.; Tu, D.; Tong, L.; Sarwar, M.; Bhimaraj, A.; Li, C.; Cote, L.G.; Di Carlo, D. A review of biosensor technologies for blood biomarkers toward monitoring cardiovascular diseases at the point-of-care. Biosens. Bioelectron. 2021, 171, 112621. [Google Scholar] [CrossRef] [PubMed]
- Sohrabi, H.; Kholafazad Kordasht, H.; Pashazadeh-Panahi, P.; Nezhad-Mokhtari, P.; Hashemzaei, M.; Reza Majidi, M.; Mosafer, J.; Oroojalian, F.; Mokhtarzadeh, A.; de la Guardia, M. Recent advances of electrochemical and optical biosensors for detection of C-reactive protein as a major inflammatory biomarker. Microchem. J. 2020, 158, 105287. [Google Scholar] [CrossRef]
- John, S.A.; Price, P.S. Existing and emerging technologies for point-of-care testing. Clin. Biochem. Rev. 2014, 35, 155–167. [Google Scholar]
- Vashist, S.K.; Luppa, P.B.; Yeo, L.Y.; Ozcan, A.; Luong, J.H.T. Emerging Technologies for next-generation point-of-care testing. Trend Biotechnol. 2015, 33, 692–705. [Google Scholar] [CrossRef]
- Zarei, M. Portable biosensing devices for point-of-care diagnostics: Recent developments and applications. Trend Anal. Chem. 2017, 91, 26–41. [Google Scholar] [CrossRef]
- Tsounidi, D.; Petrou, S.P.; Raptis, I. Current progress on biosensors and Point-of-Care devices for sepsis diagnosis. IEEE Sens. J. 2021, 21, 12840–12855. [Google Scholar] [CrossRef]
- Noh, S.; Kim, J.; Kim, G.; Park, C.; Jang, H.; Lee, M.; Lee, T. Recent advances in CRP biosensor based on electrical, electrochemical and optical methods. Sensors 2021, 21, 3024. [Google Scholar] [CrossRef]
- Salvo, P.; Dini, V.; Kirchhain, A.; Janowska, A.; Oranges, T.; Chiricozzi, A.; Lomonaco, T.; Di Francesco, F.; Romanelli, M. Sensors and biosensors for C-reactive protein, temperature and pH, and their applications for monitoring wound healing: A Review. Sensors 2017, 17, 2952. [Google Scholar] [CrossRef] [Green Version]
- Bakirhan, K.N.; Ozcelikay, G.; Ozkan, A.S. Recent progress on the sensitive detection of cardiovascular diseasemarkers by electrochemical-based biosensors. J. Pharm. Biomed. Anal. 2018, 159, 406–424. [Google Scholar] [CrossRef] [PubMed]
- Kim, C.-H.; Ahn, J.-H.; Kim, J.-Y.; Choi, J.-M.; Lim, K.-C.; Jung Park, T.; Heo, N.S.; Lee, H.G.; Kim, G.-W.; Choi, Y.-K. CRP detection from serum for chip-based point-of-care testing system. Biosens. Bioelectron. 2013, 41, 322–327. [Google Scholar] [CrossRef]
- Molinero-Fernández, Á.; López, M.Á.; Escarpa, A. Electrochemical microfluidic micromotors-based immunoassay for C-reactive protein determination in preterm neonatal samples with sepsis suspicion. Anal. Chem. 2020, 92, 5048–5054. [Google Scholar] [CrossRef]
- Koukouvinos, G.; Petrou, P.; Misiakos, K.; Drygiannakis, D.; Raptis, I.; Stefanitsis, G.; Martini, S.; Nikita, D.; Goustouridis, D.; Moser, I.; et al. Simultaneous determination of CRP and D-dimer in human blood plasma samples with White Light Reflectance Spectroscopy. Biosens. Bioelectron. 2016, 84, 89–96. [Google Scholar] [CrossRef] [PubMed]
- Wang, W.; Mai, Z.; Chen, Y.; Wang, J.; Li, L.; Su, Q.; Li, X.; Hong, X. A label-free fiber optic SPR biosensor for specific detection of C-reactive protein. Sci. Rep. 2017, 7, 16904. [Google Scholar] [CrossRef] [PubMed]
- Seok, S.J.; Ju, H. Plasmonic optical biosensors for detecting C-reactive protein: A review. Micromachines 2020, 11, 895. [Google Scholar] [CrossRef]
- Brouwer, N.; van Pelt, J. Validation and evaluation of eight commercially available point of care CRP methods. Clin. Chim. Acta 2015, 439, 195–201. [Google Scholar] [CrossRef] [PubMed]
- Koukouvinos, G.; Goustouridis, D.; Misiakos, K.; Kakabakos, S.; Raptis, I.; Petrou, P. Rapid C-reactive protein determination in whole blood with a White Light Reflectance Spectroscopy label-free immunosensor for Point-of-Care applications. Sens. Actuator B 2018, 260, 282–288. [Google Scholar] [CrossRef]
- Koukouvinos, G.; Petrou, P.; Goustouridis, D.; Misiakos, K.; Kakabakos, S.; Raptis, I. Development and Bioanalytical Applications of a White Light Reflectance Spectroscopy Label-Free Sensing Platform. Biosensors 2017, 7, 46. [Google Scholar] [CrossRef] [Green Version]
- Anastasiadis, V.; Koukouvinos, G.; Petrou, P.S.; Economou, A.; Dekker, J.; Harjanne, M.; Heimala, P.; Goustouridis, D.; Raptis, I.; Kakabakos, S.E. Multiplexed mycotoxins determination employing white light reflectance spectroscopy and silicon chips with silicon oxide areas of different thickness. Biosens. Bioelectron. 2020, 153, 112035. [Google Scholar] [CrossRef] [PubMed]
- Stavra, E.; Petrou, P.S.; Koukouvinos, G.; Economou, A.; Goustouridis, D.; Misiakos, K.; Raptis, I.; Kakabakos, S.E. Fast, sensitive and selective determination of herbicide glyphosate in water samples with a White Light Reflectance Spectroscopy immunosensor. Talanta 2020, 214, 120854. [Google Scholar] [CrossRef]






| Sample# | Amount Added (μg/mL) | Amount Determined (μg/mL) | % Recovery |
|---|---|---|---|
| 1 | 0 | 0.53 | - |
| 0.25 | 0.79 | 104 | |
| 0.50 | 1.1 | 114 | |
| 1.0 | 1.4 | 87.0 | |
| 2 | 0 | 0.92 | - |
| 0.50 | 1.5 | 116 | |
| 1.0 | 1.9 | 98.0 | |
| 2.0 | 2.8 | 94.0 | |
| 3 | 0 | 1.8 | - |
| 1.0 | 2.9 | 110 | |
| 2.0 | 4.7 1 | 95.0 | |
| 5.0 | 7.7 1 | 98.0 |
| Commercial Device | Method | Sample Type | Sample Volume (μL) | Analysis Time (min) | Dynamic Range (μg/mL) | Device Weight (kg) |
|---|---|---|---|---|---|---|
| PATHFAST (Mitsubisi Chemical) | chemiluminescence enzyme immunoassay | whole blood plasma/serum | 100 | <17 | 0.05–30 | 28 |
| AFIAS (Boditech) | fluorescent solid-phase sandwich immunoassay | whole blood plasma/serum | 10 | 3 | 0.5–200 | 15.1 |
| iChroma II (Boditech) | immunochromatographic fluorescent | whole blood plasma/serum | 10 | 3 | 2.5–300 | 1.3 |
| AQT90 Flex (Radiometer) | solid-phase sandwich immunoassay | whole blood plasma | 2000 | <13 | 5–500 | 35 |
| SMART (Eurolyser) | latex enhanced immunoturbidimetric assay | whole blood plasma/serum | 5 | 3–4 | 2–240 0.5–120 | 3.4 |
| CUBE (Eurolyser) | latex enhanced immunoturbidimetric assay | whole blood plasma/serum | 5 | 3–4 | 2–240 0.5–120 | 2.4 |
| Afinion™ (Abbott) | solid-phase immunoassay | whole blood plasma/serum | 2.5 | 3–4 | 5–200 5–160 | 3.4 |
| Microsemi LC-667G (Horiba) | immunoturbidimetric assay | whole blood plasma/serum | 18 | 4 | 0–200 0–150 | 19 |
| Innovastar®® (Diagnostic Systems GmbH) | immunoturbidimetric assay | whole blood plasma | 10 | 6.5 | 5–400 2–160 | 4 |
| Spinit®® (biosurfit SA) | Surface Plasmon Resonance immunoassay | whole blood plasma/serum | 8 | <4 | 2–300 | 4.1 |
| QuickRead go (Aidian) | immunoturbidimetric assay | whole blood plasma/serum | - | 2 | 5–200 | 1.7 |
| Nano-Check™ (Nano-Ditech) | immunochromatographic assay | whole blood plasma/serum | 15 | 15 | 0.5–20 | - |
| Proposed device | WLRS solid-phase sandwich immunoassay | plasma/serum | 10 | 12 | 0.05–200 | 10 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tsounidi, D.; Koukouvinos, G.; Christianidis, V.; Legaki, E.; Giogli, V.; Panagiotopoulou, K.; Taka, S.; Ekaterinidi, Z.; Kakabakos, S.; Raptis, I.; et al. Development of a Point-of-Care System Based on White Light Reflectance Spectroscopy: Application in CRP Determination. Biosensors 2021, 11, 268. https://doi.org/10.3390/bios11080268
Tsounidi D, Koukouvinos G, Christianidis V, Legaki E, Giogli V, Panagiotopoulou K, Taka S, Ekaterinidi Z, Kakabakos S, Raptis I, et al. Development of a Point-of-Care System Based on White Light Reflectance Spectroscopy: Application in CRP Determination. Biosensors. 2021; 11(8):268. https://doi.org/10.3390/bios11080268
Chicago/Turabian StyleTsounidi, Dimitra, Georgios Koukouvinos, Vasilios Christianidis, Evangelia Legaki, Vasiliki Giogli, Konstantina Panagiotopoulou, Styliani Taka, Zoi Ekaterinidi, Sotirios Kakabakos, Ioannis Raptis, and et al. 2021. "Development of a Point-of-Care System Based on White Light Reflectance Spectroscopy: Application in CRP Determination" Biosensors 11, no. 8: 268. https://doi.org/10.3390/bios11080268
APA StyleTsounidi, D., Koukouvinos, G., Christianidis, V., Legaki, E., Giogli, V., Panagiotopoulou, K., Taka, S., Ekaterinidi, Z., Kakabakos, S., Raptis, I., & Petrou, P. (2021). Development of a Point-of-Care System Based on White Light Reflectance Spectroscopy: Application in CRP Determination. Biosensors, 11(8), 268. https://doi.org/10.3390/bios11080268