The New Era of Mesenchymal Stromal/Stem Cell Functional Application: State of the Art, Therapeutic Challenges and Future Directions
A topical collection in Cells (ISSN 2073-4409). This collection belongs to the section "Cellular Immunology".
Viewed by 8092Editors
Interests: mesenchymal stromal cells; NKG2D; innate immunity; leukemia and lymphoma; anti-tumor immunity
Special Issues, Collections and Topics in MDPI journals
Interests: mesenchymal stem/stromal cells (MSCs); tissue sources of MSCs; immunomodulation properties; extracellular vesicles (EVs); environmental challenges; efficient MSC immunotherapy
Special Issues, Collections and Topics in MDPI journals
Topical Collection Information
Dear Colleagues,
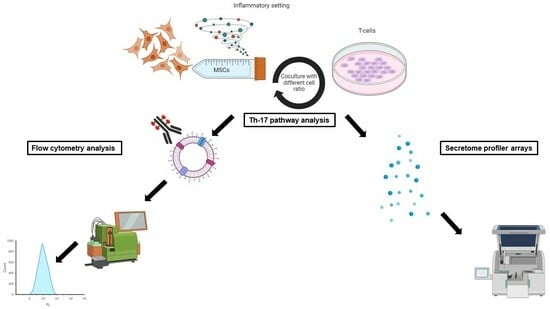
Mesenchymal stromal cells (MSCs) hold great promise in the field of immunotherapy and regenerative medicine. Indeed, a significant amount of experimental evidence supports the notion that MSCs i) can finely regulate both innate and adaptive immune response and ii) may show the property to differentiate into both mature mesodermal and ectodermal cells. However, some conflicting results have been reported on the molecular mechanisms responsible for their immunosuppressive and totipotential properties of differentiation. The specific identification of phenotypic and functional behavior of these cells will further trigger their clinical use for a variety of autoimmune and degenerative diseases. As part of their molecular mechanisms of action, MSCs produce extracellular matrix protein and closely interact with the tissue environment, displaying a combination of trophic and immunomodulatory actions. These therapeutic effects are likely governed by cell-to cell contact, paracrine pathways, including a role for extracellular vesicles (EVs) and their functional plasticity which means they can adapt their behavior in the face of tissue challenges. MSCs can also be present within the tumor microenvironment and influence tumor cell growth and tumor immune response, as well as the therapeutic effect of anti-blastic drugs and immune-checkpoint blockers.
It is time to bridge MSCs from the bench and clinical applications by translating basic science into medical programs. The great contribution of colleagues involved in the field will significantly enrich the debate and open up new horizons for the use of MSCs. Accordingly, a better knowledge and characterization of the biological and immunological characteristics of MSCs will increase the safety and efficiency of their clinical application.
Prof. Dr. Alessandro Poggi
Dr. Mehdi Najar
Collection Editors
Manuscript Submission Information
Manuscripts should be submitted online at www.mdpi.com by registering and logging in to this website. Once you are registered, click here to go to the submission form. Manuscripts can be submitted until the deadline. All submissions that pass pre-check are peer-reviewed. Accepted papers will be published continuously in the journal (as soon as accepted) and will be listed together on the collection website. Research articles, review articles as well as short communications are invited. For planned papers, a title and short abstract (about 100 words) can be sent to the Editorial Office for announcement on this website.
Submitted manuscripts should not have been published previously, nor be under consideration for publication elsewhere (except conference proceedings papers). All manuscripts are thoroughly refereed through a single-blind peer-review process. A guide for authors and other relevant information for submission of manuscripts is available on the Instructions for Authors page. Cells is an international peer-reviewed open access semimonthly journal published by MDPI.
Please visit the Instructions for Authors page before submitting a manuscript. The Article Processing Charge (APC) for publication in this open access journal is 2700 CHF (Swiss Francs). Submitted papers should be well formatted and use good English. Authors may use MDPI's English editing service prior to publication or during author revisions.
Keywords
- MSCs
- mesenchymal stromal cells
- immunotherapy
- regenerative medicine
- immune
- tumor