Advances of MRI in Radiation Oncology
(Closed)
Share This Topical Collection
Editor
 Prof. Dr. Indra J. Das
Prof. Dr. Indra J. Das
 Prof. Dr. Indra J. Das
Prof. Dr. Indra J. Das
E-Mail
Website
Guest Editor
Department of Radiation Oncology, Northwestern Memorial Hospital, Northwest University Feinberg School of Medicine, Galter Pavilion LC 178, Chicago, IL 60611, USA
Interests: MR-linac; radiation dosimetry; treament planning; IMRT/VMAT; SBRT; proton beam
Special Issues, Collections and Topics in MDPI journals
Topical Collection Information
Dear Colleague,
Radiation oncology treatment planning requires CT data for dose calculation; however, CT lacks soft-tissue visualization and characterization. MR images are best suited for soft-tissue, especially liver, pancreas, kidney, prostate, and brain tissues. MR images have been augmented using image fusion but their accuracy can be questionable. Additionally, MR images do not provide electron density information needed for dose calculation. Moving structures pose additional challenges in radiation oncology. The active trend in radiation oncology is to use MR images with help of synthetic CT for image-guided radiation therapy. Integrated MR imaging and linear accelerator system (MRL) provides optimum treatment for soft tissue and moving structures is a new frontier in radiation oncology. The focus of this Special Issue is to review current MR imaging options, as well as imaging-assisted therapies, and adaptive therapies in radiation oncology. This issue will cover MR imaging parameters/sequences in low and high magnetic fields, MR-linacs, synthetic CT, dose calculation, motion management as well as every aspect of MR use in radiation oncology.
Prof. Dr. Indra J. Das
Guest Editor
Manuscript Submission Information
Manuscripts should be submitted online at www.mdpi.com by registering and logging in to this website. Once you are registered, click here to go to the submission form. Manuscripts can be submitted until the deadline. All submissions that pass pre-check are peer-reviewed. Accepted papers will be published continuously in the journal (as soon as accepted) and will be listed together on the collection website. Research articles, review articles as well as short communications are invited. For planned papers, a title and short abstract (about 100 words) can be sent to the Editorial Office for announcement on this website.
Submitted manuscripts should not have been published previously, nor be under consideration for publication elsewhere (except conference proceedings papers). All manuscripts are thoroughly refereed through a single-blind peer-review process. A guide for authors and other relevant information for submission of manuscripts is available on the Instructions for Authors page. Journal of Clinical Medicine is an international peer-reviewed open access semimonthly journal published by MDPI.
Please visit the Instructions for Authors page before submitting a manuscript.
The Article Processing Charge (APC) for publication in this open access journal is 2600 CHF (Swiss Francs).
Submitted papers should be well formatted and use good English. Authors may use MDPI's
English editing service prior to publication or during author revisions.
Keywords
- MR imaging
- MR sequence
- low and high magnetic-field
- MR-linac
- adaptive therapy
- motion management
- synthetic CT
Published Papers (22 papers)
Open AccessReview
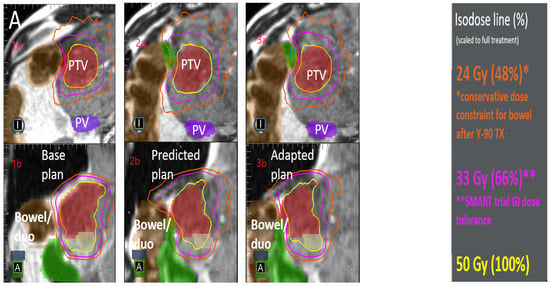
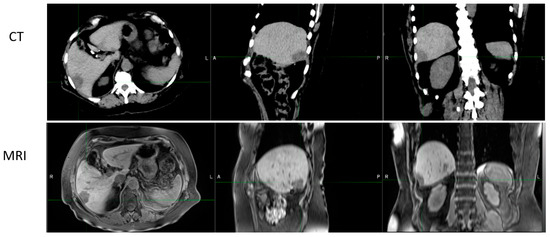
Local Therapies for Hepatocellular Carcinoma and Role of MRI-Guided Adaptive Radiation Therapy
by
Yirong Liu, Brian Chou, Amulya Yalamanchili, Sara N. Lim, Laura A. Dawson and Tarita O. Thomas
Cited by 2 | Viewed by 2190
Abstract
Hepatocellular carcinoma (HCC) is the most common liver tumor, with a continually rising incidence. The curative treatment for HCC is surgical resection or liver transplantation; however, only a small portion of patients are eligible due to local tumor burden or underlying liver dysfunction.
[...] Read more.
Hepatocellular carcinoma (HCC) is the most common liver tumor, with a continually rising incidence. The curative treatment for HCC is surgical resection or liver transplantation; however, only a small portion of patients are eligible due to local tumor burden or underlying liver dysfunction. Most HCC patients receive nonsurgical liver-directed therapies (LDTs), including thermal ablation, transarterial chemoembolization (TACE), transarterial radioembolization (TARE), and external beam radiation therapy (EBRT). Stereotactic ablative body radiation (SABR) is a specific type of EBRT that can precisely deliver a high dose of radiation to ablate tumor cells using a small number of treatments (or fractions, typically 5 or less). With onboard MRI imaging, MRI-guided SABR can improve therapeutic dose while minimizing normal tissue exposure. In the current review, we discuss different LDTs and compare them with EBRT, specifically SABR. The emerging MRI-guided adaptive radiation therapy has been reviewed, highlighting its advantages and potential role in HCC management.
Full article
►▼
Show Figures
Open AccessArticle
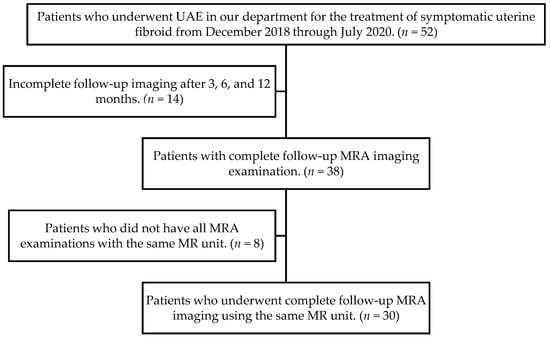
Use of Non-Contrast-Enhanced MR Angiography to Assess Recanalization after Uterine Artery Embolization
by
Juliana Yumi Ishisaki, Hitomi Kato, Yoshiki Kuwatsuru, Hiroshi Toei, Ayako Hoshina, Naoki Takemasa, Masafumi Arai and Ryohei Kuwatsuru
Cited by 1 | Viewed by 2020
Abstract
The purpose of this study was to examine the use of non-contrast-enhanced MR angiography (MRA) for assessing recanalization of uterine arteries (UAs) after uterine artery embolization (UAE) for symptomatic fibroids. Pre-procedural and follow-up unenhanced MRA images of 30 patients were reviewed, and the
[...] Read more.
The purpose of this study was to examine the use of non-contrast-enhanced MR angiography (MRA) for assessing recanalization of uterine arteries (UAs) after uterine artery embolization (UAE) for symptomatic fibroids. Pre-procedural and follow-up unenhanced MRA images of 30 patients were reviewed, and the extent to which the UAs could be visualized was classified on a 4-point scale. An increase in the score between consecutive time points indicates that a previously inconspicuous segment of the UA became visible on follow-up images. Patients were divided into two groups according to the presence (or absence) of recanalization. The median UA visualization score at each follow-up was significantly lower than that at baseline (
p < 0.01), but there was no significant difference between the scores of the follow-up images. Recanalization was detected in 63% (19/30) of patients. In these patients, the mean decrease in uterine and largest fibroid volume at 12 months after UAE was inferior to the mean decrease in patients for whom recanalization was not detected. Based on MRA assessment, recanalization after UAE occurred in 63% of patients but did not compromise the reduction in uterine and dominant fibroid volumes within 12 months after UAE.
Full article
►▼
Show Figures
Open AccessArticle
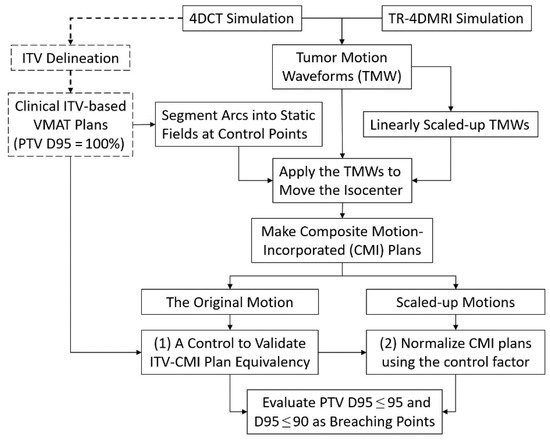
A Simulation Study of Tolerance of Breathing Amplitude Variations in Radiotherapy of Lung Cancer Using 4DCT and Time-Resolved 4DMRI
by
Guang Li, Admir Sehovic, Lee Xu, Pawas Shukla, Lei Zhang, Ying Zhou, Ping Wang, Abraham Wu, Andreas Rimner and Pengpeng Zhang
Cited by 1 | Viewed by 1713
Abstract
As patient breathing irregularities can introduce a large uncertainty in targeting the internal tumor volume (ITV) of lung cancer patients, and thereby affect treatment quality, this study evaluates dose tolerance of tumor motion amplitude variations in ITV-based volumetric modulated arc therapy (VMAT). A
[...] Read more.
As patient breathing irregularities can introduce a large uncertainty in targeting the internal tumor volume (ITV) of lung cancer patients, and thereby affect treatment quality, this study evaluates dose tolerance of tumor motion amplitude variations in ITV-based volumetric modulated arc therapy (VMAT). A motion-incorporated planning technique was employed to simulate treatment delivery of 10 lung cancer patients’ clinical VMAT plans using original and three scaling-up (by 0.5, 1.0, and 2.0 cm) motion waveforms from single-breath four-dimensional computed tomography (4DCT) and multi-breath time-resolved 4D magnetic resonance imaging (TR-4DMRI). The planning tumor volume (PTV = ITV + 5 mm margin) dose coverage (PTV D95%) was evaluated. The repeated waveforms were used to move the isocenter in sync with the clinical leaf motion and gantry rotation. The continuous VMAT arcs were broken down into many static beam fields at the control points (2°-interval) and the composite plan represented the motion-incorporated VMAT plan. Eight motion-incorporated plans per patient were simulated and the plan with the native 4DCT waveform was used as a control. The first (D95% ≤ 95%) and second (D95% ≤ 90%) plan breaching points due to motion amplitude increase were identified and analyzed. The PTV D95% in the motion-incorporated plans was 99.4 ± 1.0% using 4DCT, closely agreeing with the corresponding ITV-based VMAT plan (PTV D95% = 100%). Tumor motion irregularities were observed in TR-4DMRI and triggered D95% ≤ 95% in one case. For small tumors, 4 mm extra motion triggered D95% ≤ 95%, and 6–8 mm triggered D95% ≤ 90%. For large tumors, 14 mm and 21 mm extra motions triggered the first and second breaching points, respectively. This study has demonstrated that PTV D95% breaching points may occur for small tumors during treatment delivery. Clinically, it is important to monitor and avoid systematic motion increase, including baseline drift, and large random motion spikes through threshold-based beam gating.
Full article
►▼
Show Figures
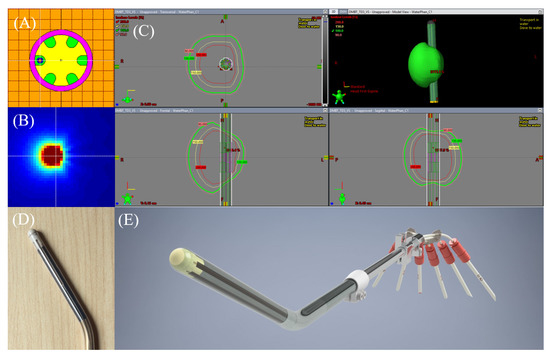
Open AccessArticle
A Novel Workflow with a Customizable 3D Printed Vaginal Template and a Direction Modulated Brachytherapy (DMBT) Tandem Applicator for Adaptive Interstitial Brachytherapy of the Cervix
by
James J. Sohn, Mitchell Polizzi, Dylan Richeson, Somayeh Gholami, Indra J. Das and William Y. Song
Cited by 2 | Viewed by 2378
Abstract
A novel clinical workflow utilizing a direction modulated brachytherapy (DMBT) tandem applicator in combination with a patient-specific, 3D printed vaginal needle-track template for an advanced image-guided adaptive interstitial brachytherapy of the cervix. The proposed workflow has three main steps: (1) pre-treatment MRI, (2)
[...] Read more.
A novel clinical workflow utilizing a direction modulated brachytherapy (DMBT) tandem applicator in combination with a patient-specific, 3D printed vaginal needle-track template for an advanced image-guided adaptive interstitial brachytherapy of the cervix. The proposed workflow has three main steps: (1) pre-treatment MRI, (2) an initial optimization of the needle positions based on the DMBT tandem positioning and patient anatomy, and a subsequent inverse optimization using the combined DMBT tandem and needles, and (3) rapid 3D printing. We retrospectively re-planned five patient cases for two scenarios; one plan with the DMBT tandem (T) and ovoids (O) with the original needle (ND) positions (DMBT + O + ND) and another with the DMBT T&O and spatially reoptimized needles (OptN) positions (DMBT + O + OptN). All retrospectively reoptimized plans have been compared to the original plan (OP) as well. The accuracy of 3D printing was verified through the image registration between the planning CT and the CT of the 3D-printed template. The average difference in D
2cc for the bladder, rectum, and sigmoid between the OPs and DMBT + O + OptNs were −8.03 ± 4.04%, −18.67 ± 5.07%, and −26.53 ± 4.85%, respectively. In addition, these average differences between the DMBT + O + ND and DMBT + O + OptNs were −2.55 ± 1.87%, −10.70 ± 3.45%, and −22.03 ± 6.01%, respectively. The benefits could be significant for the patients in terms of target coverage and normal tissue sparing and increase the optimality over free-hand needle positioning.
Full article
►▼
Show Figures
Open AccessArticle
1.5 T MR-Guided Daily Adapted SBRT on Lymph Node Oligometastases from Prostate Cancer
by
Luca Nicosia, Giovanna Trapani, Michele Rigo, Niccolò Giaj-Levra, Rosario Mazzola, Edoardo Pastorello, Francesco Ricchetti, Francesco Cuccia, Vanessa Figlia, Matilde Fiorini and Filippo Alongi
Cited by 4 | Viewed by 1883
Abstract
Introduction: The aim of our study was to evaluate the efficacy and toxicity of a daily adaptive MR-guided SBRT on 1.5 T MR-linac in patients affected by lymph node oligometastases from PCa.
Materials and Methods: The present study is a prospective observational study
[...] Read more.
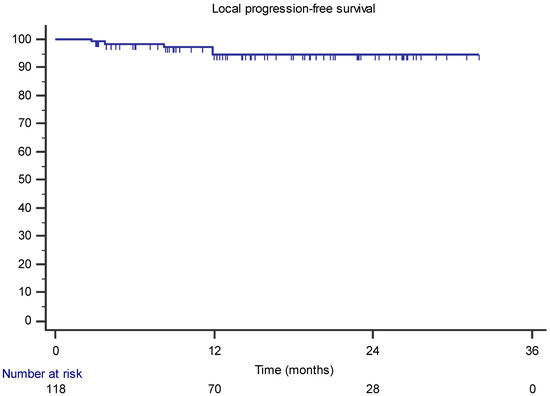
Introduction: The aim of our study was to evaluate the efficacy and toxicity of a daily adaptive MR-guided SBRT on 1.5 T MR-linac in patients affected by lymph node oligometastases from PCa.
Materials and Methods: The present study is a prospective observational study conducted in a single institution (protocol n°: MRI/LINAC n. 23748). Patients with oligometastatic lymph nodes from PCa treated with daily adaptive MR-guided SBRT on 1.5 T MR-linac were included in the study. There was a minimum required follow-up of 3 months after SBRT. The primary end-point was local progression-free survival (LPFS). The secondary end-points were: nodal progression-free survival (NPFS), progression-free survival (PFS), and toxicity.
Results: A total of 118 lymph node oligometastases from PCa were treated with daily adaptive 1.5 T MR-guided SBRT in 63 oligometastatic patients. Of the patients, 63.5% were oligorecurrent and 36.5% were oligoprogressive. The two-year LPFS was 90.7%. The median NPFS was 22.3 months and the 2-year NPFS was 46.5%. Receiving hormone therapy before SBRT was correlated with a lower NPFS at the multivariate analysis (1 y NPFS 87.1% versus 42.8%;
p = 0.002–HR 0.199, 95% CI 0.073–0.549). Furthermore, the oligorecurrent state during ADT was correlated with a lower NPFS than was the oligoprogressive state. The median PFS was 10.3 months and the 2-year PFS was 32.4%. Patients treated with hormone therapy before SBRT had a significantly lower 1-year PFS the others (28% versus 70.4%;
p = 0.01–HR 0.259, 95% CI 0.117–0.574). No acute and late toxicities occurred during treatment.
Conclusions: The present study is the largest prospective study of 1.5 T lymph node SBRT on MR-linac in patients with PCa. Lymph node SBRT by 1.5 T MR-linac provides high local control rates with an excellent toxicity profile.
Full article
►▼
Show Figures
Open AccessArticle
Evaluation of a New, Highly Flexible Radiofrequency Coil for MR Simulation of Patients Undergoing External Beam Radiation Therapy
by
Kiaran P. McGee, Norbert G. Campeau, Robert J. Witte, Philip J. Rossman, Jackie A. Christopherson, Erik J. Tryggestad, Debra H. Brinkmann, Daniel J. Ma, Sean S. Park, Dan W. Rettmann and Fraser J. Robb
Cited by 2 | Viewed by 1947
Abstract
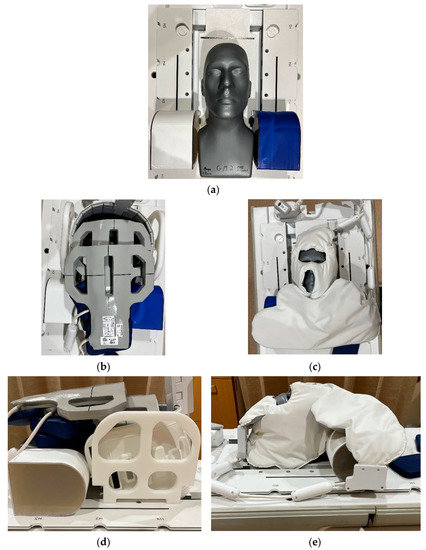
Purpose: To evaluate the performance of a new, highly flexible radiofrequency (RF) coil system for imaging patients undergoing MR simulation. Methods: Volumetric phantom and in vivo images were acquired with a commercially available and prototype RF coil set. Phantom evaluation was performed using
[...] Read more.
Purpose: To evaluate the performance of a new, highly flexible radiofrequency (RF) coil system for imaging patients undergoing MR simulation. Methods: Volumetric phantom and in vivo images were acquired with a commercially available and prototype RF coil set. Phantom evaluation was performed using a silicone-filled humanoid phantom of the head and shoulders. In vivo assessment was performed in five healthy and six patient subjects. Phantom data included T
1-weighted volumetric imaging, while in vivo acquisitions included both T
1- and T
2-weighted volumetric imaging. Signal to noise ratio (SNR) and uniformity metrics were calculated in the phantom data, while SNR values were calculated in vivo. Statistical significance was tested by means of a non-parametric analysis of variance test. Results: At a threshold of
p = 0.05, differences in measured SNR distributions within the entire phantom volume were statistically different in two of the three paired coil set comparisons. Differences in per slice average SNR between the two coil sets were all statistically significant, as well as differences in per slice image uniformity. For patients, SNRs within the entire imaging volume were statistically significantly different in four of the nine comparisons and seven of the nine comparisons performed on the per slice average SNR values. For healthy subjects, SNRs within the entire imaging volume were statistically significantly different in seven of the nine comparisons and eight of the nine comparisons when per slice average SNR was tested. Conclusions: Phantom and in vivo results demonstrate that image quality obtained from the novel flexible RF coil set was similar or improved over the conventional coil system. The results also demonstrate that image quality is impacted by the specific coil configurations used for imaging and should be matched appropriately to the anatomic site imaged to ensure optimal and reproducible image quality.
Full article
►▼
Show Figures
Open AccessReview
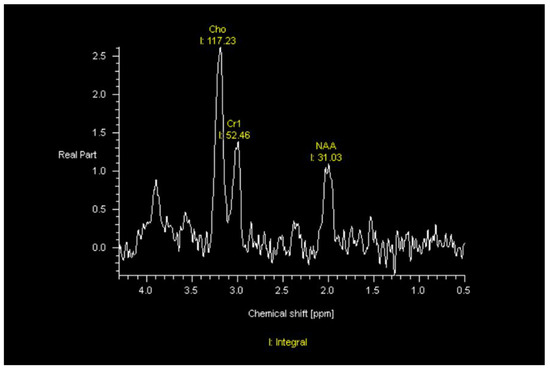
Imaging of GBM in the Age of Molecular Markers and MRI Guided Adaptive Radiation Therapy
by
Salah Dajani, Virginia B. Hill, John A. Kalapurakal, Craig M. Horbinski, Eric G. Nesbit, Sean Sachdev, Amulya Yalamanchili and Tarita O. Thomas
Cited by 4 | Viewed by 3098
Abstract
Glioblastoma (GBM) continues to be one of the most lethal malignancies and is almost always fatal. In this review article, the role of radiation therapy, systemic therapy, as well as the molecular basis of classifying GBM is described. Technological advances in the treatment
[...] Read more.
Glioblastoma (GBM) continues to be one of the most lethal malignancies and is almost always fatal. In this review article, the role of radiation therapy, systemic therapy, as well as the molecular basis of classifying GBM is described. Technological advances in the treatment of GBM are outlined as well as the diagnostic imaging characteristics of this tumor. In addition, factors that affect prognosis such as differentiating progression from treatment effect is discussed. The role of MRI guided radiation therapy and how this technology may provide a mechanism to improve the care of patients with this disease are described.
Full article
►▼
Show Figures
Open AccessReview
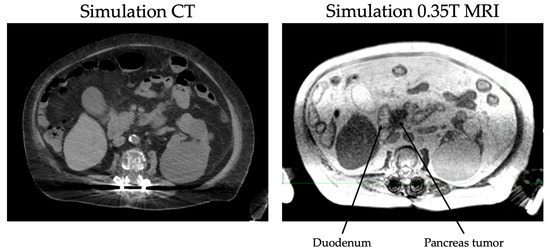
Evolution of Radiation Therapy in Pancreas Cancer Management toward MRI-Guided Adaptive Radiation Therapy
by
Amulya Yalamanchili, Tarita O. Thomas, Salah Dajani and John P. Hayes
Cited by 2 | Viewed by 3549
Abstract
Pancreas cancer has a poor prognosis despite aggressive treatment and is the fourth leading cause of cancer death in the United States. At diagnosis, most patients have either metastatic or locally advanced disease. In this article, we review the evolution of treatments in
[...] Read more.
Pancreas cancer has a poor prognosis despite aggressive treatment and is the fourth leading cause of cancer death in the United States. At diagnosis, most patients have either metastatic or locally advanced disease. In this article, we review the evolution of treatments in locally advanced pancreas cancer (LAPC) and discuss the various radiation therapy fractionation schemes. Furthermore, we examine the data supporting dose escalation and the delivery of ablative biologically effective doses in the setting of LAPC. Finally, we review the role of MRI-guided radiation therapy in escalating dose while sparing organs at risk in the era of stereotactic magnetic resonance-guided adaptive radiation therapy.
Full article
►▼
Show Figures
Open AccessArticle
Emergence of MR-Linac in Radiation Oncology: Successes and Challenges of Riding on the MRgRT Bandwagon
by
Indra J. Das, Poonam Yadav and Bharat B. Mittal
Cited by 7 | Viewed by 3056
Abstract
The special issue of
JCM on “Advances of MRI in Radiation Oncology” provides a unique forum for scientific literature related to MR imaging in radiation oncology. This issue covered many aspects, such as MR technology, motion management, economics, soft-tissue–air interface issues, and disease
[...] Read more.
The special issue of
JCM on “Advances of MRI in Radiation Oncology” provides a unique forum for scientific literature related to MR imaging in radiation oncology. This issue covered many aspects, such as MR technology, motion management, economics, soft-tissue–air interface issues, and disease sites such as the pancreas, spine, sarcoma, prostate, head and neck, and rectum from both camps—the Unity and MRIdian systems. This paper provides additional information on the success and challenges of the two systems. A challenging aspect of this technology is low throughput and the monumental task of education and training that hinders its use for the majority of therapy centers. Additionally, the cost of this technology is too high for most institutions, and hence widespread use is still limited. This article highlights some of the difficulties and how to resolve them.
Full article
►▼
Show Figures
Open AccessReview
History of Technological Advancements towards MR-Linac: The Future of Image-Guided Radiotherapy
by
Nikhil Rammohan, James W. Randall and Poonam Yadav
Cited by 17 | Viewed by 4668
Abstract
Image-guided radiotherapy (IGRT) enables optimal tumor targeting and sparing of organs-at-risk, which ultimately results in improved outcomes for patients. Magnetic resonance imaging (MRI) revolutionized diagnostic imaging with its superior soft tissue contrast, high spatiotemporal resolution, and freedom from ionizing radiation exposure. Over the
[...] Read more.
Image-guided radiotherapy (IGRT) enables optimal tumor targeting and sparing of organs-at-risk, which ultimately results in improved outcomes for patients. Magnetic resonance imaging (MRI) revolutionized diagnostic imaging with its superior soft tissue contrast, high spatiotemporal resolution, and freedom from ionizing radiation exposure. Over the past few years there has been burgeoning interest in MR-guided radiotherapy (MRgRT) to overcome current challenges in X-ray-based IGRT, including but not limited to, suboptimal soft tissue contrast, lack of efficient daily adaptation, and incremental exposure to ionizing radiation. In this review, we present an overview of the technologic advancements in IGRT that led to MRI-linear accelerator (MRL) integration. Our report is organized in three parts: (1) a historical timeline tracing the origins of radiotherapy and evolution of IGRT, (2) currently available MRL technology, and (3) future directions and aspirations for MRL applications.
Full article
►▼
Show Figures
Open AccessArticle
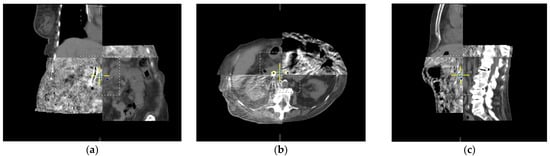
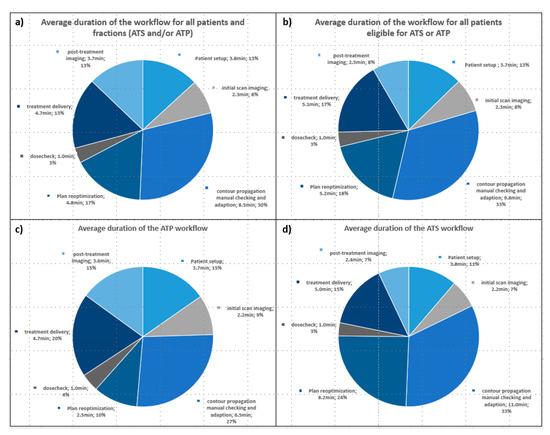
First Experience and Prospective Evaluation on Feasibility and Acute Toxicity of Online Adaptive Radiotherapy of the Prostate Bed as Salvage Treatment in Patients with Biochemically Recurrent Prostate Cancer on a 1.5T MR-Linac
by
Daniel Wegener, Alexandra Thome, Frank Paulsen, Cihan Gani, Jessica Boldt, Sarah Butzer, Daniela Thorwarth, David Moennich, Marcel Nachbar, Arndt-Christian Müller, Daniel Zips and Simon Boeke
Cited by 10 | Viewed by 2459
Abstract
Introduction: Novel MRI-linear accelerator hybrids (MR-Linacs, MRL) promise an optimization of radiotherapy (RT) through daily MRI imaging with enhanced soft tissue contrast and plan adaptation on the anatomy of the day. These features might potentially improve salvage RT of prostate cancer (SRT), where
[...] Read more.
Introduction: Novel MRI-linear accelerator hybrids (MR-Linacs, MRL) promise an optimization of radiotherapy (RT) through daily MRI imaging with enhanced soft tissue contrast and plan adaptation on the anatomy of the day. These features might potentially improve salvage RT of prostate cancer (SRT), where the clinical target volume is confined by the mobile organs at risk (OAR) rectum and bladder. So far, no data exist about the feasibility of the MRL technology for SRT. In this study, we prospectively examined patients treated with SRT on a 1.5 T MRL and report on workflow, feasibility and acute toxicity. Patients and Methods: Sixteen patients were prospectively enrolled within the MRL-01 study (NCT: NCT04172753). All patients were staged and had an indication for SRT after radical prostatectomy according to national guidelines. RT consisted of 66 Gy in 33 fractions or 66.5/70 Gy in 35 fractions in case of a defined high-risk region. On the 1.5 T MRL, daily plan adaption was performed using one of two workflows: adapt to shape (ATS, using contour adaptation and replanning) or adapt to position (ATP, rigid replanning onto the online anatomy with virtual couch shift). Duration of treatment steps, choice of workflow and treatment failure were recorded for each fraction of each patient. Patient-reported questionnaires about patient comfort were evaluated as well as extensive reporting of acute toxicity (patient reported and clinician scored). Results: A total of 524/554 (94.6%) of fractions were successfully treated on the MRL. No patient-sided treatment failures occurred. In total, ATP was chosen in 45.7% and ATS in 54.3% of fractions. In eight cases, ATP was performed on top of the initial ATS workflow. Mean (range) duration of all fractions (on-table time until end of treatment) was 25.1 (17.6–44.8) minutes. Mean duration of the ATP workflow was 20.60 (17.6–25.2) minutes and of the ATS workflow 31.3 (28.2–34.1) minutes. Patient-reported treatment experience questionnaires revealed high rates of tolerability of the treatment procedure. Acute toxicity (RTOG, CTC as well as patient-reported CTC, IPSS and ICIQ) during RT and 3 months after was mild to moderate with a tendency of recovery to baseline levels at 3 months post RT. No G3+ toxicity was scored for any item. Conclusions: In this first report on SRT of prostate cancer patients on a 1.5 T MRL, we could demonstrate the feasibility of both available workflows. Daily MR-guided adaptive SRT of mean 25.1 min per fraction was well tolerated in this pretreated collective, and we report low rates of acute toxicity for this treatment. This study suggests that SRT on a 1.5 T MRL can be performed in clinical routine and it serves as a benchmark for future analyses.
Full article
►▼
Show Figures
Open AccessReview
Towards Accurate and Precise Image-Guided Radiotherapy: Clinical Applications of the MR-Linac
by
James W. Randall, Nikhil Rammohan, Indra J. Das and Poonam Yadav
Cited by 12 | Viewed by 2981
Abstract
Advances in image-guided radiotherapy have brought about improved oncologic outcomes and reduced toxicity. The next generation of image guidance in the form of magnetic resonance imaging (MRI) will improve visualization of tumors and make radiation treatment adaptation possible. In this review, we discuss
[...] Read more.
Advances in image-guided radiotherapy have brought about improved oncologic outcomes and reduced toxicity. The next generation of image guidance in the form of magnetic resonance imaging (MRI) will improve visualization of tumors and make radiation treatment adaptation possible. In this review, we discuss the role that MRI plays in radiotherapy, with a focus on the integration of MRI with the linear accelerator. The MR linear accelerator (MR-Linac) will provide real-time imaging, help assess motion management, and provide online adaptive therapy. Potential advantages and the current state of these MR-Linacs are highlighted, with a discussion of six different clinical scenarios, leading into a discussion on the future role of these machines in clinical workflows.
Full article
►▼
Show Figures
Open AccessArticle
Investigation of Isotoxic Dose Escalation and Plan Quality with TDABC Analysis on a 0.35 T MR-Linac (MRL) System in Ablative 5-Fraction Stereotactic Magnetic Resonance-Guided Radiation Therapy (MRgRT) for Primary Pancreatic Cancer
by
Robert Hawranko, James J. Sohn, Keith Neiderer, Ed Bump, Timothy Harris, Emma C. Fields, Elisabeth Weiss and William Y. Song
Cited by 8 | Viewed by 2225
Abstract
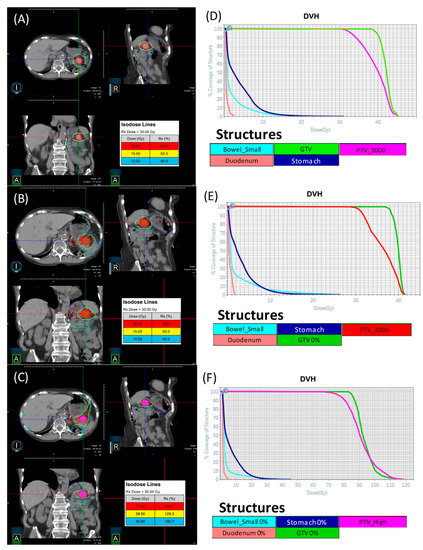
This study investigates plan quality generated by an MR-Linac (MRL) treatment planning system (TPS) for 5-fraction stereotactic body radiation therapy (SBRT) of primary pancreatic cancer (PCa). In addition, an isotoxic dose escalation was investigated with the MRL TPS based on stereotactic MR-guided adaptive
[...] Read more.
This study investigates plan quality generated by an MR-Linac (MRL) treatment planning system (TPS) for 5-fraction stereotactic body radiation therapy (SBRT) of primary pancreatic cancer (PCa). In addition, an isotoxic dose escalation was investigated with the MRL TPS based on stereotactic MR-guided adaptive radiation therapy (SMART) trial constraints. A clinical workflow was developed for adaptive and non-adaptive treatments with the MRL, on which a time-driven activity-based costing (TDABC) analysis was performed to quantify clinical efficacy. Fifteen PCa patients previously treated with a conventional Linac were retrospectively re-planned for this study. Three plans were generated for each patient using the original prescription dose (PD) and organ at risk (OAR) constraints (Plan 1), following SMART trial’s OAR constraints but with the original PD (Plan 2), starting with Plan 2, following an isotoxic dose escalation strategy where the dose was escalated until any one of the SMART trial’s OAR constraints reached its limit (Plan 3). Conformity index (CI) and the ratio of the 50% isodose volume to PTV (R50%) conformity metrics were calculated for all 45 MRL plans, in addition to standard dose-volume indices. Forty-five MRL plans were created which met their respective dosimetric criteria described above. For Plan 1, the MRL TPS successfully achieved equivalent or lower OAR doses while maintaining the prescribed PTV coverage for the 15 plans. A maximum dose to the small bowel was reduced on average by 4.97 Gy (range: 1.11–10.58 Gy). For Plan 2, the MRL TPS successfully met all SMART trial OAR constraints while maintaining equivalent PTV coverage. For Plan 3, the MRL TPS was able to escalate the prescription dose from the original 25–33 Gy by, on average, 36 Gy (range: 15–70 Gy), and dose to the PTV was successfully escalated to at least 50 Gy for all 15 plans. These achievements were made possible, in part, due to the omission of the ITV afforded by the MRL’s real-time target tracking technology and sharper dose penumbra due to its unique dual-focus MLC design. The 0.35T MRL TPS can generate plans that are equivalent to conventional Linac-based plans for SBRT of PCa. Through analyzing Plan 2 and 3 strategies, and due to the real-time target localization capabilities of the MRL system, increased OAR sparing and/or target dose escalation are possible.
Full article
►▼
Show Figures
Open AccessArticle
T1ρ for Radiotherapy Treatment Response Monitoring in Rectal Cancer Patients: A Pilot Study
by
Ernst S. Kooreman, Max Tanaka, Leon C. ter Beek, Femke P. Peters, Corrie A. M. Marijnen, Uulke A. van der Heide and Petra J. van Houdt
Cited by 4 | Viewed by 2325
Abstract
Quantitative MRI has the potential to produce imaging biomarkers for the prediction of early response to radiotherapy treatment. In this pilot study, a potential imaging biomarker, the T
1ρ relaxation time, is assessed for this purpose. A T
1ρ sequence was implemented on
[...] Read more.
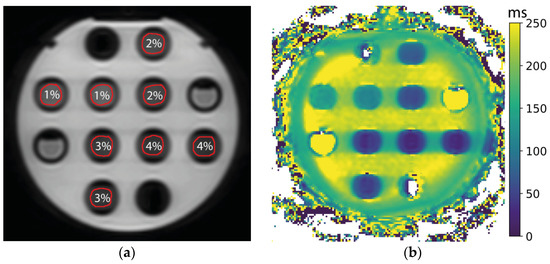
Quantitative MRI has the potential to produce imaging biomarkers for the prediction of early response to radiotherapy treatment. In this pilot study, a potential imaging biomarker, the T
1ρ relaxation time, is assessed for this purpose. A T
1ρ sequence was implemented on a 1.5 T MR-linac system, a system that combines an MRI with a linear accelerator for radiation treatment. An agar phantom with concentrations of 1–4%
w/
w was constructed for technical validation of the sequence. Phantom images were assessed in terms of short-term repeatability and signal-to-noise ratio. Twelve rectal cancer patients, who were treated with 5 × 5 Gy, were imaged on each treatment fraction. Individual changes in the T
1ρ values of the gross tumor volume (GTV) showed an increase for most patients, although a paired
t-test comparing values in the GTV from the first to the last treatment fraction showed no statistically significant difference. The phantom measurements showed excellent short-term repeatability (0.5–1.5 ms), and phantom T
1ρ values corresponded to the literature values. T
1ρ imaging was implemented successfully on the MR-linac, with a repeatability comparable to diagnostic systems, although clinical benefit in terms of treatment response monitoring remains to be demonstrated.
Full article
►▼
Show Figures
Open AccessArticle
Clinical Implementational and Site-Specific Workflows for a 1.5T MR-Linac
by
David A. P. Dunkerley, Daniel E. Hyer, Jeffrey E. Snyder, Joël J. St-Aubin, Carryn M. Anderson, Joseph M. Caster, Mark C. Smith, John M. Buatti and Sridhar Yaddanapudi
Cited by 7 | Viewed by 3473
Abstract
MR-guided adaptive radiotherapy (MRgART) provides opportunities to benefit patients through enhanced use of advanced imaging during treatment for many patients with various cancer treatment sites. This novel technology presents many new challenges which vary based on anatomic treatment location, technique, and potential changes
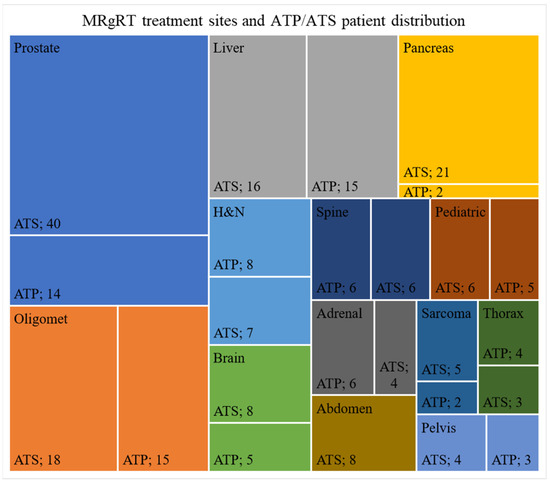
[...] Read more.
MR-guided adaptive radiotherapy (MRgART) provides opportunities to benefit patients through enhanced use of advanced imaging during treatment for many patients with various cancer treatment sites. This novel technology presents many new challenges which vary based on anatomic treatment location, technique, and potential changes of both tumor and normal tissue during treatment. When introducing new treatment sites, considerations regarding appropriate patient selection, treatment planning, immobilization, and plan-adaption criteria must be thoroughly explored to ensure adequate treatments are performed. This paper presents an institution’s experience in developing a MRgART program for a 1.5T MR-linac for the first 234 patients. The paper suggests practical treatment workflows and considerations for treating with MRgART at different anatomical sites, including imaging guidelines, patient immobilization, adaptive workflows, and utilization of bolus.
Full article
►▼
Show Figures
Open AccessReview
Magnetic Resonance Guided Radiotherapy for Head and Neck Cancers
by
Laila A. Gharzai, Benjamin S. Rosen, Bharat Mittal, Michelle L. Mierzwa and Poonam Yadav
Cited by 5 | Viewed by 2703
Abstract
Radiotherapy is an integral component of head/neck squamous cell carcinomas (HNSCCs) treatment, and technological developments including advances in image-guided radiotherapy over the past decades have offered improvements in the technical treatment of these cancers. Integration of magnetic resonance imaging (MRI) into image guidance
[...] Read more.
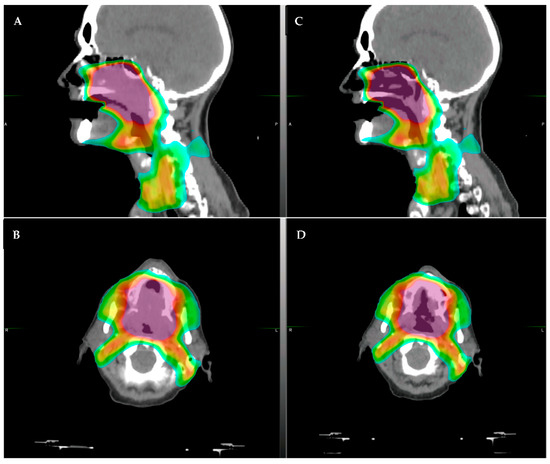
Radiotherapy is an integral component of head/neck squamous cell carcinomas (HNSCCs) treatment, and technological developments including advances in image-guided radiotherapy over the past decades have offered improvements in the technical treatment of these cancers. Integration of magnetic resonance imaging (MRI) into image guidance through the development of MR-guided radiotherapy (MRgRT) offers further potential for refinement of the techniques by which HNSCCs are treated. This article provides an overview of the literature supporting the current use of MRgRT for HNSCC, challenges with its use, and developing research areas.
Full article
►▼
Show Figures
Open AccessArticle
Proposal and Evaluation of a Physician-Free, Real-Time On-Table Adaptive Radiotherapy (PF-ROAR) Workflow for the MRIdian MR-Guided LINAC
by
Jacob C. Ricci, Justin Rineer, Amish P. Shah, Sanford L. Meeks and Patrick Kelly
Cited by 7 | Viewed by 2075
Abstract
With the implementation of MR-LINACs, real-time adaptive radiotherapy has become a possibility within the clinic. However, the process of adapting a patient’s plan is time consuming and often requires input from the entire clinical team, which translates to decreased throughput and limited patient
[...] Read more.
With the implementation of MR-LINACs, real-time adaptive radiotherapy has become a possibility within the clinic. However, the process of adapting a patient’s plan is time consuming and often requires input from the entire clinical team, which translates to decreased throughput and limited patient access. In this study, the authors propose and simulate a workflow to address these inefficiencies in staffing and patient throughput. Two physicians, three radiation therapists (RTT), and a research fellow each adapted bladder and bowel contours for 20 fractions from 10 representative patient plans. Contouring ability was compared via calculation of a Dice Similarity Index (DSI). The DSI for bladder and bowel based on each potential physician–therapist pair, as well as an inter-physician comparison, exhibited good overlap amongst all comparisons (
p = 0.868). Plan quality was compared through calculation of the conformity index (CI), as well as an evaluation of the plan’s dose to a ‘gold standard’ set of structures. Overall, non-physician plans passed 91.2% of the time. Of the eight non-physician plans that failed their clinical evaluation, six also failed their evaluation against the ‘gold standard’. Another two plans that passed their clinical evaluation subsequently failed in their evaluation against the ‘gold standard’. Thus, the PF-ROAR process has a success rate of 97.5%, with 78/80 plans correctly adapted to the gold standard or halted at treatment. These findings suggest that a physician-free workflow can be well tolerated provided RTTs continue to develop knowledge of MR anatomy and careful attention is given to understanding the complexity of the plan prior to treatment.
Full article
►▼
Show Figures
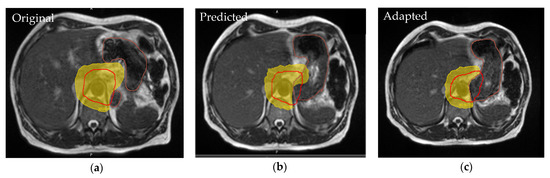
Open AccessReview
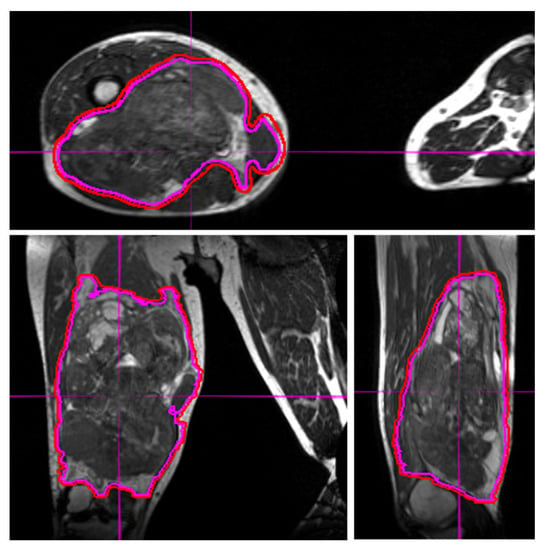
The Role of MRI-Guided Radiotherapy for Soft Tissue Sarcomas
by
Grace C. Blitzer, Poonam Yadav and Zachary S. Morris
Cited by 3 | Viewed by 2286
Abstract
Soft tissue sarcomas (STS) are a rare class of tumors that originate from mesenchymal tissues and occur most frequently in the extremities, trunk, and retroperitoneum. Surgical resection with R0 margins is the primary curative treatment for most localized STS. In this setting, radiation
[...] Read more.
Soft tissue sarcomas (STS) are a rare class of tumors that originate from mesenchymal tissues and occur most frequently in the extremities, trunk, and retroperitoneum. Surgical resection with R0 margins is the primary curative treatment for most localized STS. In this setting, radiation therapy is used either pre-operatively or post-operatively to reduce the rate of local recurrence. Modern pre- or post-operative radiation therapy rely on the use of MRI sequences to guide target delineation during treatment planning. MRI-guided radiotherapy also offers unique advantages over CT-guided approaches in differentiating STS from surrounding normal soft tissues and enabling better identification of target volumes on daily imaging. For patients with unresectable STS, radiation therapy may offer the best chance for local tumor control. However, most STS are relatively radioresistant with modest rates of local control achieved using conventionally fractionated radiation. Specialized techniques such as hypofractionated radiation may allow for dose intensification and may increase rates of local control for STS. In these settings, MRI becomes even more critical for the delineation of targets and organs at risk and management of tumor and organ at risk motion during and between radiotherapy treatment fractions.
Full article
►▼
Show Figures
Open AccessArticle
MRI-Linac Economics II: Rationalizing Schedules
by
Peter A. S. Johnstone, John Kerstiens, Stuart Wasserman and Stephen A. Rosenberg
Cited by 7 | Viewed by 1768
Abstract
Objective: Two benefits of MR-guided radiotherapy (MRgRT) are the ability to track target structures while treatment is being delivered and the ability to adapt plans daily for some lesions based on changing anatomy. These unique capacities come at two costs: increased capital for
[...] Read more.
Objective: Two benefits of MR-guided radiotherapy (MRgRT) are the ability to track target structures while treatment is being delivered and the ability to adapt plans daily for some lesions based on changing anatomy. These unique capacities come at two costs: increased capital for acquisition and greatly decreased workflow. An adaptive gated stereotactic body radiotherapy (MRgART) treatment routinely takes ~90 min to perform and requires the presence of both a physician and a physicist. This may significantly limit daily capacity. We previously described how “simple cases” were necessary for proton facilities to allow for debt management. In this manuscript, we seek to determine the optimal scheduling of different MRgRT plans to recoup capital costs. Materials/Methods: We assumed an MR-linac (MRL) was completely scheduled with patients over workdays of varying duration. Treatment times and reimbursement data from our facility for varying complexities of patients were extrapolated for varying numbers treated daily. We then derived the number of adaptive and non-adaptive patients required daily to optimize the schedules. HOPPS data were used to model reimbursement. Results: A single MRL treating 14 non-gated, non-adaptive IMRT patients over an 8 h workday would take about 4.8 years to cover initial acquisition and installation costs. However, such patients may be more quickly and efficiently treated with a conventional linear accelerator, while MRgART cases may only be treated with an MRL. By treating four of these daily, that same MRL room would cover costs in 2.4 years. Personnel, maintenance costs, and profit further complicate any business case for treating non-adaptive patients or for extending hours. Conclusions: In our previously published paper discussing proton therapy, we noted that debt is not variable with capacity; this remains true with MRgRT. Different from protons, a clinically optimal case load of adaptive patients provides an optimal business case as well. This requires a large patient cadre to ensure continuing throughput. As improvements in MRgRT are brought to the clinic, shorter adaptive and non-adaptive treatment times will help improve the timeframe to recoup costs but will require even more appropriate patients.
Full article
Open AccessArticle
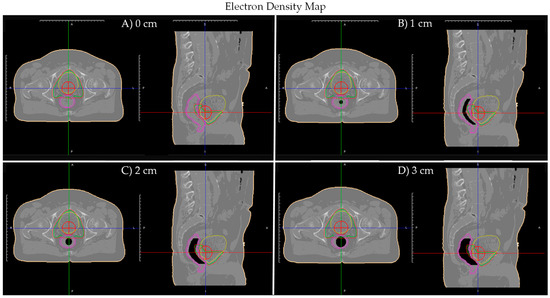
Dosimetric Effects of Air Cavities for MRI-Guided Online Adaptive Radiation Therapy (MRgART) of Prostate Bed after Radical Prostatectomy
by
Jonathan Pham, Minsong Cao, Stephanie M. Yoon, Yu Gao, Amar U. Kishan and Yingli Yang
Cited by 7 | Viewed by 2172
Abstract
Purpose: To evaluate dosimetric impact of air cavities and their corresponding electron density correction for 0.35 tesla (T) Magnetic Resonance-guided Online Adaptive Radiation Therapy (MRgART) of prostate bed patients. Methods: Three 0.35 T MRgRT plans (anterior–posterior (AP) beam, AP–PA beams, and clinical intensity
[...] Read more.
Purpose: To evaluate dosimetric impact of air cavities and their corresponding electron density correction for 0.35 tesla (T) Magnetic Resonance-guided Online Adaptive Radiation Therapy (MRgART) of prostate bed patients. Methods: Three 0.35 T MRgRT plans (anterior–posterior (AP) beam, AP–PA beams, and clinical intensity modulated radiation therapy (IMRT)) were generated on a prostate bed patient’s (Patient A) planning computed tomography (CT) with artificial rectal air cavities of various sizes (0–3 cm, 0.5 cm increments). Furthermore, two 0.35 T MRgART plans (‘Deformed’ and ‘Override’) were generated on a prostate bed patient’s (Patient B) daily magnetic resonance image (MRI) with artificial rectal air cavities of various sizes (0–3 cm, 0.5 cm increments) and on five prostate bed patient’s (Patient 1–5) daily MRIs (2 MRIs: Fraction A and B) with real air cavities. For each MRgART plan, daily MRI electron density map was obtained by deformable registration with simulation CT. In the ‘Deformed’ plan, a clinical IMRT plan is calculated on the daily MRI with electron density map obtained from deformable registration only. In the ‘Override’ plan, daily MRI and simulation CT air cavities are manually corrected and bulk assigned air and water density on the registered electron density map, respectively. Afterwards, the clinical IMRT plan is calculated. Results: For the MRgRT plans, AP and AP–PA plans’ rectum/rectal wall max dose increased with increasing air cavity size, where the 3 cm air cavity resulted in a 20%/17% and 13%/13% increase, relative to no air cavity, respectively. Clinical IMRT plan was robust to air cavity size, where dose change remained less than 1%. For the MRgART plans, daily MRI electron density maps, obtained from deformable registration with simulation CT, was unable to accurately produce electron densities reflecting the air cavities. However, for the artificial daily MRI air cavities, dosimetric change between ‘Deformed’ and ‘Override’ plan was small (<4%). Similarly, for the real daily MRI air cavities, clinical constraint changes between ‘Deformed’ and ‘Override’ plan was negligible and did not lead to change in clinical decision for adaptive planning except for two fractions. In these fractions, the ‘Override’ plan indicated that the bladder max dose and rectum V35.7 exceeded the constraint, while the ‘Deformed’ plan showed acceptable dose, although the absolute difference was only 0.3 Gy and 0.03 cc, respectively. Conclusion: Clinical 0.35 T IMRT prostate bed plans are dosimetrically robust to air cavities. MRgART air cavity electron density correction shows clinically insignificant change and is not warranted on low-field systems.
Full article
►▼
Show Figures
Open AccessArticle
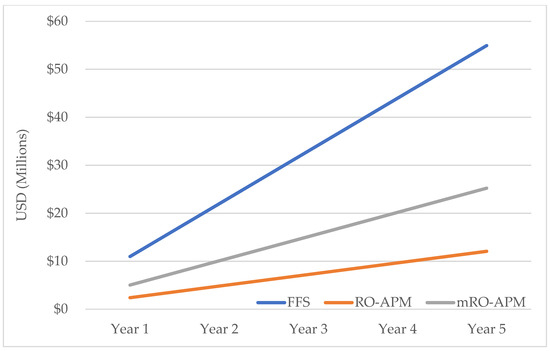
Assessment of MRI-Linac Economics under the RO-APM
by
Russell F. Palm, Kurt G. Eicher, Austin J. Sim, Susan Peneguy, Stephen A. Rosenberg, Stuart Wasserman and Peter A. S. Johnstone
Cited by 3 | Viewed by 2292
Abstract
The implementation of the radiation oncology alternative payment model (RO-APM) has raised concerns regarding the development of MRI-guided adaptive radiotherapy (MRgART). We sought to compare technical fee reimbursement under Fee-For-Service (FFS) to the proposed RO-APM for a typical MRI-Linac (MRL) patient load and
[...] Read more.
The implementation of the radiation oncology alternative payment model (RO-APM) has raised concerns regarding the development of MRI-guided adaptive radiotherapy (MRgART). We sought to compare technical fee reimbursement under Fee-For-Service (FFS) to the proposed RO-APM for a typical MRI-Linac (MRL) patient load and distribution of 200 patients. In an exploratory aim, a modifier was added to the RO-APM (mRO-APM) to account for the resources necessary to provide this care. Traditional Medicare FFS reimbursement rates were compared to the diagnosis-based reimbursement in the RO-APM. Reimbursement for all selected diagnoses were lower in the RO-APM compared to FFS, with the largest differences in the adaptive treatments for lung cancer (−89%) and pancreatic cancer (−83%). The total annual reimbursement discrepancy amounted to −78%. Without implementation of adaptive replanning there was no difference in reimbursement in breast, colorectal and prostate cancer between RO-APM and mRO-APM. Accommodating online adaptive treatments in the mRO-APM would result in a reimbursement difference from the FFS model of −47% for lung cancer and −46% for pancreatic cancer, mitigating the overall annual reimbursement difference to −54%. Even with adjustment, the implementation of MRgART as a new treatment strategy is susceptible under the RO-APM.
Full article
►▼
Show Figures
Open AccessArticle
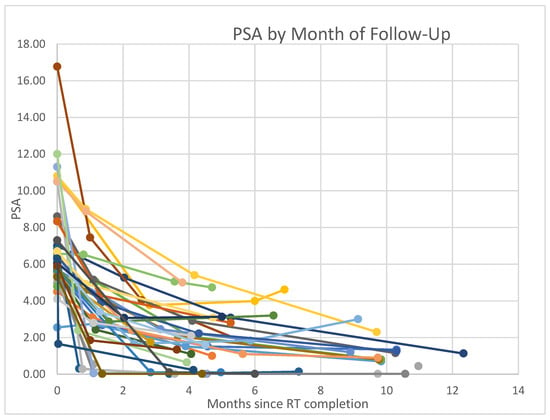
Non-Adaptive MR-Guided Radiotherapy for Prostate SBRT: Less Time, Equal Results
by
Maria L. Sandoval, Irini Youssef, Kujtim Latifi, G. Daniel Grass, Javier Torres-Roca, Stephen Rosenberg, Kosj Yamoah and Peter A. Johnstone
Cited by 14 | Viewed by 2558
Abstract
Background: The use of stereotactic body radiation therapy (SBRT) is widely utilized for treatment of localized prostate cancer. Magnetic-resonance-guided radiotherapy (MRgRT) was introduced in 2014 and has recently been implemented in SBRT for prostate cancer as it provides an opportunity for smaller margins
[...] Read more.
Background: The use of stereotactic body radiation therapy (SBRT) is widely utilized for treatment of localized prostate cancer. Magnetic-resonance-guided radiotherapy (MRgRT) was introduced in 2014 and has recently been implemented in SBRT for prostate cancer as it provides an opportunity for smaller margins and adaptive daily planning. Currently, the only publications of MRgRT for prostate SBRT describe European clinical experiences which utilized adaptive planning. However, adaptive planning adds significantly to the time required for daily treatment. Objectives: Since prostate SBRT has demonstrated acceptable toxicity for several years, we did not consider daily adaptation critical to the process of prostate SBRT. After Institutional Review Board approval, we analyzed and now report our experience using MRgRT without adaptation. Methods: Between 25 September 2019 and 21 December 2020, 35 consecutive patients were treated with MRgRT prostate SBRT at our center. Patients treated with MRgRT included favorable intermediate risk (43%) and unfavorable intermediate risk (54%), and only one patient had low-risk prostate cancer. Nine patients (25%) received adjuvant leuprolide for a median of 4.5 months (range 4–6 m). Our clinical pathway allows for a maximum prostate gland volume of 60 cc; median prostate volume of this cohort was 35.0 cc (range 17–58.4 cc). Median pre-treatment PSA was 6.30 (range 2.55–16.77). Each patient was treated with 36.25 Gy delivered in five fractions over 2 weeks with urethral sparing to a maximal dose of 35 Gy. Target volumes included the prostate gland and proximal seminal vesicles with a 3 mm margin. Results: Median follow-up as of 26 May 2021 was 11.97 months (range 4.37–19.80). First follow-up data are available for all patients, with a median of 1.10 month from completion of treatment (0.63–3.40). The median PSA at first visit was 2.75 (range 0.02–9.00) with a median AUA symptom score of 9 (range 1–24). Second follow-up data are available for 34 patients at a median of 4.45 months (range 2.57–8.90). At second follow-up, the median PSA was 1.60 (range 0.02–5.40) with a median AUA symptom score of 6 (range 1–33). Seventeen patients had third follow-up data with a median of 9.77 months (range 4.70–12.33) after SBRT. The median PSA was 1.13 (range 0.02–4.73) with an AUA score of 9 (2–22) at the third follow-up. We observed a statistically significant decrease in PSA between pre-treatment and at first follow-up (
p < 0.005). The most common toxicity was grade 2 urethritis, managed in all cases by tamsulosin. One patient developed grade 2 tenesmus relieved by topical steroids. No cases of grade ≥ 3 toxicity were seen in our patient population. Conclusions: By avoiding the extra time required for plan adaptation, MRgRT without daily adaptation allows for successful prostate SBRT with manageable toxicity. We continue to reserve our limited adaptive treatment slots for preoperative pancreatic and ultra-central lung SBRT patients, which require time-intensive respiratory gating and adaptive planning.
Full article
►▼
Show Figures
Planned Papers
The below list represents only planned manuscripts. Some of these
manuscripts have not been received by the Editorial Office yet. Papers
submitted to MDPI journals are subject to peer-review.
- Role of Low Field MRI in Radiation Oncology
- Synthetic CT and Its Role in Management of Radiation Therapy
- Deep Learning: A New Paradigm for Electron Density Mapping in MRI-Only Radiotherapy
- MRI Guided Radiotherapy in the Treatment of Brain Tumors
- First Results of Prostate Cancer Salvage RT on A 1.5T MRL