Making Biomarkers Relevant to Healthcare Innovation and Precision Medicine
Abstract
:1. Introduction
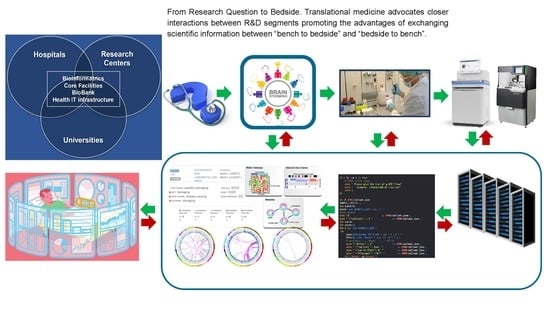
1.1. Convergence of Biomarkers, Translational Research, Personalized Medicine, and Future Healthcare
| Drug | Biomarker | Labeling Sections |
|---|---|---|
| Abemaciclib | ESR (Hormone Receptor) | Indications and Usage, Adverse Reactions, Clinical Studies |
| Abemaciclib | ERBB2 (HER2) | Indications and Usage, Adverse Reactions, Clinical Studies |
| Ado-Trastuzumab Emtansine | ERBB2 (HER2) | Indications and Usage, Dosage and Administration, Adverse Reactions, Clinical Pharmacology, Clinical Studies |
| Afatinib | EGFR | Indications and Usage, Dosage and Administration, Adverse Reactions, Clinical Studies |
| Alectinib | ALK | Indications and Usage, Dosage and Administration, Adverse Reactions, Clinical Pharmacology, Clinical Studies |
| Alpelisib | ERBB2 (HER2) | Indications and Usage, Dosage and Administration, Adverse Reactions, Clinical Studies |
| Alpelisib | ESR (Hormone Receptor) | Indications and Usage, Dosage and Administration, Adverse Reactions, Clinical Studies |
| Alpelisib | PIK3CA | Indications and Usage, Dosage and Administration, Adverse Reactions, Clinical Studies |
| Anastrozole | ESR, PGR (Hormone Receptor) | Indications and Usage, Adverse Reactions, Drug Interactions, Clinical Studies |
| Arsenic Trioxide | PML-RARA | Indications and Usage, Clinical Studies |
| Atezolizumab | CD274 (PD-L1) | Indications and Usage, Dosage and Administration, Adverse Reactions, Clinical Pharmacology, Clinical Studies |
| Atezolizumab | Gene Signature (T-effector) | Clinical Studies |
| Atezolizumab | EGFR | Indications and Usage, Clinical Studies |
| Atezolizumab | ALK | Indications and Usage, Clinical Studies |
| Avapritinib | PDGFRA | Indications and Usage, Dosage and Administration, Clinical Studies |
| Avelumab | CD274 (PD-L1) | Clinical Studies |
| Belinostat | UGT1A1 | Dosage and Administration, Clinical Pharmacology |
| Binimetinib | BRAF | Indications and Usage, Dosage and Administration, Warnings and Precautions, Adverse Reactions, Use in Specific Populations, Clinical Studies |
| Binimetinib | UGT1A1 | Clinical Pharmacology |
| Blinatumomab | BCR-ABL1 (Philadelphia chromosome) | Adverse Reactions, Clinical Studies |
| Bosutinib | BCR-ABL1 (Philadelphia chromosome) | Indications and Usage, Dosage and Administration, Warnings and Precautions, Adverse Reactions, Use in Specific Populations, Clinical Studies |
| Brentuximab Vedotin | ALK | Clinical Studies |
| Brentuximab Vedotin | TNFRSF8 (CD30) | Indications and Usage, Dosage and Administration, Adverse Reactions, Use in Specific Populations, Clinical Studies |
| Brigatinib | ALK | Indications and Usage, Dosage and Administration, Adverse Reactions, Clinical Studies |
| Busulfan | BCR-ABL1 (Philadelphia chromosome) | Clinical Studies |
| Cabozantinib | RET | Clinical Studies |
| Capecitabine | DPYD | Warnings and Precautions, Patient Counseling Information |
| Capmatinib | MET | Indications and Usage, Dosage and Administration, Clinical Studies |
| Ceritinib | ALK | Indications and Usage, Dosage and Administration, Warnings and Precautions, Adverse Reactions, Clinical Studies |
| Cetuximab | EGFR | Indications and Usage, Dosage and Administration, Adverse Reactions, Clinical Studies |
| Cetuximab | RAS | Indications and Usage, Dosage and Administration, Warnings and Precautions, Adverse Reactions, Clinical Studies |
| Cisplatin | TPMT | Adverse Reactions |
| Cobimetinib | BRAF | Indications and Usage, Dosage and Administration, Adverse Reactions, Clinical Studies |
| Crizotinib | ALK | Indications and Usage, Dosage and Administration, Adverse Reactions, Use in Specific Populations, Clinical Pharmacology, Clinical Studies |
| Crizotinib | ROS1 | Indications and Usage, Dosage and Administration, Adverse Reactions, Use in Specific Populations, Clinical Studies |
| Dabrafenib | BRAF | Indications and Usage, Dosage and Administration, Warnings and Precautions, Adverse Reactions, Clinical Pharmacology, Clinical Studies, Patient Counseling Information |
| Dabrafenib | G6PD | Warnings and Precautions, Adverse Reactions, Patient Counseling Information |
| Dabrafenib | RAS | Dosage and Administration, Warnings and Precautions |
| Dacomitinib | EGFR | Indications and Usage, Dosage and Administration, Adverse Reactions, Use in Specific Populations, Clinical Studies |
| Dasatinib | BCR-ABL1 (Philadelphia chromosome) | Indications and Usage, Dosage and Administration, Warnings and Precautions, Adverse Reactions, Use in Specific Populations, Clinical Studies |
| Denileukin Diftitox | IL2RA (CD25 antigen) | Indications and Usage, Clinical Studies |
| Dinutuximab | MYCN | Clinical Studies |
| Docetaxel | ESR, PGR (Hormone Receptor) | Clinical Studies |
| Durvalumab | CD274 (PD-L1) | Clinical Pharmacology, Clinical Studies |
| Duvelisib | Chromosome 17p | Clinical Studies |
| Enasidenib | IDH2 | Indications and Usage, Dosage and Administration, Clinical Pharmacology, Clinical Studies |
| Encorafenib | BRAF | Indications and Usage, Dosage and Administration, Warnings and Precautions, Adverse Reactions, Use in Specific Populations, Clinical Pharmacology, Clinical Studies |
| Encorafenib | RAS | Dosage and Administration, Warnings and Precautions, Clinical Studies |
| Enfortumab Vedotin-ejfv | NECTIN4 | Clinical Studies |
| Entrectinib | ROS1 | Indications and Usage, Dosage and Administration, Adverse Reactions, Use in Specific Populations, Clinical Pharmacology, Clinical Studies |
| Entrectinib | NTRK | Indications and Usage, Dosage and Administration, Adverse Reactions, Use in Specific Populations, Clinical Pharmacology, Clinical Studies |
| Erdafitinib | FGFR | Indications and Usage, Dosage and Administration, Adverse Reactions, Clinical Studies, Patient Counseling Information |
| Erdafitinib | CYP2C9 | Use in Specific Populations, Clinical Pharmacology |
| Eribulin | ERBB2 (HER2) | Clinical Studies |
| Eribulin | ESR, PGR (Hormone Receptor) | Clinical Studies |
| Erlotinib | EGFR | Indications and Usage, Dosage and Administration, Adverse Reactions, Clinical Studies |
| Everolimus | ERBB2 (HER2) | Indications and Usage, Dosage and Administration, Warnings and Precautions, Adverse Reactions, Use in Specific Populations, Clinical Pharmacology, Clinical Studies |
| Everolimus | ESR (Hormone Receptor) | Indications and Usage, Dosage and Administration, Warnings and Precautions, Adverse Reactions, Use in Specific Populations, Clinical Pharmacology, Clinical Studies |
| Exemestane | ESR, PGR (Hormone Receptor) | Indications and Usage, Dosage and Administration, Clinical Studies |
| Fam-Trastuzumab Deruxtecan-nxki | ERBB2 (HER2) | Indications and Usage, Warnings and Precautions, Adverse Reactions, Use in Specific Populations, Clinical Pharmacology, Clinical Studies |
| Fluorouracil | DPYD | Warnings and Precautions, Patient Counseling Information |
| Flutamide | G6PD | Warnings |
| Fulvestrant | ERBB2 (HER2) | Indications and Usage, Adverse Reactions, Clinical Studies |
| Fulvestrant | ESR, PGR (Hormone Receptor) | Indications and Usage, Adverse Reactions, Clinical Pharmacology, Clinical Studies |
| Gefitinib | EGFR | Indications and Usage, Dosage and Administration, Clinical Studies |
| Gefitinib | CYP2D6 | Clinical Pharmacology |
| Gemtuzumab Ozogamicin | CD33 | Indications and Usage, Dosage and Administration, Adverse Reactions, Clinical Studies |
| Gilteritinib | FLT3 | Indications and Usage, Dosage and Administration, Clinical Studies |
| Goserelin | ESR, PGR (Hormone Receptor) | Indications and Usage, Clinical Studies |
| Ibrutinib | Chromosome 17p | Indications and Usage, Clinical Studies |
| Ibrutinib | Chromosome 11q | Clinical Studies |
| Ibrutinib | MYD88 | Clinical Studies |
| Imatinib | KIT | Indications and Usage, Dosage and Administration, Clinical Studies |
| Imatinib | BCR-ABL1 (Philadelphia chromosome) | Indications and Usage, Dosage and Administration, Warnings and Precautions, Adverse Reactions, Use in Specific Populations, Clinical Pharmacology, Clinical Studies |
| Imatinib | PDGFRB | Indications and Usage, Dosage and Administration, Clinical Studies |
| Imatinib | FIP1L1-PDGFRA | Indications and Usage, Dosage and Administration, Clinical Studies |
| Inotuzumab Ozogamicin | BCR-ABL1 (Philadelphia chromosome) | Clinical Studies |
| Ipilimumab | HLA-A | Clinical Studies |
| Ipilimumab | Microsatellite Instability, Mismatch Repair | Indications and Usage, Adverse Reactions, Use in Specific Populations, Clinical Studies |
| Ipilimumab | CD274 (PD-L1) | Indications and Usage, Dosage and Administration, Use in Specific Populations, Clinical Studies |
| Ipilimumab | ALK | Indications and Usage, Adverse Reactions, Clinical Studies |
| Ipilimumab | EGFR | Indications and Usage, Adverse Reactions, Clinical Studies |
| Irinotecan | UGT1A1 | Dosage and Administration, Warnings and Precautions, Clinical Pharmacology |
| Isatuximab- irfc | Chromosome 17p | Clinical Studies |
| Isatuximab- irfc | Chromosome 4p;14q | Clinical Studies |
| Isatuximab- irfc | Chromosome 14q;16q | Clinical Studies |
| Ivosidenib | IDH1 | Indications and Usage, Dosage and Administration, Clinical Pharmacology, Clinical Studies |
| Ixabepilone | ERBB2 (HER2) | Clinical Studies |
| Ixabepilone | ESR, PGR (Hormone Receptor) | Clinical Studies |
| Lapatinib | ERBB2 (HER2) | Indications and Usage, Dosage and Administration, Adverse Reactions, Use in Specific Populations, Clinical Studies |
| Lapatinib | ESR, PGR (Hormone Receptor) | Indications and Usage, Dosage and Administration, Adverse Reactions, Use in Specific Populations, Clinical Studies |
| Lapatinib | HLA-DQA1 | Clinical Pharmacology |
| Lapatinib | HLA-DRB1 | Clinical Pharmacology |
| Larotrectinib | NTRK | Indications and Usage, Dosage and Administration, Adverse Reactions, Clinical Studies |
| Lenvatinib | Microsatellite Instability, Mismatch Repair | Indications and Usage, Adverse Reactions, Clinical Studies |
| Letrozole | ESR, PGR (Hormone Receptor) | Indications and Usage, Adverse Reactions, Clinical Studies |
| Lorlatinib | ALK | Indications and Usage, Adverse Reactions, Clinical Studies |
| Lorlatinib | ROS1 | Adverse Reactions |
| Lutetium Dotatate Lu-177 | SSTR | Indications and Usage, Adverse Reactions, Clinical Pharmacology, Clinical Studies |
| Mercaptopurine | TPMT | Dosage and Administration, Warnings and Precautions, Adverse Reactions, Clinical Pharmacology |
| Mercaptopurine | NUDT15 | Dosage and Administration, Warnings and Precautions, Clinical Pharmacology |
| Midostaurin | FLT3 | Indications and Usage, Dosage and Administration, Adverse Reactions, Clinical Studies |
| Midostaurin | NPM1 | Clinical Studies |
| Midostaurin | KIT | Clinical Studies |
| Neratinib | ERBB2 (HER2) | Indications and Usage, Adverse Reactions, Clinical Studies |
| Neratinib | ESR, PGR (Hormone Receptor) | Clinical Studies |
| Nilotinib | BCR-ABL1 (Philadelphia chromosome) | Indications and Usage, Dosage and Administration, Warnings and Precautions, Adverse Reactions, Use in Specific Populations, Clinical Pharmacology, Clinical Studies |
| Nilotinib | UGT1A1 | Clinical Pharmacology |
| Niraparib | BRCA, Genomic Instability (Homologous Recombination Deficiency) | Indications and Usage, Dosage and Administration, Clinical Studies |
| Nivolumab | BRAF | Adverse Reactions, Clinical Studies |
| Nivolumab | CD274 (PD-L1) | Indications and Usage, Dosage and Administration, Use in Specific Populations, Clinical Pharmacology, Clinical Studies |
| Nivolumab | Microsatellite Instability, Mismatch Repair | Indications and Usage, Clinical Studies |
| Nivolumab | EGFR | Indications and Usage, Adverse Reactions, Clinical Studies |
| Nivolumab | ALK | Indications and Usage, Adverse Reactions, Clinical Studies |
| Obinutuzumab | MS4A1 (CD20 antigen) | Clinical Studies |
| Olaparib | BRCA | Indications and Usage, Dosage and Administration, Warnings and Precautions, Adverse Reactions, Clinical Studies |
| Olaparib | ERBB2 (HER2) | Indications and Usage, Dosage and Administration, Adverse Reactions, Clinical Studies |
| Olaparib | ESR, PGR (Hormone Receptor) | Indications and Usage, Clinical Studies |
| Olaparib | BRCA, Genomic Instability (Homologous Recombination Deficiency) | Indications and Usage, Dosage and Administration, Adverse Reactions, Clinical Studies |
| Olaparib (5) | Homologous Recombination Repair | Indications and Usage, Dosage and Administration, Adverse Reactions, Clinical Studies |
| Olaparib (6) | PPP2R2A | Clinical Studies |
| Olaratumab | PDGFRA | Clinical Studies |
| Omacetaxine | BCR-ABL1 (Philadelphia chromosome) | Clinical Studies |
| Osimertinib | EGFR | Indications and Usage, Dosage and Administration, Adverse Reactions, Clinical Studies |
| Palbociclib | ESR (Hormone Receptor) | Indications and Usage, Adverse Reactions, Clinical Studies |
| Palbociclib | ERBB2 (HER2) | Indications and Usage, Adverse Reactions, Clinical Studies |
| Panitumumab | EGFR | Adverse Reactions, Clinical Pharmacology, Clinical Studies |
| Panitumumab | RAS | Indications and Usage, Dosage and Administration, Warnings and Precautions, Adverse Reactions, Clinical Studies |
| Pazopanib | UGT1A1 | Clinical Pharmacology |
| Pazopanib | HLA-B | Clinical Pharmacology |
| Pembrolizumab | BRAF | Adverse Reactions, Clinical Studies |
| Pembrolizumab | CD274 (PD-L1) | Indications and Usage, Dosage and Administration, Adverse Reactions, Clinical Studies |
| Pembrolizumab | Microsatellite Instability, Mismatch Repair | Indications and Usage, Dosage and Administration, Adverse Reactions, Use in Specific Populations, Clinical Studies |
| Pembrolizumab | EGFR | Indications and Usage, Adverse Reactions, Clinical Studies |
| Pembrolizumab | ALK | Indications and Usage, Adverse Reactions, Clinical Studies |
| Pembrolizumab | Tumor Mutational Burden | Indications and Usage, Dosage and Administration, Clinical Studies |
| Pemigatinib | FGFR2 | Indication and Usage, Dosage and Administration, Clinical Studies |
| Pertuzumab | ERBB2 (HER2) | Indications and Usage, Dosage and Administration, Warnings and Precautions, Adverse Reactions, Clinical Pharmacology, Clinical Studies |
| Pertuzumab | ESR, PGR (Hormone Receptor) | Clinical Studies |
| Ponatinib | BCR-ABL1 (Philadelphia chromosome) | Indications and Usage, Warnings and Precautions, Adverse Reactions, Use in Specific Populations, Clinical Studies |
| Raloxifene | ESR (Hormone Receptor) | Clinical Studies |
| Ramucirumab | EGFR | Indications and Usage, Dosage and Administration, Adverse Reactions, Clinical Studies |
| Ramucirumab | RAS | Clinical Studies |
| Rasburicase | G6PD | Boxed Warning, Contraindications, Warnings and Precautions |
| Rasburicase | CYB5R | Boxed Warning, Contraindications, Warnings and Precautions |
| Regorafenib | RAS | Indications and Usage, Clinical Studies |
| Ribociclib | ESR, PGR (Hormone Receptor) | Indications and Usage, Adverse Reactions, Clinical Studies |
| Ribociclib | ERBB2 (HER2) | Indications and Usage, Adverse Reactions, Clinical Studies |
| Rituximab | MS4A1 (CD20 antigen) | Indications and Usage, Dosage and Administration, Adverse Reactions, Use in Specific Populations, Clinical Studies |
| Rucaparib | BRCA | Indications and Usage, Dosage and Administration, Adverse Reactions, Clinical Studies |
| Rucaparib | CYP2D6 | Clinical Pharmacology |
| Rucaparib | CYP1A2 | Clinical Pharmacology |
| Rucaparib | BRCA, Loss of Heterozygosity (Homologous Recombination Deficiency) | Warnings and Precautions, Adverse Reactions, Clinical Studies |
| Sacituzumab Govitecan-hziy | UGT1A1 | Warnings and Precautions, Clinical Pharmacology |
| Selpercatinib | RET | Indications and Usage, Dosage and Administration, Adverse Reactions, Use in Specific Populations, Clinical Studies |
| Talazoparib | BRCA | Indications and Usage, Dosage and Administration, Adverse Reactions, Clinical Studies |
| Talazoparib | ERBB2 (HER2) | Indications and Usage, Adverse Reactions, Clinical Studies |
| Tamoxifen | ESR, PGR (Hormone Receptor) | Indications and Usage, Adverse Reactions, Clinical Pharmacology, Clinical Studies |
| Tamoxifen | F5 (Factor V Leiden) | Warnings and Precautions |
| Tamoxifen | F2 (Prothrombin) | Warnings and Precautions |
| Tamoxifen | CYP2D6 | Clinical Pharmacology |
| Thioguanine | TPMT | Dosage and Administration, Warnings, Precautions, Clinical Pharmacology |
| Thioguanine | NUDT15 | Dosage and Administration, Warnings, Precautions, Clinical Pharmacology |
| Tipiracil and Trifluridine | ERBB2 (HER2) | Indications and Usage, Adverse Reactions, Clinical Studies |
| Tipiracil and Trifluridine | RAS | Indications and Usage, Clinical Studies |
| Toremifene | ESR (Hormone Receptor) | Indications and Usage, Clinical Studies |
| Trametinib | BRAF | Indications and Usage, Dosage and Administration, Adverse Reactions, Clinical Pharmacology, Clinical Studies |
| Trametinib | G6PD | Adverse Reactions |
| Trametinib | RAS | Warnings and Precautions |
| Trastuzumab | ERBB2 (HER2) | Indications and Usage, Dosage and Administration, Clinical Pharmacology, Clinical Studies |
| Trastuzumab | ESR, PGR (Hormone Receptor) | Clinical Studies |
| Tretinoin | PML-RARA | Indications and Usage, Warnings, Clinical Pharmacology |
| Tucatinib | ERBB2 (HER2) | Indications and Usage, Adverse Reactions, Clinical Studies |
| Vemurafenib | BRAF | Indications and Usage, Dosage and Administration, Warnings and Precautions, Adverse Reactions, Use in Specific Populations, Clinical Pharmacology, Clinical Studies, Patient Counseling Information |
| Vemurafenib | RAS | Warnings and Precautions, Adverse Reactions |
| Venetoclax | Chromosome 17p | Clinical Studies |
| Venetoclax | Chromosome 11q | Clinical Studies |
| Venetoclax | TP53 | Clinical Studies |
| Venetoclax | IDH1 | Clinical Studies |
| Venetoclax | IDH2 | Clinical Studies |
| Venetoclax | IGH | Clinical Studies |
| Venetoclax | NPM1 | Clinical Studies |
| Venetoclax | FLT3 | Clinical Studies |
| Vincristine | BCR-ABL1 (Philadelphia chromosome) | Indications and Usage, Adverse Reactions, Clinical Studies |

1.2. Understanding the Patient through Biomarkers: Brief History and Trends, beyond “Discovery” by Correlation
1.3. Biomarkers towards Precision Medicine in Cancer
1.4. A Perspective on the Role of Biomarkers in Clinical Medicine
2. Applications of Biomarkers in Precision Medicine
2.1. Prevention and Early Intervention
2.2. Optimum Therapy Selection
2.3. Drug Safety
2.4. Patient Compliance
2.5. Improvement Rate of Success of Clinical Trials
2.6. Healthcare Benefit Cost Reduction
3. Therapeutic Treatment and Biomarkers

4. Treatment: Current Guidelines and Opportunities for Novel Tests by Working within the Existing Frameworks
5. Clinical Research: Information-Based and Adaptive Protocols through Biomarker Testing
6. Regulatory Approval and Availability of Physician Use and Patient Access
7. Clinical Utilization: Uptake Trends and Challenges in Impacting Clinical Medicine

8. Application of Biomarkers and Surrogate Endpoints in Clinical Efficacy Analysis and Formation of Clinical Practice Guidelines
9. Oncotype DX and Mamma/BluePrint Tests for Breast Cancer
10. Ethnic Disparities in Biomarkers
11. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Snyder, M.; Du, J.; Gerstein, M. Personal genome sequencing: Current approaches and challenges. Genes Dev. 2010, 24, 423–431. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Snyder, M.; Weissman, S.; Gerstein, M. Personal phenotypes to go with personal genomes. Mol. Syst. Biol. 2009, 5, 273. [Google Scholar] [CrossRef]
- NIH Definitions Working Group. Biomarkers and Surrogate Endpoints: Clinical Research and Applications. In Proceedings of the NIH-FDA Conference, Bethesda, MD, USA, 15–16 April 1999; Elsevier: Amsterdam, The Netherlands, 2000; pp. 1–9. [Google Scholar]
- Lesko, L.J.; Atkinson, A.J., Jr. Use of biomarkers and surrogate endpoints in drug development and regulatory decision making: Criteria, validation, strategies. Annu. Rev. Pharmacol. Toxicol. 2001, 41, 347–366. [Google Scholar] [CrossRef] [PubMed]
- Biomarkers Definitions Working Group; Atkinson, A.J., Jr.; Colburn, W.A.; DeGruttola, V.G.; DeMets, D.L.; Downing, G.J.; Hoth, D.F.; Oates, J.A.; Peck, C.C.; Schooley, R.T. Biomarkers and surrogate endpoints: Preferred definitions and conceptual framework. Clin. Pharmacol. Ther. 2001, 69, 89–95. [Google Scholar]
- Anderson, J.E.; Hansen, L.L.; Mooren, F.C.; Post, M.; Hug, H.; Zuse, A.; Los, M. Methods and biomarkers for the diagnosis and prognosis of cancer and other diseases: Towards personalized medicine. Drug Resist. Updates Rev. Comment. Antimicrob. Anticancer. Chemother. 2006, 9, 198–210. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Collins, C.D.; Purohit, S.; Podolsky, R.H.; Zhao, H.S.; Schatz, D.; Eckenrode, S.E.; Yang, P.; Hopkins, D.; Muir, A.; Hoffman, M.; et al. The application of genomic and proteomic technologies in predictive, preventive and personalized medicine. Vasc. Pharmacol. 2006, 45, 258–267. [Google Scholar] [CrossRef] [PubMed]
- Phillips, K.A.; Van Bebber, S.; Issa, A.M. Diagnostics and biomarker development: Priming the pipeline. Nat. Rev. Drug Discov. 2006, 5, 463–469. [Google Scholar] [CrossRef] [PubMed]
- Laterza, O.F.; Hendrickson, R.C.; Wagner, J.A. Molecular Biomarkers. Drug Inf. J./Drug Inf. Assoc. 2007, 41, 573–585. [Google Scholar] [CrossRef]
- US Food and Drug Administration. Challenge and Opportunity on the Critical Path to New Medical Products; US Food and Drug Administration (FDA): Silver Spring, MD, USA, 2004.
- Hodson, R. Precision medicine. Nature 2016, 537, S49. [Google Scholar] [CrossRef] [Green Version]
- Ashley, E.A. Towards precision medicine. Nat. Rev. Genet. 2016, 17, 507–522. [Google Scholar] [CrossRef]
- Bahcall, O. Precision medicine. Nature 2015, 526, 335. [Google Scholar] [CrossRef]
- Gromova, M.; Vaggelas, A.; Dallmann, G.; Seimetz, D. Biomarkers: Opportunities and Challenges for Drug Development in the Current Regulatory Landscape. Biomark. Insights 2020, 15, 1177271920974652. [Google Scholar] [CrossRef]
- Jose, J. Statins and its hepatic effects: Newer data, implications, and changing recommendations. J. Pharm. Bioallied Sci. 2016, 8, 23–28. [Google Scholar] [CrossRef]
- Keown, P. Book Review: Biomarkers in drug development: A handbook of practice, application and strategy. Biomark. Med. 2010, 4, 795–798. [Google Scholar] [CrossRef] [Green Version]
- Rifai, N.; Gillette, M.A.; Carr, S.A. Protein biomarker discovery and validation: The long and uncertain path to clinical utility. Nat. Biotechnol. 2006, 24, 971–983. [Google Scholar] [CrossRef]
- Gutman, S.; Kessler, L.G. The US Food and Drug Administration perspective on cancer biomarker development. Nat. Rev. Cancer 2006, 6, 565–571. [Google Scholar] [CrossRef]
- Even-Desrumeaux, K.; Baty, D.; Chames, P. State of the art in tumor antigen and biomarker discovery. Cancers 2011, 3, 2554–2596. [Google Scholar] [CrossRef] [Green Version]
- Davis, K.D.; Aghaeepour, N.; Ahn, A.H.; Angst, M.S.; Borsook, D.; Brenton, A.; Burczynski, M.E.; Crean, C.; Edwards, R.; Gaudilliere, B.; et al. Discovery and validation of biomarkers to aid the development of safe and effective pain therapeutics: Challenges and opportunities. Nat. Rev. Neurol. 2020, 16, 381–400. [Google Scholar] [CrossRef]
- US Food and Drug Administration—National Institutes of Health Biomarker Working Group. BEST (Biomarkers, EndpointS, and Other Tools) Resource; FDA: Silver Spring, MD, USA, 2016.
- European Medicines Agency. Guideline on the Clinical Investigation of Medicines for the Treatment of Alzheimer’s Disease; EMA: Amsterdam, The Netherlands, 2018. [Google Scholar]
- Niculescu, A.B.; Le-Niculescu, H.; Levey, D.; Roseberry, K.; Soe, K.C.; Rogers, J.; Khan, F.; Jones, T.; Judd, S.; McCormick, M.A.; et al. Towards precision medicine for pain: Diagnostic biomarkers and repurposed drugs. Mol. Psychiat. 2019, 24, 501–522. [Google Scholar] [CrossRef]
- Nagakura, Y. The need for fundamental reforms in the pain research field to develop innovative drugs. Expert Opin. Drug Discov. 2017, 12, 39–46. [Google Scholar] [CrossRef]
- Crimini, E.; Repetto, M.; Aftimos, P.; Botticelli, A.; Marchetti, P.; Curigliano, G. Precision medicine in breast cancer: From clinical trials to clinical practice. Cancer Treat. Rev. 2021, 98, 102223. [Google Scholar] [CrossRef] [PubMed]
- Bradbury, A.R.; Olopade, O.I. Genetic susceptibility to breast cancer. Rev. Endocr. Metab. Disord. 2007, 8, 255–267. [Google Scholar] [CrossRef] [PubMed]
- Antoniou, A.C.; Cunningham, A.P.; Peto, J.; Evans, D.G.; Lalloo, F.; Narod, S.A.; Risch, H.A.; Eyfjord, J.E.; Hopper, J.L.; Southey, M.C.; et al. The BOADICEA model of genetic susceptibility to breast and ovarian cancers: Updates and extensions. Br. J. Cancer 2008, 98, 1457–1466. [Google Scholar] [CrossRef] [PubMed]
- Antoniou, A.; Pharoah, P.D.; Narod, S.; Risch, H.A.; Eyfjord, J.E.; Hopper, J.L.; Loman, N.; Olsson, H.; Johannsson, O.; Borg, A.; et al. Average Risks of Breast and Ovarian Cancer Associated with BRCA1 or BRCA2 Mutations Detected in Case Series Unselected for Family History: A Combined Analysis of 22 Studies. Am. J. Hum. Genet. 2003, 72, 1117–1130. [Google Scholar] [CrossRef] [Green Version]
- Begg, C.B.; Haile, R.W.; Borg, A.; Malone, K.E.; Concannon, P.; Thomas, D.C.; Langholz, B.; Bernstein, L.; Olsen, J.H.; Lynch, C.F.; et al. Variation of breast cancer risk among BRCA1/2 carriers. JAMA 2008, 299, 194–201. [Google Scholar] [CrossRef] [Green Version]
- Brohet, R.M.; Velthuizen, M.E.; Hogervorst, F.B.L.; Meijers-Heijboer, H.E.; Seynaeve, C.; Collée, M.J.; Verhoef, S.; Ausems, M.G.E.M.; Hoogerbrugge, N.; Van Asperen, C.J.; et al. Breast and ovarian cancer risks in a large series of clinically ascertained families with a high proportion of BRCA1 and BRCA2 Dutch founder mutations. J. Med. Genet. 2014, 51, 98–107. [Google Scholar] [CrossRef]
- Chen, S.; Iversen, E.S.; Friebel, T.; Finkelstein, D.; Weber, B.L.; Eisen, A.; Peterson, L.E.; Schildkraut, J.M.; Isaacs, C.; Peshkin, B.N.; et al. Characterization of BRCA1 and BRCA2 Mutations in a Large United States Sample. J. Clin. Oncol. 2006, 24, 863–871. [Google Scholar] [CrossRef] [Green Version]
- Evans, D.G.; Shenton, A.; Woodward, E.; Lalloo, F.; Howell, A.; Maher, E.R. Penetrance estimates for BRCA1 and BRCA2 based on genetic testing in a Clinical Cancer Genetics service setting: Risks of breast/ovarian cancer quoted should reflect the cancer burden in the family. BMC Cancer 2008, 8, 155. [Google Scholar] [CrossRef] [Green Version]
- Ford, D.; Easton, D.; Stratton, M.; Narod, S.; Goldgar, D.; Devilee, P.; Bishop, T.; Weber, B.; Lenoir, G.; Chang-Claude, J.; et al. Genetic Heterogeneity and Penetrance Analysis of the BRCA1 and BRCA2 Genes in Breast Cancer Families. Am. J. Hum. Genet. 1998, 62, 676–689. [Google Scholar] [CrossRef] [Green Version]
- Gabai-Kapara, E.; Lahad, A.; Kaufman, B.; Friedman, E.; Segev, S.; Renbaum, P.; Beeri, R.; Gal, M.; Grinshpun-Cohen, J.; Djemal, K.; et al. Population-based screening for breast and ovarian cancer risk due to BRCA1 and BRCA2. Proc. Natl. Acad. Sci. USA 2014, 111, 14205–14210. [Google Scholar] [CrossRef] [Green Version]
- Kuchenbaecker, K.B.; Hopper, J.L.; Barnes, D.R.; Phillips, K.A.; Mooij, T.M.; Roos-Blom, M.J.; Jervis, S.; van Leeuwen, F.E.; Milne, R.L.; Andrieu, N.; et al. Risks of breast, ovarian, and contralateral breast cancer for BRCA1 and BRCA2 mutation carriers. JAMA 2017, 317, 2402–2416. [Google Scholar] [CrossRef] [Green Version]
- Thompson, D.; Easton, D. Breast Cancer Linkage Consortium. Variation in cancer risks, by mutation position, in BRCA2 mutation carriers. Am. J. Hum. Genet. 2001, 68, 410–419. [Google Scholar] [CrossRef] [Green Version]
- King, M.-C.; Marks, J.H.; Mandell, J.B. Breast and Ovarian Cancer Risks Due to Inherited Mutations in BRCA1 and BRCA2. Science 2003, 302, 643–646. [Google Scholar] [CrossRef]
- Struewing, J.P.; Hartge, P.; Wacholder, S.; Baker, S.M.; Berlin, M.; McAdams, M.; Timmerman, M.M.; Brody, L.C.; Tucker, M.A. The risk of cancer associated with specific mutations of BRCA1 and BRCA2 among Ashkenazi Jews. N. Engl. J. Med. 1997, 336, 1401–1408. [Google Scholar] [CrossRef]
- Spear, B.B.; Heath-Chiozzi, M.; Huff, J. Clinical application of pharmacogenetics. Trends Mol. Med. 2001, 7, 201–204. [Google Scholar] [CrossRef]
- Government of Australia; National Health and Medical Research Council. Personalized Medicine and Genetics. 2013. Available online: https://www.nhmrc.gov.au/_files_nhmrc/file/your_health/genetics/g004_personalised_medicine_genetics_131120.pdf (accessed on 29 January 2022).
- Food and Drug Administration. Principles for Codevelopment of an In Vitro Companion Diagnostic Device with Therapeutic Product. Available online: http://www.fda.gov/downloads/MedicalDevices/DeviceRegulationandGuidance/GuidanceDocuments/UCM510824.pdf (accessed on 29 January 2022).
- Mansfield, E.A. FDA perspective on companion diagnostics: An evolving paradigm. Clin. Cancer Res. 2014, 20, 1453–1457. [Google Scholar] [CrossRef] [Green Version]
- Dracopoli, N.C.; Boguski, M.S. The Evolution of Oncology Companion Diagnostics from Signal Transduction to Immuno-Oncology. Trends Pharmacol. Sci. 2017, 38, 41–54. [Google Scholar] [CrossRef]
- Cobleigh, M.A.; Vogel, C.L.; Tripathy, D.; Robert, N.J.; Scholl, S.; Fehrenbacher, L.; Wolter, J.M.; Paton, V.; Shak, S.; Lieberman, G.; et al. Multinational study of the efficacy and safety of humanized anti-HER2 monoclonal antibody in women who have HER2-overexpressing metastatic breast cancer that has progressed after chemotherapy for metastatic disease. J. Clin. Oncol. 1999, 17, 2639–2648. [Google Scholar] [CrossRef]
- Food and Drug Administration. List of Cleared or Approved Companion Diagnostic devices (In Vitro and Imaging Tools). Available online: http://www.fda.gov/MedicalDevices/ProductsandMedicalprocedures/inVitroDiagnostics/ucm301431.htm (accessed on 29 November 2021).
- Schiller, G.J. High-risk acute myelogenous leukemia: Treatment today… and tomorrow. Hematology 2013, 2013, 201–208. [Google Scholar] [CrossRef] [Green Version]
- Lin, T.L.; Levy, M.Y. Acute myeloid leukemia: Focus on novel therapeutic strategies. Clin. Med. Insights Oncol. 2012, 6, 205–217. [Google Scholar] [CrossRef] [Green Version]
- Rydapt®. 2017 European Medicines Agency-EMA. Available online: https://www.ema.europa.eu/en/medicines/human/EPAR/rydapt (accessed on 27 November 2021).
- Temple, R.J. Qualification of Biomarkers as Surrogate Endpoints of Chronic Disease Risk. In Proceedings of the Committee on Qualification of Biomarkers and Surrogate. Endpoints in Chronic Disease, Meeting 2 Workshop, Washington, DC, USA, 6 April 2009. [Google Scholar]
- Ball, J.R.; Micheel, C.M. (Eds.) 2 Review: Evaluating and Regulating Biomarker Use. In Evaluation of Biomarkers and Surrogate Endpoints in Chronic Disease; Institute of Medicine (US) Committee on Qualification of Biomarkers and Surrogate Endpoints in Chronic Disease; National Academies Press: Washington, DC, USA, 2010. Available online: https://www.ncbi.nlm.nih.gov/books/NBK220288/ (accessed on 1 February 2022).
- McVeigh, T.P.; Kerin, M.J. Clinical use of the Oncotype DX genomic test to guide treatment decisions for patients with invasive breast cancer. Breast Cancer Targets Ther. 2017, 9, 393–400. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Paik, S.; Shak, S.; Tang, G.; Kim, C.; Baker, J.; Cronin, M.; Baehner, F.L.; Walker, M.G.; Watson, D.; Park, T.; et al. A multigene assay to predict recurrence of tamoxifen-treated, node-negative breast cancer. N. Engl. J. Med. 2004, 351, 2817–2826. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Habel, L.A.; Shak, S.; Jacobs, M.K.; Capra, A.; Alexander, C.; Pho, M.; Baker, J.; Walker, M.; Watson, D.; Hackett, J.; et al. A population-based study of tumor gene expression and risk of breast cancer death among lymph node-negative patients. Breast Cancer Res. 2006, 8, R25. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tang, G.; Shak, S.; Paik, S.; Anderson, S.J.; Costantino, J.P.; Geyer, C.E., Jr.; Mamounas, E.P.; Wickerham, D.L.; Wolmark, N. Comparison of the prognostic and predictive utilities of the 21-gene Recurrence Score assay and Adjuvant! for women with node-negative, ER-positive breast cancer: Results from NSABP B-14 and NSABP B-20. Breast. Cancer Res. Treat. 2011, 127, 133–142. [Google Scholar] [CrossRef] [Green Version]
- Sgroi, D.C.; Sestak, I.; Cuzick, J.; Zhang, Y.; Schnabel, C.A.; Schroeder, B.; Erlander, M.G.; Dunbier, A.; Sidhu, K.; Lopez-Knowles, E.; et al. Prediction of late distant recurrence in patients with oestrogen-receptor-positive breast cancer: A prospective comparison of the breast-cancer index (BCI) assay, 21-gene recurrence score, and IHC4 in the TransATAC study population. Lancet. Oncol. 2013, 14, 1067–1076. [Google Scholar] [CrossRef] [Green Version]
- Sestak, I.; Dowsett, M.; Zabaglo, L.; Lopez-Knowles, E.; Ferree, S.; Cowens, J.W.; Cuzick, J. Factors predicting late recurrence for estrogen receptor-positive breast cancer. J. Natl. Cancer Inst. 2013, 105, 1504–1511. [Google Scholar] [CrossRef] [Green Version]
- Sparano, J.A.; Gray, R.J.; Makower, D.F.; Pritchard, K.I.; Albain, K.S.; Hayes, D.F.; Geyer, C.E., Jr.; Dees, E.C.; Perez, E.A.; Olson, J.A., Jr.; et al. Prospective Validation of a 21-Gene Expression Assay in Breast Cancer. N. Engl. J. Med. 2015, 373, 2005–2014. [Google Scholar] [CrossRef]
- Early Breast Cancer Trialists’ Collaborative Group. Comparisons between different polychemotherapy regimens for early breast cancer: Meta-analyses of long-term outcome among 100,000 women in 123 randomised trials. Lancet 2012, 379, 432–444. [Google Scholar] [CrossRef] [Green Version]
- van ’t Veer, L.J.; Dai, H.; van de Vijver, M.J.; He, Y.D.; Hart, A.A.; Mao, M.; Peterse, H.L.; van der Kooy, K.; Marton, M.J.; Witteveen, A.T.; et al. Gene expression profiling predicts clinical outcome of breast cancer. Nature 2002, 415, 530–536. [Google Scholar] [CrossRef] [Green Version]
- Tian, S.; Roepman, P.; Van’t Veer, L.J.; Bernards, R.; de Snoo, F.; Glas, A.M. Biological functions of the genes in the mammaprint breast cancer profile reflect the hallmarks of cancer. Biomark. Insights 2010, 5, 129–138. [Google Scholar] [CrossRef] [Green Version]
- Buyse, M.; Loi, S.; van ’t Veer, L.; Viale, G.; Delorenzi, M.; Glas, A.M.; d’Assignies, M.S.; Bergh, J.; Lidereau, R.; Ellis, P.; et al. Validation and clinical utility of a 70-gene prognostic signature for women with node-negative breast cancer. J. Natl. Cancer Inst. 2006, 98, 1183–1192. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Knauer, M.; Mook, S.; Rutgers, E.J.; Bender, R.A.; Hauptmann, M.; van de Vijver, M.J.; Koornstra, R.H.; Bueno-de-Mesquita, J.M.; Linn, S.C.; van ’t Veer, L.J. The predictive value of the 70-gene signature for adjuvant chemotherapy in early breast cancer. Breast Cancer Res. Treat. 2010, 120, 655–661. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Drukker, C.A.; Bueno-de-Mesquita, J.M.; Retel, V.P.; van Harten, W.H.; van Tinteren, H.; Wesseling, J.; Roumen, R.M.; Knauer, M.; van ’t Veer, L.J.; Sonke, G.S.; et al. A prospective evaluation of a breast cancer prognosis signature in the observational RASTER study. Int. J. Cancer 2013, 133, 929–936. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cardoso, F.; van ’t Veer, L.J.; Bogaerts, J.; Slaets, L.; Viale, G.; Delaloge, S.; Pierga, J.Y.; Brain, E.; Causeret, S.; DeLorenzi, M.; et al. 70-Gene Signature as an Aid to Treatment Decisions in Early-Stage Breast Cancer. N. Engl. J. Med. 2016, 375, 717–729. [Google Scholar] [CrossRef] [Green Version]
- Mittempergher, L.; Delahaye, L.J.; Witteveen, A.T.; Snel, M.H.; Mee, S.; Chan, B.Y.; Dreezen, C.; Besseling, N.; Luiten, E.J.; Glas, A.M. Performance Characteristics of the BluePrint® Breast Cancer Diagnostic Test. Transl. Oncol. 2020, 13, 100756. [Google Scholar] [CrossRef]
- Perjeta. Prescribing Information. Genentech. 2020. Available online: https://bit.ly/3m56D27 (accessed on 2 September 2021).
- van Golen, K.L.; Cristofanilli, M. The Third International Inflammatory Breast Cancer Meeting. Breast Cancer Res. 2013, 15, 318–321. [Google Scholar] [CrossRef] [Green Version]
- Woodward, W.A.; Cristofanilli, M.; Merajver, S.D.; Van Laere, S.; Pusztai, L.; Bertucci, F.; Berditchevski, F.; Polyak, K.; Overmoyer, B.; Devi, G.R.; et al. Scientific Summary from the Morgan Welch MD Anderson Cancer Center Inflammatory Breast Cancer (IBC) Program 10(th) Anniversary Conference. J. Cancer 2017, 8, 3607–3614. [Google Scholar] [CrossRef] [Green Version]
- Soliman, A.S.; Banerjee, M.; Lo, A.C.; Ismail, K.; Hablas, A.; Seifeldin, I.A.; Ramadan, M.; Omar, H.G.; Fokuda, A.; Harford, J.B.; et al. High proportion of inflammatory breast cancer in the Population-based Cancer Registry of Gharbiah, Egypt. Breast J. 2009, 15, 432–434. [Google Scholar] [CrossRef] [Green Version]
- Zayed, H. The Qatar genome project: Translation of whole-genome sequencing into clinical practice. Int. J. Clin. Pract. 2016, 70, 832–834. [Google Scholar] [CrossRef]
- Zayed, H. The Arab genome: Health and wealth. Gene 2016, 592, 239–243. [Google Scholar] [CrossRef]
- Abdul Rahim, H.F.; Ismail, S.I.; Hassan, A.; Fadl, T.; Khaled, S.M.; Shockley, B.; Nasrallah, C.; Qutteina, Y.; Elmaghraby, E.; Yasin, H.; et al. Willingness to participate in genome testing: A survey of public attitudes from Qatar. J. Hum. Genet. 2020, 65, 1067–1073. [Google Scholar] [CrossRef] [PubMed]
- Al-Dewik, N.; Al-Mureikhi, M.; Shahbeck, N.; Ali, R.; Al-Mesaifri, F.; Mahmoud, L.; Othman, A.; AlMulla, M.; Sulaiman, R.A.; Musa, S.; et al. Clinical genetics and genomic medicine in Qatar. Mol. Genet. Genomic. Med. 2018, 6, 702–712. [Google Scholar] [CrossRef] [PubMed]
- Qoronfleh, M.W.; Chouchane, L.; Mifsud, B.; Al Emadi, M.; Ismail, S. THE FUTURE OF MEDICINE, healthcare innovation through precision medicine: Policy case study of Qatar. Life Sci. Soc. Policy. 2020, 16, 12. [Google Scholar] [CrossRef] [PubMed]



Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Al-Dewik, N.I.; Younes, S.N.; Essa, M.M.; Pathak, S.; Qoronfleh, M.W. Making Biomarkers Relevant to Healthcare Innovation and Precision Medicine. Processes 2022, 10, 1107. https://doi.org/10.3390/pr10061107
Al-Dewik NI, Younes SN, Essa MM, Pathak S, Qoronfleh MW. Making Biomarkers Relevant to Healthcare Innovation and Precision Medicine. Processes. 2022; 10(6):1107. https://doi.org/10.3390/pr10061107
Chicago/Turabian StyleAl-Dewik, Nader I., Salma N. Younes, Musthafa Mohamed Essa, Surajit Pathak, and M. Walid Qoronfleh. 2022. "Making Biomarkers Relevant to Healthcare Innovation and Precision Medicine" Processes 10, no. 6: 1107. https://doi.org/10.3390/pr10061107
APA StyleAl-Dewik, N. I., Younes, S. N., Essa, M. M., Pathak, S., & Qoronfleh, M. W. (2022). Making Biomarkers Relevant to Healthcare Innovation and Precision Medicine. Processes, 10(6), 1107. https://doi.org/10.3390/pr10061107