COVID-19 and Brain (Closed)
A topical collection in Brain Sciences (ISSN 2076-3425). This collection belongs to the section "Systems Neuroscience".
Viewed by 20433Editors
Interests: stroke; neuroimmunology; COVID-19; migraine; Parkinson’s disease; education; advocacy
Special Issues, Collections and Topics in MDPI journals
Interests: circadian rhythms; insomnia; sleep; sleep disorders; melatonin; shift work; light; sleepiness-related crashes
Interests: rehabilitation; movement disorders; COVID-19 and brain
Interests: organizational psychology; statistics; workplace mental health and wellbeing; health care workforces
Special Issues, Collections and Topics in MDPI journals
Topical Collection Information
Dear Colleagues,
We are delighted to share the good news with you that the MDPI journal Brain Sciences has launched a Special Issue entitled "COVID-19 and Brain".
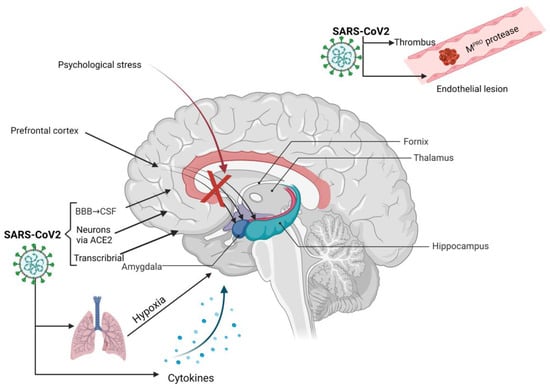
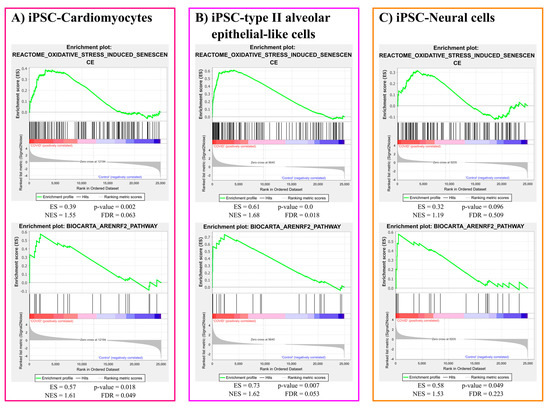
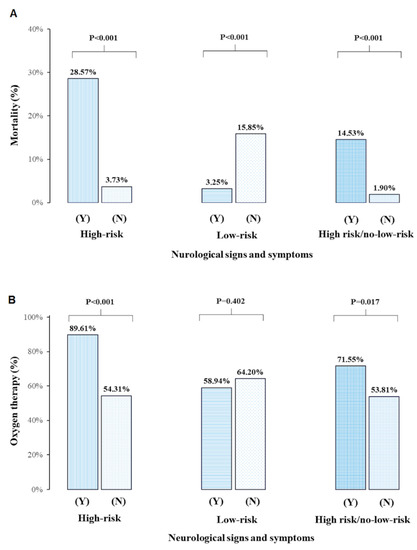
"COVID-19 and Brain" is dedicated to promoting and improving the basic and translational knowledge of how the human nervous system and immune systems interact in the context of acute COVID-19; it will explore the long-term neurological impact of COVID-19 and how these interactions lead to disease processes, as well as the progress of—and prognostication of—acute and long-term neurological syndromes in association with COVID-19 infection.
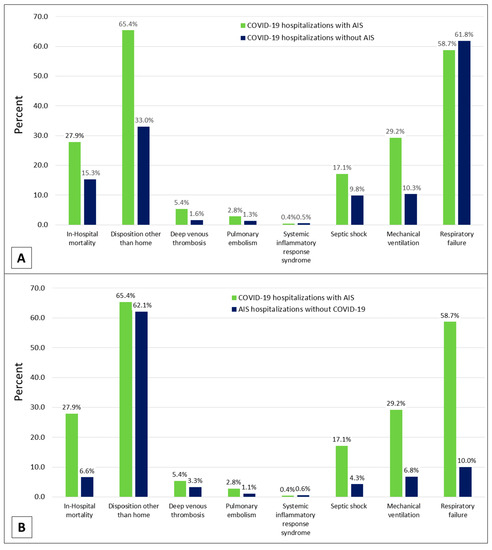
Neuroimmunology plays a key role in four leading disorders (stroke, migraine, dementia, and neurotrauma) that are responsible for nearly 80% of deaths and disability in low-to-middle-income countries with an opportunity to improve care globally. The pathobiology of these disorders, in relation to post-COVID-19 and brain involvement, appears to share similar acute and ongoing processes at the cellular level.
The COVID-19 pandemic is a timely reminder of the importance of neuroinflammation in brain health given the shared pathobiology of COVID-19, acute stroke, and many other acquired neurological disorders.
We welcome your submissions to "COVID-19 and Brain".
Prof. Dr. Tissa Wijeratne
Collection Editor
Prof. Dr. Shantha Rajaratnam
Prof. Dr. Meg E. Morris
Dr. Leila Karimi
Co-Collection Editors
Manuscript Submission Information
Manuscripts should be submitted online at www.mdpi.com by registering and logging in to this website. Once you are registered, click here to go to the submission form. Manuscripts can be submitted until the deadline. All submissions that pass pre-check are peer-reviewed. Accepted papers will be published continuously in the journal (as soon as accepted) and will be listed together on the collection website. Research articles, review articles as well as short communications are invited. For planned papers, a title and short abstract (about 100 words) can be sent to the Editorial Office for announcement on this website.
Submitted manuscripts should not have been published previously, nor be under consideration for publication elsewhere (except conference proceedings papers). All manuscripts are thoroughly refereed through a single-blind peer-review process. A guide for authors and other relevant information for submission of manuscripts is available on the Instructions for Authors page. Brain Sciences is an international peer-reviewed open access monthly journal published by MDPI.
Please visit the Instructions for Authors page before submitting a manuscript. The Article Processing Charge (APC) for publication in this open access journal is 2200 CHF (Swiss Francs). Submitted papers should be well formatted and use good English. Authors may use MDPI's English editing service prior to publication or during author revisions.
Keywords
- neuroimmunology
- COVID-19
- brain
- post COVID-19 neurological syndrome
- brain fog
- fatigue