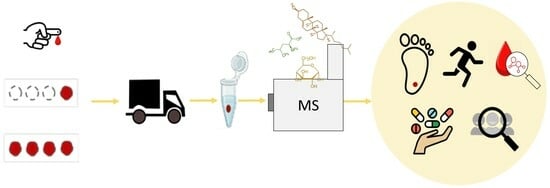
Revolutionizing Blood Collection: Innovations, Applications, and the Potential of Microsampling Technologies for Monitoring Metabolites and Lipids
Abstract
:1. Introduction
2. Microsampling Devices
2.1. Dried Blood Spot (DBS)
2.1.1. DBS on Filter Paper
2.1.2. Capitainer® B Quantitative DBS (qDBS)
2.1.3. HemaSpotTM HF
2.1.4. HemaSpotTM SE
2.1.5. Telimmune Plasma Separation Card
2.2. Volumetric Tip Microsampling
2.2.1. Volumetric Absorptive Microsampling
2.2.2. TASSO M-20
2.3. Microneedle-Based Devices
2.3.1. TAP Capillary
2.3.2. HemaPEN®
3. Stability
3.1. Metabolome Stability for Untargeted Metabolomics
3.2. Targeted Metabolite Stability
4. Extraction Procedure
4.1. Extraction of Untargeted Metabolites
4.2. Extraction of Targeted Metabolites
| Type | Sample | Extraction | Source |
|---|---|---|---|
| DBS | whole blood | 125 µL MeOH 200 µL IPA | [59] |
| DBS | whole blood | 225 µL MeOH:H2O (80:20, v/v) + 0.01% FA | [29] |
| DBS | whole blood plasma | 100 µL MeOH:H2O (4:1, v/v) 80 µL MeOH | [5] |
| DBS | whole blood | 100 µL MeOH (80%) | [23] |
| DBS | whole blood | 450 µL MeOH + 150 MTBE | [63] |
| DBS | whole blood | 20 µL, 50 µL, 200 µL MeOH 20 µL, 50 µL, 200 µL ACN 20 µL, 50 µL, 200 µL MeOH/ACN (1:1 v/v) | [57] |
| DBS | whole blood | 40 µL H2O + 160 µL MeOH | [3] |
| DBS | whole blood | 225 µL MeOH/H2O (80:20 v/v) + 0.01% FA | [29] |
| DBS | whole blood plasma | 200 µL MeOH:ACN:H2O (40:40:20, v/v/v) | [58] |
| DBS | whole blood | 4 mL CHCl3/MeOH (1:1 v/v) + 1.6 mL LiCl solution (50 mM) | [64] |
| DBS | whole blood | MeOH/CHCl3 (90:10 v/v) | [54] |
| hemaPEN® | whole blood | ACN:H2O (60:40 v/v) | [18] |
| hemaPEN® | whole blood | MeOH:H2O (80:20, v/v) | [48] |
| hemaPEN® | whole blood | 70 µL MeOH:H2O (80:20, v/v) + 0,01% formic acid | [47] |
| VAMS | whole blood | MeOH:H2O (80:20, v:v) MeOH:H2O (60:40, v:v) | [61] |
| VAMS | whole blood | 200 µL MeOH | [62] |
| VAMS | whole blood | MeOH/MBTE (50:50 v/v) | [54] |
| TELIMMUNE | plasma |
| [55] |
| TELIMMUNE | plasma | 500 µL MeOH: H2O (50:50, v:v) | [36] |
| TELIMMUNE | plasma | 20 µL MeOH | [35] |
| TELIMMUNE | plasma | 25 µL of phosphate-buffered saline (pH 7.4) | [65] |
5. Microsampling Applications Monitoring Lipids and Metabolites
5.1. Population Studies and Newborn Screening
5.2. Nutritional Studies
5.3. Drug Discovery
5.4. Microsampling in Sport
5.5. Multi-Omics and Microsampling
6. Conclusions and Future Directions
Author Contributions
Funding
Conflicts of Interest
References
- Thangavelu, M.U.; Wouters, B.; Kindt, A.; Reiss, I.K.M.; Hankemeier, T. Blood Microsampling Technologies: Innovations and Applications in 2022. Anal. Sci. Adv. 2023, 4, 5–6. [Google Scholar] [CrossRef]
- Lei, B.U.W.; Prow, T.W. A Review of Microsampling Techniques and Their Social Impact. Biomed. Microdevices 2019, 21, 81. [Google Scholar] [CrossRef] [PubMed]
- Trifonova, O.P.; Maslov, D.L.; Balashova, E.E.; Lokhov, P.G. Evaluation of Dried Blood Spot Sampling for Clinical Metabolomics: Effects of Different Papers and Sample Storage Stability. Metabolites 2019, 9, 277. [Google Scholar] [CrossRef] [PubMed]
- Lehmann, S.; Delaby, C.; Vialaret, J.; Ducos, J.; Hirtz, C. Current and Future Use of “Dried Blood Spot” Analyses in Clinical Chemistry. Clin. Chem. Lab. Med. 2013, 51, 1897–1909. [Google Scholar] [CrossRef]
- Palmer, E.A.; Cooper, H.J.; Dunn, W.B. Investigation of the 12-Month Stability of Dried Blood and Urine Spots Applying Untargeted UHPLC-MS Metabolomic Assays. Anal. Chem. 2019, 91, 14306–14313. [Google Scholar] [CrossRef]
- Fedoruk, M.N. Virtual Drug Testing: Redefining Sample Collection in a Global Pandemic. Bioanalysis 2020, 12, 715–718. [Google Scholar] [CrossRef]
- Coombes, E.J.; Gamlen, T.R.; Batstone, G.F.; Leigh, P.N. A Phenytoin Assay Using Dried Blood Spot Samples Suitable for Domiciliary Therapeutic Drug Monitoring. Ann. Clin. Biochem. 1984, 21, 519–522. [Google Scholar] [CrossRef]
- Fujimoto, T.; Tsuda, Y.; Tawa, R.; Hirose, S. Fluorescence Polarization Immunoassay of Gentamicin or Netilmicin in Blood Spotted on Filter Paper. Clin. Chem. 1989, 35, 867–869. [Google Scholar] [CrossRef]
- Cafaro, A.; Conti, M.; Pigliasco, F.; Barco, S.; Bandettini, R.; Cangemi, G. Biological Fluid Microsampling for Therapeutic Drug Monitoring: A Narrative Review. Biomedicines 2023, 11, 1962. [Google Scholar] [CrossRef]
- Pigliasco, F.; Cafaro, A.; Simeoli, R.; Barco, S.; Magnasco, A.; Faraci, M.; Tripodi, G.; Goffredo, B.M.; Cangemi, G. A Uhplc–Ms/Ms Method for Therapeutic Drug Monitoring of Aciclovir and Ganciclovir in Plasma and Dried Plasma Spots. Biomedicines 2021, 9, 1379. [Google Scholar] [CrossRef]
- Velghe, S.; Deprez, S.; Stove, C.P. Fully Automated Therapeutic Drug Monitoring of Anti-Epileptic Drugs Making Use of Dried Blood Spots. J. Chromatogr. A 2019, 1601, 95–103. [Google Scholar] [CrossRef] [PubMed]
- la Marca, G.; Malvagia, S.; Filippi, L.; Fiorini, P.; Innocenti, M.; Luceri, F.; Pieraccini, G.; Moneti, G.; Francese, S.; Dani, F.R.; et al. Rapid Assay of Topiramate in Dried Blood Spots by a New Liquid Chromatography-Tandem Mass Spectrometric Method. J. Pharm. Biomed. Anal. 2008, 48, 1392–1396. [Google Scholar] [CrossRef] [PubMed]
- Corso, G.; Paglia, G.; Garofalo, D.; D’Apolito, O. Neutral Loss Analysis of Amino Acids by Desorption Electrospray Ionization Using an Unmodified Tandem Quadrupole Mass Spectrometer. Rapid Commun. Mass. Spectrom. 2007, 21, 3777–3784. [Google Scholar] [CrossRef] [PubMed]
- D’Apolito, O.; Garofalo, D.; Paglia, G.; Zuppaldi, A.; Corso, G. Orotic Acid Quantification in Dried Blood Spots and Biological Fluids by Hydrophilic Interaction Liquid Chromatography Tandem Mass Spectrometry. J. Sep. Sci. 2010, 33, 966–973. [Google Scholar] [CrossRef]
- Paglia, G.; D’Apolito, O.; Gelzo, M.; Dello Russo, A.; Corso, G. Direct Analysis of Sterols from Dried Plasma/Blood Spots by an Atmospheric Pressure Thermal Desorption Chemical Ionization Mass Spectrometry (APTDCI-MS) Method for a Rapid Screening of Smith-Lemli-Opitz Syndrome. Analyst 2010, 135, 789–796. [Google Scholar] [CrossRef] [PubMed]
- Corso, G.; D’Apolito, O.; Gelzo, M.; Paglia, G.; Russo, A. Dello A Powerful Couple in the Future of Clinical Biochemistry: In Situ Analysis of Dried Blood Spots by Ambient Mass Spectrometry. Bioanalysis 2010, 2, 1883–1891. [Google Scholar] [CrossRef] [PubMed]
- Sadones, N.; Capiau, S.; De Kesel, P.M.M.; Lambert, W.E.; Stove, C.P. Spot Them in the Spot: Analysis of Abused Substances Using Dried Blood Spots. Bioanalysis 2014, 6, 2211–2227. [Google Scholar] [CrossRef]
- Nix, C.; Hemmati, M.; Cobraiville, G.; Servais, A.C.; Fillet, M. Blood Microsampling to Monitor Metabolic Profiles During Physical Exercise. Front. Mol. Biosci. 2021, 8, 681400. [Google Scholar] [CrossRef]
- Hemmati, M.; Nix, C.; Crommen, J.; Servais, A.C.; Fillet, M. Benefits of Microsampling and Microextraction for Metabolomics Studies. TrAC Trends Anal. Chem. 2020, 127, 115899. [Google Scholar] [CrossRef]
- Nakajima, D.; Ohara, O.; Kawashima, Y. Toward Proteome-Wide Exploration of Proteins in Dried Blood Spots Using Liquid Chromatography-Coupled Mass Spectrometry. Proteomics 2021, 21, e2100019. [Google Scholar] [CrossRef]
- Ferreira, H.B.; Guerra, I.M.S.; Melo, T.; Rocha, H.; Moreira, A.S.P.; Paiva, A.; Domingues, M.R. Dried Blood Spots in Clinical Lipidomics: Optimization and Recent Findings. Anal. Bioanal. Chem. 2022, 414, 7085–7101. [Google Scholar] [CrossRef] [PubMed]
- Guthrie, R.; Susi, A. A Simple Phenylalanine Method for Detecting Phenylketonuria in Large Populations of Newborn Infants. Pediatrics 1963, 32, 338–343. [Google Scholar] [CrossRef] [PubMed]
- Ottosson, F.; Russo, F.; Abrahamsson, A.; MacSween, N.; Courraud, J.; Nielsen, Z.K.; Hougaard, D.M.; Cohen, A.S.; Ernst, M. Effects of Long-Term Storage on the Biobanked Neonatal Dried Blood Spot Metabolome. J. Am. Soc. Mass. Spectrom. 2023, 34, 685–694. [Google Scholar] [CrossRef] [PubMed]
- Moretti, M.; Manfredi, A.; Freni, F.; Previderé, C.; Osculati, A.M.M.; Grignani, P.; Tronconi, L.; Carelli, C.; Vignali, C.; Morini, L. A Comparison between Two Different Dried Blood Substrates in Determination of Psychoactive Substances in Postmortem Samples. Forensic Toxicol. 2021, 39, 385–393. [Google Scholar] [CrossRef] [PubMed]
- Baillargeon, K.R.; Brooks, J.C.; Miljanic, P.R.; Mace, C.R. Patterned Dried Blood Spot Cards for the Improved Sampling of Whole Blood. ACS Meas. Sci. Au 2022, 2, 31–38. [Google Scholar] [CrossRef] [PubMed]
- Shaner, R.L.; Coleman, R.M.; Schulze, N.; Platanitis, K.; Brown, A.A.; Seymour, C.; Kaplan, P.; Perez, J.; Hamelin, E.I.; Johnson, R.C. Investigation of Dried Blood Sampling with Liquid Chromatography Tandem Mass Spectrometry to Confirm Human Exposure to Nerve Agents. Anal. Chim. Acta 2018, 1033, 100–107. [Google Scholar] [CrossRef] [PubMed]
- Hall, E.M.; Flores, S.R.; De Jesús, V.R. Influence of Hematocrit and Total-Spot Volume on Performance Characteristics of Dried Blood Spots for Newborn Screening. Int. J. Neonatal Screen. 2015, 1, 69–78. [Google Scholar] [CrossRef]
- Youhnovski, N.; Bergeron, A.; Furtado, M.; Garofolo, F. Pre-Cut Dried Blood Spot (PCDBS): An Alternative to Dried Blood Spot (DBS) Technique to Overcome Hematocrit Impact. Rapid Commun. Mass Spectrom. 2011, 25, 2951–2958. [Google Scholar] [CrossRef]
- Velghe, S.; Stove, C.P. Evaluation of the Capitainer-B Microfluidic Device as a New Hematocrit-Independent Alternative for Dried Blood Spot Collection. Anal. Chem. 2018, 90, 12893–12899. [Google Scholar] [CrossRef]
- Abu-Rabie, P.; Denniff, P.; Spooner, N.; Chowdhry, B.Z.; Pullen, F.S. Investigation of Different Approaches to Incorporating Internal Standard in DBS Quantitative Bioanalytical Workflows and Their Effect on Nullifying Hematocrit-Based Assay Bias. Anal. Chem. 2015, 87, 4996–5003. [Google Scholar] [CrossRef]
- Deprez, S.; Van Uytfanghe, K.; Stove, C.P. Liquid Chromatography-Tandem Mass Spectrometry for Therapeutic Drug Monitoring of Immunosuppressants and Creatinine from a Single Dried Blood Spot Using the Capitainer® QDBS Device. Anal. Chim. Acta 2023, 1242, 340797. [Google Scholar] [CrossRef] [PubMed]
- Kaduskar, O.; Bhatt, V.; Prosperi, C.; Hayford, K.; Hasan, A.Z.; Deshpande, G.R.; Tilekar, B.; Vivian Thangaraj, J.W.; Kumar, M.S.; Gupta, N.; et al. Optimization and Stability Testing of Four Commercially Available Dried Blood Spot Devices for Estimating Measles and Rubella IgG Antibodies. mSphere 2021, 6, e0049021. [Google Scholar] [CrossRef] [PubMed]
- Delahaye, L.; Veenhof, H.; Koch, B.C.P.; Alffenaar, J.W.C.; Linden, R.; Stove, C. Alternative Sampling Devices to Collect Dried Blood Microsamples: State-of-The-Art. Ther. Drug Monit. 2021, 43, 310–321. [Google Scholar] [CrossRef]
- Baillargeon, K.R.; Morbioli, G.G.; Brooks, J.C.; Miljanic, P.R.; Mace, C.R. Direct Processing and Storage of Cell-Free Plasma Using Dried Plasma Spot Cards. ACS Meas. Sci. Au 2022, 2, 457–465. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.H.; Woenker, T.; Adamec, J.; Regnier, F.E. Simple, Miniaturized Blood Plasma Extraction Method. Anal. Chem. 2013, 85, 11501–11508. [Google Scholar] [CrossRef]
- Schleif, W.S.; Harlan, R.S.; Hamblin, F.; Amankwah, E.K.; Goldenberg, N.A.; Hernandez, R.G.; Johnson, S.B.; Reed, S.; Graham, D.R. Defining the Healthy Infant Metabolome: Liquid Chromatography Tandem-Mass Spectrometry Analysis of Dried Blood Spot Extracts from the Prospective Research on Early Determinants of Illness and Children’s Health Trajectories Birth Cohort Study. J. Pediatr. 2022, 241, 251–256. [Google Scholar] [CrossRef] [PubMed]
- Bishop, L.M.; Fiehn, O. Comprehensive Lipidomic Profiling by Plasma Separation Cards. Anal. Bioanal. Chem. 2023, 415, 193–201. [Google Scholar] [CrossRef] [PubMed]
- Nys, G.; Kok, M.G.M.; Servais, A.C.; Fillet, M. Beyond Dried Blood Spot: Current Microsampling Techniques in the Context of Biomedical Applications. TrAC Trends Anal. Chem. 2017, 97, 326–332. [Google Scholar] [CrossRef]
- Kok, M.G.M.; Nix, C.; Nys, G.; Fillet, M. Targeted Metabolomics of Whole Blood Using Volumetric Absorptive Microsampling. Talanta 2019, 197, 49–58. [Google Scholar] [CrossRef]
- Kovač, J.; Panic, G.; Neodo, A.; Meister, I.; Coulibaly, J.T.; Schulz, J.D.; Keiser, J. Evaluation of a Novel Micro-Sampling Device, MitraTM, in Comparison to Dried Blood Spots, for Analysis of Praziquantel in Schistosoma Haematobium-Infected Children in Rural Côte d’Ivoire. J. Pharm. Biomed. Anal. 2018, 151, 339–346. [Google Scholar] [CrossRef]
- Denniff, P.; Spooner, N. Volumetric Absorptive Microsampling: A Dried Sample Collection Technique for Quantitative Bioanalysis. Anal. Chem. 2014, 86, 8489–8495. [Google Scholar] [CrossRef] [PubMed]
- De Kesel, P.M.M.; Lambert, W.E.; Stove, C.P. Does Volumetric Absorptive Microsampling Eliminate the Hematocrit Bias for Caffeine and Paraxanthine in Dried Blood Samples? A Comparative Study. Anal. Chim. Acta 2015, 881, 65–73. [Google Scholar] [CrossRef]
- Kok, M.G.M.; Fillet, M. Volumetric Absorptive Microsampling: Current Advances and Applications. J. Pharm. Biomed. Anal. 2018, 147, 288–296. [Google Scholar] [CrossRef] [PubMed]
- Blicharz, T.M.; Gong, P.; Bunner, B.M.; Chu, L.L.; Leonard, K.M.; Wakefield, J.A.; Williams, R.E.; Dadgar, M.; Tagliabue, C.A.; El Khaja, R.; et al. Microneedle-Based Device for the One-Step Painless Collection of Capillary Blood Samples. Nat. Biomed. Eng. 2018, 2, 151–157. [Google Scholar] [CrossRef] [PubMed]
- Catala, A.; Culp-Hill, R.; Nemkov, T.; D’Alessandro, A. Quantitative Metabolomics Comparison of Traditional Blood Draws and TAP Capillary Blood Collection. Metabolomics 2018, 14, 100. [Google Scholar] [CrossRef] [PubMed]
- Noble, L.D.; Dixon, C.; Moran, A.; Trottet, C.; Majam, M.; Ismail, S.; Msolomba, V.T.; Mathobela, K.; Queval, A.; George, J.; et al. Painless Capillary Blood Collection: A Rapid Evaluation of the Onflow Device. Diagnostics 2023, 13, 1754. [Google Scholar] [CrossRef] [PubMed]
- Deprez, S.; Paniagua-González, L.; Velghe, S.; Stove, C.P. Evaluation of the Performance and Hematocrit Independence of the HemaPEN as a Volumetric Dried Blood Spot Collection Device. Anal. Chem. 2019, 91, 14467–14475. [Google Scholar] [CrossRef] [PubMed]
- Laurent, A.; Nix, C.; Cobraiville, G.; Crommen, J.; Fillet, M. A Targeted UHPLC-MS/MS Method to Monitor Lipidomic Changes during a Physical Effort: Optimization and Application to Blood Microsamples from Athletes. J. Pharm. Biomed. Anal. 2023, 229, 115373. [Google Scholar] [CrossRef]
- Volani, C.; Malfertheiner, C.; Caprioli, G.; Fjelstrup, S.; Pramstaller, P.P.; Rainer, J.; Paglia, G. VAMS-Based Blood Capillary Sampling for Mass Spectrometry-Based Human Metabolomics Studies. Metabolites 2023, 13, 146. [Google Scholar] [CrossRef]
- Volani, C.; Caprioli, G.; Calderisi, G.; Sigurdsson, B.B.; Rainer, J.; Gentilini, I.; Hicks, A.A.; Pramstaller, P.P.; Weiss, G.; Smarason, S.V.; et al. Pre-Analytic Evaluation of Volumetric Absorptive Microsampling and Integration in a Mass Spectrometry-Based Metabolomics Workflow. Anal. Bioanal. Chem. 2017, 409, 6263–6276. [Google Scholar] [CrossRef]
- Protti, M.; Mandrioli, R.; Mercolini, L. Tutorial: Volumetric Absorptive Microsampling (VAMS). Anal. Chim. Acta 2019, 1046, 32–47. [Google Scholar] [CrossRef] [PubMed]
- Hill, J.; Taylor, R.; Magesh, R. Evaluation of Endogenous Amino Acids as Pre- Analytical Controls for Blood Samples. Available online: https://cdn2.hubspot.net/hubfs/6854050/WEB%20Pages/knowledge%20Library/Small%20Molecule/PDFs/evaluation-endogenous-amino-acids-preanalytical-controls-standards.pdf (accessed on 31 December 2023).
- Marshall, D.J.; Kim, J.J.; Brand, S.; Bryne, C.; Keevil, B.G. Assessment of Tacrolimus and Creatinine Concentration Collected Using Mitra Microsampling Devices. Ann. Clin. Biochem. 2020, 57, 389–396. [Google Scholar] [CrossRef]
- Marasca, C.; Arana, M.E.B.; Protti, M.; Cavalli, A.; Mercolini, L.; Armirotti, A. Volumetric Absorptive Microsampling of Blood for Untargeted Lipidomics. Molecules 2021, 26, 262. [Google Scholar] [CrossRef]
- Johnson, A.; Braga, C.; de Magalhães Padilha, P.; Adamec, J. Collection of Plasma Samples in Areas with Limited Healthcare Access. Methods Mol. Biol. 2023, 2628, 19–32. [Google Scholar] [CrossRef] [PubMed]
- Sakaguchi, C.A.; Nieman, D.C.; Signini, E.F.; Abreu, R.M.; Catai, A.M. Metabolomics-Based Studies Assessing Exercise-Induced Alterations of the Human Metabolome: A Systematic Review. Metabolites 2019, 9, 164. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.; Park, Y.; Jo, J.; In, S.; Park, Y.; Kim, E.; Pyo, J.; Choe, S. Analysis of Benzodiazepines and Their Metabolites Using DBS Cards and LC-MS/MS. Forensic Sci. Int. 2015, 255, 137–145. [Google Scholar] [CrossRef]
- Li, K.; Naviaux, J.C.; Monk, J.M.; Wang, L.; Naviaux, R.K. Improved Dried Blood Spot-Based Metabolomics: A Targeted, Broad-Spectrum, Single-Injection Method. Metabolites 2020, 10, 82. [Google Scholar] [CrossRef]
- Beck, O.; Kenan Modén, N.; Seferaj, S.; Lenk, G.; Helander, A. Study of Measurement of the Alcohol Biomarker Phosphatidylethanol (Peth) in Dried Blood Spot (DBS) Samples and Application of a Volumetric DBS Device. Clin. Chim. Acta 2018, 479, 38–42. [Google Scholar] [CrossRef]
- Koster, R.A.; Niemeijer, P.; Veenhof, H.; Van Hateren, K.; Alffenaar, J.W.C.; Touw, D.J. A Volumetric Absorptive Microsampling LC-MS/MS Method for Five Immunosuppressants and Their Hematocrit Effects. Bioanalysis 2019, 11, 495–508. [Google Scholar] [CrossRef]
- Paniagua-González, L.; Díaz-Louzao, C.; Lendoiro, E.; Otero-Antón, E.; Cadarso-Suárez, C.; López-Rivadulla, M.; Cruz, A.; de-Castro-Ríos, A. Volumetric Absorptive Microsampling (VAMS) for Assaying Immunosuppressants from Venous Whole Blood by LC–MS/MS Using a Novel Atmospheric Pressure Ionization Probe (UniSprayTM). J. Pharm. Biomed. Anal. 2020, 189, 113422. [Google Scholar] [CrossRef]
- Denniff, P.; Parry, S.; Dopson, W.; Spooner, N. Quantitative Bioanalysis of Paracetamol in Rats Using Volumetric Absorptive Microsampling (VAMS)TVolumetric Absorptive Microsampling. J. Pharm. Biomed. Anal. 2015, 108, 61–89. [Google Scholar] [CrossRef]
- Bernardo, M.; Mezquida, G.; Ferré, P.; Cabrera, B.; Torra, M.; Lizana, A.M.; Brunet, M. Dried Blood Spot (DBS) as a Useful Tool to Improve Clozapine, Aripiprazole and Paliperidone Treatment: From Adherence to Efficiency. Rev. De Psiquiatr. Y Salud Ment. 2022, 15, 230–237. [Google Scholar] [CrossRef]
- Gao, F.; McDaniel, J.; Chen, E.Y.; Rockwell, H.E.; Drolet, J.; Vishnudas, V.K.; Tolstikov, V.; Sarangarajan, R.; Narain, N.R.; Kiebish, M.A. Dynamic and Temporal Assessment of Human Dried Blood Spot MS/MSALL Shotgun Lipidomics Analysis. Nutr. Metab. 2017, 14, 28. [Google Scholar] [CrossRef] [PubMed]
- Koehler, K.; Marks-Nelson, E.; Braga, C.P.; Beckford, S.; Adamec, J. Validity of Plasma Collection Cards for Ferritin Assessment—A Proof-of-Concept Study. Eur. J. Haematol. 2020, 104, 554–561. [Google Scholar] [CrossRef] [PubMed]
- Hong, X.; Sadilek, M.; Gelb, M.H. A Highly Multiplexed Biochemical Assay for Analytes in Dried Blood Spots: Application to Newborn Screening and Diagnosis of Lysosomal Storage Disorders and Other Inborn Errors of Metabolism. Genet. Med. 2020, 22, 1262–1268. [Google Scholar] [CrossRef]
- Deprez, S.; Stove, C. Application of a Fully Automated Dried Blood Spot Method for Therapeutic Drug Monitoring of Immunosuppressants: Another Step Toward Implementation of Dried Blood Spot Analysis. Arch. Pathol. Lab. Med. 2023, 147, 786–796. [Google Scholar] [CrossRef] [PubMed]
- Londhe, V.; Rajadhyaksha, M. Opportunities and Obstacles for Microsampling Techniques in Bioanalysis: Special Focus on DBS and VAMS. J. Pharm. Biomed. Anal. 2020, 182, 113102. [Google Scholar] [CrossRef]
- Roberts, J.L.; Whiley, L.; Gray, N.; Gay, M.; Lawler, N.G. Advanced Microsamples: Current Applications and Considerations for Mass Spectrometry-Based Metabolic Phenotyping Pipelines. Separations 2022, 9, 175. [Google Scholar] [CrossRef]
- Malsagova, K.; Kopylov, A.; Stepanov, A.; Butkova, T.; Izotov, A.; Kaysheva, A. Dried Blood Spot in Laboratory: Directions and Prospects. Diagnostics 2020, 10, 248. [Google Scholar] [CrossRef]
- Bodamer, O.A. Screening for Phenylketonuria. Ann. Nestle Eng. 2010, 68, 53–57. [Google Scholar] [CrossRef]
- Gavrilov, D.K.; Piazza, A.L.; Pino, G.; Turgeon, C.; Matern, D.; Oglesbee, D.; Raymond, K.; Tortorelli, S.; Rinaldo, P. The Combined Impact of CLIR Post-Analytical Tools and Second Tier Testing on the Performance of Newborn Screening for Disorders of Propionate, Methionine, and Cobalamin Metabolism. Int. J. Neonatal Screen. 2020, 6, 33. [Google Scholar] [CrossRef] [PubMed]
- Schulze, A.; Lindner, M.; Kohlmüller, D.; Olgemöller, K.; Mayatepek, E.; Hoffmann, G.F. Expanded Newborn Screening for Inborn Errors of Metabolism by Electrospray Ionization-Tandem Mass Spectrometry: Results, Outcome, and Implications. Pediatrics 2003, 111, 1399–1406. [Google Scholar] [CrossRef] [PubMed]
- Taruscio, D.; Piccioli, A. Newborn Screening in Italy: A Unique Program of Public Health in Europe. Editorial. Ann. Ist. Super. Sanita 2023, 59, 1–3. [Google Scholar] [CrossRef] [PubMed]
- Ismail, I.T.; Showalter, M.R.; Fiehn, O. Inborn Errors of Metabolism in the Era of Untargeted Metabolomics and Lipidomics. Metabolites 2019, 9, 242. [Google Scholar] [CrossRef]
- Mak, J.; Peng, G.; Le, A.; Gandotra, N.; Enns, G.M.; Scharfe, C.; Cowan, T.M. Validation of a Targeted Metabolomics Panel for Improved Second-tier Newborn Screening. J. Inherit. Metab. Dis. 2023, 46, 194–205. [Google Scholar] [CrossRef]
- Brown, M.; Turgeon, C.; Rinaldo, P.; Pop, A.; Salomons, G.S.; Roullet, J.; Gibson, K.M. Longitudinal Metabolomics in Dried Bloodspots Yields Profiles Informing Newborn Screening for Succinic Semialdehyde Dehydrogenase Deficiency. JIMD Rep. 2020, 53, 29–38. [Google Scholar] [CrossRef]
- Lapalme-Remis, S.; Lewis, E.C.; De Meulemeester, C.; Chakraborty, P.; Gibson, K.M.; Torres, C.; Guberman, A.; Salomons, G.S.; Jakobs, C.; Ali-Ridha, A.; et al. Natural History of Succinic Semialdehyde Dehydrogenase Deficiency through Adulthood. Neurology 2015, 85, 861–865. [Google Scholar] [CrossRef]
- Taibl, K.R.; Dunlop, A.L.; Barr, D.B.; Li, Y.-Y.; Eick, S.M.; Kannan, K.; Ryan, P.B.; Schroder, M.; Rushing, B.; Fennell, T.; et al. Newborn Metabolomic Signatures of Maternal Per- and Polyfluoroalkyl Substance Exposure and Reduced Length of Gestation. Nat. Commun. 2023, 14, 3120. [Google Scholar] [CrossRef]
- Templer, S.P.; Seiverth, B.; Baum, P.; Stevens, W.; Seguin-Devaux, C.; Carmona, S. Improved Sensitivity of a Dual-Target HIV-1 Qualitative Test for Plasma and Dried Blood Spots. J. Clin. Microbiol. 2016, 54, 1877–1882. [Google Scholar] [CrossRef]
- Cvetko, A.; Tijardović, M.; Bilandžija-Kuš, I.; Gornik, O. Comparison of Self-Sampling Blood Collection for N-Glycosylation Analysis. BMC Res. Notes 2022, 15, 61. [Google Scholar] [CrossRef]
- Petrick, L.M.; Schiffman, C.; Edmands, W.M.B.; Yano, Y.; Perttula, K.; Whitehead, T.; Metayer, C.; Wheelock, C.E.; Arora, M.; Grigoryan, H.; et al. Metabolomics of Neonatal Blood Spots Reveal Distinct Phenotypes of Pediatric Acute Lymphoblastic Leukemia and Potential Effects of Early-Life Nutrition. Cancer Lett. 2019, 452, 71–78. [Google Scholar] [CrossRef] [PubMed]
- Pfluger, B.A.; Smith, H.V.; Weber, A.M.; Ibrahim, H.; Doumbia, L.; Bore, A.; Cissoko, A.; Douyon, S.; Kone, K.; Sangare, L.; et al. Non-Targeted Dried Blood Spot-Based Metabolomics Analysis Showed Rice Bran Supplementation Effects Multiple Metabolic Pathways during Infant Weaning and Growth in Mali. Nutrients 2022, 14, 609. [Google Scholar] [CrossRef] [PubMed]
- McNairn, M.; Brito, A.; Dillard, K.; Heath, H.; Pantaleon, M.; Fanter, R.; Pilolla, K.; Amin, S.; Frano, M.R. La Postprandial Dried Blood Spot–Based Nutritional Metabolomic Analysis Discriminates a High-Fat, High-Protein Meat-Based Diet from a High Carbohydrate Vegan Diet: A Randomized Controlled Crossover Trial. J. Acad. Nutr. Diet. 2021, 121, 931–941.e2. [Google Scholar] [CrossRef] [PubMed]
- Patel, S.R.; Bryan, P.; Spooner, N.; Timmerman, P.; Wickremsinhe, E. Microsampling for Quantitative Bioanalysis, an Industry Update: Output from an AAPS/EBF Survey. Bioanalysis 2019, 11, 619–628. [Google Scholar] [CrossRef] [PubMed]
- Ritz, N.; Bielicki, J.; Pfister, M.; van den Anker, J. Therapeutic Drug Monitoring for Anti-Infective Agents in Pediatrics. Pediatr. Infect. Dis. J. 2016, 35, 570–572. [Google Scholar] [CrossRef] [PubMed]
- Brüggemann, R.J.M.; Aarnoutse, R.E. Fundament and Prerequisites for the Application of an Antifungal TDM Service. Curr. Fungal Infect. Rep. 2015, 9, 122–129. [Google Scholar] [CrossRef] [PubMed]
- Tang, J.; de Winter, B.C.; Hesselink, D.A.; Sombogaard, F.; Wang, L.; van Gelder, T. The Pharmacokinetics and Pharmacodynamics of Mycophenolate Mofetil in Younger and Elderly Renal Transplant Recipients. Br. J. Clin. Pharmacol. 2017, 83, 812–822. [Google Scholar] [CrossRef]
- Linder, C.; Hansson, A.; Sadek, S.; Gustafsson, L.L.; Pohanka, A. Carbamazepine, Lamotrigine, Levetiracetam and Valproic Acid in Dried Blood Spots with Liquid Chromatography Tandem Mass Spectrometry; Method Development and Validation. J. Chromatogr. B Anal. Technol. Biomed. Life Sci. 2018, 1072, 116–122. [Google Scholar] [CrossRef]
- Mukai, Y.; Yoshida, T.; Kondo, T.; Miura, J.; Inotsume, N.; Toda, T. Development and Validation of a Simple Method for Simultaneously Measuring the Concentrations of BCR-ABL and Bruton Tyrosine Kinase Inhibitors in Dried Blood Spot (DBS): A Pilot Study to Obtain Candidate Conversion Equations for Predicting Plasma Concentration Based on DBS Concentration. Ther. Drug Monit. 2022, 44, 762–770. [Google Scholar] [CrossRef]
- Zimmermann, S.; Aghai, F.; Schilling, B.; Kraus, S.; Grigoleit, G.U.; Kalogirou, C.; Goebeler, M.E.; Jung, P.; Pelzer, T.; Klinker, H.; et al. Volumetric Absorptive Microsampling (VAMS) for the Quantification of Ten Kinase Inhibitors and Determination of Their in Vitro VAMS-to-Plasma Ratio. J. Pharm. Biomed. Anal. 2022, 211, 114623. [Google Scholar] [CrossRef]
- Carniel, E.; dos Santos, K.A.; de Andrade de Lima, L.; Kohlrausch, R.; Linden, R.; Antunes, M.V. Determination of Clozapine and Norclozapine in Dried Plasma Spot and Dried Blood Spot by Liquid Chromatography-Tandem Mass Spectrometry. J. Pharm. Biomed. Anal. 2022, 210, 114591. [Google Scholar] [CrossRef]
- Gianazza, E.; Brioschi, M.; Iezzi, A.; Paglia, G.; Banfi, C. Pharmacometabolomics for the Study of Lipid-Lowering Therapies: Opportunities and Challenges. Int. J. Mol. Sci. 2023, 24, 3291. [Google Scholar] [CrossRef] [PubMed]
- Amaro, F.; Carvalho, M.; de Lourdes Bastos, M.; de Pinho, P.G.; Pinto, J. Pharmacometabolomics Applied to Personalized Medicine in Urological Cancers. Pharmaceuticals 2022, 15, 295. [Google Scholar] [CrossRef] [PubMed]
- Volani, C.; Paglia, G.; Smarason, S.; Pramstaller, P.; Demetz, E.; Pfeifhofer-Obermair, C.; Weiss, G. Metabolic Signature of Dietary Iron Overload in a Mouse Model. Cells 2018, 7, 264. [Google Scholar] [CrossRef] [PubMed]
- Rago, B.; Liu, J.; Tan, B.; Holliman, C. Application of the Dried Spot Sampling Technique for Rat Cerebrospinal Fluid Sample Collection and Analysis. J. Pharm. Biomed. Anal. 2011, 55, 1201–1207. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Rodríguez, A.E.; Luis-Lima, S.; Donate-Correa, J.; Diaz-Martín, L.; Arnau, M.R.; Jiménez-Sosa, A.; Gaspari, F.; Ortiz, A.; Porrini, E. Iohexol Plasma Clearance Simplified by Dried Blood Spot (DBS) Sampling to Measure Renal Function in Conscious Mice. Sci. Rep. 2021, 11, 4591. [Google Scholar] [CrossRef] [PubMed]
- Puigarnau, S.; Fernàndez, A.; Obis, E.; Jové, M.; Castañer, M.; Pamplona, R.; Portero-Otin, M.; Camerino, O. Metabolomics Reveals That Fittest Trail Runners Show a Better Adaptation of Bioenergetic Pathways. J. Sci. Med. Sport. 2022, 25, 425–431. [Google Scholar] [CrossRef]
- Cendali, F.; D’Alessandro, A.; Nemkov, T. Dried Blood Spot Characterization of Sex-based Metabolic Responses to Acute Running Exercise. Anal. Sci. Adv. 2023, 4, 37–48. [Google Scholar] [CrossRef]
- Nemkov, T.; Cendali, F.; Stefanoni, D.; Martinez, J.L.; Hansen, K.C.; San-Millán, I.; D’Alessandro, A. Metabolic Signatures of Performance in Elite World Tour Professional Male Cyclists. Sports Med. 2023, 53, 1651–1665. [Google Scholar] [CrossRef]
- Bassini, A.; Sartoretto, S.; Jurisica, L.; Magno-França, A.; Anderson, L.; Pearson, T.; Razavi, M.; Chandran, V.; Martin, L.; Jurisica, I.; et al. Sportomics Method to Assess Acute Phase Proteins in Olympic Level Athletes Using Dried Blood Spots and Multiplex Assay. Sci. Rep. 2022, 12, 19824. [Google Scholar] [CrossRef]
- Olivier, M.; Asmis, R.; Hawkins, G.A.; Howard, T.D.; Cox, L.A. The Need for Multi-Omics Biomarker Signatures in Precision Medicine. Int. J. Mol. Sci. 2019, 20, 4781. [Google Scholar] [CrossRef] [PubMed]
- Byeon, S.K.; Madugundu, A.K.; Garapati, K.; Ramarajan, M.G.; Saraswat, M.; Kumar-M, P.; Hughes, T.; Shah, R.; Patnaik, M.M.; Chia, N.; et al. Development of a Multiomics Model for Identification of Predictive Biomarkers for COVID-19 Severity: A Retrospective Cohort Study. Lancet Digit. Health 2022, 4, e632–e645. [Google Scholar] [CrossRef]
- Kovarik, J.J.; Bileck, A.; Hagn, G.; Meier-Menches, S.M.; Frey, T.; Kaempf, A.; Hollenstein, M.; Shoumariyeh, T.; Skos, L.; Reiter, B.; et al. A Multi-Omics Based Anti-Inflammatory Immune Signature Characterizes Long COVID-19 Syndrome. iScience 2023, 26. [Google Scholar] [CrossRef] [PubMed]
- Mendiola, A.S.; Yan, Z.; Dixit, K.; Johnson, J.R.; Bouhaddou, M.; Meyer-Franke, A.; Shin, M.G.; Yong, Y.; Agrawal, A.; MacDonald, E.; et al. Defining Blood-Induced Microglia Functions in Neurodegeneration through Multiomic Profiling. Nat. Immunol. 2023, 24, 1173–1187. [Google Scholar] [CrossRef]
- Shi, L.; Xu, J.; Green, R.; Wretlind, A.; Homann, J.; Buckley, N.J.; Tijms, B.M.; Vos, S.J.B.; Lill, C.M.; ten Kate, M.; et al. Multiomics Profiling of Human Plasma and Cerebrospinal Fluid Reveals ATN-Derived Networks and Highlights Causal Links in Alzheimer’s Disease. Alzheimer’s Dement. 2023, 19, 3350–3364. [Google Scholar] [CrossRef] [PubMed]
- Campeau, A.; Mills, R.H.; Stevens, T.; Rossitto, L.A.; Meehan, M.; Dorrestein, P.; Daly, R.; Nguyen, T.T.; Gonzalez, D.J.; Jeste, D.V.; et al. Multi-Omics of Human Plasma Reveals Molecular Features of Dysregulated Inflammation and Accelerated Aging in Schizophrenia. Mol. Psychiatry 2022, 27, 1217–1225. [Google Scholar] [CrossRef] [PubMed]
- Sveinbjornsson, G.; Ulfarsson, M.O.; Thorolfsdottir, R.B.; Jonsson, B.A.; Einarsson, E.; Gunnlaugsson, G.; Rognvaldsson, S.; Arnar, D.O.; Baldvinsson, M.; Bjarnason, R.G.; et al. Multiomics Study of Nonalcoholic Fatty Liver Disease. Nat. Genet. 2022, 54, 1652–1663. [Google Scholar] [CrossRef]
- Song, X.; Zhu, Z.; Qian, X.; Liu, X.; Chen, S.; Tang, H. Multi-Omics Characterization of Type 2 Diabetes Mellitus-Induced Cognitive Impairment in the Db/Db Mouse Model. Molecules 2022, 27, 1904. [Google Scholar] [CrossRef]
- Fang, X.; Miao, R.; Wei, J.; Wu, H.; Tian, J. Advances in Multi-Omics Study of Biomarkers of Glycolipid Metabolism Disorder. Comput. Struct. Biotechnol. J. 2022, 20, 5935–5951. [Google Scholar] [CrossRef]
- Shen, X.; Kellogg, R.; Panyard, D.J.; Bararpour, N.; Castillo, K.E.; Lee-McMullen, B.; Delfarah, A.; Ubellacker, J.; Ahadi, S.; Rosenberg-Hasson, Y.; et al. Multi-Omics Microsampling for the Profiling of Lifestyle-Associated Changes in Health. Nat. Biomed. Eng. 2023. [Google Scholar] [CrossRef]
- Chen, R.; Mias, G.I.; Li-Pook-Than, J.; Jiang, L.; Lam, H.Y.K.; Chen, R.; Miriami, E.; Karczewski, K.J.; Hariharan, M.; Dewey, F.E.; et al. Personal Omics Profiling Reveals Dynamic Molecular and Medical Phenotypes. Cell 2012, 148, 1293–1307. [Google Scholar] [CrossRef] [PubMed]
- Zhuang, Y.-J.; Mangwiro, Y.; Wake, M.; Saffery, R.; Greaves, R.F. Multi-Omics Analysis from Archival Neonatal Dried Blood Spots: Limitations and Opportunities. Clin. Chem. Lab. Med. 2022, 60, 1318–1341. [Google Scholar] [CrossRef] [PubMed]


| Device | Company | Sample Type | Collection | Volume | Volumetric | Potential HCT Bias |
|---|---|---|---|---|---|---|
| Whatman® 903 | Cytiva, Global | Dry whole blood | Capillary blood after finger-prick | 20–80 µL | ✘ | ✔ |
| Capitainer® B | Capitainer AB | Dry whole blood | Capillary blood after finger-prick | 10 µL | ✔ | ✘ |
| HemaSpotTMHF | Spot On Sciences | Dry whole blood | Capillary blood after finger-prick | ~18.7 µL/blade ~150 µL/device | ✔ | ✘ |
| HemaSpotTM SE | Spot On Sciences | Dry serum | Capillary blood after finger-prick | ~150 µL/device | ✔ | ✔ |
| Telimmune UNO/DUO | Telimmune | Dry plasma | Capillary blood after finger-prick | 3.2 µL | ✔ | ✘ |
| Mitra® | Trajan Scientific | Dry whole blood | Capillary blood after finger-prick | 10, 20, 30 µL | ✔ | ✘ |
| TASSO M-20 | Tasso INC. | Dry whole blood | Capillary blood from the upper arm. Push-button device | 17.5 µL | ✔ | ✘ |
| TAP II TAP Micro | YourBio Health | Liquid whole blood | Capillary blood from the upper arm. Push-button device | up to 350 µL up to 600 µL | ✔ | ✘ |
| hemaPEN® | Trajan Scientific | Dry whole blood | Capillary blood after finger-prick | 2.74 µL 10.96 µL/device | ✔ | ✘ |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bossi, E.; Limo, E.; Pagani, L.; Monza, N.; Serrao, S.; Denti, V.; Astarita, G.; Paglia, G. Revolutionizing Blood Collection: Innovations, Applications, and the Potential of Microsampling Technologies for Monitoring Metabolites and Lipids. Metabolites 2024, 14, 46. https://doi.org/10.3390/metabo14010046
Bossi E, Limo E, Pagani L, Monza N, Serrao S, Denti V, Astarita G, Paglia G. Revolutionizing Blood Collection: Innovations, Applications, and the Potential of Microsampling Technologies for Monitoring Metabolites and Lipids. Metabolites. 2024; 14(1):46. https://doi.org/10.3390/metabo14010046
Chicago/Turabian StyleBossi, Eleonora, Elena Limo, Lisa Pagani, Nicole Monza, Simone Serrao, Vanna Denti, Giuseppe Astarita, and Giuseppe Paglia. 2024. "Revolutionizing Blood Collection: Innovations, Applications, and the Potential of Microsampling Technologies for Monitoring Metabolites and Lipids" Metabolites 14, no. 1: 46. https://doi.org/10.3390/metabo14010046
APA StyleBossi, E., Limo, E., Pagani, L., Monza, N., Serrao, S., Denti, V., Astarita, G., & Paglia, G. (2024). Revolutionizing Blood Collection: Innovations, Applications, and the Potential of Microsampling Technologies for Monitoring Metabolites and Lipids. Metabolites, 14(1), 46. https://doi.org/10.3390/metabo14010046