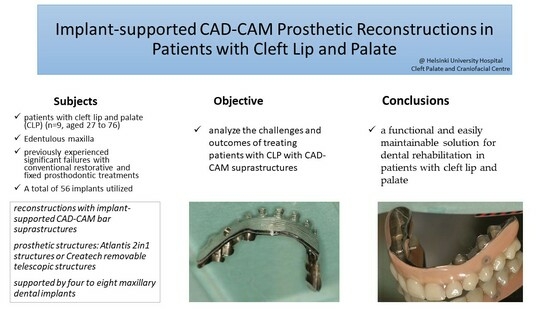
Use of Individually Designed CAD/CAM Suprastructures for Dental Reconstruction in Patients with Cleft Lip and Palate
Abstract
:1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Qureshi, W.A.; Beiraghi, S.; Leon-Salazar, V. Dental anomalies associated with unilateral and bilateral cleft lip and palate. J. Dent. Child. (Chic.) 2012, 79, 69–73. [Google Scholar]
- Worley, M.L.; Patel, K.G.; Kilpatrick, L.A. Cleft Lip and Palate. Clin. Perinatol. 2018, 45, 661–678. [Google Scholar] [CrossRef]
- Téllez-Conti, C.; Mora, D., II; Díaz-Báez, D.; Ocampo-Arias, I.J.; Jiménez-Luna, N.E.; Niño-Paz, J.C.; González-Carrera, M.C. Craniofacial Growth Analysis of Individuals With and Without Cleft Lip and Palate in Colombia. Cleft Palate Craniofac. J. 2021, 59, 577–588. [Google Scholar] [CrossRef]
- Mangione, F.; Nguyen, L.; Foumou, N.; Bocquet, E.; Dursun, E. Cleft palate with/without cleft lip in French children: Radiographic evaluation of prevalence, location and coexistence of dental anomalies inside and outside cleft region. Clin. Oral Investig. 2018, 22, 689–695. [Google Scholar] [CrossRef]
- De Stefani, A.; Bruno, G.; Balasso, P.; Mazzoleni, S.; Baciliero, U.; Gracco, A. Prevalence of Hypodontia in Unilateral and Bilateral Cleft Lip and Palate Patients Inside and Outside Cleft Area: A Case-Control Study. J. Clin. Pediatr. Dent. 2019, 43, 126–130. [Google Scholar] [CrossRef]
- Suzuki, A.; Nakano, M.; Yoshizaki, K.; Yasunaga, A.; Haruyama, N.; Takahashi, I. A Longitudinal Study of the Presence of Dental Anomalies in the Primary and Permanent Dentitions of Cleft Lip and/or Palate Patients. Cleft Palate Craniofac. J. 2017, 54, 309–320. [Google Scholar] [CrossRef]
- Tan, E.L.Y.; Yow, M.; Kuek, M.C.; Wong, H.C. Dental maturation of unilateral cleft lip and palate. Ann. Maxillofac. Surg. 2012, 2, 158–162. [Google Scholar] [CrossRef]
- Doğan, E.; Ergican, G.Ö.; Doğan, S. Maxillary Development in Patients with Unilateral Cleft Lip and Palate Compared with Individuals Having Skeletal Class I and Class III Malocclusion. J. Clin. Pediatr. Dent. 2021, 45, 140–145. [Google Scholar] [CrossRef]
- Chiu, Y.T.; Liao, Y.F. Is cleft severity related to maxillary growth in patients with unilateral cleft lip and palate? Cleft Palate Craniofac. J. 2012, 49, 535–540. [Google Scholar] [CrossRef]
- Chen, Z.-Q.; Wu, J.; Chen, R.-J. Sagittal maxillary growth pattern in unilateral cleft lip and palate patients with unrepaired cleft palate. Craniofac. Surg. 2012, 23, 491–493. [Google Scholar] [CrossRef]
- Gundlach, K.K.; Bardach, J.; Filippow, D.; Stahl-de Castrillon, F.; Lenz, J.H. Two-stage palatoplasty, is it still a valuable treatment protocol for patients with a cleft of lip, alveolus, and palate? J. Craniomaxillofac. Surg. 2013, 41, 62–70. [Google Scholar] [CrossRef] [PubMed]
- Semb, G.; Brattström, V.; Mølsted, K.; Prahl-Andersen, B.; Shaw, W.C. The Eurocleft study: Intercenter study of treatment outcome in patients with complete cleft lip and palate. Part 1: Introduction and treatment experience. Cleft Palate Craniofac. J. 2005, 42, 64–68. [Google Scholar] [CrossRef]
- Xu, H.; Salyer, K.E.; Genecov, E.R. Primary bilateral two-stage cleft lip/nose repair: Part II. J. Craniofac. Surg. 2009, 20, 1927–1933. [Google Scholar] [CrossRef]
- Movahhedian, N.; Vossoughi, M.; Hajati-Sisakht, M. A Cone-Beam Computed Tomographic Study of Alveolar Bone Morphology in Patients with Unilateral Cleft Lip and Palate. Cleft Palate Craniofac. J. 2020, 57, 273–281. [Google Scholar] [CrossRef] [PubMed]
- Sahni, V.; Grover, V.; Sood, S.; Jain, A. The Periodontal Status of Orofacial Cleft Patients: A Systematic Review and Meta-Analysis. Cleft Palate Craniofac. J. 2022. [Google Scholar] [CrossRef]
- Marzouk, T.; Youssef, M.; Tsigarida, A.; McKinney, C.; Wong, C.; DeLucia, L.; Shah, R.; Wang, H.; Malmstrom, H.; Shope, E. Association between oral clefts and periodontal clinical measures: A meta-analysis. Int. J. Paediatr. Dent. 2022, 32, 558–575. [Google Scholar] [CrossRef] [PubMed]
- Passinato Gheller, S.A.; Porto, A.N.; Borba, A.M.; Veiga, K.A.; Aranha, A.M.F. Periodontal Findings in Children and Adolescents with Cleft Lip and/or Palate: A Case-Control Study. Pediatr. Dent. 2021, 43, 133–139. [Google Scholar]
- Leu, G.R.; Ebert, B.E.; Roby, B.B.; Scott, A.R. Cleft Palate Repair by Otolaryngologist-Head and Neck Surgeons: Risk Factors for Postoperative Fistula. Laryngoscope 2021, 131, 1281–1285. [Google Scholar] [CrossRef]
- Duskova, M.; Kotova, M.; Sedlackova, K.; Leamerova, E.; Horak, J. Bone reconstruction of the maxillary alveolus for subsequent insertion of a dental implant in patients with cleft lip and palate. J. Craniofac. Surg. 2007, 18, 630–638. [Google Scholar] [CrossRef]
- Thalji, G.; McGraw, K.; Cooper, L.F. Maxillary Complete Denture Outcomes: A Systematic Review of Patient-Based Outcomes. Int. J. Oral Maxillofac. Implants 2016, 31, 169–188. [Google Scholar] [CrossRef]
- Murat, S.; Gurbuz, A.; Genc, F. Prosthetic rehabilitation of a patient with bilateral cleft lip and palate using osseointegrated implants and extracoronal resilient attachments: A case report. Cleft Palate Craniofac. J. 2011, 48, 342–347. [Google Scholar] [CrossRef] [PubMed]
- Kern, J.-S.; Kern, T.; Wolfart, S.; Heussen, N. A systematic review and meta-analysis of removable and fixed implant-supported prostheses in edentulous jaws: Post-loading implant loss. Clin. Oral Implants Res. 2016, 27, 174–195. [Google Scholar] [CrossRef] [PubMed]
- Frederick, R.; Hogan, A.C.; Seabolt, N.; Stocks, R.M.S. An Ideal Multidisciplinary Cleft Lip and Cleft Palate Care Team. Oral Dis. 2022, 28, 1412–1417. [Google Scholar] [CrossRef] [PubMed]
- Figueras-Alvarez, O.; Cantó-Navés, O.; Real-Voltas, F.; Roig, M. Protocol for the clinical assessment of passive fit for multiple implant-supported prostheses: A dental technique. J. Prosthet. Dent. 2021, 126, 727–730. [Google Scholar] [CrossRef]
- Wegscheider, W.; Bratschko, R.; Plischka, G.; Haas, M.; Permann, R.; Parsche, E. The system of prosthetic treatment for CLAP patients. J. Craniomaxillofac. Surg. 1989, 17, 49–51. [Google Scholar] [CrossRef] [PubMed]
- Mirchandani, B.; Zhou, T.; Heboyan, A.; Yodmongkol, S.; Buranawat, B. Biomechanical Aspects of Various Attachments for Implant Overdentures: A Review. Polymers 2021, 13, 3248. [Google Scholar] [CrossRef]
- Mumcu, E.; Dayan, S.C.; Genceli, E.; Geckili, O. Comparison of four-implant-retained overdentures and implant-supported fixed prostheses using the All-on-4 concept in the maxilla in terms of patient satisfaction, quality of life, and marginal bone loss: A 2-year retrospective study. Quintessence Int. 2020, 51, 388–396. [Google Scholar] [CrossRef]
- Morton, D.; Gallucci, G.; Lin, W.S.; Pjetursson, B.; Polido, W.; Roehling, S.; Sailer, I.; Aghaloo, T.; Albera, H.; Bohner, L.; et al. Group 2 ITI Consensus Report: Prosthodontics and implant dentistry. Clin. Oral Implants Res. 2018, 29, 215–223. [Google Scholar] [CrossRef]
- Tuna, H.S.; Pekkan, G.; Buyukgural, B. Rehabilitation of an Edentulous Cleft Lip and Palate Patient With a Soft Palate Defect Using a Bar-Retained, Implant-Supported Speech-Aid Prosthesis: A Clinical Report. Cleft Palate Craniofac. J. 2009, 46, 97–102. [Google Scholar] [CrossRef]
- Boven, G.C.; Raghoebar, G.M.; Vissink, A.; Meijer, H.J. Improving masticatory performance, bite force, nutritional state and patient’s satisfaction with implant overdentures: A systematic review of the literature. J. Oral Rehabil. 2015, 42, 220–233. [Google Scholar] [CrossRef] [PubMed]
- Kutkut, A.; Bertoli, E.; Frazer, R.; Pinto-Sinai, G.; Hidalgo, R.F.; Studts, J. A systematic review of studies comparing conventional complete denture and implant retained overdenture. J. Prosthodont. Res. 2018, 62, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Gaggl, A.; Schultes, G.; Kärcher, H.; Mossböck, R. Periodontal disease in patients with cleft palate and patients with unilateral and bilateral clefts of lip, palate, and alveolus. J. Periodontol. 1999, 70, 171–178. [Google Scholar] [CrossRef] [PubMed]
- Zanolla, J.; Amado, F.M.; da Silva, W.S.; Ayub, B.; de Almeida, A.L.; Soares, S. Success rate in implant-supported overdenture and implant-supported fixed denture in cleft lip and palate patients. Ann. Maxillofac. Surg. 2016, 6, 223–227. [Google Scholar] [CrossRef]
- Wermker, K.; Jung, S.; Joos, U.; Kleinheinz, J. Dental implants in cleft lip, alveolus, and palate patients: A systematic review. Int. J. Oral Maxillofac. Implants 2014, 29, 384–390. [Google Scholar] [CrossRef]
- Arshad, M.; Ameri, N.; Heidari, A.; Shirani, G. Dental rehabilitation of a cleft lip and palate patient by implant-supported overdenture: A case report. Clin. Case Rep. 2020, 8, 1932–1936. [Google Scholar] [CrossRef]
- Di Francesco, F.; De Marco, G.; Capcha, E.B.; Lanza, A.; Cristache, C.M.; Vernal, R.; Cafferata, E.A. Patient satisfaction and survival of maxillary overdentures supported by four or six splinted implants: A systematic review with meta-analysis. BMC Oral Health 2021, 21, 247. [Google Scholar] [CrossRef]
- Leven, J.; Ali, R.; Butterworth, C.J. Zygomatic implant-supported prosthodontic rehabilitation of edentulous patients with a history of cleft palate: A clinical report. J. Prosthet. Dent. 2022, 127, 684–688. [Google Scholar] [CrossRef] [PubMed]
- Mommaerts, M.Y. Additively manufactured sub-periosteal jaw implants. Int. J. Oral Maxillofac. Surg. 2017, 46, 938–940. [Google Scholar] [CrossRef]
- Gray, D.; Patel, J. Implant-supported overdentures: Part 1. Br. Dent. J. 2021, 231, 94–100. [Google Scholar] [CrossRef]
- Lin, W.S.; Chou, J.C.; Metz, M.J.; Harris, B.T.; Morton, D. Use of intraoral digital scanning for a CAD/CAM-fabricated milled bar and superstructure framework for an implant-supported, removable complete dental prosthesis. J. Prosthet. Dent. 2015, 113, 509–515. [Google Scholar] [CrossRef]
- Wismeijer, D.; Joda, T.; Flügge, T.; Fokas, G.; Tahmaseb, A.; Bechelli, D.; Bohner, L.; Bornstein, M.; Burgoyne, A.; Caram, S.; et al. Group 5 ITI Consensus Report: Digital technologies. Clin. Oral Implants Res. 2018, 29, 436–442. [Google Scholar] [CrossRef] [PubMed]



| Patient No. | Bone Grafting | Sinus Lift |
|---|---|---|
| 1 | Autogenous bone chips | Hydrolift |
| 2 | None | Condensation |
| 3 | Iliac crest | None |
| 4 | BioOss | Hydrolift |
| 5 | Iliac crest | Lateral window |
| 6 | Iliac crest | None |
| 7 | None | None |
| 8 | Iliac crest | Lateral window |
| 9 | None | None |
| Patient No. | Sex | Diagnosis | Age (y) | Primary Reason for Treatment | Earlier Cleft and CMFS Operations | Opposing Dentition |
|---|---|---|---|---|---|---|
| 1 | M | BCLP | 65 | Secondary caries in dental bridge | Primary closure 4 mo, palatoplasty 2 y, Le Fort I 41 y. | Own teeth |
| 2 | F | BCLP | 65 | Secondary caries in dental bridge | Primary closure 6 y, naso- and rhinoplasty 10 y, palatoplasty 11 y, lip plasty 13 y, oronasal fistula closure 20 y. | Partial removable denture |
| 3 | M | UCLP | 66 | Periodontitis | Primary closure unknown. No cleft augmentation. | 2in1 |
| 4 | M | UCLP | 61 | Periodontitis | Primary closure 2 mo, palatoplasty 2.5 y, lip and rhinoplasty 6 y, lip plasty 7 y, fistula closure 15 y. | Own teeth |
| 5 | F | UCLP | 54 | Periodontitis | Primary closure unknown. Palatal closure 2 y. | Own teeth |
| 6 | F | UCLP | 62 | Secondary caries in dental crowns | Primary lip closure 4 mo, palatal closure 2 y, lip plasty 20 y. | Partial removable denture |
| 7 | F | UCLP | 27 | Periodontitis | Primary closure 3 mo, cleft augmentation 13 y. | Own teeth |
| 8 | M | BCLP | 76 | Edentulous jaws, reason unknown | Primary closure unknown as small child. No later operations. | Complete denture |
| 9 | M | UCLP | 47 | Secondary caries in dental bridge | Primary closure unknown. Le fort I osteotomy. Septoplasty. | Own teeth |
| Patient No. | Oronasal Fistula | Number of Mx Implants | Type of Fixture | Prosthodontics | Complications | Follow-Up (mo) |
|---|---|---|---|---|---|---|
| 1 | Significant | 6 | AnyRidge | Createch | Prosthesis fracture 16 months | 45 |
| 2 | Significant | 6 | Ankylos | Createch | None | 22 |
| 3 | None | 4 | Ankylos | Createch | None | 49 |
| 4 | None | 8 | Ankylos | Isus/Atlantis | Failure of osseointegration (n = 1) | 49 |
| 5 | None | 7 | Ankylos | Createch | None | 29 |
| 6 | None | 8 | Ankylos | Isus/Atlantis | None | 102 |
| 7 | Minor | 8 | Straumann BL | Createch | None | 13 |
| 8 | Significant | 4 | Ankylos | Createch | None | 12 |
| 9 | Minor | 5 | Ankylos | Isus/Atlantis | None | 12 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mäntynen, P.; Laurila, M.; Strausz, T.; Mauno, J.; Leikola, J.; Suojanen, J. Use of Individually Designed CAD/CAM Suprastructures for Dental Reconstruction in Patients with Cleft Lip and Palate. Dent. J. 2023, 11, 212. https://doi.org/10.3390/dj11090212
Mäntynen P, Laurila M, Strausz T, Mauno J, Leikola J, Suojanen J. Use of Individually Designed CAD/CAM Suprastructures for Dental Reconstruction in Patients with Cleft Lip and Palate. Dentistry Journal. 2023; 11(9):212. https://doi.org/10.3390/dj11090212
Chicago/Turabian StyleMäntynen, Pilvi, Marisa Laurila, Tommi Strausz, Jari Mauno, Junnu Leikola, and Juho Suojanen. 2023. "Use of Individually Designed CAD/CAM Suprastructures for Dental Reconstruction in Patients with Cleft Lip and Palate" Dentistry Journal 11, no. 9: 212. https://doi.org/10.3390/dj11090212
APA StyleMäntynen, P., Laurila, M., Strausz, T., Mauno, J., Leikola, J., & Suojanen, J. (2023). Use of Individually Designed CAD/CAM Suprastructures for Dental Reconstruction in Patients with Cleft Lip and Palate. Dentistry Journal, 11(9), 212. https://doi.org/10.3390/dj11090212