Effect of Supplementation on Levels of Homovanillic and Vanillylmandelic Acids in Children with Autism Spectrum Disorders
Abstract
:1. Introduction
2. Results
3. Discussion
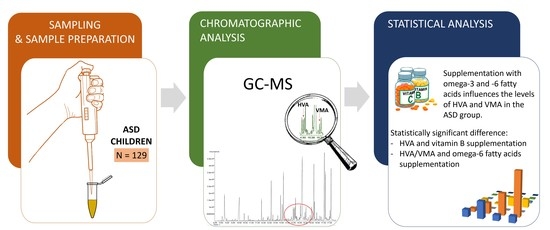
4. Materials and Methods
4.1. Subjects
4.2. Sample Preparation
4.3. Solvents and Derivatizing Agents for GC-MS Analysis
4.4. Urinary Creatinine Determination
4.5. Analytical Methods
4.6. Statistical Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. The ICD-10 Classification of Mental and Behavioural Disorders: Diagnostic Criteria for Research; World Health Organization: Geneva, Switzerland, 2003. [Google Scholar]
- Yates, K.; Le Couteur, A. Diagnosing autism. Paediatr. Child Health 2009, 19, 55–59. [Google Scholar] [CrossRef]
- Hozyasz, K.K.; Gryglicka, H.; Żółkowska, J. Gluten-free diet in the treatment of autism spectrum disorders—A short overview. Gastroenterol. Rev. 2010, 4, 195–201. [Google Scholar] [CrossRef]
- Ecker, C.; Murphy, D. Neuroimaging in autism—From basic science to translational research. Nat. Rev. Neurol. 2014, 10, 82–91. [Google Scholar] [CrossRef] [PubMed]
- Dunlap, J.J. Autism Spectrum Disorder Screening and Early Action. J. Nurse Pract. 2019, 15, 496–501. [Google Scholar] [CrossRef]
- Yates, K.; Le Couteur, A. Diagnosing autism/autism spectrum disorders. Paediatr. Child Health 2016, 26, 513–518. [Google Scholar] [CrossRef]
- Matelski, L.; Van de Water, J. Risk factors in autism: Thinking outside the brain. J. Autoimmun. 2016, 67, 1–7. [Google Scholar] [CrossRef] [Green Version]
- Yenkoyan, K.; Grigoryan, A.; Fereshetyan, K.; Yepremyan, D. Advances in understanding the pathophysiology of autism spectrum disorders. Behav. Brain Res. 2017, 331, 92–101. [Google Scholar] [CrossRef]
- Rossignol, D.A.; Frye, R.E. Evidence linking oxidative stress, mitochondrial dysfunction, and inflammation in the brain of individuals with autism. Front. Physiol. 2014, 5, 150. [Google Scholar] [CrossRef] [Green Version]
- Sauer, M.A.K.; Stanton, M.J.; Hans, M.S.; Grabrucker, A.M. Autism Spectrum Disorders: Etiology and Pathology. In Autism Spectrum Disorders; Grabrucker, A.M., Ed.; Exon Publications: Brisbane, Australia, 2021; pp. 1–16. [Google Scholar] [CrossRef]
- Bjørklund, G.; Waly, M.I.; Al-Farsi, Y.; Saad, K.; Dadar, M.; Rahman, M.; Elhoufey, A.; Chirumbolo, S.; Jóźwik-Pruska, J.; Kałużna-Czaplińska, J. The Role of Vitamins in Autism Spectrum Disorder: What Do We Know? J. Mol. Neurosci. 2019, 67, 373–387. [Google Scholar] [CrossRef]
- Bjørklund, G.; Meguid, N.A.; Dadar, M.; Pivina, L.; Kałużna-Czaplińska, J.; Jóźwik-Pruska, J.; Aaseth, J.; Chartrand, M.S.; Waly, M.I.; Al-Farsi, Y.; et al. Specialized Diet Therapies: Exploration for Improving Behavior in Autism Spectrum Disorder (ASD). Curr. Med. Chem. 2020, 27, 6771–6786. [Google Scholar] [CrossRef]
- Liu, X.; Liu, J.; Xiong, X.; Yang, T.; Hou, N.; Liang, X.; Chen, J.; Cheng, Q.; Li, T. Correlation between Nutrition and Symptoms: Nutritional Survey of Children with Autism Spectrum Disorder in Chongqing, China. Nutrients 2016, 8, 294. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tsujiguchi, H.; Miyagi, S.; Nguyen, T.; Hara, A.; Ono, Y.; Kambayashi, Y.; Shimizu, Y.; Nakamura, H.; Suzuki, K.; Suzuki, F.; et al. Relationship between Autistic Traits and Nutrient Intake among Japanese Children and Adolescents. Nutrients 2020, 12, 2258. [Google Scholar] [CrossRef] [PubMed]
- Murray, R.K.; Granner, D.K.; Mayes, P.A.; Rodwell, V.W. Biochemia Harpera, 3rd ed.; Wydawnictwo Lekarskie PZWL: Warsaw, Poland, 1995; pp. 607–608. [Google Scholar]
- Li, Y.-J.; Li, Y.-M.; Xiang, D.-X. Supplement intervention associated with nutritional deficiencies in autism spectrum disorders: A systematic review. Eur. J. Nutr. 2017, 8, 2571–2582. [Google Scholar] [CrossRef] [PubMed]
- Prokopiak, A. Autyzm a odżywianie. O czym nauczyciel wiedzieć powinien. Lub. Rocz. Pedagog. 2013, 32, 100–118. [Google Scholar] [CrossRef]
- Gevi, F.; Belardo, A.; Zolla, L. A metabolomics approach to investigate urine levels of neurotransmitters and related metabolites in autistic children. Biochim. Biophys. Acta (BBA) Mol. Basis Dis. 2020, 1866, 165859. [Google Scholar] [CrossRef]
- Clarke, C.J.; Haselden, J.N. Metabolic Profiling as a Tool for Understanding Mechanisms of Toxicity. Toxicol. Pathol. 2008, 36, 140–147. [Google Scholar] [CrossRef]
- Yang, C.; Richardson, A.D.; Osterman, A.; Smith, J.W. Profiling of central metabolism in human cancer cells by two-dimensional NMR, GC-MS analysis, and isotopomer modeling. Metabolomics 2007, 4, 13–29. [Google Scholar] [CrossRef]
- Struck, W.; Siluk, D.; Yumba-Mpanga, A.; Markuszewski, M.; Kaliszan, R.; Markuszewski, M.J. Liquid chromatography tandem mass spectrometry study of urinary nucleosides as potential cancer markers. J. Chromatogr. A 2013, 1283, 122–131. [Google Scholar] [CrossRef]
- Waszczuk-Jankowska, M.; Markuszewski, M.J.; Markuszewski, M.; Kaliszan, R. Comparison of RP-HPLC columns used for determination of nucleoside metabolic patterns in urine of cancer patients. Bioanalysis 2012, 4, 1185–1194. [Google Scholar] [CrossRef]
- Kośliński, P.; Bujak, R.; Daghir, E.; Markuszewski, M.J. Metabolic profiling of pteridines for determination of potential biomarkers in cancer diseases. Electrophoresis 2011, 32, 2044–2054. [Google Scholar] [CrossRef]
- Medical Services Advisory Committee. Urinary Metabolic Profiling for Detection of Metabolic Disorders; Medical Services Advisory Committee: Canberra, Australia, 2009; pp. 29–35. [Google Scholar]
- Ahmed, S.S.; Santosh, W.; Kumar, S.; Christlet, H.T.T. Metabolic profiling of Parkinson’s disease: Evidence of biomarker from gene expression analysis and rapid neural network detection. J. Biomed. Sci. 2009, 16, 63. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- James, S.J.; Cutler, P.; Melnyk, S.; Jernigan, S.; Janak, L.; Gaylor, D.W.; Neubrander, J.A. Metabolic biomarkers of increased oxidative stress and impaired methylation capacity in children with autism. Am. J. Clin. Nutr. 2004, 80, 1611–1617. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, A.; Zhou, W.; Qu, L.; He, F.; Wang, H.; Wang, Y.; Cai, C.; Li, X.; Zhou, W.; Wang, M. Altered Urinary Amino Acids in Children with Autism Spectrum Disorders. Front. Cell. Neurosci. 2019, 13, 7. [Google Scholar] [CrossRef] [PubMed]
- Dettmer, K.; Aronov, P.A.; Hammock, B.D. Mass spectrometry-based metabolomics. Mass Spectrom. Rev. 2007, 26, 51–78. [Google Scholar] [CrossRef] [PubMed]
- Gika, H.G.; Theodoridis, G.A.; Plumb, R.S.; Wilson, I.D. Current practice of liquid chromatography–mass spectrometry in metabolomics and metabonomics. J. Pharm. Biomed. Anal. 2014, 87, 12–25. [Google Scholar] [CrossRef] [PubMed]
- Keppler, E.A.H.; Jenkins, C.; Davis, T.J.; Bean, H.D. Advances in the application of comprehensive two-dimensional gas chromatography in metabolomics. TrAC Trends Anal. Chem. 2018, 109, 275–286. [Google Scholar] [CrossRef]
- Wong, J.-M.T.; Malec, P.; Mabrouk, O.S.; Ro, J.; Dus, M.; Kennedy, R.T. Benzoyl chloride derivatization with liquid chromatography–mass spectrometry for targeted metabolomics of neurochemicals in biological samples. J. Chromatogr. A 2016, 1446, 78–90. [Google Scholar] [CrossRef] [Green Version]
- Krajcovicova-Kudlackova, M.; Valachovicova, M.; Mislanova, C.; Hudecova, Z.; Sustrova, M.; Ostatnikova, D. Plasma concentrations of selected antioxidants in autistic children and adolescents. Bratisl. Lek. List. 2009, 110, 247–250. [Google Scholar]
- Gonzalez-Riano, C.; Sanz-Rodríguez, M.; Escudero-Ramirez, J.; Lorenzo, M.P.; Barbas, C.; Cubelos, B.; Garcia, A. Target and untargeted GC–MS based metabolomic study of mouse optic nerve and its potential in the study of neurological visual diseases. J. Pharm. Biomed. Anal. 2018, 153, 44–56. [Google Scholar] [CrossRef] [Green Version]
- Yi, L.; Shi, S.; Yi, Z.; He, R.; Lu, H.; Liang, Y. MeOx-TMS derivatization for GC-MS metabolic profiling of urine and application in the discrimination between normal C57BL/6J and type 2 diabetic KK-Ay mice. Anal. Methods 2014, 6, 4380–4387. [Google Scholar] [CrossRef]
- Li, M.; Wang, X.; Aa, J.; Qin, W.; Zha, W.; Ge, Y.; Liu, L.; Zheng, T.; Cao, B.; Shi, J.; et al. GC/TOFMS analysis of metabolites in serum and urine reveals metabolic perturbation of TCA cycle in db/db mice involved in diabetic nephropathy. Am. J. Physiol. Renal Physiol. 2013, 304, F1317–F1324. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, Q.; Qiao, Y.; Xu, X.-J.; You, X.; Tao, Y. Urine Organic Acids as Potential Biomarkers for Autism-Spectrum Disorder in Chinese Children. Front. Cell. Neurosci. 2019, 13, 150. [Google Scholar] [CrossRef] [PubMed]
- Kałużna-Czaplińska, J.; Żurawicz, E.; Struck, W.; Markuszewski, M. Identification of organic acids as potential biomarkers in the urine of autistic children using gas chromatography/mass spectrometry. J. Chromatogr. B Anal. Technol. Biomed. Life Sci. 2014, 966, 70–76. [Google Scholar] [CrossRef] [PubMed]
- Bitar, T.; Mavel, S.; Emond, P.; Nadal-Desbarats, L.; Lefèvre, A.; Mattar, H.; Soufia, M.; Blasco, H.; Vourc’H, P.; Hleihel, W.; et al. Identification of metabolic pathway disturbances using multimodal metabolomics in autistic disorders in a Middle Eastern population. J. Pharm. Biomed. Anal. 2018, 152, 57–65. [Google Scholar] [CrossRef]
- Emond, P.; Mavel, S.; Aïdoud, N.; Nadal-Desbarats, L.; Montigny, F.; Bonnet-Brilhault, F.; Barthélémy, C.; Merten, M.; Sarda, P.; Laumonnier, F.; et al. GC-MS-based urine metabolic profiling of autism spectrum disorders. Anal. Bioanal. Chem. 2013, 405, 5291–5300. [Google Scholar] [CrossRef] [Green Version]
- Mavel, S.; Nadal-Desbarats, L.; Blasco, H.; Bonnet-Brilhault, F.; Barthélémy, C.; Montigny, F.; Sarda, P.; Laumonnier, F.; Vourc′h, P.; Andres, C.R.; et al. 1H–13C NMR-based urine metabolic profiling in autism spectrum disorders. Talanta 2013, 114, 95–102. [Google Scholar] [CrossRef] [Green Version]
- Kałużna-Czaplińska, J. Noninvasive urinary organic acids test to assess biochemical and nutritional individuality in autistic children. Clin. Biochem. 2011, 44, 686–691. [Google Scholar] [CrossRef]
- Gątarek, P.; Jóźwik-Pruska, J.; Bjørklund, G.; Chirumbolo, S.; Kałużna-Czaplińska, J. Urinary carboxylic acids (UCAs) in subjects with autism spectrum disorder and their association with bacterial overgrowth. Rev. Anal. Chem. 2020, 39, 78–87. [Google Scholar] [CrossRef]
- Kałuzna-Czaplińska, J.; Socha, E.; Rynkowski, J. Determination of homovanillic acid and vanillylmandelic acid in urine of autistic children by gas chromatography/mass spectrometry. Med. Sci. Monit. 2010, 16, 445–450. [Google Scholar]
- Piras, C.; Mussap, M.; Noto, A.; De Giacomo, A.; Cristofori, F.; Spada, M.; Fanos, V.; Atzori, L.; Francavilla, R. Alterations of the Intestinal Permeability are Reflected by Changes in the Urine Metabolome of Young Autistic Children: Preliminary Results. Metabolites 2022, 12, 104. [Google Scholar] [CrossRef]
- Chamberlin, B.A.; Sweeley, C.C. Metabolic profiles of urinary organic acids recovered from absorbent filter paper. Clin. Chem. 1987, 33, 572–576. [Google Scholar] [CrossRef] [PubMed]
- Bralley, J.; Lord, R. Organic Acids. Laboratory Evaluations in Molecular Medicine: Nutrients, Toxicants, and Cell Regulators; Institute for Advances in Molecular Medicine: Norcross, GA, USA, 2001; pp. 175–208. [Google Scholar]
- Noto, A.; Fanos, V.; Barberini, L.; Grapov, D.; Fattuoni, C.; Zaffanello, M.; Casanova, A.; Fenu, G.; De Giacomo, A.; De Angelis, M.; et al. The urinary metabolomics profile of an Italian autistic children population and their unaffected siblings. J. Matern.-Fetal Neonatal Med. 2014, 27, 46–52. [Google Scholar] [CrossRef] [PubMed]
- Kuśmierek, K.; Głowacki, R.; Bald, E. Analysis of urine for cysteine, cysteinylglycine, and homocysteine by high-performance liquid chromatography. Anal. Bioanal. Chem. 2006, 385, 855–860. [Google Scholar] [CrossRef]
- Soldin, S.J.; Hill, J.G. Simultaneous liquid-chromatographic analysis for 4-hydroxy-3-methoxymandelic acid and 4-hydroxy-3-methoxyphenylacetic acid in urine. Clin. Chem. 1980, 26, 291–294. [Google Scholar] [CrossRef] [PubMed]
- Fu, B.; Chen, H.; Yan, Z.; Zhang, Z.; Chen, J.; Liu, T.; Li, K. A simple ultrasensitive electrochemical sensor for simultaneous determination of homovanillic acid and vanillylmandelic acid in human urine based on MWCNTs-Pt nanoparticles as peroxidase mimics. J. Electroanal. Chem. 2020, 866, 114165. [Google Scholar] [CrossRef]
- Wishart, D.S.; Jewison, T.; Guo, A.C.; Wilson, M.; Knox, C.; Liu, Y.; Djoumbou, Y.; Mandal, R.; Aziat, F.; Dong, E.; et al. HMDB 3.0—The Human Metabolome Database in 2013. Nucleic Acids Res. 2013, 41, D801–D807. [Google Scholar] [CrossRef]
- Southan, C.; DeWolf, W.E.; Kruse, L.I. Inactivation of dopamine β-hydroxylase by p-cresol: Evidence for a second, minor site of covalent modification at tyrosine 357. Biochim. Biophys. Acta (BBA) Protein Struct. Mol. Enzymol. 1990, 1037, 256–258. [Google Scholar] [CrossRef]
- Kosillo, P.; Bateup, H.S. Dopaminergic Dysregulation in Syndromic Autism Spectrum Disorders: Insights from Genetic Mouse Models. Front. Neural Circuits 2021, 15, 700968. [Google Scholar] [CrossRef]
- Adcock, J.; Barnett, N.W.; Costin, J.W.; Francis, P.; Lewis, S. Determination of selected neurotransmitter metabolites using monolithic column chromatography coupled with chemiluminescence detection. Talanta 2005, 67, 585–589. [Google Scholar] [CrossRef]
- Launay, J.-M.; Bursztejn, C.; Ferrari, P.; Dreux, C.; Braconnier, A.; Zarifian, E.; Lancrenon, S.; Fermanian, J. Catecholamines metabolism in infantile autism: A controlled study of 22 autistic children. J. Autism Dev. Disord. 1987, 17, 333–347. [Google Scholar] [CrossRef]
- Martineau, J.; Barthélémy, C.; Jouve, J.; Muh, J.-P.; Lelord, G. Monoamines (Serotonin and Catecholamines) And Their Derivatives in Infantile Autism: Age-Related Changes and Drug Effects. Dev. Med. Child Neurol. 2008, 34, 593–603. [Google Scholar] [CrossRef] [PubMed]
- Shaw, W. Increased urinary excretion of a 3-(3-hydroxyphenyl)-3-hydroxypropionic acid (HPHPA), an abnormal phenylalanine metabolite ofClostridiaspp. in the gastrointestinal tract, in urine samples from patients with autism and schizophrenia. Nutr. Neurosci. 2010, 13, 135–143. [Google Scholar] [CrossRef] [PubMed]
- Sikorski, Z.E. Chemia Żywności: Odżywcze i Zdrowotne Właściwości Składników Żywności; Wydawnictwo Naukowo-Techniczne: Warsaw, Poland, 2007; Volume 3, pp. 25–29. [Google Scholar]
- Gabriele, S.; Sacco, R.; Persico, A.M. Blood serotonin levels in autism spectrum disorder: A systematic review and meta-analysis. Eur. Neuropsychopharmacol. 2014, 24, 919–929. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, K.; Sekine, Y.; Ouchi, Y.; Tsujii, M.; Yoshikawa, E.; Futatsubashi, M.; Tsuchiya, K.; Sugihara, G.; Iwata, Y.; Suzuki, K.; et al. Brain Serotonin and Dopamine Transporter Bindings in Adults with High-Functioning Autism. Arch. Gen. Psychiatry 2010, 67, 59–68. [Google Scholar] [CrossRef] [Green Version]
- Shaw, W. Dopamine excess and/or norepinephrine and epinephrine deficiency in autistic patients due to prenatal and/or postnatal deficiency of dopamine beta-hydroxylase. J. Orthomol. Med. 2021, 36. [Google Scholar]
- Lelord, G.; Callaway, E.; Muh, J.P.; Arlot, J.C.; Sauvage, D.; Garreau, B.; Domenech, J. Modifications in urinary homo-vanillic acid after ingestion of vitamin B6; functional study in autistic children. Rev. Neurol. 1978, 134, 797–801. [Google Scholar]
- Kałużna-Czaplińska, J.; Socha, E.; Rynkowski, J. B vitamin supplementation reduces excretion of urinary dicarboxylic acids in autistic children. Nutr. Res. 2011, 31, 497–502. [Google Scholar] [CrossRef]
- Berg, J.M.; Tymoczko, J.L.; Stryer, L. Biochemia, 3rd ed.; Wydawnictwo Naukowe PWN: Warsaw, Poland, 2005; pp. 482–485. [Google Scholar]
- Blaylock, R.L.; Strunecka, A. Immune-glutamatergic dysfunction as a central mechanism of the autism spectrum disorders. Curr. Med. Chem. 2009, 16, 157–170. [Google Scholar] [CrossRef] [Green Version]
- Dolske, M.C.; Spollen, J.; McKay, S.; Lancashire, E.; Tolbert, L. A preliminary trial of ascorbic acid as supplemental therapy for autism. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 1993, 17, 765–774. [Google Scholar] [CrossRef]
- Sheppard, K.W.; Boone, K.M.; Gracious, B.; Klebanoff, M.A.; Rogers, L.K.; Rausch, J.; Bartlett, C.; Coury, D.L.; Keim, S.A. Effect of Omega-3 and -6 Supplementation on Language in Preterm Toddlers Exhibiting Autism Spectrum Disorder Symptoms. J. Autism Dev. Disord. 2017, 47, 3358–3369. [Google Scholar] [CrossRef]
- Amminger, G.P.; Berger, G.E.; Schäfer, M.R.; Klier, C.; Friedrich, M.H.; Feucht, M. Omega-3 Fatty Acids Supplementation in Children with Autism: A Double-blind Randomized, Placebo-controlled Pilot Study. Biol. Psychiatry 2007, 61, 551–553. [Google Scholar] [CrossRef] [PubMed]
- Bent, S.; Hendren, R.L.; Zandi, T.; Law, K.; Choi, J.-E.; Widjaja, F.; Kalb, L.; Nestle, J.; Law, P. Internet-Based, Randomized, Controlled Trial of Omega-3 Fatty Acids for Hyperactivity in Autism. J. Am. Acad. Child Adolesc. Psychiatry 2014, 53, 658–666. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hibbeln, J.R.; Ferguson, T.A.; Blasbalg, T.L. Omega-3 fatty acid deficiencies in neurodevelopment, aggression and autonomic dysregulation: Opportunities for intervention. Int. Rev. Psychiatry 2006, 18, 107–118. [Google Scholar] [CrossRef] [PubMed]
- Garland, M.R.; Hallahan, B. Essential fatty acids and their role in conditions characterised by impulsivity. Int. Rev. Psychiatry 2006, 18, 99–105. [Google Scholar] [CrossRef]
- Johnson, S.M.; Hollander, E. Evidence that eicosapentaenoic acid is effective in treating autism. J. Clin. Psychiatry 2003, 64, 848–849. [Google Scholar] [CrossRef] [Green Version]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5®); American Psychiatric Association: Washington, DC, USA, 2013. [Google Scholar]
- Turck, D.; Michaelsen, K.F.; Shamir, R.; Braegger, C.; Campoy, C.; Colomb, V.; Decsi, T.; Domellöf, M.; Fewtrell, M.; Kolacek, S.; et al. World health organization 2006 child growth standards and 2007 growth reference charts: A discussion paper by the committee on nutrition of the European society for pediatric gastroenterology, hepatology, and nutrition. J. Pediatr. Gastroenterol. Nutr. 2013, 57, 258–264. [Google Scholar] [CrossRef]
- Różdżyńska-Świątkowska, A.; Kułaga, Z.; Grajda, A. Wartości Referencyjne Wysokości, Masy Ciała i Wskaźnika Masy CIAŁA dla Oceny Wzrastania i Stanu Odżywienia Dzieci i Młodzieży w Wieku 3-18 lat. Stand. Med. Ped. 2013, 10, 11–21. [Google Scholar]
- Kułaga, Z.; Różdżyńska-Świątkowska, A.; Grajda, A.; Gurzkowska, B.; Wojtyło, M.; Góźdź, M.; Świąder-Leśniak, A.; Litwin, M. Percentile charts for growth and nutritional status assessment in Polish children and adolescents from birth to 18 year of age. Stand. Med. Ped. 2015, 12, 119–135. [Google Scholar]
- Cole, T.J.; Bellizzi, M.C.; Flegal, K.M.; Dietz, W.H. Establishing a standard definition for child overweight and obesity worldwide: International survey. BMJ 2000, 320, 1240–1243. [Google Scholar] [CrossRef] [Green Version]
- Cole, T.J.; Flegal, K.M.; Nicholls, D.; Jackson, A.A. Body mass index cut offs to define thinness in children and adolescents: International survey. BMJ 2007, 335, 194. [Google Scholar] [CrossRef] [Green Version]
- Zhang, Q.; Wang, G.; Du, Y.; Zhu, L.; Jiye, A. GC/MS analysis of the rat urine for metabonomic research. J. Chromatogr. B Anal. Technol. Biomed. Life Sci. 2007, 854, 20–25. [Google Scholar] [CrossRef] [PubMed]
- Allenbrand, R.; Garg, U. Quantitation of Homovanillic Acid (HVA) and Vanillylmandelic Acid (VMA) in Urine Using Gas Chromatography-Mass Spectrometry (GC/MS). Methods Mol. Biol. 2010, 603, 261–269. [Google Scholar] [CrossRef] [PubMed]
- Pautova, A.K.; Bedova, A.Y.; Sarshor, Y.N.; Beloborodova, N.V. Determination of Aromatic Microbial Metabolites in Blood Serum by Gas Chromatography–Mass Spectrometry. J. Anal. Chem. 2018, 73, 160–166. [Google Scholar] [CrossRef]
- Park, N.H.; Hong, J.Y.; Shin, H.J.; Hong, J. Comprehensive profiling analysis of bioamines and their acidic metabolites in human urine by gas chromatography/mass spectrometry combined with selective derivatization. J. Chromatogr. A 2013, 1305, 234–243. [Google Scholar] [CrossRef]
- Tran, M.T.C.; Baglin, J.; Tran, T.T.T.; Hoang, K.T.; Phung, L.T.; Read, A.; Greaves, R.F. Development of a new biochemical test to diagnose and monitor neuroblastoma in Vietnam: Homovanillic and vanillylmandelic acid by gas chromatography–mass spectrometry. Clin. Biochem. 2014, 47, 206–215. [Google Scholar] [CrossRef]





| Name of Compound | Unit | Supplementation | Mean ± SD | Median | Min | Max | LQ | UQ | SE | p-Value * | References Values ** |
|---|---|---|---|---|---|---|---|---|---|---|---|
| HVA | μmol/mmol creatinine | yes | 26.62 ± 12.54 | 24.27 | 8.10 | 85.51 | 18.61 | 32.10 | 1.25 | 7.99 × 10−8 | 9.74 ± 3.99 |
| no | 30.04 ± 13.32 | 27.58 | 11.35 | 68.42 | 20.38 | 38.01 | 2.66 | ||||
| VMA | yes | 12.92 ± 8.32 | 11.19 | 0.33 | 56.82 | 7.19 | 16.76 | 0.82 | 2.70 × 10−9 | 7.76 ± 2.94 | |
| no | 11.25 ± 4.15 | 11.87 | 0.90 | 19.18 | 8.00 | 14.27 | 0.83 |
| Name of Compound | Unit | Mean ± SD | p-Value | |||||
|---|---|---|---|---|---|---|---|---|
| Vitamin B | Vitamin C | Vitamin D | Omega-3 | Omega-6 | Probiotic | |||
| HVA | μmol/mmol creatinine | 27.31 ± 12.72 | 0.0164 | 0.8679 | 0.9823 | 0.4189 | 0.0015 | 0.1376 |
| VMA | 12.59 ± 7.70 | 0.3620 | 0.3876 | 0.1638 | 0.8189 | 0.0025 | 0.3962 | |
| Number of Analyzed Samples | N = 129 | Boys = 120 |
|---|---|---|
| Girls = 9 | ||
| Age Ranges | 3–18 years of age | |
| number of underweight children | 13 | |
| number of normal weight children | 93 | |
| number of overweight children | 22 | |
| number of children with obesity | 1 | |
| Supplementation | Dose/Composition | ||||
|---|---|---|---|---|---|
| Yes | No | Min. | Max. | ||
| Omega-3 | EPA | 60 | 69 | 92 mg | 800 mg |
| DHA | 60 | 69 | 26 mg | 400 mg | |
| Omega-6 | GLA | 19 | 69 | 10.5 mg | 48.2 mg |
| LA | 7 | 69 | 348 mg | 2000 mg | |
| Vitamin C | 58 | 71 | 50 mg | 2200 mg | |
| Vitamin D3 | 66 | 63 | 200 IU (5 μg) | 2000 IU (50 μg) | |
| Vitamins B | B1 | 6 | 103 | 50 mg | 100 mg |
| B3 | 6 | 97 | 8 mg | 16 mg | |
| B6 | 26 | 97 | 2.5 μg | 200 mg | |
| B12 | 17 | 97 | 1 μg | 10 mg | |
| Probiotics | 50 | 79 | Contains no less than 2.5 billion Lactobacillus, Bifidobacterium, Streptococcus and Lactococcus bacteria. | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gątarek, P.; Kałużna-Czaplińska, J. Effect of Supplementation on Levels of Homovanillic and Vanillylmandelic Acids in Children with Autism Spectrum Disorders. Metabolites 2022, 12, 423. https://doi.org/10.3390/metabo12050423
Gątarek P, Kałużna-Czaplińska J. Effect of Supplementation on Levels of Homovanillic and Vanillylmandelic Acids in Children with Autism Spectrum Disorders. Metabolites. 2022; 12(5):423. https://doi.org/10.3390/metabo12050423
Chicago/Turabian StyleGątarek, Paulina, and Joanna Kałużna-Czaplińska. 2022. "Effect of Supplementation on Levels of Homovanillic and Vanillylmandelic Acids in Children with Autism Spectrum Disorders" Metabolites 12, no. 5: 423. https://doi.org/10.3390/metabo12050423
APA StyleGątarek, P., & Kałużna-Czaplińska, J. (2022). Effect of Supplementation on Levels of Homovanillic and Vanillylmandelic Acids in Children with Autism Spectrum Disorders. Metabolites, 12(5), 423. https://doi.org/10.3390/metabo12050423