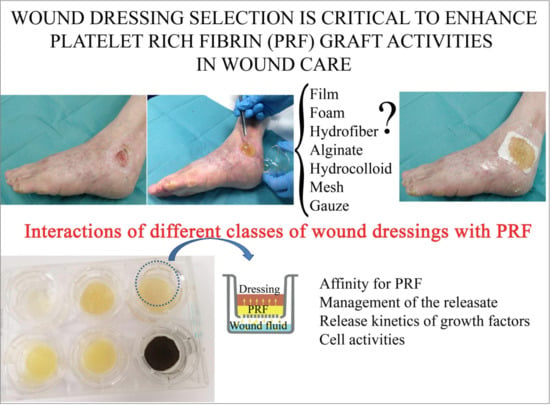
Wound Dressing Selection Is Critical to Enhance Platelet-Rich Fibrin Activities in Wound Care
Abstract
:1. Introduction
2. Results
2.1. PRP and PRF-Releasate Characterization
2.2. PR-Fibrin Stability
2.3. Affinity for PRF Differed Depending on Wound Dressing Composition
2.4. PRF Releasate Management
2.5. PDGF-BB Release Kinetics
2.6. Cell Experiments
3. Discussion
4. Materials and Methods
4.1. Platelet-Rich Fibrin (PRF)
4.2. Stability of PR-Fibrin Graft
4.3. Interaction of Different Wound Dressing Classes with PRF
4.3.1. Affinity of Different Wound Dressing Types for PRF
4.3.2. Assessment of Releasate Management (Retention/Extrusion)
4.4. Assessment of the Release Profile of PDGF-BB
4.5. Cell Culture
4.6. The Influence of Combination Products’ Releasates in Cell Behavior
4.6.1. Cell Proliferation Assay
4.6.2. Cell Adhesion Assay
4.7. Statistical Analyses
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Burgos-Alonso, N.; Lobato, I.; Hernández, I.; Sebastian, K.S.; Rodríguez, B.; Grandes, G.; Andia, I. Adjuvant Biological Therapies in Chronic Leg Ulcers. Int. J. Mol. Sci. 2017, 18, 2561. [Google Scholar] [CrossRef] [Green Version]
- Han, G.; Ceilley, R. Chronic Wound Healing: A Review of Current Management and Treatments. Adv. Ther. 2017, 34, 599–610. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Russell, D.; Atkin, L.; Betts, A.; Dowsett, C.; Fatoye, F.; Gardner, S.; Green, J.; Manu, C.; McKenzie, T.; Meally, H.; et al. Using a modified Delphi methodology to gain consensus on the use of dressings in chronic wounds management. J. Wound Care 2018, 27, 156–165. [Google Scholar] [CrossRef] [PubMed]
- Andia, I.; Abate, M. Platelet-rich plasma: Underlying biology and clinical correlates. Regen. Med. 2013, 8, 645–658. [Google Scholar] [CrossRef] [PubMed]
- Krupski, W.C.; Reilly, L.M.; Perez, S.; Moss, K.M.; Crombleholme, P.A.; Rapp, J.H. A prospective randomized trial of autologous platelet-derived wound healing factors for treatment of chronic nonhealing wounds: A preliminary report. J. Vasc. Surg. 1991, 14, 526–532. [Google Scholar] [CrossRef] [Green Version]
- Andia, I.; Maffulli, N. Platelet-rich plasma for managing pain and inflammation in osteoarthritis. Nat. Rev. Rheumatol. 2013, 9, 721–730. [Google Scholar] [CrossRef]
- Barsotti, M.C.; Losi, P.; Briganti, E.; Sanguinetti, E.; Magera, A.; Al Kayal, T.; Feriani, R.; Di Stefano, R.; Soldani, G. Effect of platelet lysate on human cells involved in different phases of wound healing. PLoS ONE 2013, 8, e84753. [Google Scholar] [CrossRef]
- Notodihardjo, S.C.; Morimoto, N.; Kakudo, N.; Mitsui, T.; Le, T.M.; Tabata, Y.; Kusumoto, K. Efficacy of Gelatin Hydrogel Impregnated With Concentrated Platelet Lysate in Murine Wound Healing. J. Surg. Res. 2019, 234, 190–201. [Google Scholar] [CrossRef]
- Marrazzo, P.; Paduano, F.; Palmieri, F.; Marreli, M.; Tatullo, M. Highly Efficient In Vitro Reparative Behaviour of Dental Pulp Stem Cells Cultured with Standardised Platelet Lysate Supplementation. Stem Cells Int. 2016, 2016, 7230987. [Google Scholar] [CrossRef] [Green Version]
- Krijgsveld, J.; Zaat, S.A.; Meeldijk, J.; van Veelen, P.A.; Fang, G.; Poolman, B.; Brandt, E.; Ehlert, J.E.; Kuijpers, A.J.; Engbers, G.H.; et al. Thrombocidins, microbicidal proteins from human blood platelets, are C-terminal deletion products of CXC chemokines. J. Biol. Chem. 2000, 275, 20374–20381. [Google Scholar] [CrossRef] [Green Version]
- Harrison, P.; Subcommittee on Platelet Physiology. The use of platelets in regenerative medicine and proposal for a new classification system: Guidance from the SSC of the ISTH. J. Thromb. Haemost. 2018, 16, 1895–1900. [Google Scholar] [CrossRef]
- Çetinkaya, R.A.; Yenilmez, E.; Petrone, P.; Yılmaz, S.; Bektöre, B.; Şimsek, B.; Kula Atik, T.; Özyurt, M.; Ünlü, A. Platelet-rich plasma as an additional therapeutic option for infected wounds with multi-drug resistant bacteria: In vitro antibacterial activity study. Eur. J. Trauma Emerg. Surg. 2019, 45, 555–565. [Google Scholar] [CrossRef]
- Draxler, D.F.; Sashindranath, M.; Medcalf, R.L. Plasmin: A Modulator of Immune Function. Semin. Thromb. Hemost. 2017, 43, 143–153. [Google Scholar] [CrossRef]
- Del Pino-Sedeño, T.; Trujillo-Martín, M.M.; Andia, I.; Aragón-Sánchez, J.; Herrera-Ramos, E.; Iruzubieta Barragán, F.J.; Serrano-Aguilar, P. Platelet-rich plasma for the treatment of diabetic foot ulcers: A meta-analysis. Wound Repair Regen. 2019, 27, 170–182. [Google Scholar] [CrossRef]
- Xia, Y.J.; Zhao, J.; Xie, J.; Lv, Y.; Cao, D.S. The Efficacy of Platelet-Rich Plasma Dressing for Chronic Nonhealing Ulcers: A Meta-Analysis of 15 Randomized Controlled Trials. Plast. Reconstr. Surg. 2019, 144, 1463–1474. [Google Scholar] [CrossRef]
- Heijnen, H.; van der Sluijs, P. Platelet secretory behaviour: As diverse as the granules … or not? J. Thromb. Haemost. 2015, 13, 2141–2151. [Google Scholar] [CrossRef] [PubMed]
- Taniguchi, Y.; Yoshioka, T.; Sugaya, H.; Gosho, M.; Aoto, K.; Kanamori, A.; Yamazaki, M. Growth factor levels in leukocyte-poor platelet-rich plasma and correlations with donor age, gender, and platelets in the Japanese population. J. Exp. Orthop. 2019, 6, 4. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Velier, M.; Magalon, J.; Daumas, A.; Cassar, M.; Francois, P.; Ghazouane, A.; Philandrianos, C.; Bertrand, B.; Frere, C.; Bernot, D.; et al. Production of platelet-rich plasma gel from elderly patients under antithrombotic drugs: Perspectives in chronic wounds care. Platelets 2018, 29, 496–503. [Google Scholar] [CrossRef] [PubMed]
- Niezgoda, J.A.; Van Gils, C.C.; Frykberg, R.G.; Hodde, J.P. Randomized clinical trial comparing OASIS Wound Matrix to Regranex Gel for diabetic ulcers. Adv. Skin Wound Care 2005, 18 Pt 1, 258–266. [Google Scholar] [CrossRef]
- Wieman, T.J.; Smiell, J.M.; Su, Y. Efficacy and safety of a topical gel formulation of recombinant human platelet-derived growth factor-BB (becaplermin) in patients with chronic neuropathic diabetic ulcers. A phase III randomized placebo-controlled double-blind study. Diabetes Care 1998, 21, 822–827. [Google Scholar] [CrossRef]
- Robson, M.C.; Phillips, L.G.; Thomason, A.; Robson, L.E.; Pierce, G.F. Platelet-derived growth factor BB for the treatment of chronic pressure ulcers. Lancet 1992, 339, 23–25. [Google Scholar] [CrossRef]
- Kirsner, R.S.; Warriner, R.; Michela, M.; Stasik, L.; Freeman, K. Advanced biological therapies for diabetic foot ulcers. Arch. Dermatol. 2010, 146, 857–862. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gilligan, A.M.; Waycaster, C.R.; Milne, C.T. Cost Effectiveness of Becaplermin Gel on Wound Closure for the Treatment of Pressure Injuries. Wounds 2018, 30, 197–204. [Google Scholar] [PubMed]
- Guebitz, G.M.; Nyanhongo, G.S. Enzymes as Green Catalysts and Interactive Biomolecules in Wound Dressing Hydrogels. Trends Biotechnol. 2018, 36, 1040–1053. [Google Scholar] [CrossRef] [PubMed]
- Vieira, L.F.A.; Lins, M.P.; Viana, I.M.M.N.; Dos Santos, J.E.; Smaniotto, S.; Reis, M.D.D.S. Metallic nanoparticles reduce the migration of human fibroblasts in vitro. Nanoscale Res. Lett. 2017, 12, 200. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Saco, M.; Howe, N.; Nathoo, R.; Cherpelis, B. Comparing the efficacies of alginate, foam, hydrocolloid, hydrofiber, and hydrogel dressings in the management of diabetic foot ulcers and venous leg ulcers: A systematic review and meta-analysis examining how to dress for success. Dermatol. Online J. 2016, 22, 8. [Google Scholar]
- Donaghue, V.M.; Chrzan, J.S.; Rosenblum, B.I.; Giurini, J.M.; Habershaw, G.M.; Veves, A. Evaluation of a collagen-alginate wound dressing in the management of diabetic foot ulcers. Adv. Wound Care 1998, 11, 114–119. [Google Scholar]
- Blackman, J.D.; Senseng, D.; Quinn, L.; Mazzone, T. Clinical evaluation of a semipermeable polymeric membrane dressing for the treatment of chronic diabetic foot ulcers. Diabetes Care 1994, 17, 322–325. [Google Scholar] [CrossRef]
- Zhang, Y.; Xing, S.Z. Treatment of diabetic foot ulcers using Mepillex Lite Dressing: A pilot study. Exp. Clin. Endocrinol. Diabetes 2014, 122, 227–230. [Google Scholar]
- Perez-Zabala, E.; Basterretxea, A.; Larrazabal, A.; Perez-Del-Pecho, K.; Rubio-Azpeitia, E.; Andia, I. Biological approach for the management of non-healing diabetic foot ulcers. J. Tissue Viability 2016, 25, 157–163. [Google Scholar] [CrossRef]
- De Angelis, B.; D’Autilio, M.F.L.M.; Orlandi, F.; Pepe, G.; Garcovich, S.; Scioli, M.G.; Orlandi, A.; Cervelli, V.; Gentile, P. Wound Healing: In Vitro and In Vivo Evaluation of a Bio-Functionalized Scaffold Based on Hyaluronic Acid and Platelet-Rich Plasma in Chronic Ulcers. J. Clin. Med. 2019, 8, 1486. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Faramarzi, N.; Yazdi, I.K.; Nabavinia, M.; Gemma, A.; Fanelli, A.; Caizzone, A.; Ptaszek, L.M.; Sinha, I.; Khademhosseini, A.; Ruskin, J.N.; et al. Patient-Specific Bioinks for 3D Bioprinting of Tissue Engineering Scaffolds. Adv. Healthc. Mater. 2018, 7, e1701347. [Google Scholar] [CrossRef] [PubMed]
- Milne, S.D.; Connolly, P. The influence of different dressings on the pH of the wound environment. J. Wound Care 2014, 23, 53–57. [Google Scholar] [CrossRef] [PubMed] [Green Version]





| Cell Count | Whole Blood | Platelet-Rich Plasma | |
|---|---|---|---|
| Leukocytes | (× 10−3/µL) | 5.2 ± 0.87 | 0.06 ± 0.07 (lymphocytes) |
| Erythrocytes | (× 10−6/µL) | 4.17 ± 0.48 | n.d. |
| Platelets | (× 10−3/µL) | 220 ± 0.42 | 460 ± 103 |
| Active Molecules | Concentration in PRF Releasate | Range |
|---|---|---|
| MCP-1 | 524 pg/mL | 100–1440 |
| VEGF | 166 pg/mL | 120–260 |
| HGF | 612 pg/mL | 430–870 |
| RANTES | 24 ng/mL | 22–27 |
| GRO-α | 900 pg/mL | 80–2370 |
| PDGF-BB | 12 ng/mL | 2–18 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Del Amo, C.; Perez-Valle, A.; Perez-Zabala, E.; Perez-del-Pecho, K.; Larrazabal, A.; Basterretxea, A.; Bully, P.; Andia, I. Wound Dressing Selection Is Critical to Enhance Platelet-Rich Fibrin Activities in Wound Care. Int. J. Mol. Sci. 2020, 21, 624. https://doi.org/10.3390/ijms21020624
Del Amo C, Perez-Valle A, Perez-Zabala E, Perez-del-Pecho K, Larrazabal A, Basterretxea A, Bully P, Andia I. Wound Dressing Selection Is Critical to Enhance Platelet-Rich Fibrin Activities in Wound Care. International Journal of Molecular Sciences. 2020; 21(2):624. https://doi.org/10.3390/ijms21020624
Chicago/Turabian StyleDel Amo, Cristina, Arantza Perez-Valle, Elena Perez-Zabala, Karmele Perez-del-Pecho, Ainara Larrazabal, Andima Basterretxea, Paola Bully, and Isabel Andia. 2020. "Wound Dressing Selection Is Critical to Enhance Platelet-Rich Fibrin Activities in Wound Care" International Journal of Molecular Sciences 21, no. 2: 624. https://doi.org/10.3390/ijms21020624
APA StyleDel Amo, C., Perez-Valle, A., Perez-Zabala, E., Perez-del-Pecho, K., Larrazabal, A., Basterretxea, A., Bully, P., & Andia, I. (2020). Wound Dressing Selection Is Critical to Enhance Platelet-Rich Fibrin Activities in Wound Care. International Journal of Molecular Sciences, 21(2), 624. https://doi.org/10.3390/ijms21020624