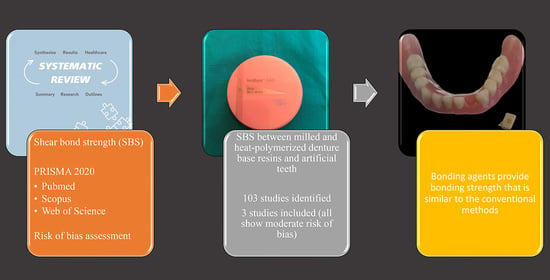
The Shear Bond Strength between Milled Denture Base Materials and Artificial Teeth: A Systematic Review
Abstract
:1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gupta, A.; Felton, D.A.; Jemt, T.; Koka, S. Rehabilitation of Edentulism and Mortality: A Systematic Review. J. Prosthodont. 2019, 28, 526–535. [Google Scholar] [CrossRef] [PubMed]
- Broers, D.L.M.; Dubois, L.; de Lange, J.; Su, N.; de Jongh, A. Reasons for Tooth Removal in Adults: A Systematic Review. Int. Dent. J. 2022, 72, 52–57. [Google Scholar] [CrossRef] [PubMed]
- Emami, E.; de Souza, R.F.; Kabawat, M.; Feine, J.S. The impact of edentulism on oral and general health. Int. J. Dent. 2013, 2013, 498305. [Google Scholar] [CrossRef]
- Helal, M.A.; Al-Gazzar, A.E.; Abas, M.; Akhtar, S.; Gad, M.M.; Al-Thobity, A.M. Comparative Effect of Different Surface Treatments on the Shear Bond Strength of Two Types of Artificial Teeth Bonded to Two Types of Denture Base Resins. J. Prosthodont. 2022, 31, 427–433. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.S.; Weyant, R.J.; Corby, P.; Kritchevsky, S.B.; Harris, T.B.; Rooks, R.; Rubin, S.M.; Newman, A.B. Edentulism and nutritional status in a biracial sample of well-functioning, community-dwelling elderly: the health, aging, and body composition study. Am. J. Clin. Nutr. 2004, 79, 295–302. [Google Scholar] [CrossRef] [Green Version]
- Roberto, L.L.; Crespo, T.S.; Monteiro-Junior, R.S.; Martins, A.M.E.B.L.; De Paula, A.M.B.; Ferreira, E.F.; Haikal, D.S. Sociodemographic determinants of edentulism in the elderly population: A systematic review and meta-analysis. Gerodontology 2019, 36, 325–337. [Google Scholar] [CrossRef] [PubMed]
- Polzer, I.; Schimmel, M.; Müller, F.; Biffar, R. Edentulism as part of the general health problems of elderly adults. Int. Dent. J. 2010, 60, 143–155. [Google Scholar]
- Müller, F.; Naharro, M.; Carlsson, G.E. What are the prevalence and incidence of tooth loss in the adult and elderly population in Europe? Clin. Oral. Implants Res. 2007, 18 (Suppl. 3), 2–14. [Google Scholar] [CrossRef] [Green Version]
- Al-Rafee, M.A. The epidemiology of edentulism and the associated factors: A literature Review. J. Family Med. Prim. Care 2020, 9, 1841–1843. [Google Scholar] [CrossRef]
- Douglass, C.W.; Shih, A.; Ostry, L. Will there be a need for complete dentures in the United States in 2020? J. Prosthet. Dent. 2002, 87, 5–8. [Google Scholar] [CrossRef]
- Borg-Bartolo, R.; Roccuzzo, A.; Molinero-Mourelle, P.; Schimmel, M.; Gambetta-Tessini, K.; Chaurasia, A.; Koca-Ünsal, R.B.; Tennert, C.; Giacaman, R.; Campus, G. Global prevalence of edentulism and dental caries in middle-aged and elderly persons: A systematic review and meta-analysis. J. Dent. 2022, 127, 104335. [Google Scholar] [CrossRef] [PubMed]
- Paulino, M.R.; Alves, L.R.; Gurgel, B.C.; Calderon, P.S. Simplified versus traditional techniques for complete denture fabrication: A systematic review. J. Prosthet Dent. 2015, 113, 12–16. [Google Scholar] [CrossRef] [PubMed]
- Al-Dwairi, Z.N.; Tahboub, K.Y.; Baba, N.Z.; Goodacre, C.J.; Özcan, M. A Comparison of the Surface Properties of CAD/CAM and Conventional Polymethylmethacrylate (PMMA). J. Prosthodont. 2019, 28, 452–457. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Prpić, V.; Schauperl, Z.; Ćatić, A.; Dulčić, N.; Čimić, S. Comparison of Mechanical Properties of 3D-Printed, CAD/CAM, and Conventional Denture Base Materials. J. Prosthodont. 2020, 29, 524–528. [Google Scholar] [CrossRef]
- Kawai, Y.; Murakami, H.; Shariati, B.; Klemetti, E.; Blomfield, J.V.; Billette, L.; Lund, J.P.; Feine, J.S. Do traditional techniques produce better conventional complete dentures than simplified techniques? J. Dent. 2005, 33, 659–668. [Google Scholar] [CrossRef]
- Kawai, Y.; Murakami, H.; Takanashi, Y.; Lund, J.P.; Feine, J.S. Efficient resource use in simplified complete denture fabrication. J. Prosthodont. 2010, 19, 512–516. [Google Scholar] [CrossRef]
- Regis, R.R.; Cunha, T.R.; Della Vecchia, M.P.; Ribeiro, A.B.; Silva-Lovato, C.H.; de Souza, R.F. A randomised trial of a simplified method for complete denture fabrication: Patient perception and quality. J. Oral Rehabil. 2013, 40, 535–545. [Google Scholar] [CrossRef]
- Batisse, C.; Nicolas, E. Comparison of CAD/CAM and Conventional Denture Base Resins: A Systematic Review. Appl. Sci. 2021, 11, 5990. [Google Scholar] [CrossRef]
- Gharechahi, J.; Asadzadeh, N.; Shahabian, F.; Gharechahi, M. Dimensional changes of acrylic resin denture bases: Conventional versus injection-molding technique. J. Dent. 2014, 11, 398–405. [Google Scholar]
- Zafar, M.S. Prosthodontic Applications of Polymethyl Methacrylate (PMMA): An Update. Polymers 2020, 12, 2299. [Google Scholar] [CrossRef]
- Lee, H.J.; Kim, C.W.; Kim, Y.S. The Level of Residual Monomer in Injection Molded Denture Base Materials. J. Korean Acad. Prosthodont. 2003, 41, 360–368. [Google Scholar]
- Matos, A.O.; Costa, J.O.; Beline, T.; Ogawa, E.S.; Assunção, W.G.; Mesquita, M.F.; Consani, R.X.; Barão, V.A. Effect of Disinfection on the Bond Strength between Denture Teeth and Microwave-Cured Acrylic Resin Denture Base. J. Prosthodont. 2018, 27, 169–176. [Google Scholar] [CrossRef] [PubMed]
- Pero, A.C.; Scavassin, P.M.; Nunes, É.M.; Policastro, V.B.; Giro, G.; Compagnoni, M.A. Bond strength of artificial teeth attached to a microwave-polymerized denture base resin after immersion in disinfectant solutions. J. Prosthodont. 2016, 25, 576–579. [Google Scholar] [CrossRef] [PubMed]
- Marra, J.; de Souza, R.F.; Barbosa, D.B.; Pero, A.C.; Compagnoni, M.A. Evaluation of the bond strength of denture base resins to acrylic resin teeth: Effect of thermocycling. J. Prosthodont. 2009, 18, 438–443. [Google Scholar] [CrossRef]
- Madhav, G.V.; Raj, S.; Yadav, N.; Mudgal, I.; Mehta, N.; Tatwadiya, R. Shear bond strength of acrylic teeth to acrylic denture base after different surface conditioning methods. J. Contemp. Dent. Pract. 2013, 14, 892–897. [Google Scholar] [PubMed]
- Chittaranjan, B.; Taruna, M.; Sudheer, N.; Patil, N.S. Evaluation of shear bond strength of three different types of artificial teeth to heat cure denture base resin: An in vitro study. Indian J. Dent. Res. 2013, 24, 321–325. [Google Scholar] [CrossRef]
- Barbosa, D.B.; Barão, V.A.; Monteiro, D.R.; Compagnoni, M.A.; Marra, J. Bond strength of denture teeth to acrylic resin: Effect of thermocycling and polymerisation methods. Gerodontology 2008, 25, 237–244. [Google Scholar] [CrossRef]
- Sari, F.; Ustun, O.; Kirmali, O. Efficacy of various pretreatments on the bond strength of denture teeth to denture base resins. Photomed. Laser Surg. 2018, 36, 214–220. [Google Scholar] [CrossRef]
- Prpić, V.; Schauperl, Z.; Glavina, D.; Ćatić, A.; Čimić, S. Comparison of shear bond strengths of different types of denture teeth to different denture base resins. J. Adv. Prosthodont. 2020, 12, 376–382. [Google Scholar] [CrossRef]
- Al-Somaiday, H.M.; Rafeeq, A.K.; Al-Samaray, M.E. Effect of Different Surface Modifications of Acrylic Teeth and Thermocycling on Shear Bond Strength to Polycarbonate Denture Base Material. Int. J. Biomater. 2022, 2022, 9855836. [Google Scholar] [CrossRef]
- Chen, L.; Li, D.; Zhou, J.; Lin, W.S.; Tan, J. Duplicating Complete Dentures with Conventional and Digital Methods: Comparisons of Trueness and Efficiency. Dent. J. 2022, 10, 35. [Google Scholar] [CrossRef] [PubMed]
- Stawarczyk, B.; Lümkemann, N.; Eichberger, M.; Wimmer, T. Accuracy of Digitally Fabricated Wax Denture Bases and Conventional Completed Complete Dentures. Dent. J. 2017, 5, 36. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gad, M.M.; Alshehri, S.Z.; Alhamid, S.A.; Albarrak, A.; Khan, S.Q.; Alshahrani, F.A.; Alqarawi, F.K. Water Sorption, Solubility, and Translucency of 3D-Printed Denture Base Resins. Dent. J. 2022, 10, 42. [Google Scholar] [CrossRef] [PubMed]
- Steinmassl, P.A.; Wiedemair, V.; Huck, C.; Klaunzer, F.; Steinmassl, O.; Grunert, I.; Dumfahrt, H. Do CAD/CAM dentures really release less monomer than conventional dentures? Clin. Oral Investig. 2017, 21, 1697–1705. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Han, W.; Li, Y.; Zhang, Y.; Lv, Y.; Zhang, Y.; Hu, P.; Liu, H.; Ma, Z.; Shen, Y. Design and fabrication of complete dentures using CAD/CAM technology. Medicine 2017, 96, e5435. [Google Scholar] [CrossRef]
- AlHelal, A.; AlRumaih, H.S.; Kattadiyil, M.T.; Baba, N.Z.; Goodacre, C.J. Comparison of retention between maxillary milled and conventional denture bases: A clinical study. J. Prosthet. Dent. 2017, 117, 233–238. [Google Scholar] [CrossRef]
- Kanazawa, M.; Inokoshi, M.; Minakuchi, S.; Ohbayashi, N. Trial of a CAD/CAM system for fabricating complete dentures. Dent. Mater. J. 2011, 30, 93–96. [Google Scholar] [CrossRef] [Green Version]
- Goodacre, B.J.; Goodacre, C.J.; Baba, N.Z.; Kattadiyil, M.T. Comparison of denture base adaptation between CAD-CAM and conventional fabrication techniques. J. Prosthet. Dent. 2016, 116, 249–256. [Google Scholar] [CrossRef]
- Ohkubo, C.; Shimpo, H.; Tokue, A.; Park, E.J.; Kim, T.H. Complete denture fabrication using piezography and CAD-CAM: A clinical report. J. Prosthet. Dent. 2018, 119, 334–338. [Google Scholar] [CrossRef]
- Kattadiyil, M.T.; Jekki, R.; Goodacre, C.J.; Baba, N.Z. Comparison of treatment outcomes in digital and conventional complete removable dental prosthesis fabrications in a predoctoral setting. J. Prosthet. Dent. 2015, 114, 818–825. [Google Scholar] [CrossRef]
- Kattadiyil, M.T.; AlHelal, A.; Goodacre, B.J. Clinical complications and quality assessments with computer-engineered complete dentures: A systematic review. J. Prosthet. Dent. 2017, 117, 721–728. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.I.; Cho, I.H.; Lee, J.S. The effect of various foods on the color stability of artificial teeth. J. Korean Acad. Prosthodont. 2009, 47, 82–90. [Google Scholar] [CrossRef] [Green Version]
- Klaiber, D.; Spintzyk, S.; Geis-Gerstorfer, J.; Klink, A.; Unkovskiy, A.; Huettig, F. Bonding Behavior of Conventional PMMA towards Industrial CAD/CAM PMMA and Artificial Resin Teeth for Complete Denture Manufacturing in a Digital Workflow. Materials 2021, 14, 3822. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Han, S.Y.; Moon, Y.H.; Lee, J. Shear bond strength between CAD/CAM denture base resin and denture artificial teeth when bonded with resin cement. J. Adv. Prosthodont. 2020, 12, 251–258. [Google Scholar] [CrossRef] [PubMed]
- Alves, A.C.; Cavalcanti, R.V.; Calderon, P.S.; Pernambuco, L.; Alchieri, J.C. Quality of life related to complete denture. Acta Odontol. Latinoam. 2018, 31, 91–96. [Google Scholar] [PubMed]
- AlZaher, Z.A.; Almaskin, D.F.; Qaw, M.S.; Abu Showmi, T.H.; Abualsaud, R.; Akhtar, S.; Gad, M.M. Chemo-Mechanical Approach to Improve Repair Bond Strength of Denture Teeth. Int. J. Dent. 2020, 2020, 8870361. [Google Scholar] [CrossRef]
- Andrade de Freitas, S.L.; Brandt, W.C.; Miranda, M.E.; Vitti, R.P. Effect of thermocycling, teeth, and polymerization methods on bond strength teeth-denture base. Int. J. Dent. 2018, 2018, 2374327. [Google Scholar] [CrossRef]
- Koodaryan, R.; Hafezeqoran, A. Effect of surface treatment methods on the shear bond strength of auto-polymerized resin to thermoplastic denture base polymer. J. Adv. Prosthodont. 2016, 8, 504–510. [Google Scholar] [CrossRef] [Green Version]
- Gharebagh, T.G.; Hamedirad, F.; Miruzadeh, K. Comparison of bond strength of acrylic, composite, and nanocomposite artificial teeth to heat-cure acrylic denture base resin. Front. Dent. 2019, 16, 166–172. [Google Scholar] [CrossRef]
- Elkassaby, A.A.; Kandil, M.M.; Alian, G.A. Microtensile vs. Flexural Bond Strength for Bond Strength Assessment. J. Res. Med. Dent. Sci. 2022, 10, 53–58. [Google Scholar]
- Sirisha, K.; Rambabu, T.; Shankar, Y.R.; Ravikumar, P. Validity of bond strength tests: A critical review: Part I. J. Conserv. Dent. 2014, 17, 305–311. [Google Scholar] [CrossRef] [Green Version]
- Van Meerbeek, B.; Peumans, M.; Poitevin, A.; Mine, A.; Van Ende, A.; Neves, A.; De Munck, J. Relationship between bond-strength tests and clinical outcomes. Dent. Mater. 2010, 26, e100–e121. [Google Scholar] [CrossRef] [PubMed]
- Patil, S.B.; Naveen, B.H.; Patil, N.P. Bonding acrylic teeth to acrylic resin denture bases: A review. Gerodontology 2006, 23, 131–139. [Google Scholar] [CrossRef] [PubMed]
- Yanikoglu, D.N.; Duymus, D.Z.; Bayindir, D.F. Comparative bond strengths of autopolymerising denture resin and light cured composite resin to denture teeth. Int. Dent. J. 2002, 52, 20–24. [Google Scholar] [CrossRef]
- Yoshida, Y.; Yoshihara, K.; Nagaoka, N.; Hayakawa, S.; Torii, Y.; Ogawa, T.; Osaka, A.; Van Meerbeek, B. Self-assembled nano-layering at the adhesive interface. J. Dent. Res. 2012, 91, 376–381. [Google Scholar] [CrossRef] [PubMed]
- Akin, H.; Kirmali, O.; Tugut, F.; Coskun, M.E. Effects of different surface treatments on the bond strength of acrylic denture teeth to polymethylmethacrylate denture base material. Photomed. Laser Surg. 2014, 32, 512–516. [Google Scholar] [CrossRef]
- Akin, H.; Tugut, F.; Guney, U.; Akar, T. Shear bond strength of denture teeth to two chemically different denture base resins after various surface treatments. J. Prosthodont. 2014, 23, 152–156. [Google Scholar] [CrossRef]
- Rosca, B.; Ramalho, S.; Sampaio-Fernandes, J.C.; Portugal, J. Reparability of two different CAD/CAM polymer materials using a light-cured composite and universal adhesives. Rev. Port. Estomatol. Med. Dentária Cir. Maxilofac. 2016, 57, 189–196. [Google Scholar] [CrossRef] [Green Version]
- Barragan, G.; Chasqueira, F.; Arantes-Oliveira, S.; Portugal, J. Ceramic repair: Influence of chemical and mechanical surface conditioning on adhesion to zirconia. Oral Health Dent. Manag. 2014, 13, 155–158. [Google Scholar]
- Seabra, B.; Arantes-Oliveira, S.; Portugal, J. Influence of multimode universal adhesives and zirconia primer application techniques on zirconia repair. J. Prosthet. Dent. 2014, 112, 182–187. [Google Scholar] [CrossRef] [PubMed]
- Mine, A.; Kabetani, T.; Kawaguchi-Uemura, A.; Higashi, M.; Tajiri, Y.; Hagino, R.; Imai, D.; Yumitate, M.; Ban, S.; Matsumoto, M.; et al. Effectiveness of current adhesive systems when bonding to CAD/CAM indirect resin materials: A review of 32 publications. Jpn. Dent. Sci. Rev. 2019, 55, 41–50. [Google Scholar] [CrossRef] [PubMed]
- Consani, R.L.; Naoe, H.T.; Mesquita, M.F.; Sinhoreti, M.A.; Mendes, W.B. Effect of ridge-lap surface treatments on the bond of resin teeth to denture base. J. Adhes. Dent. 2011, 13, 287–293. [Google Scholar]
- Srinivasan, M.; Schimmel, M.; Naharro, M.; O’Neill, C.; McKenna, G.; Müller, F. CAD/CAM milled removable complete dentures: time and cost estimation study. J. Dent. 2019, 80, 75–79. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Srinivasan, M.; Cantin, Y.; Mehl, A.; Gjengedal, H.; Müller, F.; Schimmel, M. CAD/CAM milled removable complete dentures: an in vitro evaluation of trueness. Clin. Oral. Investig. 2017, 21, 2007–2019. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Srinivasan, M.; Gjengedal, H.; Cattani-Lorente, M.; Moussa, M.; Durual, S.; Schimmel, M.; Müller, F. CAD/CAM milled complete removable dental prostheses: An in vitro evaluation of biocompatibility, mechanical properties, and surface roughness. Dent. Mater. J. 2018, 37, 526–533. [Google Scholar] [CrossRef] [Green Version]
- Bidra, A.S.; Farrell, K.; Burnham, D.; Dhingra, A.; Taylor, T.D.; Kuo, C.L. Prospective cohort pilot study of 2-visit CAD/CAM monolithic complete dentures and implant-retained overdentures: Clinical and patient-centered outcomes. J. Prosthet. Dent. 2016, 115, 578–586.e1. [Google Scholar] [CrossRef]
- Astudillo-Rubio, D.; Delgado-Gaete, A.; Bellot-Arcís, C.; Montiel-Company, J.M.; Pascual-Moscardó, A.; Almerich-Silla, J.M. Mechanical properties of provisional dental materials: A systematic review and meta-analysis. PLoS ONE 2018, 13, e0193162. [Google Scholar]
- Aldegheishem, A.; AlDeeb, M.; Al-Ahdal, K.; Helmi, M.; Alsagob, E.I. Influence of Reinforcing Agents on the Mechanical Properties of Denture Base Resin: A Systematic Review. Polymers 2021, 13, 3083. [Google Scholar] [CrossRef]

| Authors, Year | Title | n | Denture Base Material | Denture Teeth Material | Results (MPa) | Conclusions |
|---|---|---|---|---|---|---|
| Han et al. [45] (2020) | Shear bond strength between CAD/CAM denture base resin and denture artificial teeth when bonded with resin cement | 10 per group | CAD/CAM (milled) (PMMA Block-pink prepolymerized resin block) | Highly cross-linked acrylic resin teeth (VITA MFT) | 19.61 ± 3.07 | Shear bond strengths of CAD/CAM denture base materials and resin denture teeth using resin cement are comparable to those of conventional methods |
| CAD/CAM (milled) (PMMA Block-pink prepolymerized resin block | Composite resin teeth (Duracross Physio) | 21.80 ± 3.00 | ||||
| CAD/CAM (milled) (PMMA Block-pink prepolymerized resin block | Composite resin teeth (Endura Posterio) | 16.90 ± 3.48 | ||||
| CAD/CAM (milled) (Vipi Block-Pink) | Highly cross-linked acrylic resin teeth (VITA MFT) | 19.79 ± 2.41 | ||||
| CAD/CAM (milled) (Vipi Block-Pink) | Composite resin teeth (Duracross Physio) | 14.35 ± 4.56 | ||||
| CAD/CAM (milled) (Vipi Block-Pink) | Composite resin teeth (Endura Posterio) | 17.20 ± 3.46 | ||||
| Heat-polymerized (Vertex Rapid Simplified) | Highly cross-linked acrylic resin teeth (VITA MFT) | 18.84 ± 4.38 | ||||
| Heat-polymerized (Vertex Rapid Simplified) | Composite resin teeth (Duracross Physio) | 19.31 ± 5.16 | ||||
| Heat-polymerized (Vertex Rapid Simplified) | Composite resin teeth (Endura Posterio) | 10.17 ± 4.34 | ||||
| Prpić et al. [29] (2020) | Comparison of shear bond strengths of different types of denture teeth to different denture base resins | 8 per group | CAD/CAM (milled) (IvoBase CAD) | Acrylic teeth (SR Orthotyp S PE) | 12.56 ± 2.92 | Shear bond strength values between CAD/CAM (milled) denture base resins and different types of prefabricated teeth showed high shear bond strength values and are comparable with conventional methods |
| CAD/CAM (milled) (IvoBase CAD) | Nanohybrid composite teeth (Phonares II Typ) | 15.04 ± 1.68 | ||||
| CAD/CAM (milled) (IvoBase CAD) | Cross-linked teeth (SR Orthotyp DCL) | 12.84 ± 3.21 | ||||
| CAD/CAM (milled) (IvoBase CAD) | CAD/CAM (milled) denture teeth (SR Vivodent CAD) | 13.66 ± 4.27 | ||||
| Heat-polymerized (ProBase Hot) | Acrylic teeth (SR Orthotyp S PE) | 18.10 ± 2.68 | ||||
| Heat-polymerized (ProBase Hot) | Nanohybrid composite teeth (Phonares II Typ) | 12.81 ± 3.91 | ||||
| Heat-polymerized (ProBase Hot) | Cross-linked teeth (SR Orthotyp DCL) | 14.29 ± 4.27 | ||||
| Helal et al. [4] (2021) | Comparative effect of different surface treatments on the shear bond strength of two types of artificial teeth bonded to two types of denture base resins | 10 per group | CAD/CAM (milled) (AvaDent PMMA Pucks) | Acrylic teeth (Acrostone) | 9.64 ± 0.63 | According to the results, there were significant differences in the SBS between the denture teeth bonded to heat-polymerized and CAD/CAM DBRs |
| CAD/CAM (milled) (AvaDent PMMA Pucks) | Composite teeth (Eraylar- ostim) | 7.92 ± 0.61 | ||||
| Heat-polymerized (Acrostone) | Acrylic teeth (Acrostone) | 4.65 ± 0.54 | ||||
| Heat-polymerized (Acrostone) | Composite teeth (Eraylar- ostim) | 3.28 ± 0.92 |
| Authors, Year | Samples Obtained through a Standardized Process | Single Operator of the Machine | Sample Size Calculation | Blinding of the Testing Machine Operator | Specimens, Test, and Formulas According to Standard Specifications | Risk of Bias |
|---|---|---|---|---|---|---|
| Han et al. [45] (2020) | 0 | 2 | 2 | 2 | 0 | Moderate |
| Prpić et al. [29] (2020) | 0 | 2 | 2 | 2 | 0 | Moderate |
| Helal et. al. [4] (2021) | 0 | 2 | 2 | 2 | 0 | Moderate |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Prpic, V.; Catic, A.; Kraljevic Simunkovic, S.; Bergman, L.; Cimic, S. The Shear Bond Strength between Milled Denture Base Materials and Artificial Teeth: A Systematic Review. Dent. J. 2023, 11, 66. https://doi.org/10.3390/dj11030066
Prpic V, Catic A, Kraljevic Simunkovic S, Bergman L, Cimic S. The Shear Bond Strength between Milled Denture Base Materials and Artificial Teeth: A Systematic Review. Dentistry Journal. 2023; 11(3):66. https://doi.org/10.3390/dj11030066
Chicago/Turabian StylePrpic, Vladimir, Amir Catic, Sonja Kraljevic Simunkovic, Lana Bergman, and Samir Cimic. 2023. "The Shear Bond Strength between Milled Denture Base Materials and Artificial Teeth: A Systematic Review" Dentistry Journal 11, no. 3: 66. https://doi.org/10.3390/dj11030066
APA StylePrpic, V., Catic, A., Kraljevic Simunkovic, S., Bergman, L., & Cimic, S. (2023). The Shear Bond Strength between Milled Denture Base Materials and Artificial Teeth: A Systematic Review. Dentistry Journal, 11(3), 66. https://doi.org/10.3390/dj11030066