Increased Knowledge of Adult-Onset Dystonia Amongst Medical Students via Brief Video Education: A Systematic Review and Cohort Study
Abstract
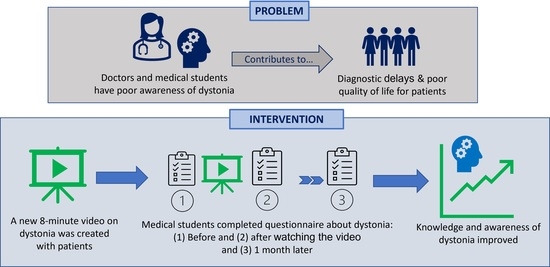
:1. Introduction
2. Materials and Methods
2.1. Systematic Review
2.1.1. Inclusion and Exclusion Criteria
2.1.2. Scoping and Literature Search
2.2. Medical Student Cohort Study
2.2.1. Brief Video Intervention
2.2.2. Data Collection—Questionnaires
2.2.3. Recruitment
Medical Students
Patients
2.2.4. Ethical Approval
2.2.5. Statistical Analysis
3. Results
3.1. Systematic Review
3.2. Cohort Study
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| LTHT | Leeds Teaching Hospitals NHS Trust |
| PD | Parkinson’s disease |
| MCQs | Multiple Choice Questions |
| UoL | University of Leeds |
| BQ | Baseline Questionnaire |
| IRQ | Immediate-recall Questionnaire |
| DRQ | Delayed-recall Questionnaire |
| SoM | School of Medicine |
| IRAS | Integrated Research Application System |
| ANOVA | Analysis of Variance |
| PRISMA | Preferred Reporting Items for Systematic Reviews and Meta-Analyses |
| SD | Standard Deviation |
| MBChB | Bachelor of Medicine and Surgery |
Appendix A
Appendix A.1. Part 1 of Questionnaire (Relating to the Student’s Demographics and Prior Exposure to Dystonia)
- What year are you in?
- (a)
- 1
- (b)
- 2
- (c)
- 3
- (d)
- 4
- (e)
- 5
- (f)
- Intercalation year
- What is your age group?
- (a)
- <22
- (b)
- 22–25
- (c)
- >25
- Are you a home (UK/EU) or international student?
- (a)
- Home (UK/EU)
- (b)
- International
- Are you a transfer student?
- (a)
- Yes
- (b)
- No
- Are you a post-graduate student? If yes, what did you study for your undergraduate degree?
- (a)
- Yes; I studied…
- (b)
- No
- Which of the following subject areas did you intercalate in, if any?
- (a)
- Neurology
- (b)
- Neuroscience
- (c)
- Other subject area
- (d)
- I am in Y5 now and did not intercalate
- (e)
- I am in Y1–4, have not intercalated yet, but intend to
- (f)
- I am in Y1–4, have not intercalated yet, and don’t intend to
- What are your career aspirations?
- (a)
- General Practice
- (b)
- Psychiatry
- (c)
- Neurology
- (d)
- Neurosurgery
- (e)
- Medicine, other than Neurology
- (f)
- Surgery, other than Neurosurgery
- (g)
- I am not sure yet
- Have you heard of dystonia before?
- (a)
- Yes
- (b)
- No
- (c)
- Unsure
- Have you ever received any teaching (formal or informal) on dystonia?
- (a)
- Yes
- (b)
- No
- Have you ever seen a patient with dystonia, or heard of dystonia being included in a differential diagnosis?
- (a)
- Yes
- (b)
- No
- On a scale of 1–5, how confident do you feel in being able to recognise dystonia in a patient?
- (a)
- 1 (not confident at all)
- (b)
- 2
- (c)
- 3
- (d)
- 4
- (e)
- 5 (very confident)
Appendix A.2. Part 2 of Questionnaire (Multiple Choice Questions Utilised in the Study)
| Multiple Choice Question | Answer Options |
| 1. What is dystonia? |
|
| 2. Which of the following is the correct description of a sensory trick? |
|
| 3. Which of the following is NOT an example of a task-specific dystonia? |
|
| 4. What is Meige syndrome? |
|
| 5. You are a foundation doctor working in A + E. Whilst clerking a patient who has come in with an eye problem, you notice that his head is twisted to the right and he struggles to fully move his head to face you when you move to stand on his left. Which of the following conditions is he most likely to have? |
|
| 6. Which of the following is NOT a type of cervical dystonia? |
|
| 7. Which symptom is NOT usually associated with dystonia? |
|
| 8. What is/are the most common type(s) of dystonia? |
|
| 9. If dystonia is suspected, who should the patient be referred to for a definitive diagnosis? |
|
| 10. What is the prevalence of dystonia in the UK? |
|
| 11. True or false: In the UK, Parkinson’s disease is more common than dystonia? |
|
| 12. Is it possible to inherit dystonia? |
|
| 13. Dystonia can occur alongside which neurological condition? |
|
| 14. You are a FY2 on your first day at your GP rotation. A 27-year-old woman comes into your afternoon clinic with a two-year history of tremors in her right hand. She mentions she works as an administrative assistant in a busy office and her tremor is typically brought on after long periods of writing. She has no other symptoms and no family history of movement disorders. Which diagnostic tools will you utilise to reach diagnosis? |
|
| 15. Which of the following is true? |
|
References
- Albanese, A.; Bhatia, K.; Bressman, S.; DeLong, M.; Fahn, S.; Fung, V.; Hallett, M.; Jankovic, J.; Jinnah, H.A.; Klein, C.; et al. Phenomenology and classification of dystonia: A consensus update. Mov. Disord. 2013, 28, 863–873. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Steeves, T.; Day, L.; Dykeman, J.; Jette, N.; Pringsheim, T. The prevalence of primary dystonia: A systematic review and meta-analysis. Mov. Disord. 2012, 27, 1789–1796. [Google Scholar] [CrossRef] [PubMed]
- Cloud, L.; Jinnah, H. Treatment strategies for dystonia. Expert Opin. Pharmacother. 2009, 11, 5–15. [Google Scholar] [CrossRef] [PubMed]
- Berman, B.; Groth, C.; Sillau, S.; Pirio Richardson, S.; Norris, S.; Junker, J.; Brüggemann, N.; Agarwal, P.; Barbano, R.L.; Espay, A.J.; et al. Risk of spread in adult-onset isolated focal dystonia: A prospective international cohort study. J. Neurol. Neurosurg. Psychiatry 2019, 91, 314–320. [Google Scholar] [CrossRef] [Green Version]
- Kuyper, D.; Parra, V.; Aerts, S.; Okun, M.; Kluger, B. Nonmotor manifestations of dystonia: A systematic review. Mov. Disord. 2011, 26, 1206–1217. [Google Scholar] [CrossRef] [Green Version]
- Tinazzi, M.; Erro, R.; Mascia, M.; Esposito, M.; Ercoli, T.; Ferrazzano, G.; Di Biasio, F.; Pellicciari, R.; Eleopra, R.; Bono, F.; et al. Demographic and clinical determinants of neck pain in idiopathic cervical dystonia. J. Neural Transm. 2020, 127, 1435–1439. [Google Scholar] [CrossRef]
- Defazio, G.; Ercoli, T.; Erro, R.; Pellicciari, R.; Mascia, M.M.; Fabbrini, G.; Albanese, A.; Lalli, S.; Eleopra, R.; Barone, P.; et al. Idiopathic Non-task-Specific Upper Limb Dystonia, a Neglected Form of Dystonia. Mov. Disord. 2020, 35, 2038–2045. [Google Scholar] [CrossRef]
- Torres-Russotto, D.; Perlmutter, J. Task-specific Dystonias. Ann. N. Y. Acad. Sci. 2008, 1142, 179–199. [Google Scholar] [CrossRef]
- Dagostino, S.; Ercoli, T.; Gigante, A.; Pellicciari, R.; Fadda, L.; Defazio, G. Sensory trick in upper limb dystonia. Parkinsonism Relat. Disord. 2019, 63, 221–223. [Google Scholar] [CrossRef]
- Ramos, V.; Karp, B.; Hallett, M. Tricks in dystonia: Ordering the complexity. J. Neurol. Neurosurg. Psychiatry 2014, 85, 987–993. [Google Scholar] [CrossRef] [Green Version]
- Frucht, L.; Perez, D.; Callahan, J.; MacLean, J.; Song, P.; Sharma, N.; Stephen, C.D. Functional Dystonia: Differentiation From Primary Dystonia and Multidisciplinary Treatments. Front. Neurol. 2021, 11, 1972. [Google Scholar] [CrossRef] [PubMed]
- Lidstone, S.; Costa-Parke, M.; Robinson, E.; Ercoli, T.; Stone, J. Functional movement disorder gender, age and phenotype study: A systematic review and individual patient meta-analysis of 4905 cases. J. Neurol. Neurosurg. Psychiatry 2022, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Tiderington, E.; Goodman, E.; Rosen, A.; Hapner, E.; Johns, M.; Evatt, M.; Freeman, A.; Factor, S.; Jinnah, H.A. How long does it take to diagnose cervical dystonia? J. Neurol. Sci. 2013, 335, 72–74. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- LaHue, S.; Albers, K.; Goldman, S.; Lo, R.; Gu, Z.; Leimpeter, A.; Fross, R.; Comyns, K.; Marras, C.; de Kleijn, A.; et al. Cervical Dystonia Incidence and Diagnostic Delay in a Multiethnic Population. Mov. Disord. 2019, 35, 450–456. [Google Scholar] [CrossRef] [PubMed]
- Comella, C.; Bhatia, K. An international survey of patients with cervical dystonia. J. Neurol. 2015, 262, 837–848. [Google Scholar] [CrossRef] [Green Version]
- Smit, M.; Albanese, A.; Benson, M.; Edwards, M.; Graessner, H.; Hutchinson, M.; Jech, R.; Krauss, J.K.; Morgante, F.; Pérez Dueñas, B.; et al. Dystonia Management: What to Expect From the Future? The Perspectives of Patients and Clinicians Within DystoniaNet Europe. Front. Neurol. 2021, 12, 753. [Google Scholar] [CrossRef]
- Bertram, K.; Williams, D. Delays to the diagnosis of cervical dystonia. J. Clin. Neurosci. 2016, 25, 62–64. [Google Scholar] [CrossRef]
- Roland, D.; Balslev, T. Use of patient video cases in medical education. Arch. Dis. Child.-Educ. Pract. Ed. 2015, 100, 210–214. [Google Scholar] [CrossRef] [Green Version]
- Tackett, S.; Slinn, K.; Marshall, T.; Gaglani, S.; Waldman, V.; Desai, R. Medical Education Videos for the World. Acad. Med. 2018, 93, 1150–1156. [Google Scholar] [CrossRef] [Green Version]
- Issa, N.; Schuller, M.; Santacaterina, S.; Shapiro, M.; Wang, E.; Mayer, R.; DaRosa, D.A. Applying multimedia design principles enhances learning in medical education. Med. Educ. 2011, 45, 818–826. [Google Scholar] [CrossRef]
- Pickering, J.; Joynes, V. A holistic model for evaluating the impact of individual technology-enhanced learning resources. Med. Teach. 2016, 38, 1242–1247. [Google Scholar] [PubMed] [Green Version]
- Jabir, S.; Ahmed, H.; Younis, A. The Awareness Of Dystonia Amongst UK Medical Students in Their Clinical Years. Internet J. Med. Educ. 2012, 2. [Google Scholar]
- Lawal, T.A.; Idowu, B.A.; Ojo, O.O.; Okubadejo, N.U. Knowledge of movement disorders among resident doctors and undergraduate clinical medical students at the Lagos University teaching hospital. Mov. Disord. 2012, 27 (Suppl. S1), S524–S592. [Google Scholar]
- Cubo, E.; Doumbe, J.; López, E.; Lopez, G.; Gatto, E.; Persi, G.; Guttman, M. Telemedicine Enables Broader Access to Movement Disorders Curricula for Medical Students. Tremor Other Hyperkinetic Mov. 2017, 7, 501. [Google Scholar]
- Nwazor, E.; Okeafor, C. Knowledge and attitude towards movement disorders among final year medical students in a Nigerian university. Mov. Disord. 2019, 34 (Suppl. S2), S608. [Google Scholar]
- Dominguez, M.; DiCapua, D.; Leydon, G.; Loomis, C.; Longbrake, E.; Schaefer, S.; Becker, K.P.; Detyniecki, K.; Gottschalk, C.; Salardini, A.; et al. A Neurology Clerkship Curriculum Using Video-Based Lectures and Just-in-Time Teaching (JiTT). MedEdPORTAL 2018, 14, 10691. [Google Scholar] [CrossRef] [PubMed]
- Menkes, D.; Reed, M. Structured Didactic Teaching Sessions Improve Medical Student Neurology Clerkship Test Scores: A Pilot Study. Open Neurol. J. 2008, 2, 8–11. [Google Scholar] [CrossRef] [Green Version]
- Hurtubise, L.; Martin, B.; Gilliland, A.; Mahan, J. To Play or Not To Play: Leveraging Video in Medical Education. J. Grad. Med. Educ. 2013, 5, 13–18. [Google Scholar] [CrossRef] [Green Version]
- Tubelo, R.; Portella, F.; Gelain, M.; de Oliveria, M.; de Oliveria, A.; Dahmer, A.; Pinto, M.E.B. Serious game is an effective learning method for primary health care education of medical students: A randomized controlled trial. Int. J. Med. Inform. 2019, 130, 103944. [Google Scholar] [CrossRef]
- Liu, R.; Relan, A.; Napolitano, J. The Efficiency of Online “Inked” Videos Versus Recorded PowerPoint Lectures on Teaching Pathophysiology to Medical Students in Pre-Clerkship Years: A Pilot Study. J. Med. Educ. Curric. Dev. 2020, 7, 238212051989703. [Google Scholar] [CrossRef] [Green Version]
- Bedi, K.; Okorie, M. A video book of ophthalmic skills for medical students. Int. J. Med. Educ. 2019, 10, 34–35. [Google Scholar] [CrossRef] [PubMed]
- Roediger, H.L., III; Karpickle, J.D. The Power of Testing Memory: Basic Research and Implications for Educational Practice. Perspect Psychol. Sci. 2006, 1, 181–210. [Google Scholar] [CrossRef] [PubMed]
- Guangul, F.M.; Suhail, A.H.; Khalit, M.I.; Khidhir, B.A. Challenges of Remote Assessment in Higher Education in Context of COVID-19: A Case Study of Middle East College. Educ. Assess. Eval. Account. 2020, 32, 519–535. [Google Scholar] [CrossRef]
- Ahmed, F.R.A.; Ahmed, T.E.; Saeed, R.A.; Alhumyani, H.; Abdel-Khalek, S.; Abu-Zinadah, H. Analysis and Challenges of Robust E-exams Performance Under COVID-19. Results Phys. 2021, 23, 10398. [Google Scholar] [CrossRef]





| Authors | Location | Number of: Universities; Students | Medical Student Year Group | Was the Study Specifically Based on Awareness of Dystonia or Movement Disorders Generally? | What Intervention was Used? |
|---|---|---|---|---|---|
| Dominguez et al.,2018 [26] | USA | 1; 135 | Year 3 | Undergraduate neurology (including movement disorders) | Video lectures; did not include patient videos |
| Jabir et al., 2012 [22] | UK | 1; 51 | Year 3, 4, 5 | Dystonia | None |
| Lawal et al., 2012 [23] | Nigeria | 1; 228 | Year 4 and 5 | Movement disorders | None |
| Cubo et al., 2017 [24] | Argentina and Cameroon | 5; 151 | Final year | Movement disorders | Videoconferences including patient videos |
| Nwazor and Okeafor, 2019 [25] | Nigeria | 1; 79 | Final year | Movement disorders | None |
| Menkes and Reed, 2008 [27] | USA | 1; 415 | Year 3 and 4 | Undergraduate neurology (including movement disorders) | Didactic teaching sessions |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Khan, S.; Sowemimo, N.; Alty, J.; Cosgrove, J. Increased Knowledge of Adult-Onset Dystonia Amongst Medical Students via Brief Video Education: A Systematic Review and Cohort Study. Geriatrics 2022, 7, 58. https://doi.org/10.3390/geriatrics7030058
Khan S, Sowemimo N, Alty J, Cosgrove J. Increased Knowledge of Adult-Onset Dystonia Amongst Medical Students via Brief Video Education: A Systematic Review and Cohort Study. Geriatrics. 2022; 7(3):58. https://doi.org/10.3390/geriatrics7030058
Chicago/Turabian StyleKhan, Sana, Nina Sowemimo, Jane Alty, and Jeremy Cosgrove. 2022. "Increased Knowledge of Adult-Onset Dystonia Amongst Medical Students via Brief Video Education: A Systematic Review and Cohort Study" Geriatrics 7, no. 3: 58. https://doi.org/10.3390/geriatrics7030058
APA StyleKhan, S., Sowemimo, N., Alty, J., & Cosgrove, J. (2022). Increased Knowledge of Adult-Onset Dystonia Amongst Medical Students via Brief Video Education: A Systematic Review and Cohort Study. Geriatrics, 7(3), 58. https://doi.org/10.3390/geriatrics7030058