One-Step Surface Functionalized Hydrophilic Polypropylene Meshes for Hernia Repair Using Bio-Inspired Polydopamine
Abstract
:1. Introduction
2. Materials and Methods
2.1. Materials
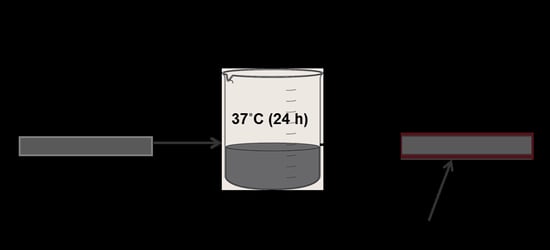
2.2. Surface Functionalization of PP Meshes Materials with Polydopamine
3. Characterization
3.1. SEM & EDX
3.2. FTIR
3.3. XRD and DSC Analysis
3.4. Water Contact Angle
3.5. Statistical Analysis
4. Results and Discussion
4.1. Surface Functionalization of PP Mesh Fibers
4.2. Surface Morphology of PP Meshes Fibers Before and After Surface Functionalization
4.3. Surface Characterization of Polydopamine Functionalized PP Meshes
4.4. Structural and Thermal Properties
4.5. Water Contact Angle
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Baylon, K.; Rodriguez-Camarillo, P.; Elias-Zuniga, A.; Diaz-Elizondo, J.A.; Gilkerson, R.; Lozano, K. Past, Present and Future of Surgical Meshes: A Review. Membranes 2017, 7, 47. [Google Scholar] [CrossRef] [PubMed]
- Biondo-Simoes, M.L.; Carvalho, L.B.; Conceicao, L.T.; Santos, K.B.; Schiel, W.A.; Arantes, M.; Silveira, T.D.; Magri, J.C.; Gomes, F.F. Comparative study of Polypropylene versus Parietex composite(R), Vicryl(R) and Ultrapro(R) meshes, regarding the formation of intraperitoneal adhesions. Acta Cir. Bras. 2017, 32, 98–107. [Google Scholar] [CrossRef] [PubMed]
- Miao, L.; Wang, F.; Wang, L.; Zou, T.; Brochu, G.; Guidoin, R. Physical Characteristics of Medical Textile Prostheses Designed for Hernia Repair: A Comprehensive Analysis of Select Commercial Devices. Materials 2015, 8, 8148–8168. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kalaba, S.; Gerhard, E.; Winder, J.S.; Pauli, E.M.; Haluck, R.S.; Yang, J. Design Strategies and Applications of Biomaterials and Devices for Hernia Repair. Bioact. Mater. 2016, 1, 2–17. [Google Scholar] [CrossRef] [PubMed]
- Sanbhal, N.; Miao, L.; Xu, R.; Khatri, A.; Wang, L. Physical structure and mechanical properties of knitted hernia mesh materials: A review. J. Ind. Text. 2017. [Google Scholar] [CrossRef]
- Guillaume, O.; Perez-Tanoira, R.; Fortelny, R.; Redl, H.; Moriarty, T.F.; Richards, R.G.; Eglin, D.; Petter Puchner, A. Infections associated with mesh repairs of abdominal wall hernias: Are antimicrobial biomaterials the longed-for solution? Biomaterials 2018, 167, 15–31. [Google Scholar] [CrossRef]
- Kokotovic, D.; Bisgaard, T.; Helgstrand, F. Long-term Recurrence and Complications Associated With Elective Incisional Hernia Repair. JAMA 2016, 316, 1575–1582. [Google Scholar] [CrossRef]
- Kulaga, E.; Ploux, L.; Balan, L.; Schrodj, G.; Roucoules, V. Mechanically Responsive Antibacterial Plasma Polymer Coatings for Textile Biomaterials. Plasma Process. Polym. 2014, 11, 63–79. [Google Scholar] [CrossRef]
- Knetsch, M.L.W.; Koole, L.H. New Strategies in the Development of Antimicrobial Coatings: The Example of Increasing Usage of Silver and Silver Nanoparticles. Polymers 2011, 3, 340–366. [Google Scholar] [CrossRef] [Green Version]
- Deeken, C.R.; Lake, S.P. Mechanical properties of the abdominal wall and biomaterials utilized for hernia repair. J. Mech. Behav. Biomed. Mater. 2017, 74, 411–427. [Google Scholar] [CrossRef]
- Poussier, M.; Deneve, E.; Blanc, P.; Boulay, E.; Bertrand, M.; Nedelcu, M.; Herrero, A.; Fabre, J.M.; Nocca, D. A review of available prosthetic material for abdominal wall repair. J. Visc. Surg. 2013, 150, 52–59. [Google Scholar] [CrossRef]
- Coda, A.; Lamberti, R.; Martorana, S. Classification of prosthetics used in hernia repair based on weight and biomaterial. Hernia 2011, 16, 9–20. [Google Scholar] [CrossRef]
- Shankaran, V.; Weber, D.J.; Reed, R.L., 2nd; Luchette, F.A. A review of available prosthetics for ventral hernia repair. Ann. Surg. 2011, 253, 16–26. [Google Scholar] [CrossRef] [PubMed]
- Greca, F.H.; de Paula, J.B.; Biondo-Simões, M.L.; da Costa, F.D.; da Silva, A.P.; Time, S.; Mansur, A. The influence of differing pore sizes on the biocompatibility of two polypropylene meshes in the repair of abdominal defects. Hernia 2001, 5, 59–64. [Google Scholar] [PubMed]
- Hazebroek, E.J.; Ng, A.; Yong, D.H.; Berry, H.; Leibman, S.; Smith, G.S. Evaluation of lightweight titanium-coated polypropylene mesh (TiMesh) for laparoscopic repair of large hiatal hernias. Surg. Endosc. 2008, 22, 2428–2432. [Google Scholar] [CrossRef] [PubMed]
- Jerabek, J.; Novotny, T.; Vesely, K.; Cagas, J.; Jedlicka, V.; Vlcek, P.; Capov, I. Evaluation of three purely polypropylene meshes of different pore sizes in an onlay position in a New Zealand white rabbit model. Hernia 2014, 18, 855–864. [Google Scholar] [CrossRef] [PubMed]
- Labay, C.; Canal, J.M.; Modic, M.; Cvelbar, U.; Quiles, M.; Armengol, M.; Arbos, M.A. Antibiotic-loaded polypropylene surgical meshes with suitable biological behaviour by plasma functionalization and polymerization. Biomaterials 2015, 71, 132–144. [Google Scholar] [CrossRef]
- Mazaki, T.; Mado, K.; Masuda, H.; Shiono, M. Antibiotic prophylaxis for the prevention of surgical site infection after tension-free hernia repair: A Bayesian and frequentist meta-analysis. J. Am. Coll. Surg. 2013, 217, 788–801. [Google Scholar] [CrossRef]
- Mazaki, T.; Mado, K.; Masuda, H.; Shiono, M.; Tochikura, N.; Kaburagi, M. A randomized trial of antibiotic prophylaxis for the prevention of surgical site infection after open mesh-plug hernia repair. Am. J. Surg. 2014, 207, 476–484. [Google Scholar] [CrossRef]
- Rosen, M.J. Polyester-based mesh for ventral hernia repair: Is it safe? Am. J. Surg. 2009, 197, 353–359. [Google Scholar] [CrossRef]
- Bringman, S.; Conze, J.; Cuccurullo, D.; Deprest, J.; Junge, K.; Klosterhalfen, B.; Parra-Davila, E.; Ramshaw, B.; Schumpelick, V. Hernia repair: The search for ideal meshes. Hernia 2010, 14, 81–87. [Google Scholar] [CrossRef] [PubMed]
- Brown, C.N.; Finch, J.G. Which mesh for hernia repair? Ann. R. Coll. Surg. Engl. 2010, 92, 272–278. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Falagas, M.E.; Kasiakou, S.K. Mesh-related infections after hernia repair surgery. Clin. Microbiol. Infect. 2005, 11, 3–8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bilsel, Y.; Abci, I. The search for ideal hernia repair; mesh materials and types. Int. J. Surg. 2012, 10, 317–321. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Harth, K.C.; Rosen, M.J.; Thatiparti, T.R.; Jacobs, M.R.; Halaweish, I.; Bajaksouzian, S.; Furlan, J.; von Recum, H.A. Antibiotic-releasing mesh coating to reduce prosthetic sepsis: An in vivo study. J. Surg. Res. 2010, 163, 337–343. [Google Scholar] [CrossRef] [PubMed]
- Faulk, D.M.; Londono, R.; Wolf, M.T.; Ranallo, C.A.; Carruthers, C.A.; Wildemann, J.D.; Dearth, C.L.; Badylak, S.F. ECM hydrogel coating mitigates the chronic inflammatory response to polypropylene mesh. Biomaterials 2014, 35, 8585–8595. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Perez-Kohler, B.; Fernandez-Gutierrez, M.; Pascual, G.; Garcia-Moreno, F.; San Roman, J.; Bellon, J.M. In vitro assessment of an antibacterial quaternary ammonium-based polymer loaded with chlorhexidine for the coating of polypropylene prosthetic meshes. Hernia 2016, 20, 869–878. [Google Scholar] [CrossRef]
- Bellon, J.M.; Rodriguez, M.; Garcia-Honduvilla, N.; Pascual, G.; Bujan, J. Partially absorbable meshes for hernia repair offer advantages over nonabsorbable meshes. Am. J. Surg. 2007, 194, 68–74. [Google Scholar] [CrossRef]
- Patel, H.; Ostergard, D.R.; Sternschuss, G. Polypropylene mesh and the host response. Int. Urogynecol. J. 2012, 23, 669–679. [Google Scholar] [CrossRef]
- Perez-Kohler, B.; Bayon, Y.; Bellon, J.M. Mesh Infection and Hernia Repair: A Review. Surg. Infect. 2016, 17, 124–137. [Google Scholar] [CrossRef]
- Liu, Y.; Fang, Y.; Qian, J.; Liu, Z.; Yang, B.; Wang, X. Bio-inspired polydopamine functionalization of carbon fiber for improving the interfacial adhesion of polypropylene composites. RSC Adv. 2015, 5, 107652–107661. [Google Scholar] [CrossRef]
- Dung The Nguyen, T.H.A.N. Surface modification of polyamide thin film composite membrane by coating of titanium dioxide nanoparticles. J. Sci. 2016, 1, 468–475. [Google Scholar] [CrossRef] [Green Version]
- Lei, Z.; Yu, Z.; Xi-Cang, R.; Cheng-Yun, N.; Guo-Xin, T.; Ying, T.A.N. Bioinspired Polydopamine Functionalization of Titanium Surface for SilverNanoparticles Immobilization with Antibacterial Property. J. Inorg. Mater. 2014, 29, 1320. [Google Scholar] [CrossRef]
- Zhang, R.-X.; Leen, B.; Liu, T.-Y.; Luis Alconero, P.; Wang, X.-L.; Van der Bruggen, B. Remarkable Anti-Fouling Performance of TiO2-Modified TFC Membranes with Mussel-Inspired Polydopamine Binding. Appl. Sci. 2017, 2017, 81. [Google Scholar] [CrossRef]
- Wei, Q.; Haag, R. Universal polymer coatings and their representative biomedical applications. Mater. Horizons 2015, 2, 567–577. [Google Scholar] [CrossRef]
- Nava-Ortiz, C.A.; Alvarez-Lorenzo, C.; Bucio, E.; Concheiro, A.; Burillo, G. Cyclodextrin-functionalized polyethylene and polypropylene as biocompatible materials for diclofenac delivery. Int. J. Pharm. 2009, 382, 183–191. [Google Scholar] [CrossRef]
- Sarau, G.; Bochmann, A.; Lewandowska, R.; Christianse, S. From Micro– to Macro–Raman Spectroscopy: Solar Silicon for a Case Study. In Advanced Aspects of Spectroscopy; InTech: Vienna, Austria, 2012. [Google Scholar] [Green Version]
- Lin, J.-H.; Pan, Y.-J.; Liu, C.-F.; Huang, C.-L.; Hsieh, C.-T.; Chen, C.-K.; Lin, Z.-I.; Lou, C.-W. Preparation and Compatibility Evaluation of Polypropylene/High Density Polyethylene Polyblends. Materials 2015, 8, 8850–8859. [Google Scholar] [CrossRef] [Green Version]






© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sanbhal, N.; Saitaer, X.; Peerzada, M.; Habboush, A.; Wang, F.; Wang, L. One-Step Surface Functionalized Hydrophilic Polypropylene Meshes for Hernia Repair Using Bio-Inspired Polydopamine. Fibers 2019, 7, 6. https://doi.org/10.3390/fib7010006
Sanbhal N, Saitaer X, Peerzada M, Habboush A, Wang F, Wang L. One-Step Surface Functionalized Hydrophilic Polypropylene Meshes for Hernia Repair Using Bio-Inspired Polydopamine. Fibers. 2019; 7(1):6. https://doi.org/10.3390/fib7010006
Chicago/Turabian StyleSanbhal, Noor, Xiakeer Saitaer, Mazhar Peerzada, Ali Habboush, Fujun Wang, and Lu Wang. 2019. "One-Step Surface Functionalized Hydrophilic Polypropylene Meshes for Hernia Repair Using Bio-Inspired Polydopamine" Fibers 7, no. 1: 6. https://doi.org/10.3390/fib7010006
APA StyleSanbhal, N., Saitaer, X., Peerzada, M., Habboush, A., Wang, F., & Wang, L. (2019). One-Step Surface Functionalized Hydrophilic Polypropylene Meshes for Hernia Repair Using Bio-Inspired Polydopamine. Fibers, 7(1), 6. https://doi.org/10.3390/fib7010006