Extrusive Luxation Injuries in Young Patients: A Retrospective Study with 5-Year Follow-Up
Abstract
:1. Introduction
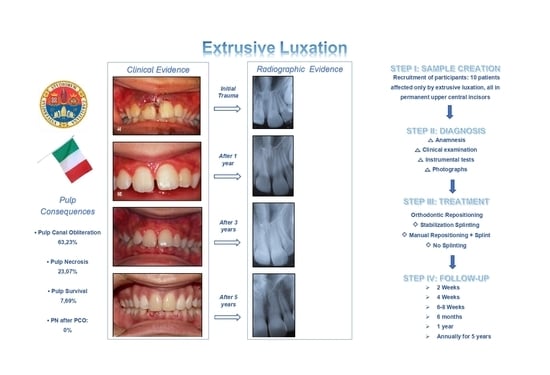
2. Materials and Methods
- Patients who had at least one permanent incisor presenting only extrusive luxation;
- Patients who were followed up continuously for at least 5 years.
- Patients who had suffered a previous trauma before the event and/or presented carious lesions;
- Patients in whom the trauma caused uncomplicated or complicated lesions to the hard tissue of the extruded teeth;
- Patients who suffered further traumatic injuries during the follow-up period;
- Patients with ongoing orthodontic therapy.
2.1. Management of Extrusions
2.2. Statistical Analysis
- PCs and mm of extrusion;
- PCs and time to treatment (in hours).
- c.
- PCs and mm of extrusion categorized into three classes (mild, moderate, severe);
- d.
- PCs and stage of maturation of the root apex (open apex (OA) and closed apex (CA));
- e.
- PCs and type of splinting (stabilization, orthodontic repositioning);
- f.
- PCs and crown color changes.
3. Results
3.1. General Data of the Selected Patients
3.2. Severity of the Extrusion
3.3. Time to Treatment
3.4. Orthodontic Repositioning, Splinting and Treatment Time
3.5. Pulp Consequences
3.5.1. Pulp Canal Obliteration
3.5.2. Pulp Necrosis
3.6. Pulp Sensitivity and Crown Color Changes
3.7. Further Dental Traumas and Orthodontic Therapies
4. Discussion
4.1. The Influence of the Initial Therapeutic Approach (Especially the Use of the Orthodontic Splint) on the Development of PN and PCO
4.2. Onset Times and Frequency of PN and PCO with Respect to the Severity of the Extrusion
4.3. Frequency of Onset Times of PN and PCO with Respect to the Root Maturity of Traumatized Teeth
4.4. Frequency of Onset of PN in Teeth already Affected by PCO
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
Ethical Approval
References
- Soriano, E.P.; Caldas, A.F., Jr.; Carvalho, M.V.D.; Amorim Filho, H.A. Prevalence and risk factors related to traumatic dental injuries. Dent. Traumatol. 2007, 23, 232–240. [Google Scholar] [CrossRef]
- Traebert, J.; Bittencourt, D.D.; Peres, K.G.; Peres, M.A.; De Lacerda, J.T.; Marcenes, W. Aetiology and rates of treatment of traumatic dental injuries among 12-year-old school children in a town in southern Brazil. Dent. Traumatol. 2006, 22, 173–178. [Google Scholar] [CrossRef]
- Schatz, J.-P.; Hakeberg, M.; Ostini, E.; Kiliaridis, S. Prevalence of traumatic injuries to permanent dentition and its association with overjet in a Swiss child population. Dent. Traumatol. 2013, 29, 110–114. [Google Scholar] [CrossRef]
- Glendor, U.; Halling, A.; Andersson, L.; Eilert-Petersson, E. Incidence of traumatic tooth injuries in children and adolescents in the county of Västmanland, Sweden. Swed. Dent. J. 1996, 20, 15–28. [Google Scholar]
- Andreasen, J.O. Luxation of permanent teeth due to trauma A clinical and radiographic follow-up study of 189 injured teeth. Eur. J. Oral Sci. 1970, 78, 273–286. [Google Scholar] [CrossRef]
- Andreasen, F.M.; Andreasen, J.O. Diagnosis of luxation injuries: The importance of standardized clinical, radiographic and photographic techniques in clinical investigations. Dent. Traumatol. 1985, 1, 160–169. [Google Scholar] [CrossRef] [PubMed]
- Andreasen, J.O.; Andreasen, F.M.; Backland, L.K.; Flores, M.T. Traumatic Dental Injuries—A Manual, 1st ed.; Munksgaard: Copenhagen, Denmark, 1999. [Google Scholar]
- Andreasen, J.O.; Andreasen, F.M.; Andersson, L. Extrusive Luxation and Lateral Luxation. In Textbook and Color Atlas of Traumatic Injuries to the Teeth, 4th ed.; Wiley-Blackwell: Copenhagen, Denmark, 2007; pp. 411–427. [Google Scholar]
- Lauridsen, E.; Hermann, N.V.; Gerds, T.A.; Ahrensburg, S.S.; Kreiborg, S.; Andreasen, J.O. Combination Injuries 3. The risk of pulp necrosis in permanent teeth with extrusion or lateral luxation and concomitant crown fractures without pulp exposure. Dent. Traumatol. 2012, 28, 379–385. [Google Scholar] [CrossRef] [PubMed]
- Andreasen, J.O.; Andreasen, J.; Andreasen, F.; Skeie, A.; Hjørting-Hansen, E.; Schwartz, O. Effect of treatment delay upon pulp and periodontal healing of traumatic dental injuries—A review article. Dent. Traumatol. 2002, 18, 116–128. [Google Scholar] [CrossRef] [PubMed]
- Bourguignon, C.; Cohenca, N.; Lauridsen, E.; Flores, M.T.; O’Connell, A.C.; Day, P.F.; Tsilingaridis, G.; Abbott, P.V.; Fouad, A.; Hicks, L.; et al. International Association of Dental Traumatology guidelines for the management of traumatic dental injuries: 1. Fractures and luxations. Dent. Traumatol. 2020, 36, 314–330. [Google Scholar] [CrossRef]
- Andreasen, F.M.; Zhjie, Y.; Thomsen, B.L.; Andersen, P.K. Occurrence of pulp canal obliteration after luxation injuries in the permanent dentition. Dent. Traumatol. 1987, 3, 103–115. [Google Scholar] [CrossRef] [PubMed]
- Andreasen, F.M.; Pedersen, B.V. Prognosis of luxated permanent teeth--the development of pulp necrosis. Endod. Dent. Traumatol. 1985, 1, 207–220. [Google Scholar] [CrossRef] [PubMed]
- Hecová, H.; Tzigkounakis, V.; Merglova, V.; Netolický, J. A retrospective study of 889 injured permanent teeth. Dent. Traumatol. 2010, 26, 466–475. [Google Scholar] [CrossRef] [PubMed]
- Oikarinen, K.; Gundlach, K.K.H.; Pfeifer, G. Late complications of luxation injuries to teeth. Dent. Traumatol. 1987, 3, 296–303. [Google Scholar] [CrossRef] [PubMed]
- Andreasen, J.O. Etiology and pathogenesis of traumatic dental injuries A clinical study of 1298 cases. Eur. J. Oral Sci. 1970, 78, 329–342. [Google Scholar] [CrossRef] [PubMed]
- Lee, R.; Barrett, E.J.; Kenny, D.J. Clinical outcomes for permanent incisor luxations in a pediatric population. II. Extrusions. Dent. Traumatol. 2003, 19, 274–279. [Google Scholar] [CrossRef]
- Lin, S.; Pilosof, N.; Karawani, M.; Wigler, R.; Kaufman, A.Y.; Teich, S.T. Occurrence and timing of complications following traumatic dental injuries: A retrospective study in a dental trauma department. J. Clin. Exp. Dent. 2016, 8, e429–e436. [Google Scholar] [CrossRef]
- Lima, T.F.R.; Nagata, J.Y.; De Souza-Filho, F.J.; de Jesus Soares, A. Post-traumatic Complications of Severe Luxations and replanted Teeth. J. Contemp. Dent. Pract. 2015, 16, 13–19. [Google Scholar] [CrossRef]
- Grossman, L.I. Intentional replantation of teeth. J. Am. Dent. Assoc. 1966, 72, 1111–1118. [Google Scholar] [CrossRef]
- Sübay, R.K.; Kayataş, M.; Caniklioğlu, C. Delayed multidisciplinary management of an extrusively luxated maxillary central incisor. Dent. Traumatol. 2007, 23, 82–84. [Google Scholar] [CrossRef]
- De Toubes, K.M.S.; De Oliveira, P.A.D.; Machado, S.N.; Pelosi, V.; Nunes, E.; Silveira, F. Clinical Approach to Pulp Canal Obliteration: A Case Series. Iran. Endod. J. 2017, 12, 527–533. [Google Scholar]
- Amaral, M.F.; de Almeida, M.M.; de Faria, L.P.; Brandini, D.A.; Poi, W.R.; Okamoto, R. Treatment of extrusive luxation in permanent teeth: Literature review with systematic criteria. J. Contemp. Dent. Pract. 2017, 18, 241–245. [Google Scholar] [PubMed]
- Flores, M.T.; Andersson, L.; Andreasen, J.O.; Bakland, L.K.; Malmgren, B.; Barnett, F.; Bourguignon, C.; DiAngelis, A.; Hicks, L.; Sigurdsson, A.; et al. Guidelines for the management of traumatic dental injuries. I. Fractures and luxations of permanent teeth. Dent. Traumatol. 2007, 23, 66–71. [Google Scholar] [CrossRef] [PubMed]
- DiAngelis, A.J.; Andreasen, J.O.; Ebeleseder, K.A.; Kenny, D.J.; Trope, M.; Sigurdsson, A.; Andersson, L.; Bourguignon, C.; Flores, M.T.; Hicks, M.L.; et al. International Association of Dental Traumatology guidelines for the management of traumatic dental injuries: 1. Fractures and luxations of permanent teeth. Dent. Traumatol. 2012, 28, 2–12. [Google Scholar] [CrossRef] [PubMed]
- Landis, J.R.; Koch, G.G. An Application of Hierarchical Kappa-type Statistics in the Assessment of Majority Agreement among Multiple Observers. Biometrics 1977, 33, 363. [Google Scholar] [CrossRef]
- Andreasen, F.M.; Kahler, B. Diagnosis of acute dental trauma: The importance of standardized documentation: A review. Dent. Traumatol. 2015, 31, 340–349. [Google Scholar] [CrossRef]
- Spinas, E.; Mameli, A.; Giannetti, L. Traumatic Dental Injuries Resulting from Sports Activities; Immediate Treatment and Five Years Follow-Up: An Observational Study. Open Dent. J. 2018, 12, 1–10. [Google Scholar] [CrossRef]
- World Health Organization. Application of the International Classification of Dental Disease to Dentistry and Stomatology ICD-DA, 3rd ed.; WHO: Geneva, Switzerland, 2007. [Google Scholar]
- Moorrees, C.F.; Fanning, E.A.; Hunt, E.E. Age Variation of Formation Stages for Ten Permanent Teeth. J. Dent. Res. 1963, 42, 1490–1502. [Google Scholar] [CrossRef] [PubMed]
- Weine, F.S. The Case Against Intentional Replantation. J. Am. Dent. Assoc. 1980, 100, 664–668. [Google Scholar] [CrossRef]
- Camp, J.H. Diagnosis and management of sports-related injuries to the teeth. Dent. Clin. N. Am. 1991, 35, 733–756. [Google Scholar] [PubMed]
- Spinas, E.; Generali, L.; Mameli, A.; Demontis, C.; Martinelli, D.; Giannetti, L. Delayed tooth replantation and inflammatory root resorption in childhood and adolescence. J. Biol. Regul. Homeost. Agents 2019, 33, 623–627. [Google Scholar]
- Spinas, E. A biological conservative approach to complex traumatic dento-alveolar lesions. J. Clin. Pediatr. Dent. 2003, 28, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Ebeleseder, K.A.; Glockner, K.; Pertl, C.; Stadtler, P. Splints made of wire and composite: An investigation of lateral tooth mobility in vivo. Dent. Traumatol. 1995, 11, 288–293. [Google Scholar] [CrossRef] [PubMed]
- American Association of Endodontists. The Recommended Guidelines of the American Association of Endodontists for The Treatment of Traumatic Dental Injuries; Revised (2013); American Association of Endodontists: Chicago, IL, USA, 2013. [Google Scholar]
- Bastos, J.V.; Côrtes, M.I.D.S. Pulp canal obliteration after traumatic injuries in permanent teeth—Scientific fact or fiction? Braz. Oral Res. 2018, 32, e75. [Google Scholar] [CrossRef] [Green Version]
- Trope, M. Root Resorption due to Dental Trauma. Endod. Top. 2002, 1, 79–100. [Google Scholar] [CrossRef] [Green Version]
- Spinas, E.; Giannetti, L.; Mameli, A.; Re, D. Dental injuries in young athletes, a five-year follow-up study. Eur. J. Paediatr. Dent. 2018, 19, 187–193. [Google Scholar] [PubMed]
- Bauss, O.; Röhling, J.; Schwestka-Polly, R. Prevalence of traumatic injuries to the permanent incisors in candidates for orthodontic treatment. Dent. Traumatol. 2004, 20, 61–66. [Google Scholar] [CrossRef] [PubMed]
- Kahler, B.; Heithersay, G.S. An evidence-based appraisal of splinting luxated, avulsed and root-fractured teeth. Dent. Traumatol. 2008, 24, 2–10. [Google Scholar] [CrossRef]
- Ebrahim, F.-H.; Kulkarni, G. Fixed orthodontic appliances in the management of severe dental trauma in mixed dentition: A case report. J. Can. Dent. Assoc. 2013, 79, d131. [Google Scholar]
- Fields, H.W.; Christensen, J.R. Orthodontic Procedures after Trauma. J. Endod. 2013, 39, S78–S87. [Google Scholar] [CrossRef]
- Elbay, Ü.Ş.; Baysal, A.; Elbay, M.; Saridag, S.; Sarıdağ, S. Multidisciplinary Approach to Delayed Treatment of Traumatic Teeth Injuries Involving Extrusive Luxation, Avulsion and Crown Fracture. Oper. Dent. 2014, 39, 566–571. [Google Scholar] [CrossRef]
- Kindelan, S.A.; Day, P.F.; Kindelan, J.D.; Spencer, J.R.; Duggal, M.S. Dental trauma: An overview of its influence on the management of orthodontic treatment. Part 1. J. Orthod. 2008, 35, 68–78. [Google Scholar] [CrossRef] [PubMed]
- Van Gorp, G.; Bormans, N.; Vanham, I.; Willems, G.; Declerck, D. Orthodontic treatment recommendation and expected adverse reactions in patients with a history of dental trauma: A survey among general dentists, paediatric dentists, and orthodontic specialists. Int. J. Paediatr. Dent. 2020, 30, 360–369. [Google Scholar] [CrossRef]
- Sandler, C.; Barry, S.; Littlewood, S.; Al-Musfir, T.; Nazzal, H. Orthodontic management of traumatized teeth: A national survey of UK orthodontists. Dent. Traumatol. 2019, 35, 241–250. [Google Scholar] [CrossRef] [PubMed]
- McCabe, P.S.; Dummer, P.M.H. Pulp canal obliteration: An endodontic diagnosis and treatment challenge. Int. Endod. J. 2012, 45, 177–197. [Google Scholar] [CrossRef] [PubMed]
- Bauss, O.; Röhling, J.; Rahman, A.; Kiliaridis, S. The Effect of Pulp Obliteration on Pulpal Vitality of Orthodontically Intruded Traumatized Teeth. J. Endod. 2008, 34, 417–420. [Google Scholar] [CrossRef]
- Kvinnsland, S.; Heyeraas, K.; Ofjord, E.S. Effect of experimental tooth movement on periodontal and pulpal blood flow. Eur. J. Orthod. 1989, 11, 200–205. [Google Scholar] [CrossRef]
- Derringer, K.A.; Jaggers, D.C.; Linden, R.W.A. Angiogenesis in human dental pulp following orthodontic tooth movement. J. Dent. Res. 1996, 75, 1761–1766. [Google Scholar] [CrossRef]
- Vandevska-Radunovic, V.; Kristiansen, A.B.; Heyeraas, K.J.; Kvinnsland, S. Changes in blood circulation in teeth and supporting tissues incident to experimental tooth movement. Eur. J. Orthod. 1994, 16, 361–369. [Google Scholar] [CrossRef]
- Yu, C.; Abbott, P.V. Responses of the pulp, periradicular and soft tissues following trauma to the permanent teeth. Aust. Dent. J. 2016, 61, 39–58. [Google Scholar] [CrossRef]
- Feiglin, B. Dental pulp response to traumatic injuries—A retrospective analysis with case reports. Dent. Traumatol. 1996, 12, 1–8. [Google Scholar] [CrossRef]
- Spinas, E.; Deias, M.; Mameli, A.; Giannetti, L. Pulp Canal Obliteration after Extrusive and Lateral Luxation in Young Permanent Teeth: A Scoping Review. Eur J Paediatr Dent. 2020, 21. in press. [Google Scholar]




| Covariate | Association with PC’s | Test Used |
|---|---|---|
| mm of extrusion (cat.) | p-value = 0.727 | Fisher’s exact test |
| Time to treatment | p-value = 0.060 * | Mann–Whitney test |
| Stage of apical maturation | p-value = 0.236 | Fisher’s exact test |
| Type of splinting | p-value = 0.345 | Fisher’s exact test |
| Crown color change | p-value = 0.318 | Fisher’s exact test |
| Patient | Gender | Age | Affected Tooth | Etiology | Root Development |
|---|---|---|---|---|---|
| C. | F | 9 years | 1.1 | Domestic | OA |
| 2.1 | Domestic | OA | |||
| B. | M | 8 years | 1.1 | Sport | OA |
| L. | M | 14 years | 1.1 | Sport | CA |
| N. | M | 16 years | 1.1 | Assault | CA |
| S. | F | 16 years | 1.1 | Domestic | CA |
| 2.1 | Domestic | CA | |||
| C. | M | 10 years | 1.1 | Sport | OA |
| 2.1 | Sport | OA | |||
| M. | M | 10 years | 1.1 | Sport | OA |
| P. | F | 8 years | 2.1 | Domestic | OA |
| G. | F | 12 years | 2.1 | Sport | CA |
| S. | F | 9 years | 1.1 | Sport | OA |
| Patient | Tooth | Apex | Severity of Extrusion | Time to Treatment (Hours) | Treatment | Onset of PCO (Years from Trauma) | Completion of PCO (Years from Trauma) | PN | Sensitivity at Baseline | Sensitivity over Time | Loss of Sensitivity (Time from Trauma) | Crown Color Change (Time from Trauma) | PN after PCO | Other Treatments |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| C. | 11 | OA | 3mm Moderate | 8 | Manual repositioning and stabilization splinting | 1 | 5 | No | Absent | Reduced at 1year | 3 years | 1–2 years | No | No |
| 21 | OA | 2mm Mild | 8 | 1 | 5 | No | Light | Slight | 3 years | 1–2 years | No | No | ||
| B. | 11 | OA | 5mm Moderate | 10 | Orthodontic repositioning | 1 | 5 | No | Absent | Reduced at 1year | 3 years | Within 1 year | No | No |
| L. | 11 | CA | 3 mm Moderate | 10 | Manual repositioning | 1 | 5 | No | Slight | Reduced at 6 months | 3 years | 2 years | No | No |
| N. | 11 | CA | 4 mm Moderate | 18 | Orthodontic repositioning | No PCO | No PCO | Within 1 yr | Slight | Slight | 1 year | Within 1 year | No | No |
| S. | 21 1.1 | CA CA | 2 mm Mild 4mm Moderate | 10 10 | Orthodontic repositioning Orthodontic repositioning | No PCO No PCO | No PCO No PCO | 6 months No PN | Slight Present | Slight Present | 4 months - | Within 1 year No | No Healed | No No |
| C. | 1.1 | OA | 5 mm Moderate | 4 | Orthodontic repositioning | 1 | 5 | No | Absent | Reduced at 1 year | 3 years | 2 years | No | No |
| 2.1 | OA | 2 mm Mild | 4 | Orthodontic repositioning | 1 | 5 | No | Slight | Slight | 3 years | 2 years | No | No | |
| M. | 1.1 | OA | 6 mm Severe | 24 | Stabilization splinting | No PCO | No PCO | Yes (within 1yr) | Absent | Absent | Absent | 3 years | IRR at 3 years | Started ortho after 1year |
| P. | 2.1 | OA | 2 mm Mild | 24 | No treatment | 1 | 5 | No | Slight | Reduced at 1 year | 3 years | 3 years | No | No |
| G. | 2.1 | CA | 6 mm Severe | 3 | Orthodontic repositioning | 1 | 5 | No | Absent | Reduced at 1 year | 1 year | Within 1 year | No | No |
| S. | 1.1 | OA | 3 mm Moderate | 8 | Stabilization splinting | 1 | 5 | No | Slight | Reduced at 1 year | 1 year | 1–2 years | No | No |
| PCO | PN | Healed | |
|---|---|---|---|
| Severity of Extrusion | |||
| Mild extrusion | I I I | I | |
| Moderate extrusion | I I I I I | I | I |
| Severe extrusion | I | I | |
| Total | 9 | 3 | 1 |
| Type of splinting | |||
| Repositioning splinting | I I I I | I I | I |
| Stabilization splinting | I I I | I | |
| No splinting | I I | ||
| Total | 9 | 3 | 1 |
| Time to treatment | |||
| <4 h | I I I | I | |
| 5 to 12 h | I I I I I | I | |
| 13 to 18 h | I | I | |
| 19 to 24 h | I | ||
| Total | 9 | 3 | 1 |
| Authors | Elbay et al. 2014 | Ebrahin and Kulkarni 2013 | Subay et al. 2007 |
|---|---|---|---|
| General information | Twelve years, male, tooth 11. The tooth was treated 20 days post-trauma. Eleven presented open apex, periapical disease, absence of pulp vitality and increased periodontal ligament space without root and bone fracture. | Seven years, male, tooth 12. The tooth was treated 14 days post-trauma. Extrusion of about 5 mm with palatal displacement. Mobility grade III. The tooth was vital and asymptomatic without pathological radiographic signs. Early stage of root development. | Thirteen years, male, tooth 11. The tooth was treated 30 days post-trauma. Mobility grade I, palatal displacement. Presence of premature occlusal contact. The tooth was not vital and radiography showed an increased periodontal ligament space. |
| Treatment | Orthodontic intrusion and calcium hydroxide apexogenesis | Orthodontic intrusion and debridement of granulation tissue and suture to promote primary wound closure. | Orthodontic intrusion and root canal treatment (CH for 1 week), after which the tooth was filled with gutta-percha. |
| Duration of treatment | Intrusion was obtained in 3 months. After a further 3 months the tooth was filled with gutta-percha. | Intrusion was obtained in 19 months. | Intrusion was obtained in 4 months with a removable appliance. |
| Outcomes | Periapical healing, no pathological radiographic or clinical signs. | Continued root development, no pathological radiographic or clinical signs. Normal pulp vitality was conserved. | The tooth appeared normal clinically and radiographically after 1 year. |
| Samples | Teeth | PCO | PN | PS | PN after PCO | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| N % | N % | N % | N % | N % | ||||||
| Andreasen et al., 1987 | 48 | 22 | 45.83 | 13 | 27.08 | 13 | 27.08 | 1 | 2.08 | |
| 31 OA | 64.58 OA | 19 OA | 39.58 OA | 2 OA | 4.16 OA | 10 OA | 20.83 OA | |||
| 17 CA | 35.42 CA | 3 CA | 6.25 CA | 11 CA | 22.92 CA | 3 CA | 6.25 CA | |||
| Lee et al., 2003 * | 55 | 19 | 34.54 | 23 | 41.81 | 6 | 10.90 | 2 | 3.63 | |
| 24 OA | 43.6 OA | 16 OA | 29.09 OA | 11 OA | 20.00 OA | |||||
| 31 CA | 56.36 CA | 3 CA | 5.45 CA | 12CA | 21.81CA | |||||
| Hecova et al., 2010 ** | 89 | 12 | 13.48 | 26 | 29.21 | 49 | 55.05 | NS | NS | |
| 8 OA | 8.99 OA | 5 OA | 5.61 OA | 2 OA | 2.24 OA | 1 OA | 1.12 OA | |||
| 81 CA | 91.01 CA | 7 CA | 7.86 CA | 24 CA | 26.96 CA | 48 CA | 53.93 CA | |||
| Total | 191 | 53 | 27.74 | 62 | 32.46 | 62 | 32.46 | 3 | 1.57 | |
| 63OA | 32.98 OA | 40 OA | 75.47 OA | 15 OA | 24.19 OA | 11 OA | 5.75 OA | |||
| 129CA | 67.02 CA | 13 CA | 24.53 CA | 47 CA | 75.81 CA | 51 CA | 26.70 CA | |||
| Current study | 13 | 9 | 69.23 | 3 | 23.07 | 1 | 7.69 | 0 | 0 | |
| 8 OA | 61.54 OA | 7 OA | 77.77 OA | 1 OA | 33.34 OA | 0 OA | 0 OA | |||
| 5 CA | 38.46 CA | 2 CA | 22.23 CA | 2 CA | 66.66 CA | 1 CA | 100 CA | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Spinas, E.; Pipi, L.; Dettori, C. Extrusive Luxation Injuries in Young Patients: A Retrospective Study with 5-Year Follow-Up. Dent. J. 2020, 8, 136. https://doi.org/10.3390/dj8040136
Spinas E, Pipi L, Dettori C. Extrusive Luxation Injuries in Young Patients: A Retrospective Study with 5-Year Follow-Up. Dentistry Journal. 2020; 8(4):136. https://doi.org/10.3390/dj8040136
Chicago/Turabian StyleSpinas, Enrico, Laura Pipi, and Claudia Dettori. 2020. "Extrusive Luxation Injuries in Young Patients: A Retrospective Study with 5-Year Follow-Up" Dentistry Journal 8, no. 4: 136. https://doi.org/10.3390/dj8040136
APA StyleSpinas, E., Pipi, L., & Dettori, C. (2020). Extrusive Luxation Injuries in Young Patients: A Retrospective Study with 5-Year Follow-Up. Dentistry Journal, 8(4), 136. https://doi.org/10.3390/dj8040136