Advances in Alkylated Chitosan and Its Applications for Hemostasis
Abstract
:1. Introduction
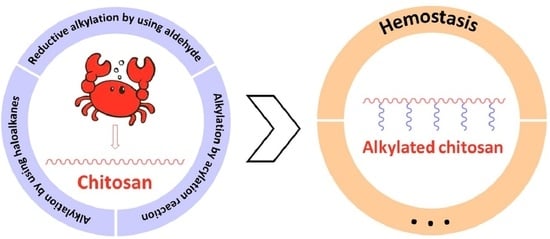
2. Synthesis of Alkylated Chitosan
2.1. Reductive Alkylation by Using Aldehyde
2.2. Alkylation through Haloalkanes and Amino Reaction
2.3. Alkylation by Acylation Reaction
3. Applications of Alkylated Chitosan for Hemostasis
3.1. Hemostatic Mechanism of Alkylated Chitosan and Effect of Molecular Structure on Hemostatic Properties
3.2. Different Forms of Alkylated Chitosan Hemostatic Materials
3.3. Alkylated Chitosan Hemostatic Material Compounded with Other Materials
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Fu, L.; Zhang, J.; Yang, G. Present status and applications of bacterial cellulose-based materials for skin tissue repair. Carbohyd. Polym. 2013, 92, 1432–1442. [Google Scholar] [CrossRef] [PubMed]
- Cheng, F.; Liu, C.; Wei, X.; Yan, T.; Li, H.; He, J.; Huang, Y. Preparation and Characterization of 2,2,6,6-Tetramethylpiperidine-1-oxyl (TEMPO)-Oxidized Cellulose Nanocrystal/Alginate Biodegradable Composite Dressing for Hemostasis Applications. ACS Sustain. Chem. Eng. 2017, 5, 3819–3828. [Google Scholar]
- Wang, Y.; Nie, J.; Fang, W.; Yang, L.; Hu, Q.; Wang, Z.; Sun, J.Z.; Tang, B.Z. Sugar-Based Aggregation-Induced emission luminogens: Design, structures, and applications. Chem. Rev. 2020, 120, 4534–4577. [Google Scholar] [CrossRef]
- Nie, J.; Pei, B.; Wang, Z.; Hu, Q. Construction of ordered structure in polysaccharide hydrogel: A review. Carbohydr. Polym. 2019, 205, 225–235. [Google Scholar] [CrossRef]
- Pei, B.; Wang, Z.; Nie, J.; Hu, Q. Highly mineralized chitosan-based material with large size, gradient mineral distribution and hierarchical structure. Carbohydr. Polym. 2019, 208, 336–344. [Google Scholar] [CrossRef]
- Chen, E.; Yang, L.; Ye, C.; Zhang, W.; Ran, J.; Xue, D.; Wang, Z.; Pan, Z.; Hu, Q. An asymmetric chitosan scaffold for tendon tissue engineering: In vitro and in vivo evaluation with rat tendon stem/progenitor cells. Acta Biomater. 2018, 73, 377–387. [Google Scholar] [CrossRef]
- Huang, X.; Sun, Y.; Nie, J.; Lu, W.; Yang, L.; Zhang, Z.; Yin, H.; Wang, Z.; Hu, Q. Using absorbable chitosan hemostatic sponges as a promising surgical dressing. Int. J. Biol. Macromol. 2015, 75, 322–329. [Google Scholar] [CrossRef]
- Qiao, F.; Ke, J.; Liu, Y.; Pei, B.; Hu, Q.; Tang, B.Z.; Wang, Z. Cationic quaternized chitosan bioconjugates with aggregation-induced emission features for cell imaging. Carbohydr. Polym. 2020, 230, 115614. [Google Scholar] [CrossRef]
- Yang, L.; Lu, W.; Pang, Y.; Huang, X.; Wang, Z.; Qin, A.; Hu, Q. Fabrication of a novel chitosan scaffold with asymmetric structure for guided tissue regeneration. RSC Adv. 2016, 6, 71567–71573. [Google Scholar] [CrossRef]
- Jin, X.; Jiang, H.; Li, G.; Fu, B.; Bao, X.; Wang, Z.; Hu, Q. Stretchable, conductive PAni-PAAm-GOCS hydrogels with excellent mechanical strength, strain sensitivity and skin affinity. Chem. Eng. J. 2020, 394, 124901. [Google Scholar] [CrossRef]
- Feng, W.; Wang, Z. Biomedical applications of chitosan-graphene oxide nanocomposites. iScience 2022, 25, 103629. [Google Scholar] [CrossRef]
- Liu, X.; Wu, Y.; Zhao, X.; Wang, Z. Fabrication and applications of bioactive chitosan-based organic-inorganic hybrid materials: A review. Carbohydr. Polym. 2021, 267, 118179. [Google Scholar] [CrossRef] [PubMed]
- Huang, X.; Bao, X.; Liu, Y.; Wang, Z.; Hu, Q. Catechol-Functional Chitosan/Silver nanoparticle composite as a highly effective antibacterial agent with Species-Specific mechanisms. Sci. Rep. 2017, 7, 1860. [Google Scholar] [CrossRef]
- Koumentakou, I.; Terzopoulou, Z.; Michopoulou, A.; Kalafatakis, I.; Theodorakis, K.; Tzetzis, D.; Bikiaris, D. Chitosan dressings containing inorganic additives and levofloxacin as potential wound care products with enhanced hemostatic properties. Int. J. Biol. Macromol. 2020, 162, 693–703. [Google Scholar] [CrossRef] [PubMed]
- Yang, S.; Miao, Q.; Huang, Y.; Jian, P.; Wang, X.; Tu, M. Preparation of cinnamaldehyde-loaded polyhydroxyalkanoate/chitosan porous microspheres with adjustable controlled-release property and its application in fruit preservation. Food Packag. Shelf Life 2020, 26, 100596. [Google Scholar] [CrossRef]
- Sun, X.; Wu, Q.; Picha, D.H.; Ferguson, M.H.; Ndukwe, I.E.; Azadi, P. Comparative performance of bio-based coatings formulated with cellulose, chitin, and chitosan nanomaterials suitable for fruit preservation. Carbohyd. Polym. 2021, 259, 117764. [Google Scholar] [CrossRef]
- Kim, J.; Kim, T.H.; Lee, J.H.; Park, Y.A.; Kang, Y.J.; Ji, H.G. Porous nanocomposite of layered double hydroxide nanosheet and chitosan biopolymer for cosmetic carrier application. Appl. Clay Sci. 2021, 205, 106067. [Google Scholar] [CrossRef]
- Chen, K.; Guo, B.; Luo, J. Quaternized carboxymethyl chitosan/organic montmorillonite nanocomposite as a novel cosmetic ingredient against skin aging. Carbohyd. Polym. 2017, 173, 100–106. [Google Scholar] [CrossRef]
- Bikiaris, N.D.; Michailidou, G.; Lazaridou, M.; Christodoulou, E.; Gounari, E.; Ofrydopoulou, A.; Lambropoulou, D.A.; Vergkizi-Nikolakaki, S.; Lykidou, S.; Nikolaidis, N. Innovative skin product emulsions with enhanced antioxidant, antimicrobial and UV protection properties containing nanoparticles of pure and modified chitosan with encapsulated fresh pomegranate juice. Polymers 2020, 12, 1542. [Google Scholar] [CrossRef]
- Li, W.; Wei, H.; Liu, Y.; Li, S.; Wang, G.; Guo, T.; Han, H. An in situ reactive spray-drying strategy for facile preparation of starch-chitosan based hydrogel microspheres for water treatment application. Chem. Eng. Process.-Process Intensif. 2021, 168, 108548. [Google Scholar] [CrossRef]
- El-Shafai, N.M.; Shawky, S.; El-Mehasseb, I.M.; El-Kemary, M.A. Sandwich nanohybrid of chitosan-polyvinyl alcohol for water treatment and Sofosbuvir drug delivery for anti-hepatitis C virus (HCV). Int. J. Biol. Macromol. 2021, 190, 927–939. [Google Scholar] [CrossRef] [PubMed]
- Jin, E.; Wang, Z.; Li, M.; Hu, Q.; Tang, B.Z.; Yuan, J. Fluorescent sizing agents based on Aggregation-Induced emission effect for accurate evaluation of permeability and coating property. Fiber. Polym. 2021, 22, 1218–1227. [Google Scholar] [CrossRef]
- Jin, E.; Wang, Z.; Hu, Q.; Li, M.; Yuan, J. Perylene-Based fluorescent sizing agent for precise evaluation of permeability and coating property of sizing paste. Adv. Fiber Mater. 2020, 2, 279–290. [Google Scholar] [CrossRef]
- Lim, C.; Lee, D.W.; Israelachvili, J.N.; Jho, Y.; Hwang, D.S. Contact time- and pH-dependent adhesion and cohesion of low molecular weight chitosan coated surfaces. Carbohyd. Polym. 2015, 117, 887–894. [Google Scholar] [CrossRef] [Green Version]
- Wang, W.; Xue, C.; Mao, X. Chitosan: Structural modification, biological activity and application. Int. J. Biol. Macromol. 2020, 164, 4532–4546. [Google Scholar] [CrossRef]
- Du, X.; Wu, L.; Yan, H.; Jiang, Z.; Li, S.; Li, W.; Bai, Y.; Wang, H.; Cheng, Z.; Kong, D.; et al. Microchannelled alkylated chitosan sponge to treat noncompressible hemorrhages and facilitate wound healing. Nat. Commun. 2021, 12, 4733. [Google Scholar] [CrossRef]
- Mourya, V.K.; Inamdara, N.; Ashutosh Tiwari, N. Carboxymethyl chitosan and its applications. Adv. Mater. Lett. 2010, 1, 11–33. [Google Scholar] [CrossRef]
- Andreica, B.; Cheng, X.; Marin, L. Quaternary ammonium salts of chitosan. A critical overview on the synthesis and properties generated by quaternization. Eur. Polym. J. 2020, 139, 110016. [Google Scholar] [CrossRef]
- Liu, W.; Sun, S.; Cheng, N. Preparation of Temperature-Sensitive Chitosan-Graft-NIPAAm/VL Copolymer Transgenic Carrier. China Patent CN 20041072351, 21 October 2004. [Google Scholar]
- Chen, Z.; Yao, X.; Liu, L.; Guan, J.; Liu, M.; Li, Z.; Yang, J.; Huang, S.; Wu, J.; Tian, F.; et al. Blood coagulation evaluation of N -alkylated chitosan. Carbohyd. Polym. 2017, 173, 259–268. [Google Scholar] [CrossRef]
- Petit, C.; Reynaud, S.; Desbrieres, J. Amphiphilic derivatives of chitosan using microwave irradiation. Toward an eco-friendly process to chitosan derivatives. Carbohyd. Polym. 2015, 116, 26–33. [Google Scholar]
- Wang, Z.; Nie, J.; Qin, W.; Hu, Q.; Tang, B.Z. Gelation process visualized by aggregation-induced emission fluorogens. Nat. Commun. 2016, 7, 12033. [Google Scholar] [CrossRef]
- Nie, J.; Wang, Z.; Hu, Q. Difference between Chitosan Hydrogels via Alkaline and Acidic Solvent Systems. Sci. Rep. 2016, 6, 36053. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nie, J.; Wang, Z.; Zhang, J.; Yang, L.; Pang, Y.; Hu, Q. High strength chitosan rod prepared via LiOH/urea solvent through centrifugation induced orientation processing. RSC Adv. 2015, 5, 66825–68243. [Google Scholar] [CrossRef]
- Almeida, E.V.R.; Frollini, E.; Castellan, A.; Coma, V. Chitosan, sisal cellulose, and biocomposite chitosan/sisal cellulose films prepared from thiourea/NaOH aqueous solution. Carbohyd. Polym. 2010, 80, 655–664. [Google Scholar] [CrossRef]
- Bi, S.; Hu, S.; Zhou, Z.; Kong, M.; Liu, Y.; Feng, C.; Cheng, X.; Chen, X. The green and stable dissolving system based on KOH/urea for homogeneous chemical modification of chitosan. Int. J. Biol. Macromol. 2018, 120, 1103–1110. [Google Scholar] [CrossRef]
- Sun, X.; Li, J.; Shao, K.; Su, C.; Bi, S.; Mu, Y.; Zhang, K.; Cao, Z.; Wang, X.; Chen, X.; et al. A composite sponge based on alkylated chitosan and diatom-biosilica for rapid hemostasis. Int. J. Biol. Macromol. 2021, 182, 2097–2107. [Google Scholar] [CrossRef]
- Pei, L.; Cai, Z.; Shang, S.; Song, Z. Synthesis and antibacterial activity of alkylated chitosan under basic ionic liquid conditions. J. Appl. Polym. Sci. 2014, 131. [Google Scholar] [CrossRef]
- Le Tien, C.; Lacroix, M.; Ispas-Szabo, P.; Mateescu, M. N-acylated chitosan: Hydrophobic matrices for controlled drug release. J. Control Release 2003, 93, 1–13. [Google Scholar] [CrossRef]
- Rodrigues, M.R. Synthesis and investigation of chitosan derivatives formed by reaction with acyl chlorides. J. Carbohyd. Chem. 2005, 24, 41–54. [Google Scholar] [CrossRef]
- Hu, Y.; Du, Y.; Yang, J.; Tang, Y.; Li, J.; Wang, X. Self-aggregation and antibacterial activity of N-acylated chitosan. Polymer 2007, 48, 3098–3106. [Google Scholar] [CrossRef]
- Zhen, Z.; Fujun, J.; Zicong, W.; Ju, J.; Feng, L.; Yiliang, W.; Zhiping, W.; Shunqing, T.; Chaoxi, W.; Yifei, W. O-acylation of chitosan nanofibers by short-chain and long-chain fatty acids. Carbohyd. Polym. 2017, 177, 203–209. [Google Scholar]
- Wang, X.; Dang, Q.; Liu, C.; Chang, G.; Song, H.; Xu, Q.; Ma, Y.; Li, B.; Zhang, B.; Cha, D. Antibacterial porous sponge fabricated with capric acid-grafted chitosan and oxidized dextran as a novel hemostatic dressing. Carbohyd. Polym. 2022, 277, 118782. [Google Scholar] [CrossRef] [PubMed]
- Liu, M.; Yang, J.; Guan, J.; Huang, S.; Li, Z.; Jing, M. Effect of grafted chain length on hemostatic activity of N-Alkylated chitosan. In Proceedings of the 4th Annual International Conference on Material Engineering and Application (ICMEA 2017), Wuhan, China, 15–17 December 2017; Volume 146, pp. 229–234. [Google Scholar]
- Huang, Y.; Feng, L.; Zhang, Y.; He, L.; Wang, C.; Xu, J.; Wu, J.; Kirk, T.B.; Guo, R.; Xue, W. Hemostasis mechanism and applications of N-alkylated chitosan sponge. Polym. Advan. Technol. 2017, 28, 1107–1114. [Google Scholar] [CrossRef]
- Huang, Y.; Zhang, Y.; Feng, L.; He, L.; Guo, R.; Xue, W. Synthesis of N-alkylated chitosan and its interactions with blood. Artif. Cells Nanomed. Biotechnol. 2018, 46, 544–550. [Google Scholar] [CrossRef]
- Wang, X.; Guan, J.; Zhuang, X.; Li, Z.; Huang, S.; Yang, J.; Liu, C.; Li, F.; Tian, F.; Wu, J.; et al. Exploration of blood coagulation of N-Alkyl chitosan nanofiber membrane in vitro. Biomacromolecules 2018, 19, 731–739. [Google Scholar] [CrossRef]
- Dowling, M.B.; Kumar, R.; Keibler, M.A.; Hess, J.R.; Bochicchio, G.V.; Raghavan, S.R. A self-assembling hydrophobically modified chitosan capable of reversible hemostatic action. Biomaterials 2011, 32, 3351–3357. [Google Scholar] [CrossRef] [PubMed]
- Dowling, M.B.; Smith, W.; Balogh, P.; Duggan, M.J.; Macintire, I.C.; Harris, E.; Mesar, T.; Raghavan, S.R.; King, D.R. Hydrophobically-modified chitosan foam: Description and hemostatic efficacy. J. Surg. Res. 2015, 193, 316–323. [Google Scholar] [CrossRef] [PubMed]
- Logun, M.T.; Dowling, M.B.; Raghavan, S.R.; Wallace, M.L.; Schmiedt, C.; Stice, S.; Karumbaiah, L. Expanding hydrophobically modified chitosan foam for internal surgical hemostasis: Safety evaluation in a murine model. J. Surg. Res. 2019, 239, 269–277. [Google Scholar]
- Chaturvedi, A.; Dowling, M.B.; Gustin, J.P.; Scalea, T.M.; Raghavan, S.R.; Pasley, J.D.; Narayan, M. Hydrophobically modified chitosan gauze: A novel topical hemostat. J. Surg. Res. 2017, 207, 45–52. [Google Scholar] [CrossRef]
- Chen, Z.; Han, L.; Liu, C.; Du, Y.; Hu, X.; Du, G.; Shan, C.; Yang, K.; Wang, C.; Li, M.; et al. A rapid hemostatic sponge based on large, mesoporous silica nanoparticles and N-alkylated chitosan. Nanoscale 2018, 10, 20234–20245. [Google Scholar] [CrossRef]
- Zhang, Y.; Guan, J.; Wu, J.; Ding, S.; Yang, J.; Zhang, J.; Dong, A.; Deng, L. N-alkylated chitosan/graphene oxide porous sponge for rapid and effective hemostasis in emergency situations. Carbohyd. Polym. 2019, 219, 405–413. [Google Scholar] [CrossRef] [PubMed]






| Chitosan Derivatives | Synthesis | Physical Properties | Applications |
|---|---|---|---|
| Alkylated chitosan | with Aldehyde | Amphiphilicity | Hemostasis |
| with Haloalkane | Antibacterial [26] | ||
| Acylation | |||
| Carboxymethyl chitosan [27] | Hydrophilicity | Cosmetic | |
| Schiff base reaction | Drug delivery | ||
| pH responsiveness | Miscellaneous | ||
| Quaternary ammonium salts of chitosan [28] | Directly quaternary ammonium at the amine units | Water solubility | Gene therapy |
| Drug delivery | |||
| Side chain quaternary ammonium | Positive charge | Wound healing | |
| Tissue engineering | |||
| NIPAAm-chitosan [29] | Acylation | Temperature sensitivity | DNA delivery |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jin, H.; Wang, Z. Advances in Alkylated Chitosan and Its Applications for Hemostasis. Macromol 2022, 2, 346-360. https://doi.org/10.3390/macromol2030022
Jin H, Wang Z. Advances in Alkylated Chitosan and Its Applications for Hemostasis. Macromol. 2022; 2(3):346-360. https://doi.org/10.3390/macromol2030022
Chicago/Turabian StyleJin, Huiyang, and Zhengke Wang. 2022. "Advances in Alkylated Chitosan and Its Applications for Hemostasis" Macromol 2, no. 3: 346-360. https://doi.org/10.3390/macromol2030022
APA StyleJin, H., & Wang, Z. (2022). Advances in Alkylated Chitosan and Its Applications for Hemostasis. Macromol, 2(3), 346-360. https://doi.org/10.3390/macromol2030022