Insights into the Antimicrobial Potential of Dithiocarbamate Anions and Metal-Based Species
Abstract
:1. Introduction
2. Chemistry
3. Screening of Dithiocarbamates for Antimicrobial Activity
3.1. Organic Derivatives
3.2. Transition Metal Dithiocarbamates
3.3. Main Group Element Dithiocarbamates
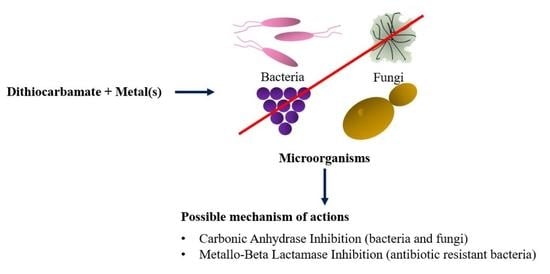
4. Possible Mechanisms of Action
4.1. Carbonic Anhydrase Inhibitors
4.1.1. Bacteria
4.1.2. Fungi
4.1.3. Protozoa
4.2. Metallo-Beta-Lactamase Inhibitors
5. Overview
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Bacteria | Infections and Diseases |
|---|---|
| Acinetobacter baumannii | Pneumonia, urinary tract infections, blood-stream infections, wound infections, and meningitis |
| Aeromonas hydrophila | Soft-tissue infections, diarrhea, bacteremia, and septicemia |
| Aggregatibacter actinomycetemcomitans | Chronic and localized aggressive periodontitis |
| Bacillus cereus | Food poisoning, ocular infection, bacteremia, and pneumonia |
| Bacillus pumilus | Bacteremia and sepsis |
| Bacillus subtilis | Bacteremia, endocarditis, pneumonia, and septicemia |
| Citrobacter freundii | Gastroenteritis, neonatal meningitis, septicemia, and urinary tract infections |
| Enterobacter aerogenes | Iatrogenic bacteremia, septicemia, pneumonia, urinary tract infections, and wound infections |
| Enterobacter cloacae | Nosocomial bloodstream infections |
| Enterococcus faecalis | Foodborne infections, endocarditis, bacteremia, urinary tract infections, intra-abdomen, pelvis, and soft tissue infections |
| Enterococcus raffinosus | Nosocomial infections, including bacteremia, urinary tract infection, wound, and abscesses |
| Escherichia coli | Urinary tract infections, diarrhea, sepsis, meningitis, respiratory infections, and pericarditis |
| Fusobacterium nucleatum | Periodontal disease and colorectal cancer |
| Klebsiella pneumoniae | Urinary tract infections, pneumonia, septicemia, wound infections, and soft tissue infections |
| Lactobacillus plantarum | Part of the normal microbiota and a lactic acid bacterium |
| Legionella pneumophila | Legionnaires’ disease and pneumonia |
| Leuconostoc mesenteroides | Part of the normal microbiota and a lactic acid bacterium |
| Listeria monocytogenes | Listeriosis—a foodborne infection |
| Mycobacterium marinum | Chronic skin infections—aquarium granuloma, swimming pool granuloma or fish tank granuloma |
| Mycobacterium tuberculosis | Tuberculosis |
| Pasteurella multocida | Bacteremia, cellulitis, endocarditis, lymphadenopathy, meningitis, and osteomyelitis |
| Porphyromonas gingivalis | Periodontal disease and putative causative agent for rheumatoid arthritis, and neurodegenerative diseases |
| Proteus mirabilis | Kidney failure, kidney stones, pneumonia, and sepsis |
| Pseudomonas aeruginosa | Bacteremia, chronic lung infection, acute ulcerative keratitis, and urinary tract infections |
| Rhodococcus sp. | Rhodococcus equi in the genus causes zoonotic infection and infections in immunosuppressed patients, including those in HIV patients |
| Salmonella enterica serotype Typhi | Typhoid fever |
| Salmonella enterica serotype Typhimurium | Salmonellosis |
| Serratia mercescens | Respiratory tract, the urinary tract, surgical wounds, and soft tissues in hospitalized patients |
| Shigella flexneri | Shigellosis (diarrhea, severe abdominal pain, cramping, septicemia, pneumonia, and haemolytic uremic syndrome) |
| Staphylococcus aureus | Skin (Scalded skin syndrome, skin abscesses) soft tissue, bone (osteomyelitis), joint and central intravenous line infections, endocarditis, staphylococcal meningitis, septic arthritis, and toxic shock syndrome |
| Staphylococcus epidermidis | Prosthetic valve endocarditis (PVE) infections, intracardiac abscesses, bacteremia, and neonatal sepsis |
| Staphylococcus haemolyticus | Meningitis, endocarditis, prosthetic joint infections, and bacteremia in immunocompromised individuals |
| Staphylococcus sciuri | Subcutaneous abscesses, dermatitis, and surgical wound infections |
| Staphylococcus simulans | Skin and soft tissue infections |
| Streptococcus pneumoniae | Pneumonia and sepsis |
| Streptococcus pyogenes | Pharyngitis (Strep Throat), cellulitis, Scarlet Fever, Streptococcal Toxic Shock Syndrome, impetigo, acute rheumatic fever, and type II necrotizing fasciitis |
| Streptococcus sanguinis | Bacterial endocarditis |
| Vibrio cholerae | Cholera |
| Fungi | Infections and Diseases |
|---|---|
| Alaternaria solani | Septic arthritis, osteomyelitis, and epiglottitis |
| Alternaria alternata | Rhinosinusitis |
| Aspergillus carbonarius | Human kidney diseases such as chronic interstitial nephropathy and renal diseases |
| Aspergillus flavus | Chronic granulomatous sinusitis, keratitis, cutaneous aspergillosis, wound infections, and osteomylitis |
| Aspergillus fumigatus | Abscesses, pleural empyema, cholangitis, thrombophlebitis, and haemolytic uraemic syndrome |
| Aspergillus niger | Respiratory infections associated with pneumonia in immunocompromised individuals |
| Aspergillus parasiticus | Produces aflatoxins known as carcinogens for liver cancer |
| Candida albicans (formerly known as Miconia albicans) | Candidiasis, including vaginal candidiasis, and candidemia |
| Candida auris | Invasive candidiasis in immunocompromised patients |
| Candida glabrata | Superficial candidiasis, including vulvovaginitis, oral thrush, and candidemia |
| Candida parapsilosis | Candidal arthritis and candidemia |
| Candida pseudotropicalis | Fungemia and invasive diseases in spleen and kidney in immunocompromised individuals |
| Candida tropicalis | Candidemia |
| Cryptococcus neoformans | Cryptococcosis and cryptococcal meningitis |
| Curvularia senegalensis | A plant pathogen, but an etiologic agent of allergic sinusitis, keratitis, and endophthalmites in immunocompetent and immunosuppressed patients |
| Fusarium solani | Keratitis, onychomycosis, endophthalmitis, and skin and musculoskeletal infections |
| Fusarium oxysporium | Urinary tract infection, diarrhea, sepsis, meningitis, respiratory infections, pericarditis, and septicemia of poultry |
| Helminthosporium solani | A plant pathogen that causes silver scurf in potatoes |
| Microsporum canis | Zoophilic dermatophytosis but occasionally causes human skin infections |
| Microsporum gypseum | Dermatophytosis |
| Penicillium citrinum | Mycotic keratitis, urinary tract infection, and pneumonia in immunocompromised individuals |
| Rhizoctonia solani | A plant pathogen that causes damping-off on cultivated plants including potato, legumes, and vegetables |
| Sacchoromyces cerevisiae | Part of the normal microbiota but has been shown to cause fungemia in critically ill patients |
| Sporothrix schenckii | Sporotrichosis, also known as rose garden disease |
| Trichoderma reesie | A soil fungus that rarely causes human diseases |
| Trichoderma viride | Pulmonary mycoma in immunocompromised individuals |
| Trichophyton longifusus | Dermatophytosis |
| Trichophyton mentagrophytes | Dermatophytosis |
| Trichophyton rubrum | Dermatophytosis |
| Trichothecium roseum | A plant pathogen that causes pink rot on apples and white stains on grapes |
| Parasites | Infections and Diseases |
|---|---|
| Leishmania major | Leishmaniasis |
| Toxoplasma gondii | Toxoplasmosis |
| Trichomonas vaginalis | Trichomoniasis |
References
- Hogarth, G. Transition metal dithiocarbamates: 1978–2003. In Progress in Inorganic Chemistry; Karlin, K.D., Ed.; John Wiley & Sons: Hoboken, NJ, USA, 2005; Volume 53, pp. 71–561. [Google Scholar] [CrossRef]
- Heard, P.J. Main group dithiocarbamate complexes. In Progress in Inorganic Chemistry; Karlin, K.D., Ed.; John Wiley & Sons: Hoboken, NJ, USA, 2005; Volume 53, pp. 1–69. [Google Scholar] [CrossRef]
- Karle, I.L.; Estlin, J.A.; Britts, K. The crystal and molecular structure of tetraethylthiuram disulfide, C10N2H20S4. Acta Crystallogr. 1967, 22, 273–280. [Google Scholar] [CrossRef] [PubMed]
- Viola-Rhenals, M.; Patel, K.R.; Jaimes-Santamaria, L.; Wu, G.; Liu, J.; Dou, Q.P. Recent advances in Antabuse (disulfiram): The importance of its metal-binding ability to its anticancer activity. Curr. Med. Chem. 2018, 25, 506–524. [Google Scholar] [CrossRef]
- Guardiola, F.A.; Cuesta, A.; Meseguer, J.; Esteban, M.A. Risks of using antifouling biocides in aquaculture. Int. J. Mol. Sci. 2012, 13, 1541–1560. [Google Scholar] [CrossRef] [PubMed]
- Lefton, J.B.; Pekar, K.B.; Runčevski, T. The crystal structure of Zineb, seventy-five years later. Cryst. Growth Des. 2020, 20, 851–857. [Google Scholar] [CrossRef]
- Aly, A.A.; Brown, A.B.; Bedair, T.M.I.; Ishak, E.A. Dithiocarbamate salts: Biological activity, preparation, and utility in organic synthesis. J. Sulfur Chem. 2012, 33, 605–617. [Google Scholar] [CrossRef]
- Lal, N. Dithiocarbamates: A versatile class of compounds in medicinal chemistry. Chem. Biol. Interface 2014, 4, 321–340. [Google Scholar]
- Bala, V.; Gupta, G.; Sharma, V.L. Chemical and medicinal versatility of dithiocarbamates: An overview. Mini Rev. Med. Chem. 2014, 14, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Thind, T.S.; Hollomon, D.W. Thiocarbamate fungicides: Reliable tools in resistance management and future outlook. Pest Manag. Sci. 2018, 74, 1547–1551. [Google Scholar] [CrossRef] [PubMed]
- Hogarth, G. Metal-dithiocarbamate complexes: Chemistry and biological activity. Mini Rev. Med. Chem. 2012, 12, 1202–1215. [Google Scholar] [CrossRef] [PubMed]
- Buac, D.; Schmitt, S.; Ventro, G.; Kona, F.R.; Dou, Q.P. Dithiocarbamate-based coordination compounds as potent proteasome inhibitors in human cancer cells. Mini Rev. Med. Chem. 2012, 12, 1193–1201. [Google Scholar] [CrossRef] [Green Version]
- Nagy, E.M.; Ronconi, L.; Nardon, C.; Fregona, D. Noble metal-dithiocarbamates precious allies in the fight against cancer. Mini Rev. Med. Chem. 2012, 12, 1216–1229. [Google Scholar] [CrossRef] [PubMed]
- Fleming, A. On the antibacterial action of cultures of a penicillium, with special reference to their use in the isolation of B. influenzæ. Br. J. Exp. Pathol. 1929, 10, 226–236. [Google Scholar] [CrossRef]
- D’Costa, V.M.; King, C.E.; Kalan, L.; Morar, M.; Sung, W.W.; Schwarz, C.; Froese, D.; Zazula, G.; Calmels, F.; Debruyne, R.; et al. Antibiotic resistance is ancient. Nature 2011, 477, 457–461. [Google Scholar] [CrossRef] [PubMed]
- Beardsley, J.; Hallidat, C.L.; Chen, S.C.; Sorrell, T.C. Responding to the emergence of antifungal drug resistance: Perspectives from the bench and the bedside. Future Microbiol. 2018, 13, 1175–1191. [Google Scholar] [CrossRef] [Green Version]
- Perlin, D.S.; Rautemaa-Richardson, R.; Alastruey-Izquierdo, A. The global problem of antifungal resistance: Prevalence, mechanisms, and management. Lancet Infect. Dis. 2017, 17, e383–e392. [Google Scholar] [CrossRef]
- Gielen, M.; Tiekink, E.R.T. (Eds.) Metallotherapeutic drugs and metal-based diagnostic agents: The use of metals in medicine; John Wiley & Sons Ltd.: Chichester, UK, 2005. [Google Scholar] [CrossRef]
- Claudel, M.; Schwarte, J.V.; Fromm, K.M. New antimicrobial strategies based on metal complexes. Chemistry 2020, 2, 56. [Google Scholar] [CrossRef]
- Frei, A. Metal complexes, an untapped source of antibiotic potential? Antibiotics 2020, 9, 90. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Frei, A.; Zuegg, J.; Elliott, A.G.; Baker, M.; Braese, S.; Brown, C.; Chen, F.; Dowson, C.G.; Dujardin, G.; Jung, N.; et al. Metal complexes as a promising source for new antibiotics. Chem. Sci. 2020, 11, 2627–2639. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Anthony, E.J.; Bolitho, E.M.; Bridgewater, H.E.; Carter, O.W.L.; Donnelly, J.M.; Imberti, C.; Lant, E.C.; Lermyte, F.; Needham, R.J.; Palau, M.; et al. Metallodrugs are unique: Opportunities and challenges of discovery and development. Chem. Sci. 2020, 11, 12888–12917. [Google Scholar] [CrossRef]
- Fleming, A. On the specific antibacterial properties of penicillin and potassium tellurite. Incorporating a method of demonstrating some bacterial antagonisms. J. Pathol. Bacteriol. 1932, 35, 831–842. [Google Scholar] [CrossRef]
- Tiekink, E.R.T. Therapeutic potential of selenium and tellurium compounds: Opportunities yet unrealised. Dalton Trans. 2012, 41, 6390–6395. [Google Scholar] [CrossRef] [PubMed]
- Taylor, R.; Wood, P.A. A million crystal structures: The whole is greater than the sum of its parts. Chem. Rev. 2019, 119, 9427–9477. [Google Scholar] [CrossRef] [PubMed]
- Kang, M.S.; Choi, E.K.; Choi, D.H.; Ryu, S.Y.; Lee, H.H.; Kang, H.C.; Koh, J.T.; Kim, O.S.; Hwang, Y.C.; Yoon, S.J.; et al. Antibacterial activity of pyrrolidine dithiocarbamate. FEMS Microbiol. Lett. 2008, 280, 250–254. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Capms, M.; Boothroyd, J.C. Toxoplasma gondii: Selective killing of extracellular parasites by oxidation using pyrrolidine dithiocarbamate. Exp. Parasitol. 2001, 98, 206–214. [Google Scholar] [CrossRef]
- Choi, E.K.; Lee, H.H.; Kang, M.S.; Kim, B.G.; Lim, H.S.; Kim, S.M.; Kang, I.C. Potentiation of bacterial killing activity of zinc chloride by pyrrolidine dithiocarbamate. J Microbiol. 2010, 48, 40–43. [Google Scholar] [CrossRef]
- Vuksanović, V.; Leka, Z.; Terzić, N. Antibacterial effect of synthesized dithiocarbamate K-daap. Fresenius Environ. Bull. 2013, 22, 3803–3807. [Google Scholar]
- Arvanitis, N.; Kotzamanidis, C.Z.; Skaracis, G.N.; Karagouni, A.D. The effectiveness of commercial antimicrobial compounds against saccharolytic microorganisms isolated from a beet sugar production line. World J. Microbiol. Biotechnol. 2004, 20, 291–296. [Google Scholar] [CrossRef]
- Ejelonu, B.C.; Olagboye, S.A.; Oyeneyin, O.E.; Ebiesuwa, O.A.; Bada, O.E. Synthesis, characterization and antimicrobial activities of sulfadiazine schiff base and phenyl Dithiocarbamate mixed ligand metal complexes. Open J. Appl. Sci. 2018, 8, 346–354. [Google Scholar] [CrossRef] [Green Version]
- Ndukwe, G.I.; Nzeneri, J.U.; Abayeh, O.J. Antibacterial assay of two synthesized dithiocarbamate ligands. Am. J. Chem. 2018, 5, 51–57. [Google Scholar]
- Mambaa, S.M.; Mishra, A.K.; Mambaa, B.B.; Njobeh, P.B.; Dutton, M.F.; Fosso-Kankeu, E. Spectral, thermal and in vitro antimicrobial studies of cyclohexylamine-N-dithiocarbamate transition metal complexes. Spectrochim. Acta A Mol. Biomol. Spectrosc. 2010, 77, 579–587. [Google Scholar] [CrossRef] [PubMed]
- Aspatwar, A.; Hammarén, M.; Koskinen, S.; Luukinen, B.; Barker, H.; Carta, F.; Supuran, C.T.; Parikka, M.; Parkkila, S. β-CA specific inhibitor dithiocarbamate Fc14–584B: A novel antimycobacterial agent with potential to treat drug-resistant tuberculosis. J. Enzyme Inhib. Med. Chem. 2017, 32, 832–840. [Google Scholar] [CrossRef] [Green Version]
- Chauhan, H.P.S.; Bakshi, A.; Bhatiya, S. Synthetic, spectral as well as in vitro antimicrobial studies on some bismuth(III) bis(N,N-dialkyldithiocarbamato)alkylenedithiophosphates. Appl. Organomet. Chem. 2010, 24, 317–325. [Google Scholar] [CrossRef]
- Ferreira, I.P.; de Lima, G.M.; Paniago, E.B.; Takahashi, J.A.; Pinheiro, C.B. Synthesis, characterization and antifungal activity of new dithiocarbamate-based complexes of Ni(II), Pd(II) and Pt(II). Inorg. Chim. Acta 2014, 423, 443–449. [Google Scholar] [CrossRef]
- Ariza-Roldán, A.O.; López-Cardoso, E.M.; Rosas-Valdez, M.E.; Roman-Bravo, P.P.; Vargas-Pineda, D.G.; Cea-Olivares, R.; Acevedo-Quiroz, M.; Razo-Hernández, R.S.; Alvarez-Fitz, P.; Jancik, V. Synthesis, characterization, antimicrobial and theoretical studies of the first main group tris(ephedrinedithiocarbamate) complexes of As(III), Sb(III), Bi(III), Ga(III) and In(III). Polyhedron 2017, 134, 221–229. [Google Scholar] [CrossRef]
- Chen, B.J.; Jamaludin, N.S.; Khoo, C.H.; See, T.H.; Sim, J.H.; Cheah, Y.K.; Halim, S.N.A.; Seng, H.L.; Tiekink, E.R.T. In vitro antibacterial and time kill evaluation of mononuclear phosphanegold(I) dithiocarbamates. J. Inorg. Biochem. 2016, 163, 68–80. [Google Scholar] [CrossRef] [Green Version]
- Onwudiwe, D.C.; Ekennia, A.C. Synthesis, characterization, thermal, antimicrobial and antioxidant studies of some transition metal dithiocarbamates. Res. Chem. Intermed. 2017, 43, 1465–1485. [Google Scholar] [CrossRef]
- Khan, S.A.; Ahmad, W.; Munawar, K.S.; Kanwal, S. Synthesis, spectroscopic characterization and biological evaluation of Ni(II), Cu(II) and Zn(II) complexes of diphenyldithiocarbamate. Indian J. Pharm. Sci. 2018, 80, 480–488. [Google Scholar] [CrossRef]
- Hussien, A.K.; Yousif, E.I.; Hasan, H.A.; Ahmed, R.M. Metal complexes derived from mixed azo-linked schiff-base ligand with dithiocarbamate derivative: Formation, spectral characterization and biological study. Orient. J. Chem. 2018, 34, 1492–1503. [Google Scholar] [CrossRef]
- Shahzadi, S.; Ali, S.; Fettouhi, M. Synthesis, spectroscopy, in vitro biological activity and X-ray structure of (4-methylpiperidine-dithiocarbamato-S,S’) triphenyltin(IV). J. Chem. Crystallogr. 2008, 38, 273–278. [Google Scholar] [CrossRef]
- Zia-ur-Rehman; Muhammad, N.; Shuja, S.; Ali, S.; Butler, I.S.; Meetsma, A.; Khan, M. New dimeric, trimeric and supramolecular organotin(IV) dithiocarboxylates: Synthesis, structural characterization and biocidal activities. Polyhedron 2009, 28, 3439–3448. [Google Scholar] [CrossRef]
- Jangir, S.; Bala, V.; Lal, N.; Kumar, L.; Sarswat, A.; Kumar, L.; Kushwaha, B.; Singh, P.; Shukla, P.K.; Maikhuri, J.P.; et al. A unique dithiocarbamate chemistry during design & synthesis of novel sperm-immobilizing agents. Org. Biomol. Chem. 2014, 12, 3090–3099. [Google Scholar] [CrossRef]
- Mukherjee, T.; Sen, B.; Patra, A.; Banerjee, S.; Hundal, G.; Chattopadhyay, P. Cyclometalated rhodium(III) complexes bearing dithiocarbamate derivative: Synthesis, characterization, interaction with DNA and biological study. Polyhedron 2014, 69, 127–134. [Google Scholar] [CrossRef]
- Zia-ur-Rehman; Shahzadi, S.; Ali, S.; Jin, G.X. Preparation, spectroscopy, antimicrobial assay, and X-ray structure of dimethyl bis-(4-methylpiperidine dithiocarbamato-S,S’)-tin(IV). Turk. J. Chem. 2007, 31, 435–442. [Google Scholar]
- Kalia, S.B.; Kaushal, G.; Kumar, M.; Cameotra, S.S.; Sharma, A.; Verma, M.L.; Kanwar, S.S. Antimicrobial and toxicological studies of some metal complexes of 4-methylpiperazine-1-carbodithioate and phenanthroline mixed ligands. Braz. J. Microbiol. 2009, 40, 916–922. [Google Scholar] [CrossRef] [PubMed]
- Yilmaz, V.T.; Yazıcılar, T.K.; Cesur, H.; Ozkanca, R.; Maras, F.Z. Metal complexes of phenylpiperazine-based dithiocarbamate ligands. Synthesis, characterization, spectroscopic, thermal, and antimicrobial activity studies. Synth. React. Inorg. Met. Org. Chem. 2003, 33, 589–605. [Google Scholar] [CrossRef]
- Manoussakis, G.; Bolosi, C.; Ecateriniadouz, L.; Sarris, C. Synthesis, characterization and anti-bacterial studies of mixed-ligand complexes of dithiocarbamato-thiocyanato and iron(III), nickel(II), copper(II) and zinc(II). Eur. J. Med. Chem. 1987, 22, 421–425. [Google Scholar] [CrossRef]
- Gölcü, A. Transition metal complexes of propranolol dithiocarbamate: Synthesis, characterization, analytical properties and biological activity. Transit. Met. Chem. 2006, 31, 405–412. [Google Scholar] [CrossRef]
- Gölcü, A.; Yavuz, P. Spectral, analytical, thermal, and antimicrobial studies of novel sodium 2-[4(2-hydroxy-3-izopropylaminopropoxy)phenyl]acetamide (atenolol) dithiocarbamate and its divalent transition metal complexes. Russ. J. Coord. Chem. 2008, 34, 106–114. [Google Scholar] [CrossRef]
- Ejelonu, B.C. Synthesis, characterization and in-vitro antimicrobial studies of M2+ complexes of p-chlorophenyl-, p-bromophenyl-dithiocarbamates. Open J. Appl. Sci. 2019, 9, 587–594. [Google Scholar] [CrossRef] [Green Version]
- Ekennia, A.C.; Onwudiwe, D.C.; Osowole, A.A. Spectral, thermal stability and antibacterial studies of copper, nickel and cobalt complexes of N-methyl-N-phenyl dithiocarbamate. J. Sulfur Chem. 2015, 36, 96–104. [Google Scholar] [CrossRef]
- Ekennia, A.C.; Onwudiwe, D.C.; Osowole, A.A.; Olasunkanmi, L.O.; Ebenso, E.E. Synthesis, biological, and quantum chemical studies of Zn(II) and Ni(II) mixed-ligand complexes derived from N,N-disubstituted dithiocarbamate and benzoic acid. J. Chem. 2016, 2016, 5129010. [Google Scholar] [CrossRef]
- Botha, N.L.; Ajibade, P.A.; Ashafa, A.O.T. Synthesis, spectroscopic characterization, antifungal and antibacterial studies of copper(II) dithiocarbamate complexes. J. Pharm. Sci. Res. 2018, 10, 2111–2114. [Google Scholar]
- de Lima, G.M.; Menezes, D.C.; Cavalcanti, C.A.; dos Santos, J.A.F.; Ferreira, I.P.; Paniago, E.B.; Wardell, J.L.; Wardell, S.M.S.V.; Krambrock, K.; Mendes, I.C.; et al. Synthesis, characterisation and biological aspects of copper(II) dithiocarbamate complexes, [Cu{S2CNR(CH2CH2OH)}2], (R = Me, Et, Pr and CH2CH2OH). J. Mol. Struct. 2011, 988, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Ferreira, I.P.; de Lima, G.M.; Paniago, E.B.; Takahashi, J.A.; Krambrock, K.; Pinheiro, C.B.; Wardell, J.L.; Visentin, L.C. Synthesis, characterization, structural and biological aspects of copper(II) dithiocarbamate complexes—Part II, [Cu{S2CN(Me)(R1)}2], [Cu{S2CN(Me)(R2)}2] and [Cu{S2CN(R3)(R4)}2] {R1 = –CH2CH(OMe)2, R2 = 2-methyl-1,3-dioxolane, R3 = –CH2(CH2)2N=CHPhOCH2Ph and R4 = –CH2CH2OH}. J. Mol. Struct. 2013, 1048, 357–366. [Google Scholar] [CrossRef]
- Balakrishnan, S.; Duraisamy, S.; Kasi, M.; Kandasamy, S.; Sarkar, R.; Kumarasamy, A. Syntheses, physicochemical characterization, antibacterial studies on potassium morpholine dithiocarbamate nickel(II), copper(II) metal complexes and their ligands. Heliyon 2019, 5, e01687. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Verma, S.K.; Singh, V.K. Synthesis, electrochemical, fluorescence and antimicrobial studies of 2-chloro-3-amino-1,4-naphthoquinone bearing mononuclear transition metal dithiocarbamate complexes [M{k2S,S-S2C–piperazine–C2H4N(H)ClNQ}n]. RSC Adv. 2015, 5, 53036–53046. [Google Scholar] [CrossRef]
- Maurya, V.K.; Singh, A.K.; Singh, R.P.; Yadav, S.; Kumar, K.; Prakash, P.; Prasad, L.B. Synthesis and evaluation of Zn(II) dithiocarbamate complexes as potential antibacterial, antibiofilm, and antitumor agents. J. Coord. Chem. 2019, 72, 3338–3358. [Google Scholar] [CrossRef]
- Sathiyaraj, E.; Tamilvanan, S.; Thirumaran, S.; Ciattini, S. Effect of functionalization of N-bound organic moiety in zinc(II) dithiocarbamate complexes on structure, biological properties and morphology of zinc sulfide nanoparticles. Polyhedron 2017, 128, 133–144. [Google Scholar] [CrossRef]
- Patra, M.; Gasser, G. The medicinal chemistry of ferrocene and its derivatives. Nat. Rev. Chem. 2017, 1, 0066. [Google Scholar] [CrossRef]
- Ludwig, B.S.; Correia, J.D.G.; Kühn, F.E. Ferrocene derivatives as anti-infective agents. Coord. Chem. Rev. 2019, 396, 22–48. [Google Scholar] [CrossRef]
- Verma, S.K.; Singh, V.K. Synthesis and characterization of ferrocene functionalized transition metal dithiocarbamate complexes: Investigations of antimicrobial, electrochemical properties and a new polymorphic form of [Cu{k2S,S-S2CN(CH2C4H3O)CH2Fc}2]. J. Organomet. Chem. 2015, 791, 214–224. [Google Scholar] [CrossRef]
- Manav, N.; Mishra, A.K.; Kaushik, N.K. In vitro antitumour and antibacterial studies of some Pt(IV) dithiocarbamate complexes. Spectrochim. Acta A Mol. Biomol. Spectrosc. 2006, 65, 32–35. [Google Scholar] [CrossRef]
- Shaheen, F.; Badshah, A.; Gielen, M.; Dusek, M.; Fejfarova, K.; de Vos, D.; Mirza, B. Synthesis, characterization, antibacterial and cytotoxic activity of new palladium(II) complexes with dithiocarbamate ligands: X-ray structure of bis(dibenzyl-1-S:S’-dithiocarbamato)Pd(II). J. Organomet. Chem. 2007, 692, 3019–3026. [Google Scholar] [CrossRef]
- Oladipo, S.D.; Omondi, B.; Mocktar, C. Synthesis and structural studies of nickel(II)- and copper(II)-N,N’-diarylformamidine dithiocarbamate complexes as antimicrobial and antioxidant agents. Polyhedron 2019, 170, 712–722. [Google Scholar] [CrossRef]
- Onwudiwe, D.C.; Ekennia, A.C.; Hosten, E. Syntheses, characterization, and antimicrobial properties of nickel(II) dithiocarbamate complexes containing NiS4 and NiS2PN moieties. J. Coord. Chem. 2016, 69, 2454–2468. [Google Scholar] [CrossRef]
- Awang, N.; Baba, I.; Yamin, B.M.; Halim, A.A. Preparation, characterization and antimicrobial assay of 1,10-phenanthroline and 2,2′-bipyridyl adducts of cadmium(II) N-sec-butyl-N-propyldithiocarbamate: Crystal structure of Cd[S2CN(i-C4H9)(C3H7)]2(2,2′-bipyridyl). World Appl. Sci. J. 2011, 12, 1568–1574. [Google Scholar]
- Onwudiwe, D.C.; Nthwane, Y.B.; Ekennia, A.C.; Hosten, E. Synthesis, characterization and antimicrobial properties of some mixed ligand complexes of Zn(II) dithiocarbamate with different N-donor ligands. Inorg. Chim. Acta 2016, 447, 134–141. [Google Scholar] [CrossRef]
- Rani, P.J.; Thirumaran, S. Synthesis, characterization, cytotoxicity and antimicrobial studies on bis(N-furfuryl-N-(2-phenylethyl)dithiocarbamato-S,S’)zinc(II) and its nitrogen donor adducts. Eur. J. Med. Chem. 2013, 62, 139–147. [Google Scholar] [CrossRef] [PubMed]
- Bharty, M.K.; Dani, R.K.; Nath, P.; Bharti, A.; Singh, N.K.; Prakash, O.; Singh, R.K.; Butcher, R.J. Syntheses, structural and thermal studies on Zn(II) complexes of 5-aryl-1,3,4-oxadiazole-2-thione and dithiocarbamates: Antibacterial activity and DFT calculations. Polyhedron 2015, 98, 84–95. [Google Scholar] [CrossRef]
- Nabipour, H. Synthesis of a new dithiocarbamate cobalt complex and its nanoparticles with the study of their biological properties. Int. J. Nano Dimens. 2011, 1, 225–232. [Google Scholar] [CrossRef] [Green Version]
- Al-Janabi, A.S.M.; Kadhim, M.M.; Al-Nassiry, A.I.A.; Yousef, T.A. Antimicrobial, computational, and molecular docking studies of Zn (II) and Pd (II) complexes derived from piperidine dithiocarbamate. Appl. Organomet. Chem. 2021, 35, e6108. [Google Scholar] [CrossRef]
- El-Said, A.I.; Zidan, A.S.A.; El-Meligy, M.S.; Aly, A.A.M.; Mohammed, O.F. Complexes of tris(o-phenanthroline)nickel(II) and copper(II) bromide with dithiocarbamates derived from α-amino acids. Transit. Met. Chem. 2001, 26, 13–19. [Google Scholar] [CrossRef]
- Rani, P.J.; Thirumaran, S.; Ciattini, S. Synthesis and characterization of Ni(II) and Zn(II) complexes of (furan-2- yl)methyl(2-(thiophen-2-yl)ethyl)dithiocarbamate (ftpedtc): X-ray structures of [Zn(ftpedtc)2(py)] and [Zn(ftpedtc)Cl(1,10-phen)]. Spectrochim. Acta A Mol. Biomol. Spectrosc. 2015, 137, 1164–1173. [Google Scholar] [CrossRef]
- Khan, H.; Badshah, A.; Murtaz, G.; Said, M.; Zia-ur-Rehman; Neuhausen, C.; Todorova, M.; Jean-Claude, B.J.; Butler, I.S. Synthesis, characterization and anticancer studies of mixed ligand dithiocarbamate palladium(II) complexes. Eur. J. Med. Chem. 2011, 46, 4071–4077. [Google Scholar] [CrossRef] [PubMed]
- Khan, H.; Badshah, A.; Said, M.; Murtaza, G.; Sirajuddin, M.; Ahmad, J.; Butler, I.S. Synthesis, structural characterization and biological screening of heteroleptic palladium(II) complexes. Inorg. Chim. Acta 2016, 447, 176–182. [Google Scholar] [CrossRef]
- Odola, A.J.; Woods, J.A.O. Synthesis, characterization and antimicrobial activity studies of new nickel(II) mixed ligand complexes of disubstituted dithiocarbamates with ethylsalicylaldiminate. Arch. Appl. Sci. Res. 2011, 3, 463–470. [Google Scholar]
- Odola, A.J.; Woods, J.A.O. New nickel(II) mixed ligand complexes of dithiocarbamates with Schiff base. J. Chem. Pharm. Res. 2011, 3, 865–871. [Google Scholar]
- Asuquo, I.G.; Ekanem, A.N.; Ikpe, E.E. Synthesis, characterization and antibacterial studies of nickel (II) mixed ligand complexes of dithiocarbamate ligands with Schiff base. Elixir Appl. Chem. 2014, 76, 28493–28501. [Google Scholar]
- Sovilj, S.P.; Avramović, N.; Katsaros, N. Syntheses and properties of mixed dinuclear copper(II) complexes with heterocyclic dithiocarbamates and a cyclic octadentate tertiary amine. Transit. Met. Chem. 2004, 29, 737–742. [Google Scholar] [CrossRef]
- Sovilj, S.P.; Mitić, D.; Drakulić, B.J.; Milenković, M. Spectroscopic properties and antimicrobial activity of dioxomolybdenum(VI) complexes with heterocyclic S,S’-ligands. J. Serbian Chem. Soc. 2012, 77, 53–66. [Google Scholar] [CrossRef]
- Mukherjee, T.; Mukherjee, M.; Sen, B.; Banerjee, S.; Hundal, G.; Chattopadhyay, P. Synthesis, characterization, interactions with DNA and bovine serum albumin (BSA), and antibacterial activity of cyclometalated iridium(III) complexes containing dithiocarbamate derivatives. J. Coord. Chem. 2014, 67, 2643–2660. [Google Scholar] [CrossRef]
- Ajibade, P.A.; Idemudia, O.G.; Okoh, A.I. Synthesis, characterization and antibacterial studies of metal complexes of sulfadiazine with N-alkyl-N-phenyldithiocarbamate. Bull Chem. Soc. Ethiop. 2013, 27, 77–84. [Google Scholar] [CrossRef]
- Ekennia, A.C.; Onwudiwe, D.C.; Olasunkanmi, L.O.; Osowole, A.A.; Ebenso, E.E. Synthesis, DFT calculation, and antimicrobial studies of novel Zn(II), Co(II), Cu(II), and Mn(II) heteroleptic complexes containing benzoylacetone and dithiocarbamate. Bioinorg. Chem. Appl. 2015, 2015, 789063. [Google Scholar] [CrossRef] [Green Version]
- Kim, Y.T.; Yum, S.; Heo, J.S.; Kim, W.; Jung, Y.; Kim, Y.M. Dithiocarbamate chitosan as a potential polymeric matrix for controlled drug release. Drug Dev. Ind. Pharm. 2014, 40, 192–200. [Google Scholar] [CrossRef]
- Kean, W.F.; Kean, I.R.L. Clinical pharmacology of gold. Inflammopharmacology 2008, 3, 112–125. [Google Scholar] [CrossRef]
- Glišić, B.Đ.; Djuran, M.I. Gold complexes as antimicrobial agents: An overview of different biological activities in relation to the oxidation state of the gold ion and the ligand structure. Dalton Trans. 2014, 43, 5950–5969. [Google Scholar] [CrossRef] [PubMed]
- Tan, Y.J.; Tan, Y.S.; Yeo, C.I.; Chew, J.; Tiekink, E.R.T. In vitro anti-bacterial and time kill evaluation of binuclear tricyclohexylphosphanesilver(I) dithiocarbamates, {Cy3PAg(S2CNRR′)}2. J. Inorg. Biochem. 2019, 192, 107–118. [Google Scholar] [CrossRef] [PubMed]
- Desai, R.M.; Shah, M.K.; Shah, V.H. Preparation and antimicrobial screening of Cu (II), Ni (II), Zn (II) Cd (II) complexes. E J. Chem. 2006, 3, 137–141. [Google Scholar] [CrossRef] [Green Version]
- Hasan, H.A.; Yousif, E.I.; Al-Jeboori, M.J. Metal-assisted assembly of dinuclear metal(II) dithiocarbamate Schiff-base macrocyclic complexes: Synthesis and biological studies. Glob. J. Inorg. Chem. 2012, 3, 10. [Google Scholar]
- Siddiqi, K.S.; Khan, S.; Nami, S.A.A.; El-ajaily, M.M. Polynuclear transition metal complexes with thiocarbohydrazide and dithiocarbamates. Spectrochim. Acta A Mol. Biomol. Spectrosc. 2007, 67, 995–1002. [Google Scholar] [CrossRef] [PubMed]
- Menezes, D.C.; de Lima, G.M.; de Oliveira, G.S.; Boas, A.V.; Nascimento, A.M.A.; Vieira, F.T. In vitro antibacterial activity of dithiocarbamate organotin(IV) complexes towards Staphylococcus aureus. Main Group Met. Chem. 2008, 31, 21–27. [Google Scholar] [CrossRef] [Green Version]
- Awang, N.; Baba, I.; Yamin, B.M.; Othman, M.S.; Kamaludin, N.F. Synthesis, characterization and biological activities of organotin (IV) methylcyclohexyldithiocarbamate compounds. Am. J. Appl. Sci. 2011, 8, 310–317. [Google Scholar] [CrossRef] [Green Version]
- Awang, N.; Mokhtar, N.; Zin, N.M.; Kamaludin, N.F. Antibacterial activity of organotin(IV) methyl and ethyl cylohexyldithiocarbamate compounds. J. Chem. Pharm. Res. 2015, 7, 379–383. [Google Scholar]
- Awang, N.; Mohktar, S.M.; Zin, N.M.; Kamaludin, N.F. Evaluation of antimicrobial activities of organotin(IV) alkylphenyl dithiocarbamate compounds. Asian J. Appl. Sci. 2015, 8, 165–172. [Google Scholar] [CrossRef] [Green Version]
- Adeyemi, J.O.; Onwudiwe, D.C.; Ekennia, A.C.; Uwaoma, R.C.; Hosten, E.C. Synthesis, characterization and antimicrobial studies of organotin(IV) complexes of N-methyl-N-phenyldithiocarbamate. Inorg. Chim. Acta 2018, 477, 148–159. [Google Scholar] [CrossRef]
- Adeyemi, J.O.; Onwudiwe, D.C.; Ekennia, A.C.; Okafor, S.N.; Hosten, E.C. Organotin(IV) N-butyl-N-phenyldithiocarbamate complexes: Synthesis, characterization, biological evaluation and molecular docking studies. J. Mol. Struct. 2019, 1192, 15–26. [Google Scholar] [CrossRef]
- Adeyemi, J.O.; Onwudiwe, D.C.; Ekennia, A.C.; Anokwuru, C.P.; Nundkumar, N.; Singh, M.; Hosten, E.C. Synthesis, characterization and biological activities of organotin(IV) diallyldithiocarbamate complexes. Inorg. Chim. Acta 2019, 485, 64–72. [Google Scholar] [CrossRef]
- Shahzadi, S.; Ahmad, S.U.; Ali, S.; Yaqub, S.; Ahmed, F. Chloro-diorganotin(IV) complexes of pipyridyl dithiocarbamate: Syntheses and determination of kinetic parameters, spectral characteristics and biocidal properties. J. Iran. Chem. Soc. 2006, 3, 38–45. [Google Scholar] [CrossRef]
- Shaheen, F.; Zia-ur-Rehman; Ali, S.; Meetsma, A. Structural properties and antibacterial potency of new supramolecular organotin(IV) dithiocarboxylates. Polyhedron 2012, 31, 697–703. [Google Scholar] [CrossRef]
- Basirah, A.; Hasan, M.F.A.; Sidek, N.M.; Khairul, W.M.; Ismail, N. Synthesis, characterization and antimicrobial activity of organotin(IV) complexes featuring bis-2-methoxyethyl dithiocarbamate as ligand. J. Appl. Sci. Res. 2013, 9, 5562–5567. [Google Scholar]
- Parveen, B.; Bukhari, I.H.; Shahzadi, S.; Ali, S.; Hussain, S.; Ali, K.G.; Shahid, M. Synthesis and spectroscopic characterization of mononuclear/binuclear organotin(IV) complexes with 1H-1,2,4-triazole-3-thiol: Comparative studies of their antibacterial/antifungal potencies. J. Serb. Chem. Soc. 2015, 80, 755–766. [Google Scholar] [CrossRef]
- Mahato, M.; Mukherji, S.; Hecke, K.V.; Harms, K.; Ghosh, A.; Nayek, H.P. Mononuclear homoleptic organotin(IV) dithiocarbamates: Syntheses, structures and antimicrobial activities. J. Organomet. Chem. 2017, 853, 27–34. [Google Scholar] [CrossRef]
- Adeyemi, J.O.; Onwudiwe, D.C. Chemistry and some biological potential of bismuth and antimony dithiocarbamate complexes. Molecules 2020, 25, 305. [Google Scholar] [CrossRef] [Green Version]
- Chauhan, H.P.S.; Singh, U.P.; Shaik, Ν.M. Synthetic and spectral characterization as well as in vitro antimicrobial activity of bis(N,N’-dialkyldithiocarbamato) arsenic(III) alkylenedithiophosphates. Main Group Met. Chem. 2006, 29, 221–231. [Google Scholar] [CrossRef]
- Chauhan, H.P.S.; Carpenter, J.; Joshi, S. Mixed bis(morpholine-4-dithiocarbamato-S,S′) antimony(III) complexes: Synthesis, characterization and biological studies. Appl. Organomet. Chem. 2014, 28, 605–613. [Google Scholar] [CrossRef]
- Chauhan, H.P.S.; Carpenter, J.; Joshi, S. Synthetic aspects, spectral, thermal studies and antimicrobial screening on bis(N,N-dimethyldithiocarbamato-S,S’)antimony(III) complexes with oxo or thio donor ligands. Spectrochim. Acta Part A Molec. Biomol. Spectros. 2014, 130, 230–237. [Google Scholar] [CrossRef] [PubMed]
- Chauhan, H.P.S.; Singh, U.P. Synthetic, spectral, thermal and antimicrobial studies of bis(N,N-dialkyldithiocarbamato)arsenic(III) and antimony(III) complexes with diphenyldithiophosphate and diphenyldithiophosphinate. Appl. Organomet. Chem. 2006, 20, 404–410. [Google Scholar] [CrossRef]
- Tamilvanan, S.; Gurumoorthy, G.; Thirumaran, S.; Ciattini, S. Synthesis, characterization, cytotoxicity and antimicrobial studies on Bi(III) dithiocarbamate complexes containing furfuryl group and their use for the preparation of Bi2O3 nanoparticles. Polyhedron 2017, 121, 70–79. [Google Scholar] [CrossRef]
- Sharma, D.K.; Singh, Y.; Sharma, J. Monophenylantimony(III) derivatives of cyclic dithiocarbamates; Synthesis, spectroscopic characterization, and antimicrobial study. Phosphorus Sulfur Silicon Relat. Elem. 2013, 188, 1194–1204. [Google Scholar] [CrossRef]
- Beniwal, S.; Chhimpa, S.; Gaur, D.; John, P.J.; Singh, Y.; Sharma, J. Syntheses, characterization, antibacterial activity and molecular modelling of phenylantimony(III) heteroleptic derivatives containing substituted oximes and piperidine dithiocarbamate. Appl. Organomet. Chem. 2017, 31, e3725. [Google Scholar] [CrossRef]
- Beniwal, S.; Kumar, A.; Chhimpa, S.; Rai, J.; John, P.J.; Singh, Y.; Sharma, J. Synthesis and characterization of antimony (III) heteroleptic derivatives having oxygen, nitrogen and sulfur containing organic moieties with their antibacterial and antioxidant activities. Phosphorus Sulfur Silicon Relat. Elem. 2019, 194, 879–886. [Google Scholar] [CrossRef]
- Beniwal, S.; Kumar, A.; Chhimpa, S.; John, P.J.; Singh, Y.; Sharma, J. Syntheses, characterization, powder X-ray diffraction analysis and antibacterial and antioxidant activities of triphenylantimony(V) heteroleptic derivatives containing substituted oximes and morpholine dithiocarbamate. Appl. Organomet. Chem. 2019, 33, e4712. [Google Scholar] [CrossRef]
- Nocentini, A.; Supuran, C.T. Carbonic anhydrases: An overview. In Carbonic Anhydrases; Supuran, C.T., Nocentini, A., Eds.; Elsevier: Amsterdam, The Netherlands, 2019; Chapter 1; pp. 3–16. [Google Scholar] [CrossRef]
- Supuran, C.T. Carbonic anhydrase inhibitors and activators for novel therapeutic applications. Future Med. Chem. 2011, 3, 1165–1180. [Google Scholar] [CrossRef]
- Supuran, C.T. Advances in structure-based drug discovery of carbonic anhydrase inhibitors. Expert Opin. Drug Discov. 2017, 12, 61–88. [Google Scholar] [CrossRef]
- Capasso, C.; Supuran, C.T. Bacterial, fungal and protozoan carbonic anhydrases as drug targets. Expert Opin. Ther. Targets 2015, 19, 1689–1704. [Google Scholar] [CrossRef]
- Carta, F.; Aggarwal, M.; Maresca, A.; Scozzafava, A.; McKenna, R.; Supuran, C.T. Dithiocarbamates: A new class of carbonic anhydrase inhibitors. Crystallographic and kinetic investigations. Chem. Commun. 2012, 48, 1868–1870. [Google Scholar] [CrossRef] [Green Version]
- Supuran, C.T.; Capasso, C. An overview of the bacterial carbonic anhydrases. Metabolites 2017, 7, 56. [Google Scholar] [CrossRef] [Green Version]
- Swanson, M.; Hammer, B. Legionella pneumophila pathogenesis: A fateful journey from amoebae to macrophages. Annu. Rev. Microbiol. 2000, 54, 567–613. [Google Scholar] [CrossRef]
- Supuran, C.T. Legionella pneumophila carbonic anhydrases: Underexplored antibacterial drug targets. Pathogens 2016, 5, 44. [Google Scholar] [CrossRef] [Green Version]
- Nishimori, I.; Vullo, D.; Minakuchi, T.; Scozzafava, A.; Osman, S.M.; AlOthman, Z.; Capasso, C.; Supuran, C.T. Anion inhibition studies of two new β-carbonic anhydrases from the bacterial pathogen Legionella pneumophila. Bioorg. Med. Chem. Lett. 2014, 24, 1127–1132. [Google Scholar] [CrossRef]
- Byrne, S.T.; Gu, P.; Zhou, J.; Denkin, S.M.; Chong, C.; Sullivan, D.; Liu, J.O.; Zhang, Y. Pyrrolidine dithiocarbamate and diethyldithiocarbamate are active against growing and nongrowing persister Mycobacterium tuberculosis. Antimicrob. Agents Chemother. 2007, 51, 4495–4497. [Google Scholar] [CrossRef] [Green Version]
- Maresca, A.; Carta, F.; Vullo, D.; Supuran, C.T. Dithiocarbamates strongly inhibit the β-class carbonic anhydrases from Mycobacterium tuberculosis. J. Enzyme Inhib. Med. Chem. 2013, 28, 407–411. [Google Scholar] [CrossRef] [PubMed]
- Aspatwar, A.; Hammaren, M.; Parikka, M.; Parkkila, S.; Carta, F.; Bozdag, M.; Vullo, D.; Supuran, C.T. In vitro inhibition of Mycobacterium tuberculosis β-carbonic anhydrase 3 with Mono-and dithiocarbamates and evaluation of their toxicity using zebrafish developing embryos. J. Enzyme Inhib. Med. Chem. 2020, 35, 65–71. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McBryde, E.S.; Meehan, M.T.; Doan, T.N.; Ragonnet, R.; Marais, B.J.; Guernier, V.; Trauer, J.M. The risk of global epidemic replacement with drug-resistant Mycobacterium tuberculosis strains. Int. J. Infect. Dis. 2017, 56, 14–20. [Google Scholar] [CrossRef] [Green Version]
- Monti, S.M.; Maresca, A.; Viparelli, F.; Carta, F.; De Simone, G.; Mühlschlegel, F.A.; Scozzafava, A.; Supuran, C.T. Dithiocarbamates are strong inhibitors of the beta-class fungal carbonic anhydrases from Cryptococcus neoformans, Candida albicans and Candida glabrata. Bioorg. Med. Chem. Lett. 2012, 22, 859–862. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bozdag, M.; Carta, F.; Vullo, D.; Isik, S.; AlOthman, Z.; Osman, S.M.; Scozzafava, A.; Supuran, C.T. Dithiocarbamates with potent inhibitory activity against the Saccharomyces cerevisiae β-carbonic anhydrase. J. Enzyme Inhib. Med. Chem. 2016, 31, 132–136. [Google Scholar] [CrossRef]
- Pal, D.S.; Mondal, D.K.; Datta, R. Identification of metal dithiocarbamates as a novel class of antileishmanial agents. Antimicrob. Agents Chemother. 2015, 59, 2144–2152. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alvar, J.; Vélez, I.D.; Bern, C.; Herrero, M.; Desjeux, P.; Cano, J.; Jannin, J.; den Boer, M.; The WHO (World Health Organization) Leishmaniasis Control Team. Leishmaniasis worldwide and global estimates of its incidence. PLoS ONE 2012, 7, e35671. [Google Scholar] [CrossRef] [PubMed]
- Tooke, C.L.; Hinchliffe, P.; Bragginton, E.C.; Colenso, C.K.; Hirvonen, V.H.; Takebayashi, Y.; Spencer, J. β-Lactamases and β-lactamase inhibitors in the 21st century. J. Mol. Biol. 2019, 431, 3472–3500. [Google Scholar] [CrossRef] [PubMed]
- Bush, K. Past and present perspectives on β-lactamases. Antimicrob. Agents Chemother. 2018, 62, 1–20. [Google Scholar] [CrossRef] [Green Version]
- Boyd, S.E.; Livermore, D.M.; Hooper, D.C.; Hope, W.W. Metallo-β-lactamases: Structure, function, epidemiology, treatment options, and the development pipeline. Antimicrob. Agents Chemother. 2020, 64, 1–20. [Google Scholar] [CrossRef]
- Codjoe, F.S.; Donko, E.S. Carbapenem resistance: A review. Med. Sci. 2018, 6, 1. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Boucher, H.W.; Talbot, G.H.; Bradley, J.S.; Edwards, J.E.; Gilbert, D.; Rice, L.B.; Scheld, M.; Spellberg, B.; Bartlett, J. Bad bugs, no drugs: No ESKAPE! An update from the Infectious Diseases Society of America. Clin. Infect. Dis. 2009, 48, 1–12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Palzkill, T. Metallo-β-lactamase structure and function. Ann. N. Y. Acad. Sci. 2013, 1277, 91–104. [Google Scholar] [CrossRef]
- Klingler, F.-M.; Wichelhaus, T.A.; Frank, D.; Cuesta-Bernal, J.; El-Delik, J.; Müller, H.F.; Sjuts, H.; Göttig, S.A.; Koenigs, A.; Pos, K.M.; et al. Approved drugs containing thiols as inhibitors of metallo-β-lactamases: Strategy to combat multidrug-resistant bacteria. J. Med. Chem. 2015, 58, 3626–3630. [Google Scholar] [CrossRef] [PubMed]
- Somboro, A.M.; Tiwari, D.; Bester, L.A.; Parboosing, R.; Chonco, L.; Kruger, H.G.; Arvidsson, P.I.; Govender, T.; Naicker, T.; Essack, S.Y. NOTA: A potent metallo-β-lactamase inhibitor. J. Antimicrob. Chemother. 2015, 70, 1594–1596. [Google Scholar] [CrossRef] [Green Version]
- Zhang, E.; Wang, M.M.; Huang, S.C.; Xu, S.M.; Cui, D.Y.; Bo, Y.L.; Bai, P.Y.; Hua, Y.G.; Xiao, C.L.; Qin, S. NOTA analogue: A first dithiocarbamate inhibitor of metallo-β-lactamases. Bioorg. Med. Chem. Lett. 2018, 28, 214–221. [Google Scholar] [CrossRef]
- Wang, M.-M.; Chu, W.-C.; Yang, Y.; Yang, Q.-Q.; Qin, S.-S.; Zhang, E. Dithiocarbamates: Efficient metallo-β-lactamase inhibitors with good antibacterial activity when combined with meropenem. Bioorg. Med. Chem. Lett. 2018, 28, 3436–3440. [Google Scholar] [CrossRef]
- Chen, C.; Yang, K.-W.; Wu, L.-Y.; Li, J.-Q.; Sun, L.-Y. Disulfiram as a potent metallo-β-lactamase inhibitor with dual functional mechanisms. Chem. Commun. 2020, 56, 2755–2758. [Google Scholar] [CrossRef]
- Ge, Y.; Xu, L.-W.; Liu, Y.; Sun, L.-Y.; Gao, H.; Li, J.-Q.; Yang, K. Dithiocarbamate as a valuable scaffold for the inhibition of metallo-β-lactmases. Biomolecules 2019, 9, 699. [Google Scholar] [CrossRef] [Green Version]
- Laws, M.; Shaaban, A.; Rahman, K.M. Antibiotic resistance breakers: Current approaches and future directions. FEMS Microb. Rev. 2019, 43, 490–516. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Carter, O.W.L.; Xu, Y.; Sadler, P.J. Minerals in biology and medicine. RSC Adv. 2021, 11, 1939–1951. [Google Scholar] [CrossRef]
- Prasad, P.; Ajay Gupta, A.; Sasmal, P.K. Aggregation-induced emission active metal complexes: A promising strategy to tackle bacterial infections. Chem. Commun. 2021, 57, 174–186. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.M.; Tiekink, E.R.T. A structural survey of poly-functional dithiocarbamate ligands and the aggregation patterns they sustain. Inorganics 2021, 9, 7. [Google Scholar] [CrossRef]


| Formulation/R(R’)NCS2(−) | Method | Activity | Ref. |
|---|---|---|---|
| R = H; R’ = Me | Broth dilution | MIC = 20 μg/mL against B. cereus; limited antibacterial effects on probiotic bacteria L. plantarum and L. mesenteroides | [30] |
| R = H; R’ = Ph | Disc diffusion | Active against 12 bacterial species and 10 fungi (zone of inhibition ranging 6–8 mm at MIC 1 × 104 and 1.25 × 104 μg/mL, respectively) | [31,32] |
| R = H; R’ = Cy | Disc diffusion | Showed improved percentage of minimum inhibitory zone towards A. flavus, A. carbonarius, A. niger, S. Typhi, B. subtilis, B. cereus, P. aeruginosa, and P. mirabilis at increased concentration; showed no significant concentration effect on A. fumigatus | [32,33] |
| R = H; R’ = CH2CH2N(CH2)5 | Broth dilution/zebrafish model | Growth inhibition on M. marinum at approximate 18 μg/mL. Significantly inhibited bacterial growth in zebrafish larvae at approximate 73 μg/ml | [34] a |
| R = H; R’ = N(CH2CH2)2NMe | Broth dilution | Growth inhibition on M. marinum at approximate 17 μg/ml | [34] a |
| R = R’ = Me | Broth dilution/well diffusion | MIC = 20 μg/mL against B. cereus [28]. Greater activity towards Gram-positive bacteria (S. aureus and B. subtilis) than Gram-negative bacteria (E. coli and P. aeruginosa) compared to chloramphenicol [32] | [30,35] |
| R = Me; R’ = CH2CH(OMe)2 and R = Me; R’ = 2-methyl-1,3-dioxolane | Broth dilution | The species with R’ = CH2CH(OMe)2 presented at least 6-fold greater activities against A. flavus, A. niger, and A. parasiticus | [36] |
| R = Me; R’ = (1R,2S)-1-methyl-2-phenyl-2-hydroxy]ethyl | Broth dilution | Mild activity towards S. aureus, S. sciuri, and drug-resistant bacterial strains: extended spectrum beta-lactamase producing E. coli, methicillin-resistant S. epidermidis, S. haemolyticus, and S. simulans | [37] |
| R = Et; R’ = Et | Well diffusion/disc diffusion | Greater sensitivity towards Gram-positive bacteria than Gram-negative bacterial strains compared to chloramphenicol | [35,38] |
| R = Et; R’ = Ph | Disc diffusion | Tested against 4 bacterial species: E. coli, P. aeruginosa, S. Typhi, and S. aureus; zone of inhibition in the range 4–10 mm at 100 μg/mL; inactive towards S. aureus. Additionally, tested against 2 fungal organisms: A. flavus and F. oxysporium; zone of inhibition in the ranging (range) 9–10 mm at 100 μg/mL | [39] |
| R = Ph; R’ = Ph | Disc diffusion | Active against Gram-positive bacteria: B. subtilis, S. aureus, and Rhodococcus sp. with zone of inhibition in the range 12–22 mm; inactive towards Gram-negative bacteria namely, E. coli, P. aeruginosa, and Enterobacter sp. Active against 4 fungal organisms: A. niger, A. flavus, C. albicans, and Acetomyceta sp.; zone of inhibition in the range 16–18 mm at 100 μg/mL | [40,41] |
| Y(CH2CH2)2NCS2(−) | |||
| Y = CMe | Well diffusion/tube diffusion | Active against 6 bacterial species: E. coli, B. subtilis, S. flexneri, S. aureus, P. aeruginosa, and S. Typhi with zones of inhibition in the range 12–20 mm. Active against 4 fungi: T. longifusus, M. canis, F. solani, and C. glabrata; zone of inhibition in the range 10–38 mm | [42] |
| Y = CCH2Ph | Well diffusion | Mild activity against E. coli, S. Typhi, P. aeruginosa, and S. aureus with zones of inhibition in the range 12–22 mm. Active against 5 fungi: A. nigar, A. flavus, H. solani, A. solani, and Fusarium sp.; range of inhibition: 12.6–43.5 mm at 200 μg/mL | [43] |
| Y = NMe | Broth dilution/well diffusion/agar dilution | Weak sensitivity towards 10 bacterial species (E. coli, P. aeruginosa, S. aureus, E. faecalis, V. cholerae, S. pneumoniae, B. cereus, B. subtilis, S. flexneri, and S. Typhi) and 5 fungi (C. albicans, T. longifusus, M. canis, F. solani, and C. glabrata). | [44,45,46,47] |
| Y = NC(=S)S(CH2)2N(CH2)5 | Broth micro-dilution | Active against 6 species of fungi (C. albicans, C. neoformans, S. schenckii, and T. mentagrophytes, A. fumigates, and C. parapsilosis) | [44] |
| Y = NC(=S)S(CH2)3Me | Broth micro-dilution | Active against 4 species of fungi (C. albicans, C. neoformans, A. fumigates, and C. parapsilosis) and displayed spermicidal activity at minimum effective concentration (MEC) 31.6 mM | [44] |
| Y = CHCH2Ph | Well diffusion | Tested against 4 bacterial species: E. coli, V. cholerae, S. pneumoniae, and B. cereus with zones of inhibition in the range 3–7 mm at 100 μg/mL | [45] |
| Y = NPh | Disc diffusion | Active against S. Tyhimurium, P. aeruginosa, B. pumilus, S. aureus, C. albicans, and A. niger. with zones of inhibition in the range 14–45 mm at 1750 μg/mL | [48] |
| Y = NC6H4NO2-4 | Disc diffusion | Showed activities against B. pumilus, S. aureus, C. albicans, and A. niger with zones of inhibition in the range 25–42 mm at 1000 μg/mL; inactive towards E. coli | [48] |
| Y = NC6H4F-4 | Disc diffusion | Showed activities against E. coli, S. Typhimurium, P. aeruginosa, B. pumilus, S. aureus, C. albicans and A. niger with zones of inhibition in the range 23–42 mm at 2500 μg/mL | [48] |
| Y = O | Well diffusion | Tested against 4 bacterial species: E. coli, V. cholerae, S. pneumoniae, and B. cereus with zones of inhibition in the range 4–8 mm at 100 μg/mL | [45] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yeo, C.I.; Tiekink, E.R.T.; Chew, J. Insights into the Antimicrobial Potential of Dithiocarbamate Anions and Metal-Based Species. Inorganics 2021, 9, 48. https://doi.org/10.3390/inorganics9060048
Yeo CI, Tiekink ERT, Chew J. Insights into the Antimicrobial Potential of Dithiocarbamate Anions and Metal-Based Species. Inorganics. 2021; 9(6):48. https://doi.org/10.3390/inorganics9060048
Chicago/Turabian StyleYeo, Chien Ing, Edward R. T. Tiekink, and Jactty Chew. 2021. "Insights into the Antimicrobial Potential of Dithiocarbamate Anions and Metal-Based Species" Inorganics 9, no. 6: 48. https://doi.org/10.3390/inorganics9060048
APA StyleYeo, C. I., Tiekink, E. R. T., & Chew, J. (2021). Insights into the Antimicrobial Potential of Dithiocarbamate Anions and Metal-Based Species. Inorganics, 9(6), 48. https://doi.org/10.3390/inorganics9060048