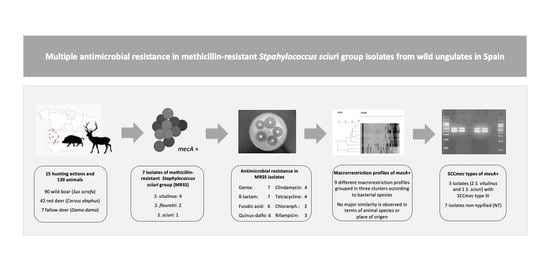
Multiple Antimicrobial Resistance in Methicillin-Resistant Staphylococcus sciuri Group Isolates from Wild Ungulates in Spain
Abstract
:1. Introduction
2. Results
2.1. Prevalence and Species of MRS
2.2. Antimicrobial Resistance Patterns
2.3. Types of SCCmec and DNA Macrorestriction Profiles
3. Discussion
4. Materials and Methods
4.1. Game States
4.2. Sample Collection
4.3. Bacterial Culture, Detection of the mecA Gene and Conservation
4.4. Species Identification
4.5. Antimicrobial Resistance and Identification of Antimicrobial Resistance Genes
4.6. Typing of Staphylococcal Cassette Chromosome mec (SCCmec)
4.7. Phylogenetic Analysis Using Pulsed-Field Gel Electrophoresis (PFGE)
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Gortázar, C.; Ruiz-Fons, J.; Höfle, U. Infections shared with wildlife: An updated perspective. Eur. J. Wildl. Res. 2016, 62, 511–525. [Google Scholar] [CrossRef]
- Torres, R.T.; Fernandes, J.; Carvalho, J.; Cunha, M.V.; Caetano, T.; Mendo, S.; Serrano, E.; Fonseca, C. Wild boar as a reservoir of antimicrobial resistance. Sci. Total Environ. 2019, 717, 135001. [Google Scholar] [CrossRef]
- Partridge, S.R.; Kwong, S.M.; Firth, N.; Jensen, S.O. Mobile Genetic Elements Associated with Antimicrobial Resistance. Clin. Microbiol. Rev. 2018, 31, e00088-17. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jevons, M.P. “Celbenin”-resistant staphylococci. Br. Med. J. 1961, 1, 124–125. [Google Scholar] [CrossRef]
- Sjostrom, J.E.; Lofdahl, S.; Philipson, L. Transformation reveals a chromosomal locus of the gene(s) for methicillin resistance in Staphylococcus aureus. J. Bacteriol. 1975, 123, 905–915. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hartman, B.J.; Tomasz, A. Low-affinity penicillin-binding protein associated with beta-lactam resistance in Staphylococcus aureus. J. Bacteriol. 1984, 158, 513–516. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nowakiewicz, A.; Ziółkowska, G.; Zieba, P.; Gnat, S.; Wojtanowicz-Markiewicz, K.; Trościańczyk, A. Coagulase-positive Staphylococcus isolated from wildlife: Identification, molecular characterization and evaluation of resistance profiles with focus on a methicillin-resistant strain. Comp. Immunol. Microbiol. Infect. Dis. 2016, 44, 21–28. [Google Scholar] [CrossRef] [PubMed]
- Porrero, M.C.; Mentaberre, G.; Sánchez, S.; Fernández-Llario, P.; Casas-Díaz, E.; Mateos, A.; Vidal, D.; Lavín, S.; Fernández-Garayzábal, J.F.; Domínguez, L. Carriage of Staphylococcus aureus by free-living wild animals in Spain. Appl. Environ. Microbiol. 2014, 80, 4865–4870. [Google Scholar] [CrossRef] [Green Version]
- Porrero, M.C.; Mentaberre, G.; Sánchez, S.; Fernández-Llario, P.; Gómez-Barrero, S.; Navarro-Gonzalez, N.; Serrano, E.; Casas-Díaz, E.; Marco, I.; Fernández-Garayzabal, J.F.; et al. Methicillin resistant Staphylococcus aureus (MRSA) carriage in different free-living wild animal species in Spain. Vet. J. 2013, 198, 127–130. [Google Scholar] [CrossRef] [PubMed]
- Sousa, M.; Silva, N.; Manageiro, V.; Ramos, S.; Coelho, A.; Gonçalves, D.; Caniça, M.; Torres, C.; Igrejas, G.; Poeta, P. First report on MRSA CC398 recovered from wild boars in the north of Portugal. Are we facing a problem? Sci. Total. Environ. 2017, 596–597, 26–31. [Google Scholar] [CrossRef]
- de Neeling, A.J.; van den Broek, M.J.M.; Spalburg, E.C.; van Santen-Verheuvel, M.G.; Dam-Deisz, W.D.C.; Boshuizen, H.C.; van de Giessen, A.W.; van Duijkeren, E.; Huijsdens, X.W. High prevalence of methicillin resistant Staphylococcus aureus in pigs. Vet. Microbiol. 2007, 122, 366–372. [Google Scholar] [CrossRef]
- Khanna, T.; Friendship, R.; Dewey, C.; Weese, J.S. Methicillin resistant Staphylococcus aureus colonization in pigs and pig farmers. Vet. Microbiol. 2008, 128, 298–303. [Google Scholar] [CrossRef]
- Meemken, D.; Blaha, T. Research on the occurrence of methicillin-resistant Staphylococcus aureus (MRSA) in domestic pigs and wild boars in Germany. Dtsch. Tierarztl. Wochenschr. 2009, 116, 297–301. [Google Scholar] [CrossRef]
- De Vos, P.; Garrity, G.; Jones, D. Gen. Staphylococcus. In Bergey´s Manual of Systematic Bacteriology; Springer: Berlin/Heidelberg, Germany, 2009; Volume 3, pp. 392–421. [Google Scholar]
- Kloos, W.E.; Schleifer, K.H.; Smith, R.F. Characterization of Staphylococcus sciuri sp. nov. and its subspecies. Int. J. Syst. Bacteriol. 1976, 26, 22–37. [Google Scholar] [CrossRef]
- Couto, I.; Sanches, I.S.; Sá-Leão, R.; De Lencastre, H. Molecular characterization of Staphylococcus sciuri strains isolated from humans. J. Clin. Microbiol. 2000, 38, 1136–1143. [Google Scholar] [CrossRef] [Green Version]
- Nemeghaire, S.; Argudín, M.A.; Feßler, A.T.; Hauschild, T.; Schwarz, S.; Butaye, P. The ecological importance of the Staphylococcus sciuri species group as a reservoir for resistance and virulence genes. Vet. Microbiol. 2014, 171, 342–356. [Google Scholar] [CrossRef]
- Nemeghaire, S.; Vanderhaeghen, W.; Angeles Argudín, M.; Haesebrouck, F.; Butaye, P. Characterization of methicillin-resistant Staphylococcus sciuri isolates from industrially raised pigs, cattle and broiler chickens. J. Antimicrob. Chemother. 2014, 69, 2928–2934. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bhargava, K.; Zhang, Y. Characterization of methicillin-resistant coagulase-negative staphylococci (MRCoNS) in retail meat. Food Microbiol. 2014, 42, 56–60. [Google Scholar] [CrossRef]
- Piessens, V.; De Vliegher, S.; Verbist, B.; Braem, G.; Van Nuffel, A.; De Vuyst, L.; Heyndrickx, M.; Van Coillie, E. Characterization of coagulase-negative staphylococcus species from cows’ milk and environment based on bap, icaA, and mecA genes and phenotypic susceptibility to antimicrobials and teat dips. J. Dairy Sci. 2012, 95, 7027–7038. [Google Scholar] [CrossRef] [Green Version]
- Karakulska, J.; Fijałkowski, K.; Nawrotek, P.; Pobucewicz, A.; Poszumski, F.; Czernomysy-Furowicz, D. Identification and methicillin resistance of coagulase-negative staphylococci isolated from nasal cavity of healthy horses. J. Microbiol. 2012, 50, 444–451. [Google Scholar] [CrossRef]
- Davis, J.A.; Jackson, C.R.; Fedorka-Cray, P.J.; Barrett, J.B.; Brousse, J.H.; Gustafson, J.; Kucher, M. Carriage of methicillin-resistant staphylococci by healthy companion animals in the US. Lett. Appl. Microbiol. 2014, 59, 1–8. [Google Scholar] [CrossRef]
- Kumar, D.; Pornsukarom, S.; Sivaraman, G.K.; Thakur, S. Environmental Dissemination of Multidrug Methicillin-Resistant Staphylococcus sciuri after Application of Manure from Commercial Swine Production Systems. Foodborne Pathog. Dis. 2018, 15, 210–217. [Google Scholar] [CrossRef] [PubMed]
- Schoenfelder, S.M.K.; Dong, Y.; Feßler, A.T.; Schwarz, S.; Schoen, C.; Köck, R.; Ziebuhr, W. Antibiotic resistance profiles of coagulase-negative staphylococci in livestock environments. Vet. Microbiol. 2017, 200, 79–87. [Google Scholar] [CrossRef]
- Mama, O.M.; Ruiz-Ripa, L.; Lozano, C.; González-Barrio, D.; Ruiz-Fons, J.F.; Torres, C. High diversity of coagulase negative staphylococci species in wild boars, with low antimicrobial resistance rates but detection of relevant resistance genes. Comp. Immunol. Microbiol. Infect. Dis. 2019, 64, 125–129. [Google Scholar] [CrossRef]
- Plan Nacional de Resistencias a Antibióticos. Jiacra Report. Primer Análisis Integrado del Consumo de Antibióticos en España. Available online: https://www.resistenciaantibioticos.es/es/publicaciones/informe-jiacra-espana (accessed on 30 June 2021).
- Frey, Y.; Rodriguez, J.P.; Thomann, A.; Schwendener, S.; Perreten, V. Genetic characterization of antimicrobial resistance in coagulase-negative staphylococci from bovine mastitis milk. J. Dairy Sci. 2013, 96, 2247–2257. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Couto, I.; De Lencastre, H.; Severina, E.; Kloos, W.; Webster, J.A.; Hubner, R.J.; Sanches, I.S.; Tomasz, A. Ubiquitous presence of a mecA homologue in natural isolates of Staphylococcus sciuri. Microb. Drug Resist. 1996, 2, 377–391. [Google Scholar] [CrossRef] [PubMed]
- Hanssen, A.M.; Kjeldsen, G.; Ericson Sollid, J.U. Local Variants of Staphylococcal Cassette Chromosome mec in Sporadic Methicillin-Resistant Staphylococcus aureus and Methicillin-Resistant Coagulase-Negative Staphylococci: Evidence of Horizontal Gene Transfer? Antimicrob. Agents Chemother. 2004, 48, 285–296. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, Y.; Agidi, S.; Lejeune, J.T. Diversity of staphylococcal cassette chromosome in coagulase-negative staphylococci from animal sources. J. Appl. Microbiol. 2009, 107, 1375–1383. [Google Scholar] [CrossRef] [PubMed]
- Vanderhaeghen, W.; Vandendriessche, S.; Crombé, F.; Dispas, M.; Denis, O.; Hermans, K.; Haesebrouck, F.; Butaye, P. Species and staphylococcal cassette chromosome mec (SCCmec) diversity among methicillin-resistant non-Staphylococcus aureus staphylococci isolated from pigs. Vet. Microbiol. 2012, 158, 123–128. [Google Scholar] [CrossRef] [PubMed]
- Lakhundi, S.; Zhang, K. Methicillin-Resistant Staphylococcus aureus: Molecular Characterization, Evolution, and Epidemiology. Clin. Microbiol. Rev. 2018, 31, e00020-18. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jones, M.E.; Köhrer, K.; Schmitz, F.J. Multiplex PCR for the Rapid Simultaneous Speciation and Detection of Methicillin-Resistance and Genes Encoding Toxin Production in Staphylococcus aureus. In Methods in Molecular Medicine; Antibiotic Resistance Methods and Protocols; Gillespie, S.H., Ed.; Humana Press: Totowa, NJ, USA, 2001; Volume 48, pp. 103–112. [Google Scholar]
- Clark, A.E.; Kaleta, E.J.; Arora, A.; Wolk, D.M. Matrix-assisted laser desorption ionization-time of flight mass spectrometry: A fundamental shift in the routine practice of clinical microbiology. Clin. Microbiol. Rev. 2013, 26, 547–603. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- EUCAST. Clinical Breakpoint Bacteria (v. 10). Available online: https://eucast.org/ (accessed on 30 June 2021).
- Martineau, F.; Picard, F.J.; Lansac, N.; Menard, C.; Roy, P.H.; Ouellette, M.; Bergeron, M.G. Correlation between the resistance genotype determined by multiplex PCR assays and the antibiotic susceptibility patterns of Staphylococcus aureus and Staphylococcus epidermidis. Antimicrob. Agents Chemother. 2000, 44, 231–238. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Strommenger, B.; Kettlitz, C.; Werner, G.; Witte, W. Multiplex PCR assay for simultaneous detection of nine clinically relevant antibiotic resistance genes in Staphylococcus aureus. J. Clin. Microbiol. 2003, 41, 4089–4094. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Castanheira, M.; Watters, A.A.; Bell, J.M.; Turnidge, J.D.; Jones, R.N. Fusidic acid resistance rates and prevalence of resistance mechanisms among Staphylococcus spp. isolated in North America and Australia, 2007–2008. Antimicrob. Agents Chemother. 2010, 54, 3614–3617. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yamaguchi, T.; Ono, D.; Sato, A. Staphylococcal Cassette Chromosome mec (SCCmec) analysis of MRSA. In Methicillin-Resistant Staphylococcus Aureus (MRSA) Protocols. Cutting-Edge Technologies and Advancements, 3rd ed.; Ji, Y., Ed.; Methods in Molecular Biology; Humana Press: Totowa, NJ, USA, 2020; pp. 59–78. [Google Scholar]
- Center for Diseases Control and Prevention. USA. Oxacillin-Resistant Staphylococcus Aureus on PulseNet (OPN). Laboratory Protocol for Molecular Typing of S. Aureus by PFGE. Available online: https://www.cdc.gov/mrsa/pdf/ar_mras_PFGE_s_aureus.pdf (accessed on 1 July 2021).



| ID | Species | Source | Phenotypic Resistance | Genotype |
|---|---|---|---|---|
| 102 | S. vitulinus | Wild boar | P, FOX, OX, TET, C, CN, DA, QD, RD, FD | mecA, aacA-AphD, tetK, tetM |
| 114 | S. vitulinus | Red deer | P, FOX, OX, TET, C, CN, DA, QD, RD, FD | mecA, aacA-AphD, tetK, tetM |
| 119 | S. fleuretti | Wild boar | P, FOX, OX, TET, C, CN, DA, QD, FD | mecA, tetM |
| 117 | S. vitulinus | Wild boar | P, FOX, OX, TET, CN, DA, QD, RD, FD | mecA, tetM |
| 123 | S. sciuri | Wild boar | P, OX, CN, E, QD, FD | mecA |
| 125 | S. fleuretti | Wild boar | P, OX, CN, QD, FD | mecA |
| 109 | S. vitulinus | Red deer | P, OX, CN | mecA |
| 127 | S. vitulinus | Wild boar | FD | mecA |
| 121 | S. vitulinus | Wild boar | CN | mecA |
| 115 | S. vitulinus | Wild boar | CN | mecA |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rey Pérez, J.; Zálama Rosa, L.; García Sánchez, A.; Hermoso de Mendoza Salcedo, J.; Alonso Rodríguez, J.M.; Cerrato Horrillo, R.; Zurita, S.G.; Gil Molino, M. Multiple Antimicrobial Resistance in Methicillin-Resistant Staphylococcus sciuri Group Isolates from Wild Ungulates in Spain. Antibiotics 2021, 10, 920. https://doi.org/10.3390/antibiotics10080920
Rey Pérez J, Zálama Rosa L, García Sánchez A, Hermoso de Mendoza Salcedo J, Alonso Rodríguez JM, Cerrato Horrillo R, Zurita SG, Gil Molino M. Multiple Antimicrobial Resistance in Methicillin-Resistant Staphylococcus sciuri Group Isolates from Wild Ungulates in Spain. Antibiotics. 2021; 10(8):920. https://doi.org/10.3390/antibiotics10080920
Chicago/Turabian StyleRey Pérez, Joaquín, Laura Zálama Rosa, Alfredo García Sánchez, Javier Hermoso de Mendoza Salcedo, Juan Manuel Alonso Rodríguez, Rosario Cerrato Horrillo, Sofía Gabriela Zurita, and María Gil Molino. 2021. "Multiple Antimicrobial Resistance in Methicillin-Resistant Staphylococcus sciuri Group Isolates from Wild Ungulates in Spain" Antibiotics 10, no. 8: 920. https://doi.org/10.3390/antibiotics10080920
APA StyleRey Pérez, J., Zálama Rosa, L., García Sánchez, A., Hermoso de Mendoza Salcedo, J., Alonso Rodríguez, J. M., Cerrato Horrillo, R., Zurita, S. G., & Gil Molino, M. (2021). Multiple Antimicrobial Resistance in Methicillin-Resistant Staphylococcus sciuri Group Isolates from Wild Ungulates in Spain. Antibiotics, 10(8), 920. https://doi.org/10.3390/antibiotics10080920