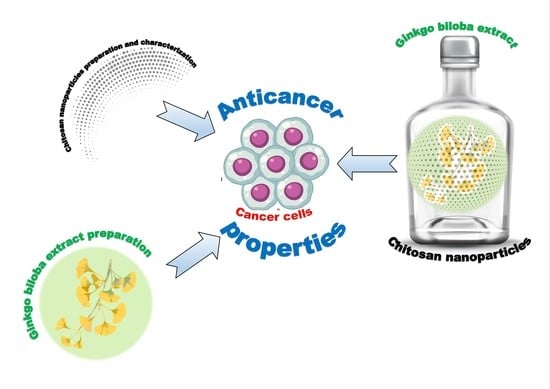
Chitosan Nanoparticles-Preparation, Characterization and Their Combination with Ginkgo biloba Extract in Preliminary In Vitro Studies
Abstract
:1. Introduction
2. Results
2.1. Characteristic of Ch(GB)NPs
2.2. Encapsulation and Loading of GBE Efficiency (GBE EE%)
2.3. Kinetics of Core Material Release
2.4. FT-IR Analysis
2.5. Cytotoxic Effect
3. Discussion
4. Materials and Methods
4.1. Materials
4.2. Methods
4.2.1. Preparation of Ch(GB)NPs
4.2.2. Characterization of Ch(GB)NPs
The Size Analysis of Ch(GB)NPs
The Morphology of Ch(GB)NPs
4.2.3. Encapsulation and Loading Efficiency
4.2.4. The Rate of Release of GBE from Ch(GB)NPs
4.2.5. FT-IR Analysis
4.2.6. Cell Culture
4.2.7. MTT Assay for Cell Viability
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kobus-Cisowska, J.; Flaczyk, E.; Siger, A.; Kmiecik, D. Effect of the extraction process on yield and composition of selected extracts from maidenhair tree green and yellow leaves. Nauka Przyr. Technol. 2015, 9, 1–15. [Google Scholar] [CrossRef] [Green Version]
- Sabaner, M.C.; Dogan, M.; Altin, S.S.; Balaman, C.; Yilmaz, C.; Omur, A.; Zeybek, I.; Palaz, M. Ginkgo Biloba affects microvascular morphology: A prospective optical coherence tomography angiography pilot study. Int. Ophthalmol. 2021, 41, 1053–1061. [Google Scholar] [CrossRef] [PubMed]
- Karavelioglu, Z.; Cakir-Koc, R. Preparation of chitosan nanoparticles as Ginkgo Biloba extract carrier: In vitro neuroprotective effect on oxidative stress-induced human neuroblastoma cells (SH-SY5Y). Int. J. Biol. Macromol. 2021, 192, 675–683. [Google Scholar] [CrossRef] [PubMed]
- Singh, B.; Kaur, P.; Gopichand; Singh, R.D.; Ahuja, P.S. Biology and chemistry of Ginkgo biloba. Fitoterapia 2008, 79, 401–418. [Google Scholar] [CrossRef]
- Wang, L.; Zhao, X.; Yang, F.; Wu, W.; Liu, Y.; Wang, L.; Wang, L.; Wang, Z. Enhanced bioaccessibility in vitro and bioavailability of Ginkgo biloba extract nanoparticles prepared by liquid anti-solvent precipitation. Int. J. Food Sci. Technol. 2019, 54, 2266–2276. [Google Scholar] [CrossRef]
- Maeda, J.; Inoue, K.; Ichimura, R.; Takahashi, M.; Kodama, Y.; Saito, N.; Yoshida, M. Essential role of constitutive androstane receptor in Ginkgo biloba extract induced liver hypertrophy and hepatocarcinogenesis. Food Chem. Toxicol. 2015, 83, 201–209. [Google Scholar] [CrossRef]
- Sati, S.C.; Joshi, S. Antibacterial activities of Ginkgo biloba L. leaf extracts. Sci. World J. 2011, 11, 2237–2242. [Google Scholar] [CrossRef] [Green Version]
- Tsuruda, T. Herbal dietary supplement: Continuing to explore cardiovascular protection. Cardiovasc. Res. 2010, 88, 387–388. [Google Scholar] [CrossRef] [Green Version]
- Wang, Y.; Lv, J.; Cheng, Y.; Du, J.; Chen, D.; Li, C.; Zhang, J. Apoptosis Induced by Ginkgo biloba (EGb761) in Melanoma Cells Is Mcl-1-Dependent. PLoS ONE 2015, 10, e0124812. [Google Scholar] [CrossRef]
- Ma, J.; Duan, W.; Han, S.; Lei, J.; Xu, Q.; Chen, X.; Jiang, Z.; Nan, L.; Li, J.; Chen, K.; et al. Ginkgolic acid suppresses the development of pancreatic cancer by inhibiting pathways driving lipogenesis. Oncotarget 2015, 6, 20993–21003. [Google Scholar] [CrossRef] [Green Version]
- DeFeudis, F.; Drieu, K. Ginkgo biloba extract (EGb 761) and CNS functions basic studies and clinical applications. Curr. Drug Targets 2005, 1, 25–58. [Google Scholar] [CrossRef] [Green Version]
- Pereira, E.; Barros, L.; Ferreira, I. Chemical characterization of Ginkgo biloba L. and antioxidant properties of its extracts and dietary supplements. Ind. Crops Prod. 2013, 51, 244–248. [Google Scholar] [CrossRef]
- Cheng, S.Y.; Zhang, W.W.; Sun, N.N.; Xu, F.; Li, L.; Liao, Y.; Cheng, H. Production of flavonoids and terpene lactones from optimized Ginkgo biloba tissue culture. Not. Bot. Horti Agrobo. 2014, 42, 88–93. [Google Scholar] [CrossRef] [Green Version]
- Lukasiewicz, M.; Kowalski, S.; Kulig, M.; Gambus, H.; Achremowicz, B. Antioxidant activity of quercetin water solutions containing beta-cyclodextrin. Acta Agrophysica 2013, 20, 423–435. [Google Scholar]
- Periferakis, A.; Periferakis, K.; Badarau, I.A.; Petran, E.M.; Popa, D.C.; Caruntu, A.; Costache, R.S.; Scheau, C.; Caruntu, C.; Costache, D.O. Kaempferol: Antimicrobial Properties, Sources, Clinical, and Traditional Applications. Int. J. Mol. Sci. 2022, 23, 15054. [Google Scholar] [CrossRef]
- Jnawali, H.N.; Jeon, D.; Jeong, M.C.; Lee, E.; Jin, B.; Ryoo, S.; Yoo, J.; Jung, I.D.; Lee, S.J.; Park, Y.M.; et al. Antituberculosis Activity of a Naturally Occurring Flavonoid, Isorhamnetin. J. Nat. Prod. 2016, 79, 961–969. [Google Scholar] [CrossRef]
- van Beek, T.A. Ginkgolides and bilobalide: Their physical, chromatographic and spectroscopic properties. Bioorg. Med. Chem. 2005, 13, 5001–5012. [Google Scholar] [CrossRef]
- Ma, Y.-C.; Mani, A.; Cai, Y.; Thomson, J.; Ma, J.; Peudru, F.; Chen, S.; Luo, M.; Zhang, J.; Chapman, R.G.; et al. An effective identification and quantification method for Ginkgo biloba flavonol glycosides with targeted evaluation of adulterated products. Phytomedicine 2016, 23, 377–387. [Google Scholar] [CrossRef]
- Ganeshpurkar, A.; Saluja, A.K. The Pharmacological Potential of Rutin. Saudi Pharm. J. 2017, 25, 149–164. [Google Scholar] [CrossRef] [Green Version]
- Palmer, B.; DeLouise, L. Nanoparticle-Enabled Transdermal Drug Delivery Systems for Enhanced Dose Control and Tissue Targeting. Molecules 2016, 21, 1719. [Google Scholar] [CrossRef] [Green Version]
- Carter, P.; Narasimhan, B.; Wang, Q. Biocompatible Nanoparticles and Vesicular Systems in Transdermal Drug Delivery for Various Skin Diseases. Int. J. Pharm. 2019, 30, 49–62. [Google Scholar] [CrossRef] [PubMed]
- Bartkowiak, A.; Brylak, W. Hydrogel microcapsules containing natural or chemically modified oligochitosan—Mechanical properties and porosity. Polimery 2006, 51, 7–8, 547–554. [Google Scholar] [CrossRef] [Green Version]
- Goyal, R.; Macri, L.K.; Kaplan, H.M.; Kohn, J. Nanoparticles and nanofibers for topical drug delivery. J. Control Release 2016, 240, 77–92. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yuan, L.; Pan, M.; Shi, K.; Hu, D.; Li, Y.; Chen, Y.; Qian, Z. Nanocarriers for promoting skin delivery of therapeutic agents. Appl. Mater. Today 2022, 27, 101438. [Google Scholar] [CrossRef]
- Zheng, Z.; Tsai, P.C.; Ramezanli, T.; Michniak-Kohn, B.B. Polymeric nanoparticles-based topical delivery systems for the treatment of dermatological diseases. WIRes Nanomed. Nanobiotechnol. 2013, 5, 205–218. [Google Scholar] [CrossRef] [Green Version]
- Sowmya, C.; Suryaprakash Reddy, C.; Amrutha, V.; Anilkumar, D.; Lohitha, M. Transdermal therapeutic systems—An overview. Int. J. Pharm. Biol. Arch. 2012, 2, 197–211. [Google Scholar]
- Bojarczuk, K.A.; Lewicki, M.; Michalczak, M.; Smoleń, A. Evaluation of students’ knowledge about skin care. J. Educ. Health Sport 2016, 6, 661–676. [Google Scholar]
- McGrath, J.A.; Uitto, J. Anatomy and organization of human skin. In Rook’s Textbook of Dermatology, 9th ed.; Griffiths, C.E.M., Barker, J., Bleiker, T.O., Chalmers, R., Creamer, D., Eds.; Wiley-Blackwell: Oxford, UK, 2016; Volume 8, pp. 1–53. [Google Scholar]
- Malinowska, M.; Sikora, E.; Ogonowski, J. Percutaneous penetration of active cosmetics ingredients. Wiad. Chem. 2013, 67, 321–344. [Google Scholar]
- Benson, H.A. Transdermal drug delivery: Penetration enhancement techniques. Curr. Drug Deliv. 2005, 2, 23–33. [Google Scholar] [CrossRef]
- Knorr, F.; Lademann, J.; Patzelt, A.; Sterry, W.; Blume-Peytavi, U.; Vogt, A. Follicular transport route– research progress and future perspectives. Eur. J. Pharm. Biopharm. 2009, 71, 173–180. [Google Scholar] [CrossRef]
- Czerwonka, W.; Puchalska, D.; Lipińska, M.; Habrat, A. Mechanisms and methods of active ingredients penetration through the skin lipid barier. Kosmetol. Estet. 2018, 7, 667–671. [Google Scholar]
- Patzelt, A.; Richter, H.; Knorr, F.; Schafer, U.; Lehr, C.M.; Daehne, L.; Sterry, W.; Lademann, J. Selective follicular targeting by modification of the particle sizes. J. Control Release 2011, 150, 45–48. [Google Scholar] [CrossRef]
- Abdel-Hafez, S.M.; Hathout, R.M.; Sammour, O.A. Tracking the transdermal penetration pathways of optimized curcumin-loaded chitosan nanoparticles via confocal laser scanning microscopy. Int. J. Biol. Macromol. 2018, 108, 753–764. [Google Scholar] [CrossRef]
- Lademann, J.; Richter, H.; Teichmann, A.; Otberg, N.; Blume-Peytavi, U.; Luengo, J.; Weiss, B.; Schaefer, U.L.; Lehr, C.M.; Wepf, R.; et al. Nanoparticles—An efficient carrier for drug delivery into the hair follicles. Eur. J. Pharm. Biopharm. 2007, 66, 159–164. [Google Scholar] [CrossRef]
- Saravanakumar, K.; Mariadoss, A.V.A.; Sathiyaseelan, A.; Wang, M.H. Synthesis and characterization of nano-chitosan capped gold nanoparticles with multifunctional bioactive properties. Int. J. Biol. Macromol. 2020, 165, 747–757. [Google Scholar] [CrossRef]
- Herdiana, Y.; Wathoni, N.; Shamsuddin, S.; Muchtaridi, M. Drug release study of the chitosan-based nanoparticles. Heliyon 2022, 8, e08674. [Google Scholar] [CrossRef]
- George, D.; Maheswari, P.U.; Begum, K.M.M.S. Chitosan-cellulose hydrogel conjugated with L-histidine and zinc oxide nanoparticles for sustained drug delivery: Kinetics and in-vitro biological studies. Carbohydr. Polym. 2020, 236, 116101. [Google Scholar] [CrossRef]
- Katas, H.; Raja, M.A.G.; Lam, K.L. Development of Chitosan Nanoparticles as a Stable Drug Delivery System for Protein/siRNA. Int. J. Biomater. 2013, 2013, 146320. [Google Scholar] [CrossRef] [Green Version]
- Weng, J.; Tong, H.H.Y.; Chow, S.F. In vitro release study of the polymeric drug nanoparticles: Development and validation of a novel method. Pharmaceutics 2020, 12, 732. [Google Scholar] [CrossRef]
- Quiñones, J.P.; Szopko, R.; Schmidt, C.; Covas, C.P. Novel drug delivery systems: Chitosan conjugates covalently attached to steroids with potential anticancer and agrochemical activity. Carbohydr. Polym. 2011, 84, 858–864. [Google Scholar] [CrossRef]
- Thai, H.; Nguyen, C.T.; Thach, L.T.; Tran, M.T.; Mai, H.D.; Nguyen, T.T.T.; Le, G.D.; Can, M.V.; Tran, L.D.; Bach, G.L.; et al. Characterization of chitosan/alginate/lovastatin nanoparticles and investigation of their toxic effects in vitro and in vivo. Sci. Rep. 2020, 10, 909. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Patel, R.; Gajra, B.; Rh, P.; Patel, G. Ganciclovir loaded chitosan nanoparticles preparation and charakterization. J. Nanomed. Nanotechnol. 2016, 7, 411. [Google Scholar]
- Son, G.H.; Lee, B.J.; Cho, C.W. Mechanisms of drug release from advanced drug formulations such as polymeric-based drug-delivery systems and lipid nanoparticles. J. Pharm. Investig. 2017, 47, 287–296. [Google Scholar] [CrossRef]
- Jonassen, H.; Kjøniksen, A.L.; Hiorth, M. Effects of ionic strength on the size and compactness of chitosan nanoparticles. Colloid Polym. Sci. 2012, 290, 919–929. [Google Scholar] [CrossRef]
- Kim, S.J.; Lim, M.H.; Chun, I.K.; Won, Y.H. Effects of Flavonoids of Ginkgo biloba on Proliferation of human skin fibroblast. Skin Pharmacol. 1997, 10, 200–205. [Google Scholar] [CrossRef]
- Chao, C.J.; Chu, C.C. Effects of Ginkgo biloba extract on cell proliferation and cytotoxicity in human hepatocellular carcinoma cells. World J. Gastroenterol. 2004, 10, 37–41. [Google Scholar] [CrossRef]
- Lee, K.H.; Kim, K.C.; Jung, Y.J.; Ham, Y.H.; Jang, J.J.; Kwon, H.; Sung, Y.C.; Kim, S.H.; Han, S.K.; Kim, C.M. Induction of apoptosis in p53-deficient human hepatoma cell line by wild-type p53 gene transduction: Inhibition by antioxidant. Mol. Cells 2001, 12, 17–24. [Google Scholar]
- Su, Y.; Sun, C.M.; Chuang, H.H.; Chang, P.T. Studies on the cytotoxic mechanisms of ginkgetin in a human ovarian adenocarcinoma cell line. Naunyn. Schmiedebergs. Arch. Pharmacol. 2000, 362, 82–90. [Google Scholar] [CrossRef]
- Ding, J.; Guo, Y. Recent advances in chitosan and its derivatives in cancer treatment. Front. Pharmacol. 2022, 13, 888740. [Google Scholar] [CrossRef]
- Qi, L.; Xu, Z.; Jiang, X.; Li, Y.; Wang, M. Cytotoxic activities of chitosan nanoparticles and copper-loaded nanoparticles. Bioorg. Med. Chem. Lett. 2005, 15, 1397–1399. [Google Scholar] [CrossRef]
- Qi, L.F.; Xu, Z.R.; Li, Y.; Jiang, X.; Han, X.Y. In vitro effects of chitosan nanoparticles on proliferation of human gastric carcinoma cell line MGC803 cells. World J. Gastroenterol. 2005, 11, 5136–5141. [Google Scholar]
- Loh, J.W.; Saunders, M.; Lim, L.Y. Cytotoxicity of Monodispersed Chitosan Nanoparticles against the Caco-2 Cells. Toxicol. Appl. Pharmacol. 2012, 262, 273–282. [Google Scholar] [CrossRef]
- Ghaheh, F.S.; Khoddami, A.; Alihosseini, F.; Gomes, A.; Ribeiro, A.; Cavaco-Paulo, A.; Silva, C. Protein-based nanoformulations for α-tocopherol encapsulation. Eng. Life Sci. 2016, 17, 523–527. [Google Scholar] [CrossRef] [Green Version]
- Calvo, P.; Remunan-Lopez, C.; Vila-Jato, J.L.; Alonso, M.J. Novel hydrophilic chitosan-polyethylene oxide nanoparticles as protein carriers. J. Appl. Polym. Sci. 1997, 63, 125–132. [Google Scholar] [CrossRef]
- Porras-Gómez, M.; Vega-Baudrit, J.; Núñez-Corrales, S. Ampicillin-loaded chitosan nanoparticles for in vitro antimicrobial screening on Escherichia coli. In Chitin-Chitosan-Myriad Functionalities in Science and Technology, 1st ed.; Dongre, R.S., Ed.; IntechOpen: London, UK, 2018; pp. 245–258. [Google Scholar]
- Siepmann, J.; Podual, K.; Sriwongjanya, M.; Peppas, N.A.; Bodmeier, R. A new model describing the swelling and drug release kinetics from hydroxypropyl methylcellulose tablets. J. Pharm. Sci. 1999, 88, 65–72. [Google Scholar] [CrossRef]






| Sample | Sonification (min) | Size (nm) | PDI |
|---|---|---|---|
| Ch(GB)NPs | - | 454.2 | 0.549 |
| Ch(GB)NPs | 5 | 374.9 | 0.512 |
| Ch(GB)NPs | 10 | 358.9 | 0.474 |
| Drug Release Model | Medium—Water (Sample A) | Medium—Saline (Sample B) |
|---|---|---|
| Zero order | 0.8298 | 0.8823 |
| First order | 0.8552 | 0.9104 |
| Higuchi | 0.9204 | 0.8586 |
| Korsmeyer–Peppas | 0.8608 | 0.8317 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Owczarek, M.; Herczyńska, L.; Sitarek, P.; Kowalczyk, T.; Synowiec, E.; Śliwiński, T.; Krucińska, I. Chitosan Nanoparticles-Preparation, Characterization and Their Combination with Ginkgo biloba Extract in Preliminary In Vitro Studies. Molecules 2023, 28, 4950. https://doi.org/10.3390/molecules28134950
Owczarek M, Herczyńska L, Sitarek P, Kowalczyk T, Synowiec E, Śliwiński T, Krucińska I. Chitosan Nanoparticles-Preparation, Characterization and Their Combination with Ginkgo biloba Extract in Preliminary In Vitro Studies. Molecules. 2023; 28(13):4950. https://doi.org/10.3390/molecules28134950
Chicago/Turabian StyleOwczarek, Monika, Lucyna Herczyńska, Przemysław Sitarek, Tomasz Kowalczyk, Ewelina Synowiec, Tomasz Śliwiński, and Izabella Krucińska. 2023. "Chitosan Nanoparticles-Preparation, Characterization and Their Combination with Ginkgo biloba Extract in Preliminary In Vitro Studies" Molecules 28, no. 13: 4950. https://doi.org/10.3390/molecules28134950
APA StyleOwczarek, M., Herczyńska, L., Sitarek, P., Kowalczyk, T., Synowiec, E., Śliwiński, T., & Krucińska, I. (2023). Chitosan Nanoparticles-Preparation, Characterization and Their Combination with Ginkgo biloba Extract in Preliminary In Vitro Studies. Molecules, 28(13), 4950. https://doi.org/10.3390/molecules28134950