Alterations in Blood Plasma Metabolome of Patients with Lesniowski-Crohn’s Disease Shortly after Surgical Treatment—Pilot Study
Abstract
:1. Introduction
2. Results
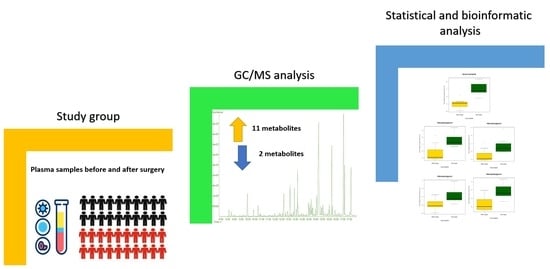
3. Discussion
4. Materials and Methods
4.1. Characteristics of Patients
4.2. Blood Collection
4.3. Metabolites Extraction and Derivatization
4.4. GC/MS System and Spectra Processing
4.5. Statistical and Bioinformatic Analysis
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Gajendran, M.; Loganathan, P.; Catinella, A.P.; Hashash, J.G. A comprehensive review and update on Crohn’s disease. Dis. Mon. 2018, 64, 20–57. [Google Scholar] [CrossRef] [PubMed]
- Ha, F.; Khalil, H. Crohn’s disease: A clinical update. Ther. Adv. Gastroenterol. 2015, 8, 352–359. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Higgins, P.D.R.; Harding, G.; Leidy, N.K.; DeBusk, K.; Patrick, D.L.; Viswanathan, H.N.; Fitzgerald, K.; Donelson, S.M.; Cyrille, M.; Ortmeier, B.G.; et al. Development and validation of the Crohn’s disease patient-reported outcomes signs and symptoms (CD-PRO/SS) diary. J. Patient-Rep. Outcomes 2018, 2, 24. [Google Scholar] [CrossRef]
- Shah, S.B.; Hanauer, S.B. Treatment of diarrhea in patients with inflammatory bowel disease: Concepts and cautions. Rev. Gastroenterol. Disord. 2007, 7, 3–10. [Google Scholar]
- Tigas, S.; Tsatsoulis, A. Endocrine and metabolic manifestations in inflammatory bowel disease. Ann. Gastroenterol. 2012, 25, 37–44. [Google Scholar]
- Sugihara, K.; Morhardt, T.L.; Kamada, N. The Role of Dietary Nutrients in Inflammatory Bowel Disease. Front. Immunol. 2019, 9, 3183. [Google Scholar] [CrossRef]
- Daniluk, U.; Daniluk, J.; Kucharski, R.; Kowalczyk, T.; Pietrowska, K.; Samczuk, P.; Filimoniuk, A.; Kretowski, A.; Lebensztejn, D.; Ciborowski, M. Untargeted Metabolomics and Inflammatory Markers Profiling in Children With Crohn’s Disease and Ulcerative Colitis—A Preliminary Study. Inflamm. Bowel. Dis. 2019, 25, 1120–1128. [Google Scholar] [CrossRef]
- Bemelman, W.A.; Warusavitarne, J.; Sampietro, G.M.; Serclova, Z.; Zmora, O.; Luglio, G.; de Buck van Overstraeten, A.; Burke, J.P.; Buskens, C.J.; Colombo, F.; et al. ECCO-ESCP Consensus on Surgery for Crohn’s Disease. J. Crohns Colitis. 2018, 12, 1–16. [Google Scholar] [CrossRef]
- Vermeire, S.; Van Assche, G.; Rutgeerts, P. Laboratory markers in IBD: Useful, magic, or unnecessary toys? Gut 2006, 55, 426–431. [Google Scholar] [CrossRef] [Green Version]
- Sobotka, L.; Soeters, P.B. Basics in clinical nutrition: Metabolic response to injury and sepsis. Eur. J. Clin. Nutr. 2009, 4, e1–e3. [Google Scholar] [CrossRef] [Green Version]
- Şimşek, T.; Şimşek, H.U.; Cantürk, N.Z. Response to trauma and metabolic changes: Posttraumatic metabolism. Ulus. Cerrahi. Derg. 2014, 30, 153–159. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aon, M.A.; Bhatt, N.; Cortassa, S.C. Mitochondrial and cellular mechanisms for managing lipid excess. Front. Physiol. 2014, 5, 282. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gurr, M.I.; Harwood, J.L.; Frayn, K.N.; Murphy, D.J.; Michell, R.H. Lipids: Biochemistry, Biotechnology and Health, 6th ed.; Wiley-Blackwell: Hoboken, NJ, USA, 2016; ISBN 978-1-118-50113-9. [Google Scholar]
- Coelho, A.I.; Berry, G.T.; Rubio-Gozalbo, M.E. Galactose metabolism and health. Curr. Op. Clin. Nut. Metab. Care 2015, 18, 422–427. [Google Scholar] [CrossRef] [PubMed]
- Mráček, T.; Drahota, Z.; Houštěk, J. The function and the role of the mitochondrial glycerol-3-phosphate dehydrogenase in mammalian tissues. Biochim. Biophys. Acta 2013, 1827, 401–410. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mosharov, E.; Crawford, M.R.; Banerjee, R. The quantitatively important relationship between homocysteine metabolism and glutathione synthesis by the transulfuration pathway and its regulation by redox changes. Biochemistry 2000, 39, 13005–13011. [Google Scholar] [CrossRef]
- Brosnan, J.T.; Brosnan, M.E. The Sulfur-Containing Amino Acids: An Overview. J. Nutr. 2006, 136, 1636S–1640S. [Google Scholar] [CrossRef] [Green Version]
- Lauridsen, C.; Jensen, S.K. α-Tocopherol incorporation in mitochondria and microsomes upon supranutritional vitamin E supplementation. Genes Nutr. 2012, 7, 475–482. [Google Scholar] [CrossRef] [Green Version]
- Stephens, N.S.; Siffledeen, J.; Su, X.; Murdoch, T.B.; Fedorak, R.N.; Slupsky, C.M. Urinary NMR metabolomic profiles discriminate inflammatory bowel disease from healthy. J. Crohns Colitis 2013, 7, E42–E48. [Google Scholar] [CrossRef] [Green Version]
- Williams, H.R.; Cox, I.J.; Walker, D.G.; North, B.V.; Patel, V.M.; Marshall, S.E.; Jewell, D.P.; Ghosh, S.; Thomas, H.J.; Teare, J.P.; et al. Characterization of inflammatory bowel disease with urinary metabolic profiling. Am. J. Gastroenterol. 2009, 104, 1435–1444. [Google Scholar] [CrossRef]
- Martin, F.-P.; Ezri, J.; Cominetti, O.; Da Silva, L.; Kussmann, M.; Godin, J.-P.; Nydegger, A. Urinary metabolic phenotyping reveals differences in the metabolic status of healthy and inflammatory bowel disease (IBD) children in relation to growth and disease activity. Int. J. Mol. Sci. 2016, 17, 1310. [Google Scholar] [CrossRef] [Green Version]
- Dawiskiba, T. Serum and urine metabolomic fingerprinting in diagnostics of inflammatory bowel diseases. World J. Gastroenterol. 2014, 20, 163. [Google Scholar] [CrossRef] [PubMed]
- Ooi, M.; Nishiumi, S.; Yoshie, T.; Shiomi, Y.; Kohashi, M.; Fukunaga, K.; Nakamura, S.; Matsumoto, T.; Hatano, N.; Shinohara, M.; et al. GC/MS-based profiling of amino acids and TCA cycle-related molecules in ulcerative colitis. Inflamm. Res. 2011, 60, 831–840. [Google Scholar] [CrossRef] [PubMed]
- Chen, R.; Zheng, J.; Li, L.; Li, C.; Chao, K.; Zeng, Z.; Chen, M.; Zhang, S. Metabolomics facilitate the personalized management in inflammatory bowel disease. Ther. Adv. Gastroenterol. 2021, 14, 175628482110644. [Google Scholar] [CrossRef] [PubMed]
- Bischoff, S.C.; Escher, J.; Hébuterne, X.; Kłęk, S.; Krznaric, Z.; Schneider, S.; Shamir, R.; Stardelova, K.; Wierdsma, N.; Wiskin, A.E.; et al. ESPEN practical guideline: Clinical Nutrition in inflammatory bowel disease. Clin. Nutr. 2020, 39, 632–653. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Harvey, R.F.; Bradshaw, J.M. A simple index of Crohn’s-disease activity. Lancet 1980, 315, 514. [Google Scholar] [CrossRef]
- Fiehn, O. Metabolomics by Gas Chromatography-Mass Spectrometry: Combined Targeted and Untargeted Profiling. Curr. Protoc. Mol. Biol. 2016, 114, 30.4.1–30.4.32. [Google Scholar] [CrossRef]
- Tsugawa, H.; Cajka, T.; Kind, T.; Ma, Y.; Higgins, B.; Ikeda, K.; Kanazawa, M.; VanderGheynst, J.; Fiehn, O.; Arita, M. MS-Dial: Data-independent MS/MS Deconvolution for Comprehensive Metabolome Analysis. Nat. Methods 2015, 12, 523–526. [Google Scholar] [CrossRef]
- Xia, J.; Wishart, D.S. MSEA: A web-based tool to identify biologically meaningful patterns in quantitative metabolomic data. Nucleic Acids Res. 2010, 38, 71–77. [Google Scholar] [CrossRef] [Green Version]



| Patient ID | Protein [g/dL] | Electrolytes | Glucose [mg/dL] | CRP [mg/L] | Creatinine [mg/dL] | AST [U/L] | ALT [U/L] | Urea [mg/dL] | Coagulation System [s] | |||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | Albumins | Na [mM] | K [mM] | Ca [mg/dL] | Mg [mg/dL] | Pinorg. [mg/dL] | PT | INR | APTT | |||||||||||||||||||||||
| B | A | B | A | B | A | B | A | B | A | B | A | B | A | B | A | B | A | B | A | B | A | B | A | B | A | B | A | B | A | B | A | |
| 1 | 5.0 | 5.1 | 2.9 | 2.3 | 143 | 139 | 4.5 | 4.4 | 8.5 | 8.2 | 2.3 | 2.6 | 3.5 | 3.8 | 97 | 71 | 52 | 95 | 0.80 | 0.82 | 18 | 20 | 13 | 26 | 46 | 42 | 11.9 | 12.2 | 0.99 | 1.01 | 30 | 32 |
| 2 | 6.2 | 5.4 | 3.1 | 3.1 | 138 | 137 | 4.4 | 4.5 | 7.6 | 8.3 | 1.7 | 2.1 | 1.8 | 3.5 | 75 | 84 | 193 | 225 | 0.58 | 0.65 | no data | no data | no data | no data | 8 | 16 | 13.7 | 15.8 | 1.14 | 1.31 | 33 | 40 |
| 3 | 6.7 | 6.4 | 3.0 | 2.7 | 140 | 144 | 4.0 | 3.7 | 8.2 | 7.6 | 1.6 | 2.1 | 3.3 | 3.7 | 106 | 83 | 85 | 132 | 0.88 | 0.78 | 15 | 17 | 23 | 42 | 18 | 41 | 13.3 | 15.8 | 1.17 | 1.41 | 40 | 40 |
| 4 | 5.7 | 4.9 | 2.8 | 2.2 | 140 | 139 | 4.0 | 2.7 | 7.8 | 7.9 | 1.8 | 1.9 | 3.2 | 2.9 | 113 | 107 | 2 | 126 | 0.73 | 0.63 | 16 | 22 | 34 | 29 | 15 | 24 | 11.2 | 10.7 | 0.93 | 0.99 | 30 | 33 |
| 5 | 5.9 | 5.7 | 2.8 | 2.8 | 140 | 142 | 3.3 | 5.0 | 8.1 | 8.8 | 2.0 | 2.8 | 3.1 | 3.0 | 101 | 82 | 76 | 29 | 0.85 | 0.97 | 44 | 52 | 39 | 66 | 20 | 19 | 12.3 | 11.8 | 1.10 | 1.04 | 32 | 28 |
| 6 | 6.8 | 7.0 | 4.2 | 3.8 | 140 | 138 | 4.1 | 4.3 | 8.8 | 8.9 | 1.7 | 1.8 | 2.4 | 3.3 | 60 | 99 | 2 | 84 | 1.15 | 0.93 | 21 | 33 | 15 | 36 | 25 | 26 | 11.3 | 11.2 | 0.99 | 0.94 | 29 | 31 |
| 7 | 6.2 | 6.2 | 2.8 | 3.0 | 139 | 141 | 4.8 | 4.6 | 8.1 | 8.4 | 2.0 | 1.6 | 2.9 | 2.7 | 76 | 91 | 181 | 100 | 0.65 | 0.69 | 16 | 11 | 23 | 35 | 14 | 26 | 11.5 | 11.9 | 1.02 | 1.06 | 33 | 33 |
| Clinical Parameter | Before Surgery | After Surgery | Laboratory Norms | Statistic | p Value | FDR Adjusted p Value | Remarks |
|---|---|---|---|---|---|---|---|
| Total protein [g/dL] | 6.1 ± 0.5 | 5.8 ± 0.8 | 6.0–8.3 | −1.56 | 0.177 | 0.40 | ns |
| Albumin [g/dL] | 3.1 ± 0.5 | 2.8 ± 0.5 | 3.4–5.4 | −2.04 | 0.09 | 0.40 | ns |
| Total cholesterol [mg/dL] | 121.3 ± 30.6 | 157.0 ± 19.1 | <200 | - | - | - | 1 |
| TG [mg/dL] | 76.0 ± 33.8 | 118.7 ± 18.6 | <150 | - | - | - | 1 |
| Na [mM] | 140.0 ± 1.5 | 140.0 ± 2.4 | 135–147 | 0.00 | 1.00 | 1.00 | ns |
| K [mM] | 4.2 ± 0.5 | 4.2 ± 0.8 | 3.0–5.5 | 0.04 | 0.97 | 1.00 | ns |
| Ca [mg/dL] | 8.1 ± 0.4 | 8.3 ± 0.5 | 8.6–10.3 | 0.84 | 0.43 | 0.58 | ns |
| Mg [mg/dL] | 1.9 ± 0.2 | 2.1 ± 0.4 | 1.8–2.4 | 1.80 | 0.12 | 0.40 | ns |
| Phosphorus (inorganic) [mg/dL] | 2.9 ± 0.6 | 3.3 ± 0.4 | 2.5–4.5 | 1.43 | 0.20 | 0.40 | ns |
| Glucose [mg/dL] | 89.7 ± 19.5 | 88.1 ± 12.0 | 72.0–99.0 | −0.17 | 0.87 | 0.99 | ns |
| CRP [mg/L] | 84.3 ± 77.2 | 113.0 ± 59.7 | <3.0 | 1.07 | 0.33 | 0.47 | ns |
| Creatinine [mg/dL] | 0.81 ± 0.19 | 0.78 ± 0.13 | 0.84–1.21 | −0.54 | 0.61 | 0.75 | ns |
| AST [U/L] | 21.7 ± 11.1 | 25.8 ± 14.7 | 8.0–48.0 | 1.74 | 0.14 | 0.40 | ns, 2 |
| ALT [U/L] | 24.5 ± 10.3 | 39.0 ± 14.4 | 7.0–55.0 | 3.22 | 0.02 | 0.37 | p, ns, 2 |
| Urea [mg/dL] | 20.9 ± 12.3 | 27.7 ± 10.1 | 7.0–20.0 | 1.97 | 0.10 | 0.40 | ns |
| PT [s] | 12.2 ± 1.0 | 12.7 ± 2.1 | 11.0–13.5 | 1.22 | 0.27 | 0.47 | ns |
| INR [s] | 1.0 ± 0.1 | 1.1 ± 0.2 | 0.8–1.1 | 1.44 | 0.20 | 0.40 | ns |
| APTT [s] | 32.4 ± 3.5 | 33.8 ± 4.6 | 30.0–40.0 | 1.10 | 0.31 | 0.47 | ns |
| Metabolite | Class of Metabolites | RT [min] | Mean [a.u.] | C.V. | Mean [a.u.] | C.V. | After/Before Ratio | p Value | FDR p Value |
|---|---|---|---|---|---|---|---|---|---|
| Glycerol-3-phosphate | Phosphoric acid deriv. | 13.12 | 0.144 | 0.518 | 0.622 | 0.657 | 4.33 | 0.00125 | 0.029 |
| α-Tocopherol | Lipids | 23.26 | 0.291 | 0.886 | 0.991 | 0.599 | 3.40 | 0.00845 | 0.140 |
| 1-Monopalmitoylglycerol | Lipids | 19.17 | 1.385 | 1.209 | 3.858 | 0.833 | 2.79 | 0.00010 | 0.004 |
| 2-Monopalmitoylglycerol | Lipids | 18.9 | 0.102 | 0.786 | 0.279 | 0.703 | 2.74 | 0.00006 | 0.004 |
| 1-Monostearoylglycerol | Lipids | 20.34 | 0.864 | 0.751 | 2.272 | 1.045 | 2.63 | 0.00008 | 0.004 |
| Succinic acid | Carboxylic acids | 8.46 | 1.482 | 0.841 | 3.705 | 1.055 | 2.50 | 0.04682 | 0.362 |
| 2-Monostearoylglycerol | Lipids | 20.1 | 0.075 | 0.534 | 0.176 | 0.814 | 2.35 | 0.00012 | 0.004 |
| L-Cysteine | Amino acids | 11.1 | 1.938 | 0.929 | 4.214 | 0.444 | 2.17 | 0.03241 | 0.342 |
| L-Methionine | Amino acids | 10.74 | 1.645 | 0.848 | 3.364 | 0.462 | 2.05 | 0.04194 | 0.362 |
| L-Lysine | Amino acids | 14.36 | 2.989 | 0.930 | 5.814 | 0.257 | 1.95 | 0.02451 | 0.315 |
| Benzoic acid ** | Carboxylic acids | 7.81 | 0.922 | 0.560 | 1.449 | 0.361 | 1.57 | 0.00511 | 0.099 |
| 3,4-Dihydroxybutanoic acid | Carboxylic acids | 9.8 | 0.452 | 0.728 | 0.151 | 0.637 | 0.33 | 0.02717 | 0.315 |
| Galactopyranose | Sugars | 14.32 | 7.096 | 1.336 | 0.661 | 1.462 | 0.09 | 0.01396 | 0.202 |
| Ribonic acid * | Sugar deriv. | 13.35 | 7/7 | 2/7 | NA |
| Patient ID | Gender | Age | Disease State |
|---|---|---|---|
| 1 | M | 42 | active |
| 2 | F | 29 | active |
| 3 | M | 43 | active |
| 4 | F | 52 | active |
| 5 | F | 60 | active |
| 6 | M | 24 | active |
| 7 | F | 26 | active |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Idkowiak, J.; Kubiak-Tomaszewska, G.; Gątarek, P.; Marczak, Ł.; Kałużna-Czaplińska, J.; Tarnowski, W.; Uryszek, M.; Bobrowska-Korczak, B. Alterations in Blood Plasma Metabolome of Patients with Lesniowski-Crohn’s Disease Shortly after Surgical Treatment—Pilot Study. Metabolites 2022, 12, 529. https://doi.org/10.3390/metabo12060529
Idkowiak J, Kubiak-Tomaszewska G, Gątarek P, Marczak Ł, Kałużna-Czaplińska J, Tarnowski W, Uryszek M, Bobrowska-Korczak B. Alterations in Blood Plasma Metabolome of Patients with Lesniowski-Crohn’s Disease Shortly after Surgical Treatment—Pilot Study. Metabolites. 2022; 12(6):529. https://doi.org/10.3390/metabo12060529
Chicago/Turabian StyleIdkowiak, Jakub, Grażyna Kubiak-Tomaszewska, Paulina Gątarek, Łukasz Marczak, Joanna Kałużna-Czaplińska, Wiesław Tarnowski, Mariusz Uryszek, and Barbara Bobrowska-Korczak. 2022. "Alterations in Blood Plasma Metabolome of Patients with Lesniowski-Crohn’s Disease Shortly after Surgical Treatment—Pilot Study" Metabolites 12, no. 6: 529. https://doi.org/10.3390/metabo12060529
APA StyleIdkowiak, J., Kubiak-Tomaszewska, G., Gątarek, P., Marczak, Ł., Kałużna-Czaplińska, J., Tarnowski, W., Uryszek, M., & Bobrowska-Korczak, B. (2022). Alterations in Blood Plasma Metabolome of Patients with Lesniowski-Crohn’s Disease Shortly after Surgical Treatment—Pilot Study. Metabolites, 12(6), 529. https://doi.org/10.3390/metabo12060529