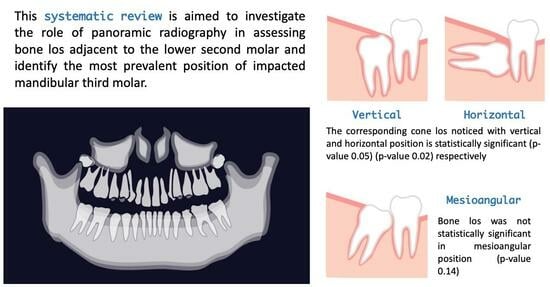
The Accuracy of Bone Assessment Distal to Lower Second Molars Using Panoramic Radiography: A Systematic Review and Meta-Analysis
Abstract
:1. Introduction
2. Materials and Methods
- P: Patients with impacted mandibular third molar.
- I: OPG.
- C: cone beam computed tomography (CBCT) or clinical measurements, including intrasurgical measurements if they are used in the included studies.
- O: Status of bone loss distal to lower second molar in cases of third molar impaction.
2.1. Inclusion Criteria
- Original studies;
- Studies reporting the effects of impacted mandibular molar on the bone distal to the lower second molar using panoramic radiography;
- Studies comparing OPG to other imaging tools for assessing bone loss distal to the lower second molar;
- Studies reporting types of impaction associated with bone loss on the distal aspect of the lower second molar;
- Studies published from January 2012 to January 2024.
2.2. Exclusion Criteria
- Case reports;
- Narrative reviews;
- Book chapters;
- Languages other than English and Spanish.
2.3. Search Strategy
2.4. Study Retrieval
2.5. Data Collection
2.6. Risk of Biased Assessment
2.7. Statistical Analysis
3. Results
3.1. Study Selection
3.2. Study Characteristics
3.3. Descriptive Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Alfadil, L.; Almajed, E. Prevalence of impacted third molars and the reason for extraction in Saudi Arabia. Saudi Dent. J. 2020, 32, 262–268. [Google Scholar] [CrossRef] [PubMed]
- Passi, D.; Singh, G.; Dutta, S.; Srivastava, D.; Chandra, L.; Mishra, S.; Srivastava, A.; Dubey, M. Study of pattern and prevalence of mandibular impacted third molar among Delhi-National Capital Region population with newer proposed classification of mandibular impacted third molar: A retrospective study. Natl. J. Maxillofac. Surg. 2019, 10, 59–67. [Google Scholar] [CrossRef] [PubMed]
- Puryer, J.; Mittal, T.; McNamara, C.; Ireland, T.; Sandy, J. Bilateral Transverse Mandibular Second Molars: A Case Report. Dent J. 2016, 4, 43. [Google Scholar] [CrossRef] [PubMed]
- Rezaei, F.; Imani, M.M.; Khavid, A.; Nabavi, A. Patterns of Mandibular Third Molar Impaction in an Iranian Subpopulation. Pesqui. Bras. Odontopediatria Clín. Integr. 2020, 20, e5411. [Google Scholar] [CrossRef]
- Garcovich, D.; Aiuto, R.; Serrano, E.; Re, D. Uncovering and autonomous eruption of palatally impacted canines. Eur. J. Paediatr. Dent. EJPD 2018, 19, 300–302. [Google Scholar] [CrossRef] [PubMed]
- Akhilanand, C.; Sachidanand, G.; RanjitKumar, P. Evaluation of impacted 3rd molars in Indian ethinicity on panoramic radiograph-a cross sectional study. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2021, 2021, 3499. [Google Scholar]
- Muhamad, A.-H.; Watted, N. Prevalence of Impacted Mandibular Third Molars in Population of Arab Israeli: A Retrospective Study. J. Med. Ment. Sci. 2016, 15, 91–98. [Google Scholar] [CrossRef]
- Carter, K.; Worthington, S. Predictors of Third Molar Impaction: A Systematic Review and Meta-analysis. J. Dent. Res. 2016, 95, 267–276. [Google Scholar] [CrossRef]
- Kaya, G.-S.; Muzaffer, M.A.; Omezli, M.; Dayı, E. Some morphological features related to mandibular third molar impaction. J. Clin. Exp. Dent. 2010, 2, 12–17. [Google Scholar] [CrossRef]
- Hattab, F.N.; Rawashdeh, M.A.; Fahmy, M.S. Impaction status of third molars in Jordanian students. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 1995, 79, 24–29. [Google Scholar] [CrossRef]
- Brown, L.H.; Berkman, S.; Cohen, D.; Kaplan, A.L.; Rosenberg, M. A radiological study of the frequency and distribution of impacted teeth. J. Dent. Assoc. S. Afr. 1982, 37, 627–630. [Google Scholar]
- Haidar, Z.; Shalhoub, S.Y. The incidence of impacted wisdom teeth in a Saudi community. Int. J. Oral Maxillofac. Surg. 1986, 15, 569–571. [Google Scholar] [CrossRef] [PubMed]
- Queck, S.L.; Tay, C.K.; Tay, K.H.; Toh, S.L.; Lim, K.C. Pattern of third molar impaction in a Singapore Chinese population: A retrospective radiographic survey. Int. J. Oral Maxillofac. Surg. 2003, 32, 548–552. [Google Scholar] [CrossRef]
- Hugoson, A.; Kugelberg, C.F. The prevalence of third molars in a Swedish population. An epidemiological study. Community Dent. Health 1988, 5, 121–138. [Google Scholar] [PubMed]
- Hashemipour, M.-A.; Tahmasbi-Arashlow, M.; Fahimi-Hanzaei, F. Incidence of impacted mandibular and maxillary third molars: A radiographic study in a Southeast Iran population. Med. Oral Patol. Oral Cir. Bucal 2013, 18, e140. [Google Scholar] [CrossRef]
- Izzetti, R.; Nisi, M.; Aringhieri, G.; Crocetti, L.; Graziani, F.; Nardi, C. Basic Knowledge and New Advances in Panoramic Radiography Imaging Techniques: A Narrative Review on What Dentists and Radiologists Should Know. Appl. Sci. 2021, 11, 858. [Google Scholar] [CrossRef]
- Deliverska, E.; Petkova, M. Complications after extraction of impacted third molars—Literature review. J. IMAB Annu. Proceeding Sci. Pap. 2016, 22, 1202–1211. [Google Scholar] [CrossRef]
- Sedaghatfar, M.; August, M.A.; Dodson, T.B. Panoramic radiographic findings as predictors of inferior alveolar nerve exposure following third molar extraction. J. Oral Maxillofac. Surg. 2005, 63, 3–7. [Google Scholar] [CrossRef]
- Anyanechi, C.E.; Saheeb, B.D.; Okechi, U.C. Is prophylactic removal of impacted mandibular third molar justified in all patients? A prospective clinical study of patients 50 years and above. Afr. Health Sci. 2019, 19, 1789–1794. [Google Scholar] [CrossRef]
- Krausz, A.A.; Machtei, E.E.; Peled, M. Effects of lower third molar extraction on attachment level and alveolar bone height of the adjacent second molar. Int. J. Oral Maxillofac. Surg. 2005, 34, 756–760. [Google Scholar] [CrossRef]
- Blakey, G.H.; Jacks, M.T.; Offenbacher, S.; Nance, P.E.; Phillips, C.; Haug, R.H.; White, R.P., Jr. Progression of periodontal disease in the second/third molar region in subjects with asymptomatic third molars. J. Oral Maxillofac. Surg. 2006, 64, 189–193. [Google Scholar] [CrossRef] [PubMed]
- McArdle, L.W.; McDonald, F.; Jones, J. Distal cervical caries in the mandibular second molar: An indication for the prophylactic removal of third molar teeth? Update. Br. J. Oral Maxillofac. Surg. 2014, 52, 185–189. [Google Scholar] [CrossRef] [PubMed]
- Glória, J.C.R.; Martins, C.C.; Armond, A.C.V.; Galvão, E.L.; Dos Santos, C.R.R.; Falci, S.G.M. Third Molar and Their Relationship with Caries on the Distal Surface of Second Molar: A Meta-analysis. J. Maxillofac. Oral Surg. 2018, 17, 129–141. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, J.C.; Gutekunst, C.-J.; Dagassan-Berndt, D.; Schmidlin, P.R.; Walter, C. Comparison of Two-Dimensional and Three-Dimensional Radiographs Using Clinically Relevant Parameters. Dent. J. 2019, 7, 50. [Google Scholar] [CrossRef] [PubMed]
- Walter, C.; Schmidt, J.C.; Rinne, C.A.; Mendes, S.; Dula, K.; Sculean, A. Cone beam computed tomography (CBCT) for diagnosis and treatment planning in periodontology: Systematic review update. Clin. Oral Investig. 2020, 24, 2943–2958. [Google Scholar] [CrossRef] [PubMed]
- Dula, K.; Benic, G.I.; Bornstein, M.; Dagassan-Berndt, D.; Filippi, A.; Hicklin, S.; Kissling-Jeger, F.; Luebbers, H.T.; Sculean, A.; Sequeira-Byron, P.; et al. SADMFR Guidelines for the Use of Cone-Beam Computed Tomography/Digital Volume Tomography. Swiss Dent. J. 2015, 125, 945–953. [Google Scholar] [CrossRef]
- Friedman, J.W. The prophylactic extraction of third molars: A public health hazard. Am. J. Public. Health 2007, 97, 1554–1559. [Google Scholar] [CrossRef]
- Fuster Torres, M.A.; Gargallo Albiol, J.; Berini Aytés, L.; Gay Escoda, C. Evaluation of the indication for surgical extraction of third molars according to the oral surgeon and the primary care dentist. Experience in the Master of Oral Surgery and Implantology at Barcelona University Dental School. Med. Oral Patol. Oral Cir. Bucal 2008, 13, E499–E504. [Google Scholar]
- AlHobail, S.Q.; Baseer, M.A.; Ingle, N.A.; Assery, M.K.; AlSanea, J.A.; AlMugeiren, O.M. Evaluation Distal Caries of the Second Molars in the Presence of Third Molars among Saudi Patients. J. Int. Soc. Prev. Community Dent. 2019, 9, 505–512. [Google Scholar] [CrossRef]
- Vranckx, M.; Fieuws, S.; Jacobs, R.; Politis, C. Prophylactic vs. symptomatic third molar removal: Effects on patient postoperative morbidity. J. Evid. Based Dent. Pract. 2021, 21, 101582. [Google Scholar] [CrossRef]
- Peretz, B.; Gotler, M.; Kaffe, I. Common errors in digital panoramic radiographs of patients with mixed dentition and patients with permanent dentition. Int. J. Dent. 2012, 2012, 584138. [Google Scholar] [CrossRef] [PubMed]
- Ramis-Alario, A.; Tarazona-Álvarez, B.; Peñarrocha-Diago, M.; Soto-Peñaloza, D.; Peñarrocha-Diago, M.; Peñarrocha-Oltra, D. Is periapical surgery follow-up with only two-dimensional radiographs reliable? A retrospective cohort type sensitivity study. Med. Oral Patol. Oral Cir. Bucal 2021, 26, e711–e718. [Google Scholar] [CrossRef] [PubMed]
- Cosola, S.; Toti, P.; Peñarrocha-Diago, M.; Covani, U.; Brevi, B.C.; Peñarrocha-Oltra, D. Standardization of the three-dimensional pose of cylindrical implants from intraoral radiographs: A preliminary study. BMC Oral Health 2021, 21, 100. [Google Scholar] [CrossRef] [PubMed]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. PLoS Med. 2009, 6, e1000100. [Google Scholar] [CrossRef] [PubMed]
- Tacconelli, E. CRD’s Guidance for Undertaking Reviews in Health Care. Lancet Infect. Dis. 2010, 10, 226. [Google Scholar] [CrossRef]
- Sideri, S.; Papageorgiou, S.N.; Eliades, T. Registration in the international prospective register of systematic reviews (PROSPERO) of systematic review protocols was associated with increased review quality. J. Clin. Epidemiol. 2018, 100, 103–110. [Google Scholar] [CrossRef] [PubMed]
- Aslam, S.; Emmanuel, P. Formulating a researchable question: A critical step for facilitating good clinical research. Indian J. Sex. Transm. Dis. AIDS 2010, 31, 47–50. [Google Scholar] [CrossRef]
- Munn, Z.; Barker, T.H.; Moola, S.; Tufanaru, C.; Stern, C.; McArthur, A.; Stephenson, M.; Aromataris, E. Methodological quality of case series studies: An introduction to the JBI critical appraisal tool. JBI Evid. Synth. 2020, 18, 2127–2133. [Google Scholar] [CrossRef]
- McHugh, M.L. Interrater reliability: The kappa statistic. Biochem. Med. 2012, 22, 276–282. [Google Scholar] [CrossRef]
- Dias, M.-J.; Franco, A.; Junqueira, J.-L.; Fayad, F.-T.; Pereira, P.-H.; Oenning, A.-C. Marginal bone loss in the second molar related to impacted mandibular third molars: Comparison between panoramic images and cone beam computed tomography. Med. Oral Patol. Oral Cir. Bucal 2020, 25, e395–e402. [Google Scholar] [CrossRef]
- Matzen, L.H.; Schropp, L.; Spin-Neto, R.; Wenzel, A. Radiographic signs of pathology determining removal of an impacted mandibular third molar assessed in a panoramic image or CBCT. Dentomaxillofac. Radiol. 2017, 46, 20160330. [Google Scholar] [CrossRef] [PubMed]
- Gupta, P.; Naik, S.R.; Ashok, L.; Khaitan, T.; Shukla, A.K. Prevalence of periodontitis and caries on the distal aspect of mandibular second molar adjacent to impacted mandibular third molar: A guide for oral health promotion. J. Fam. Med. Prim. Care 2020, 9, 2370–2374. [Google Scholar] [CrossRef]
- Tai, S.; Zhou, Y.; Pathak, J.L.; Piao, Z.; Zhou, L. The association of mandibular third molar impaction with the dental and periodontal lesions in the adjacent second molars. J. Periodontol. 2021, 92, 1392–1401. [Google Scholar] [CrossRef] [PubMed]
- Savitri, Y.; Saputra, D.; Damayanti, M. Pathological Abnormalities Due to Impaction of Third Molar Mandibular Horizontal and Mesioangular Angulation with Observation of Panoramic Radiography. Syst. Rev. Pharm. 2020, 11, 903–906. [Google Scholar]
- Ye, Z.-X.; Qian, W.-H.; Wu, Y.-B.; Yang, C. Pathologies associated with the mandibular third molar impaction. Sci. Prog. 2021, 104, 368504211013247. [Google Scholar] [CrossRef] [PubMed]
- Altan, A.; Akbulut, N. Does the Angulation of an Impacted Mandibular third Molar Affect the Prevalence of Preoperative Pathoses? J. Dent. 2019, 20, 48–52. [Google Scholar] [CrossRef]
- Shumar, A. Prevalence of impacted third molars and its associated pathologies among population in Sanaa city—Yemen. Int. Arab. J. Dent. 2020, 11, 100–104. [Google Scholar] [CrossRef]
- Cosola, S.; Kim, Y.S.; Park, Y.M.; Giammarinaro, E.; Covani, U. Coronectomy of Mandibular Third Molar: Four Years of Follow-Up of 130 Cases. Medicina 2020, 56, 654. [Google Scholar] [CrossRef]




| Checklist | Studies | |||||||
|---|---|---|---|---|---|---|---|---|
| Días et al. [40] | Matzen et al. [41] | Gupta et al. [42] | Tai et al. [43] | Savitri et al. [44] | Ye et al. [45] | Altan et al. [46] | Shumar et al. [47] | |
| Was the sample frame appropriate to address the target population? | YES | YES | * UN | YES | YES | YES | YES | YES |
| Were study participants sampled in an appropriate way? | YES | UN | UN | UN | UN | UN | UN | UN |
| Was the sample size adequate? | YES | YES | UN | YES | UN | UN | UN | UN |
| Were the study subjects and the setting described in detail? | YES | YES | YES | YES | YES | YES | YES | YES |
| Was the data analysis conducted with sufficient coverage of the identified sample? | YES | YES | YES | YES | YES | YES | YES | YES |
| Were valid methods used for the identification of the condition? | YES | YES | YES | YES | YES | YES | YES | YES |
| Was the condition measured in a standard, reliable way for all participants? | YES | YES | YES | YES | YES | YES | YES | YES |
| Was there appropriate statistical analysis? | YES | YES | YES | YES | YES | YES | YES | YES |
| Was the response rate adequate, and if not, was the low response rate managed appropriately? | YES | YES | YES | YES | YES | YES | YES | YES |
| Author & Year | Diagnostic Tool | Study Design | Study Type | Sample Size | Bone Loss% | QAT | Rob |
|---|---|---|---|---|---|---|---|
| Días et al. 2020 [40] | OPG and CBCT | Retrospective | Observational–analytical | 70 patients 124 MTMI * | OPG 62.9% CBCT 80% | JBI critical appraisal checklist | Low 100% |
| Matzen et al. 2017 [41] | OPG and CBCT | Retrospective | Observational–analytical | 379 MTMI | OPG 66% CBCT 85% | JBI critical appraisal checklist | Low 88% |
| Gupta et al. 2020 [42] | OPG | Retrospective | Prevalence | 400 patients | 39% | JBI critical appraisal checklist | Moderate 66% |
| Tai et al. 2020 [43] | OPG | Retrospective | Prevalence | 2650 MTMI | 35.30% | JBI critical appraisal checklist | Low 88% |
| Savitri et al. 2020 [44] | OPG | Retrospective | Prevalence | 53 OPGs | 33.3% | JBI critical appraisal checklist | Moderate 77% |
| Ye et al. 2021 [45] | Clinical and OPG | Retrospective | Prevalence | 262 patients 432 MTMI | 14.81% | JBI critical appraisal checklist | Moderate 77% |
| Altan et al. 2019 [46] | OPG | Retrospective | Prevalence | 954 patients 1598 MTMI | 4.9% | JBI critical appraisal checklist | Moderate 77% |
| Shumar et al. [47] | OPG | Retrospective | Prevalence | 1900 OPGs | 6.8% | JBI critical appraisal checklist | Moderate 77% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Assiri, H.; Estrugo-Devesa, A.; Roselló-Llabrés, X.; Egido-Moreno, S.; López-López, J. The Accuracy of Bone Assessment Distal to Lower Second Molars Using Panoramic Radiography: A Systematic Review and Meta-Analysis. Dent. J. 2024, 12, 73. https://doi.org/10.3390/dj12030073
Assiri H, Estrugo-Devesa A, Roselló-Llabrés X, Egido-Moreno S, López-López J. The Accuracy of Bone Assessment Distal to Lower Second Molars Using Panoramic Radiography: A Systematic Review and Meta-Analysis. Dentistry Journal. 2024; 12(3):73. https://doi.org/10.3390/dj12030073
Chicago/Turabian StyleAssiri, Hassan, Albert Estrugo-Devesa, Xavier Roselló-Llabrés, Sonia Egido-Moreno, and José López-López. 2024. "The Accuracy of Bone Assessment Distal to Lower Second Molars Using Panoramic Radiography: A Systematic Review and Meta-Analysis" Dentistry Journal 12, no. 3: 73. https://doi.org/10.3390/dj12030073
APA StyleAssiri, H., Estrugo-Devesa, A., Roselló-Llabrés, X., Egido-Moreno, S., & López-López, J. (2024). The Accuracy of Bone Assessment Distal to Lower Second Molars Using Panoramic Radiography: A Systematic Review and Meta-Analysis. Dentistry Journal, 12(3), 73. https://doi.org/10.3390/dj12030073