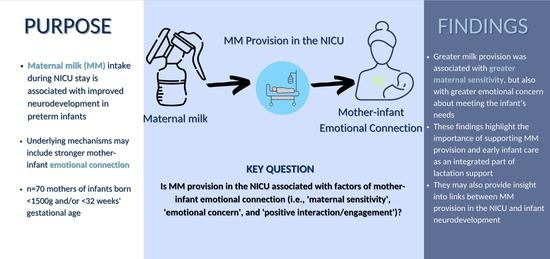
Maternal Milk Provision in the Neonatal Intensive Care Unit and Mother–Infant Emotional Connection for Preterm Infants
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Sample
2.2. Measures
2.2.1. Maternal Milk Intake
2.2.2. Mother–Infant Connection
2.2.3. Psychometrics of Mother–Infant Connection Scales
2.2.4. Covariates
2.3. Statistical Analysis
3. Results
3.1. Study Sample
3.2. Descriptive Statistics of Exposure and Outcome
3.3. Social and Background Characteristics Related to Maternal Milk Provision
3.4. Relationship between Mother–Infant Connection and Potential Covariates
3.5. Associations of Maternal Milk Provision with Mother–Infant Connection
4. Discussion
4.1. Main Associations between Maternal Milk Provision Level and Mother–Infant Connection
4.2. Constructs of Mother–Infant Connection in a Preterm Sample
4.3. Maternal Milk, Mother–Infant Connection, and Demographic Factors
4.4. Study Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bar, S.; Milanaik, R.; Adesman, A. Long-term neurodevelopmental benefits of breastfeeding. Curr. Opin. Pediatr. 2016, 28, 559–566. [Google Scholar] [CrossRef] [PubMed]
- Jarjour, I.T. Neurodevelopmental Outcome After Extreme Prematurity: A Review of the Literature. Pediatr. Neurol. 2015, 52, 143–152. [Google Scholar] [CrossRef]
- Bozzette, M. A Review of Research on Premature Infant-Mother Interaction. Newborn Infant Nurs. Rev. 2007, 7, 49–55. [Google Scholar] [CrossRef]
- Lechner, B.E.; Vohr, B.R. Neurodevelopmental outcomes of preterm infants fed human milk: A systematic review. Clin. Perinatol. 2017, 44, 69–83. [Google Scholar] [CrossRef] [PubMed]
- Belfort, M.B.; Anderson, P.J.; Nowak, V.A.; Lee, K.J.; Molesworth, C.; Thompson, D.K.; Doyle, L.W.; Inder, T.E. Breast Milk Feeding, Brain Development, and Neurocognitive Outcomes: A 7-Year Longitudinal Study in Infants Born at Less Than 30 Weeks’ Gestation. J. Pediatr. 2016, 177, 133–139.e1. [Google Scholar] [CrossRef] [Green Version]
- Schneider, N.; Garcia-Rodenas, C.L. Early nutritional interventions for brain and cognitive development in preterm infants: A review of the literature. Nutrients 2017, 9, 187. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Belfort, M.B. The Science of Breastfeeding and Brain Development. Breastfeed. Med. 2017, 12, 459–461. [Google Scholar] [CrossRef] [PubMed]
- Bowlby, J. The Bowlby-Ainsworth attachment theory. Behav. Brain Sci. 1979, 2, 637–638. [Google Scholar] [CrossRef]
- Bergman, N.J.; Ludwig, R.J.; Westrup, B.; Welch, M.G. Nurturescience versus neuroscience: A case for rethinking perinatal mother–infant behaviors and relationship. Birth Defects Res. 2019, 111, 1110–1127. [Google Scholar] [CrossRef] [PubMed]
- Tharner, A.; Luijk, M.P.; Raat, H.; Ijzendoorn, M.H.; Bakermans-Kranenburg, M.J.; Moll, H.A.; Jaddoe, V.W.; Hofman, A.; Verhulst, F.C.; Tiemeier, H. Breastfeeding and Its Relation to Maternal Sensitivity and Infant Attachment. J. Dev. Behav. Pediatr. 2012, 33, 396–404. [Google Scholar] [CrossRef]
- Lavelli, M.; Poli, M. Early mother-infant interaction during breast- and bottle-feeding. Infant Behav. Dev. 1998, 21, 667–683. [Google Scholar] [CrossRef]
- Swain, J.E.; Kim, P.; Ho, S.S. Neuroendocrinology of Parental Response to Baby-Cry. J. Neuroendocrinol. 2011, 23, 1036–1041. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, P.; Feldman, R.; Mayes, L.C.; Eicher, V.; Thompson, N.; Leckman, J.F.; Swain, J.E. Breastfeeding, brain activation to own infant cry, and maternal sensitivity. J. Child Psychol. Psychiatry 2011, 52, 907–915. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Parker, M.G.; Burnham, L.A.; Melvin, P.; Singh, R.; Lopera, A.M.; Belfort, M.B.; Moses, J.M.; Gupta, M. Addressing Disparities in Mother’s Milk for VLBW Infants Through Statewide Quality Improvement. Pediatrics 2019, 144, e20183809. [Google Scholar] [CrossRef]
- Soldateli, B.; Parker, M.; Melvin, P.; Gupta, M.; Belfort, M. Human milk feeding and physical growth in very low-birth-weight infants: A multicenter study. J. Perinatol. 2020, 40, 1246–1252. [Google Scholar] [CrossRef]
- Nagata, M.; Nagai, S.; Sobajima, H.; Ando, T.; Nishide, Y.; Honjo, S. Maternity blues and attachment to children in mothers of full-term normal infants. Acta Psychiatr. Scand. 2000, 101, 209–217. [Google Scholar] [CrossRef]
- Melnyk, B.M.; Oswalt, K.L.; Sidora-Arcoleo, K. Validation and Psychometric Properties of the Neonatal Intensive Care Unit Parental Beliefs Scale. Nurs. Res. 2014, 63, 105–115. [Google Scholar] [CrossRef] [Green Version]
- Nagata, M.; Nagai, Y.; Sobajima, H.; Ando, T.; Honjo, S. Depression in the early postpartum period and attachment to children—In mothers of NICU infants. Infant Child Dev. Int. J. Res. Pract. 2004, 13, 93–110. [Google Scholar] [CrossRef]
- Hollingshead, A.B.; Yale University, New Haven, CT, USA. Four Factor Index of Social Status. 1975; Unpublished work. [Google Scholar]
- Fenton, T.R.; Kim, J.H. A systematic review and meta-analysis to revise the Fenton growth chart for preterm infants. BMC Pediatr. 2013, 13, 59. [Google Scholar] [CrossRef] [Green Version]
- Herich, L.C.; Cuttini, M.; Croci, I.; Franco, F.; Di Lallo, D.; Baronciani, D.; Fares, K.; Gargano, G.; Raponi, M.; Zeitlin, J. Maternal education is associated with disparities in breastfeeding at time of discharge but not at initiation of enteral feeding in the neonatal intensive care unit. J. Pediatr. 2017, 182, 59–65. [Google Scholar] [CrossRef]
- Abuhammad, S.; Johnson, T. Potential impact of breastfeeding and maternal sensitivity during the first year of life: An integrative review of the literature. Int. J. Pediatr. 2018, 6, 8655–8667. [Google Scholar]
- Weaver, J.M.; Schofield, T.J.; Papp, L.M. Breastfeeding duration predicts greater maternal sensitivity over the next decade. Dev. Psychol. 2018, 54, 220–227. [Google Scholar] [CrossRef] [PubMed]
- Jonas, W.; Atkinson, L.; Steiner, M.; Meaney, M.J.; Wazana, A.; Fleming, A.S. The MAVAN Research Team Breastfeeding and maternal sensitivity predict early infant temperament. Acta Paediatr. 2015, 104, 678–686. [Google Scholar] [CrossRef] [PubMed]
- Mӧrelius, E.; Kling, K.; Haraldsson, E.; Alehagen, S. You can’t flight, you need to fight—A qualitative study of mothers’ expe-riences of feeding extremely preterm infants. J. Clin. Nurs. 2020, 29, 2420–2428. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Swanson, V.; Nicol, H.; McInnes, R.; Cheyne, H.; Mactier, H.; Callander, E. Developing Maternal Self-Efficacy for Feeding Preterm Babies in the Neonatal Unit. Qual. Health Res. 2012, 22, 1369–1382. [Google Scholar] [CrossRef]
- Underwood, M.A. Human Milk for the Premature Infant. Pediatr. Clin. N. Am. 2013, 60, 189–207. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lucas, R.; Paquette, R.; Briere, C.E.; McGrath, J.G. Furthering our understanding of the needs of mothers who are pumping breast milk for infants in the NICU: An integrative review. Adv. Neonatal Care 2014, 14, 241–252. [Google Scholar] [CrossRef] [PubMed]
- Surmeli Onay, O.; Sarilar, T.D.; Taskiran Tepe, H.; Ozen, H.; Tekin, N. The Relationship of Breastfeeding Patterns in the Neonatal Intensive Care Unit to Maternal Symptoms of Anxiety and Depression. Breastfeed. Med. 2021, 16, 251–257. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.H.; Hyun, S.; Mittal, L.; Erdei, C. Psychological risks to mother–infant bonding during the COVID-19 pandemic. Pediatr. Res. 2021, 14, 1–9. [Google Scholar] [CrossRef]
- Beauregard, J.L.; Hamner, H.C.; Chen, J.; Avila-Rodriguez, W.; Elam-Evans, L.D.; Perrine, C.G. Racial disparities in breastfeeding initiation and duration among US infants born in 2015. Morb. Mortal. Wkly. Rep. 2019, 68, 745–748. [Google Scholar] [CrossRef] [PubMed]
- Moran-Lev, H.; Farhi, A.; Bauer, S.; Nehama, H.; Yerushalmy-Feler, A.; Mandel, D.; Lubetzky, R. Association of Socioeconomic Factors and Infant Nutrition Decisions: Breastfeeding and Type of Formula. Breastfeed. Med. 2021, 16, 553–557. [Google Scholar] [CrossRef] [PubMed]
- Whitehill, L.; Smith, J.; Colditz, G.; Le, T.; Kellner, P.R. Socio-demographic factors related to parent engagement in the NICU and the impact of the SENSE program. Early Hum. Dev. 2021, 163, 105486. [Google Scholar] [CrossRef] [PubMed]
- Cox, E.D.; Nackers, K.A.; Young, H.N.; Moreno, M.A.; Levy, J.; Mangione-Smith, R.M. Influence of race and socioeconomic status on engagement in pediatric primary care. Patient Educ. Couns. 2012, 87, 319–326. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Patel, A.L.; Johnson, T.J.; Meier, P.P. Racial and socioeconomic disparities in breast milk feedings in US neonatal intensive care units. Pediatr. Res. 2021, 89, 344–352. [Google Scholar] [CrossRef] [PubMed]
- Korja, R.; Latva, R.; Lehtonen, L. The effects of preterm birth on mother–infant interaction and attachment during the infant’s first two years. Acta Obstet. Et Gynecol. Scand. 2012, 91, 164–173. [Google Scholar] [CrossRef]
- Callen, J.; Pinelli, J. A review of the literature examining the benefits and challenges, incidence and duration, and barriers to breastfeeding in preterm infants. Adv. Neonatal Care 2005, 5, 72–88. [Google Scholar] [CrossRef] [PubMed]
- Floyd, F.J.; Widaman, K.F. Factor analysis in the development and refinement of clinical assessment instruments. Psychol. Assess. 1995, 7, 286–299. [Google Scholar]


| Variables | Total (n = 70) | Exclusive Maternal Milk (n = 23) | Predominant Maternal Milk (n = 9) | Mixed Maternal Milk (n = 38) | p Value |
|---|---|---|---|---|---|
| Maternal Characteristics | |||||
| Hospital NICU | 0.0293 * | ||||
| BIDMC | 30 (42.9) | 5 (21.7) | 6 (66.7) | 19 (50.0) | |
| BWH | 40 (57.1) | 18 (78.3) | 3 (33.3) | 19 (50.0) | |
| Maternal age | 0.0255 * | ||||
| Nmiss (%) | 7 (10.0) | 3 (13.0) | 4 (10.5) | ||
| Mean ± SD | 32.5 ± 6.0 | 35.0 ± 3.7 | 34.3 ± 5.3 | 30.5 ± 6.7 | |
| Min–Max | 20.0–46.0 | 30.0–42.0 | 25.0–40.0 | 20.0–46.0 | |
| Median (IQR) | 33.0 (30.0–36.0) | 33.5 (32.0–37.0) | 34.0 (30.0–39.0) | 31.0 (26.0–35.0) | |
| Maternal race/ethnicity | 0.1432 | ||||
| Missing | 6 (8.6) | 3 (13.0) | 3 (7.9) | ||
| American Indian/Native American | 2 (3.1) | 1 (5.0) | 1 (2.9) | ||
| Asian | 2 (3.1) | 1 (11.1) | 1 (2.9) | ||
| Black/African American | 18 (28.1) | 4 (20.0) | 3 (33.3) | 11 (31.4) | |
| Hispanic/Latina | 11 (17.2) | 2 (22.2) | 9 (25.7) | ||
| White/Caucasian | 28 (43.8) | 14 (70.0) | 3 (33.3) | 11 (31.4) | |
| Other | 3 (4.7) | 1 (5.0) | 2 (5.7) | ||
| Maternal education level | 0.0006 * | ||||
| High school or GED | 11 (15.7) | 1 (11.1) | 10 (26.3) | ||
| Some college | 17 (24.3) | 1 (4.3) | 2 (22.2) | 14 (36.8) | |
| College graduate | 20 (28.6) | 8 (34.8) | 3 (33.3) | 9 (23.7) | |
| Advanced degree | 22 (31.4) | 14 (60.9) | 3 (33.3) | 5 (13.2) | |
| Medical insurance | |||||
| Yes | 70 (100) | 23 (100) | 9 (100) | 38 (100) | |
| Socioeconomic status (Hollingshead) | <0.0001 * | ||||
| Nmiss (%) | 2 (2.9) | 1 (4.3) | 1 (2.6) | ||
| Mean ± SD | 43.8 ± 13.9 | 55.3 ± 9.6 | 41.8 ± 10.7 | 37.4 ± 12.4 | |
| Min–Max | 17.0–66.0 | 24.0–66.0 | 23.5–58.5 | 17.0–66.0 | |
| Median (IQR) | 43.0 (33.5–57.0) | 57.8 (54.5–61.0) | 40.0 (37.5–43.0) | 38.5 (26.0–44.0) | |
| Maternal leave | 0.7531 | ||||
| <3 months | 4 (6.1) | 2 (8.7) | 2 (5.7) | ||
| 3 months | 14 (21.2) | 4 (17.4) | 3 (37.5) | 7 (20.0) | |
| >3 months | 26 (39.4) | 13 (56.5) | 2 (25.0) | 11 (31.4) | |
| Not returning to work | 6 (9.1) | 1 (4.3) | 1 (12.5) | 4 (11.4) | |
| Not working prior to baby | 14 (21.2) | 3 (13.0) | 2 (25.0) | 9 (25.7) | |
| Primiparous | 0.2695 | ||||
| No | 22 (31.4) | 10 (43.5) | 3 (33.3) | 9 (23.7) | |
| Yes | 48 (68.6) | 13 (56.5) | 6 (66.7) | 29 (76.3) | |
| Infant Characteristics | |||||
| Infant sex | 0.9035 | ||||
| Boy | 36 (51.4) | 11 (47.8) | 5 (55.6) | 20 (52.6) | |
| Girl | 34 (48.6) | 12 (52.2) | 4 (44.4) | 18 (47.4) | |
| Gestational Age, weeks | 0.1973 | ||||
| Mean ± SD | 28.6 ± 2.9 | 27.8 ± 2.3 | 29.1 ± 3.6 | 28.9 ± 3.0 | |
| Min–Max | 22.0–39.1 | 24.0–33.0 | 22.0–33.6 | 24.0–39.1 | |
| Median (IQR) | 28.1 (27.0–30.3) | 28.0 (26.0–29.0) | 30.0 (28.1–31.1) | 28.3 (27.0–30.9) | |
| Gestational age < 32 weeks’ gestation | 0.3187 | ||||
| No | 8 (11.4) | 1 (4.3) | 2 (22.2) | 5 (13.2) | |
| Yes | 62 (88.6) | 22 (95.7) | 7 (77.8) | 33 (86.8) | |
| Birth weight, g | 0.9785 | ||||
| Mean ± SD | 1047.7 ± 317.6 | 1039.1 ± 352.7 | 1041.1 ± 296.9 | 1054.4 ± 308.1 | |
| Min–Max | 430.0–1630.0 | 482.0–1630.0 | 430.0–1380.0 | 530.0–1490.0 | |
| Median (IQR) | 1050.0 (770.0–1360.0) | 970.0 (750.0–1370.0) | 1040.0 (910.0–1290.0) | 1050.0 (720.0–1375.0) | |
| Birth weight, <1500 g | 0.1220 | ||||
| No | 2 (2.9) | 2 (8.7) | |||
| Yes | 68 (97.1) | 21 (91.3) | 9 (100) | 38 (100) | |
| Birth weight Z score (Fenton) | 0.2874 | ||||
| Mean ± SD | −0.4 ± 1.1 | −0.2 ± 1.2 | −0.8 ± 1.1 | −0.5 ± 1.1 | |
| Min–Max | −2.3–2.3 | −2.3–2.1 | −1.8–−1.8 | −2.2–2.3 | |
| Median (IQR) | −0.5 (−1.3–0.4) | −0.3 (−1.2–0.9) | −1.2 (−1.4–−0.3) | −0.5 (−1.3–0.2) | |
| NICU length of stay, days | 0.7633 | ||||
| Mean ± SD | 86.3 ± 35.3 | 89.7 ± 28.3 | 81.9 ± 40.2 | 85.3 ± 38.5 | |
| Min–Max | 13.0–168.0 | 32.0–132.0 | 28.0–159.0 | 13.0–168.0 | |
| Median (IQR) | 87.0 (58.0–113.0) | 87.0 (74.0–111.0) | 72.0 (62.0–101.0) | 87.0 (56.0–118.0) |
| Variable | n | Mean | Std Dev | Skewness | Median | Minimum | Maximum |
|---|---|---|---|---|---|---|---|
| FACTOR 1. Maternal sensitivity | 70 | 8.37 | 3.36 | 1.39 | 8 | 5 | 20 |
| FACTOR 2. Emotional concern | 70 | 17.37 | 5.31 | −0.43 | 18 | 5 | 27 |
| FACTOR 3. Positive interaction/engagement | 70 | 6.36 | 0.87 | 2.91 | 6 | 6 | 10 |
| Maternal Milk (MM) Provision Category 1 | n | Variable | n | Mean | Std Dev | Skewness | Median | Minimum | Maximum |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 23 | FACTOR_1 | 23 | 8.78 | 4.17 | 1.76 | 8 | 5 | 20 |
| FACTOR_2 | 23 | 15.57 | 5.79 | −0.34 | 17 | 6 | 26 | ||
| FACTOR_3 | 23 | 6.87 | 1.32 | 1.42 | 6 | 6 | 10 | ||
| 2 | 9 | FACTOR_1 | 9 | 8.33 | 3.5 | 1.35 | 8 | 5 | 16 |
| FACTOR_2 | 9 | 19.44 | 4.1 | −0.17 | 19 | 13 | 25 | ||
| FACTOR_3 | 9 | 6.22 | 0.44 | 1.62 | 6 | 6 | 7 | ||
| 3 | 38 | FACTOR_1 | 38 | 8.13 | 2.81 | 0.47 | 7 | 5 | 13 |
| FACTOR_2 | 38 | 17.97 | 5.06 | −0.31 | 18 | 5 | 27 | ||
| FACTOR_3 | 38 | 6.08 | 0.27 | 3.25 | 6 | 6 | 7 |
| Variable Label | Study Site (1 = BIDMC, 2 = BWH) | Maternal Age | Primiparous | Days in NICU | Infant Sex | Birth Weight Z Score (Fenton) | Gestational Age | Maternity Employment Leave 2 | Maternal Education 3 | Maternal SES | Maternal Race/Ethnicity (1 = Caucasian, 0 = Not Caucasian) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Mother-infant emotional connection factors | |||||||||||
| FACTOR 1. Maternal sensitivity (lower scores = greater sensitivity) | |||||||||||
| 0.11 | −0.02 | 0.02 | −0.17 | −0.057 | −0.03 | 0.15 | −0.05 | 0.23 | 0.21 | −0.02 | |
| FACTOR 2. Emotional concern (lower scores = greater concern) | |||||||||||
| −0.18 | −0.06 | −0.15 | 0.04 | −0.11 | −0.004 | 0.04 | 0.08 | −0.2 | −0.31 * | −0.09 | |
| FACTOR 3. Positive interaction/engagement (lower scores = greater engagement with infant) | |||||||||||
| 0.02 | 0.3 * | −0.15 | −0.05 | 0.06 | 0.04 | 0.06 | −0.2 | 0.37 * | 0.48 * | 0.21 * | |
| Maternal milk provision | |||||||||||
| Maternal milk provision category 1 | |||||||||||
| −0.23 | −0.34 * | 0.19 | −0.03 | −0.04 | −0.1 | 0.14 | 0.15 | −0.57 * | −0.57 * | −0.33 * | |
| Factor_1 (Maternal Sensitivity) | Factor_2 (Emotional Concern) | Factor_3 (Interaction/Engagement) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Low (More) | ↔ | High (Less) | Low (More) | ↔ | High (Less) | Low (More) | ↔ | High (Less) | ||||
| Milk Provision Category 1 | β | 95% CI | p | β | 95% CI | p | β | 95% CI | p | |||
| Unadjusted | ||||||||||||
| 2 | 0.00 | −3.06 | 3.06 | 1.000 | 2.00 | −3.16 | 7.16 | 0.442 | 0.00 | −0.27 | 0.27 | 1.000 |
| 3 | −1.00 | −3.05 | 1.05 | 0.334 | 1.00 | −2.47 | 4.47 | 0.567 | 0.00 | −0.18 | 0.18 | 1.000 |
| Adjusted by gestational age, maternal education level (categorical), and clustering by site | ||||||||||||
| 2 | 0.00 | −3.38 | 3.38 | 1.000 | 3.00 | 1.14 | 4.86 | 0.002 * | 0.00 | 0.00 | 0.00 | 0.017 * |
| 3 | 2.00 | 0.76 | 3.24 | 0.002 * | 3.00 | 0.00 | 6.00 | 0.050 | 0.00 | 0.00 | 0.00 | 0.866 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Viglione, C.; Cherkerzian, S.; Timpson, W.; Liu, C.H.; Woodward, L.J.; Belfort, M.B. Maternal Milk Provision in the Neonatal Intensive Care Unit and Mother–Infant Emotional Connection for Preterm Infants. Children 2022, 9, 296. https://doi.org/10.3390/children9020296
Viglione C, Cherkerzian S, Timpson W, Liu CH, Woodward LJ, Belfort MB. Maternal Milk Provision in the Neonatal Intensive Care Unit and Mother–Infant Emotional Connection for Preterm Infants. Children. 2022; 9(2):296. https://doi.org/10.3390/children9020296
Chicago/Turabian StyleViglione, Clare, Sara Cherkerzian, Wendy Timpson, Cindy H. Liu, Lianne J. Woodward, and Mandy B. Belfort. 2022. "Maternal Milk Provision in the Neonatal Intensive Care Unit and Mother–Infant Emotional Connection for Preterm Infants" Children 9, no. 2: 296. https://doi.org/10.3390/children9020296
APA StyleViglione, C., Cherkerzian, S., Timpson, W., Liu, C. H., Woodward, L. J., & Belfort, M. B. (2022). Maternal Milk Provision in the Neonatal Intensive Care Unit and Mother–Infant Emotional Connection for Preterm Infants. Children, 9(2), 296. https://doi.org/10.3390/children9020296