Obesity: From Diagnosis to Treatment (Closed)
A topical collection in Journal of Clinical Medicine (ISSN 2077-0383). This collection belongs to the section "Endocrinology & Metabolism".
Viewed by 61347Editor
Interests: obesity; anastomosis gastric bypass; morbid obesity; esophagus
Topical Collection Information
Dear Colleagues,
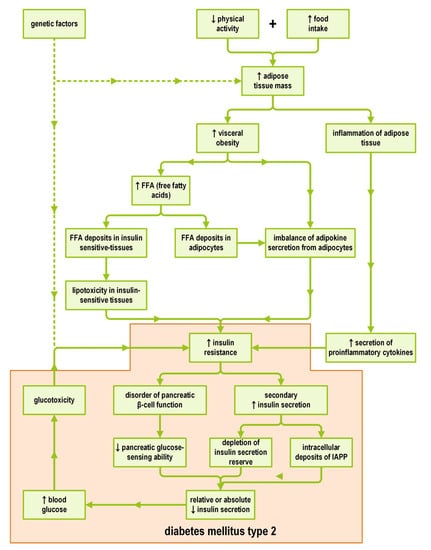
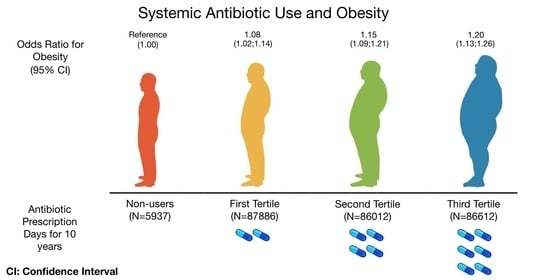
Obesity is a chronic disease with a very negative impact on health. According to the World Health Organization, 39% of adults worldwide are overweight and 13% are obese. The number of obesity cases has almost tripled since 1975. Obesity is a known risk factor for type 2 diabetes, high blood pressure, metabolic syndrome, sleep apnea, fatty liver disease, and many other comorbid conditions.
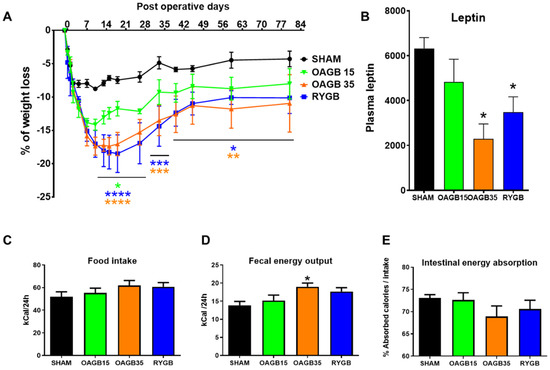
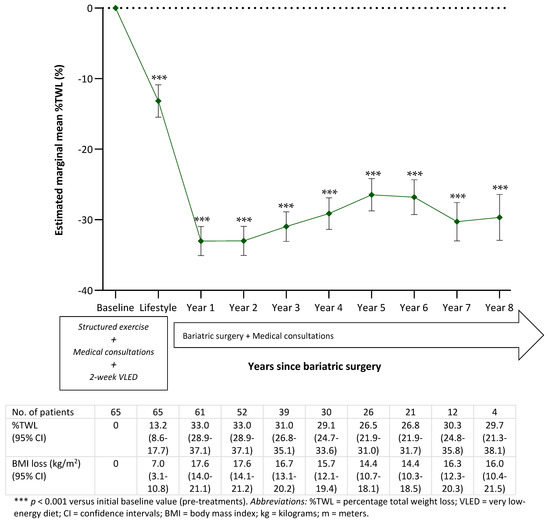
Currently, bariatric surgery is the standard treatment for obesity, resulting in significant and lasting weight loss and reducing comorbidities in patients. Despite being a relatively young medical specialty, over these last two decades bariatric and metabolic surgery has had a very sustained development. Some interventions have disappeared, others, even more efficient and secure, have appeared.
This last year, a collective awakening took place due to the COVID-19 pandemic, which highlighted that obesity was an independent factor of mortality causing devastation in the population suffering from obesity. We must meet this challenge. This evolution and perpetual improvement is only possible thanks to clinical and scientific research reported by different teams through publications.
We invite you to submit your research in the field of bariatric and metabolic surgery and nutrition, focusing on all aspects (challenge, trends, and prospects) that can improve our daily practices.
Dr. Tigran Poghosyan
Guest Editor
Manuscript Submission Information
Manuscripts should be submitted online at www.mdpi.com by registering and logging in to this website. Once you are registered, click here to go to the submission form. Manuscripts can be submitted until the deadline. All submissions that pass pre-check are peer-reviewed. Accepted papers will be published continuously in the journal (as soon as accepted) and will be listed together on the collection website. Research articles, review articles as well as short communications are invited. For planned papers, a title and short abstract (about 100 words) can be sent to the Editorial Office for announcement on this website.
Submitted manuscripts should not have been published previously, nor be under consideration for publication elsewhere (except conference proceedings papers). All manuscripts are thoroughly refereed through a single-blind peer-review process. A guide for authors and other relevant information for submission of manuscripts is available on the Instructions for Authors page. Journal of Clinical Medicine is an international peer-reviewed open access semimonthly journal published by MDPI.
Please visit the Instructions for Authors page before submitting a manuscript. The Article Processing Charge (APC) for publication in this open access journal is 2600 CHF (Swiss Francs). Submitted papers should be well formatted and use good English. Authors may use MDPI's English editing service prior to publication or during author revisions.
Keywords
- obesity
- bariatric and metabolic surgery
- nutrition
- gastric bypass
- sleeve gastrectomy
- SADI-S
- diabetes
- vitamin supplementation
- SARS-CoV-2/COVID-19
- nutritional complications