Overexpression of Platelet-Derived Growth Factor and Its Receptor Are Correlated with Oral Tumorigenesis and Poor Prognosis in Oral Squamous Cell Carcinoma
Abstract
:1. Introduction
2. Results
2.1. PDGF and PDGFR mRNA are Upregulated in OSCC Tissues
2.2. Immunohistochemical Expression of PDGF and PDGFR in OSCC Tissues
2.3. Serum PDGF-AA and PDGF-BB as Potential Diagnostic Markers
2.4. Thromobocytes Are Elevated in Cervical Lymph Node Metastasis
2.5. PDGF and PDGFR mRNA Levels Are Prognostic Values in OSCC Patients
2.6. PDGF Enhances the Tumorigenicity and Metastasis of OSCC Cells in a Dose Dependent Manner
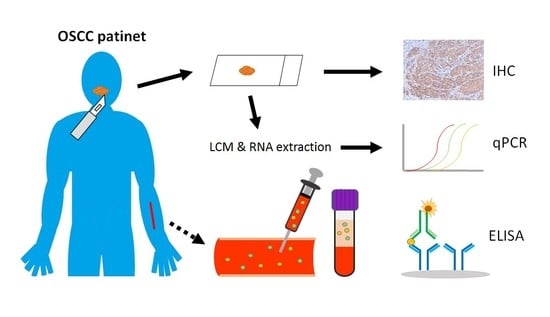
3. Material and Methods
3.1. Patients
3.2. Determination of PDGF in Serum
3.3. Quantitative Real-Time Polymerase Chain Reaction (qRT-PCR) of mRNA
3.4. Immunohistochemistry
3.5. Cell Culture, Reagents, and Phenotypic Assays
3.6. Cell Proliferation Assays
3.7. Anchorage-Independent Colony Formation
3.8. Transwell Migration and Invasion Assay
3.9. Statistics
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Health Promotion Administration, Ministry of Health and Welfare, Taiwan, Annual Report on the Causes of Death Statistics. 2018. Available online: https://www.mohw.gov.tw/dl-54578-bd0c9197-80ae-4cae-b015-0cb3a055a069.html (accessed on 21 June 2019).
- Gupta, S.; Kushwaha, V.S.; Verma, S.; Khan, H.; Bhatt, M.L.; Husain, N.; Negi, M.P.; Bhosale, V.V.; Ghatak, A. Understanding molecular markers in recurrent oral squamous cell carcinoma treated with chemoradiation. Heliyon 2016, 2, e00206. [Google Scholar] [CrossRef] [PubMed]
- Arantes, L.M.; de Carvalho, A.C.; Melendez, M.E.; Centrone, C.C.; Gois-Filho, J.F.; Toporcov, T.N.; Caly, D.N.; Tajara, E.H.; Goloni-Bertollo, E.M.; Carvalho, A.L. Validation of methylation markers for diagnosis of oral cavity cancer. Eur. J. Cancer 2015, 51, 632–641. [Google Scholar] [CrossRef] [PubMed]
- Dionne, K.R.; Warnakulasuriya, S.; Zain, R.B.; Cheong, S.C. Potentially malignant disorders of the oral cavity: Current practice and future directions in the clinic and laboratory. Int. J. Cancer 2015, 136, 503–515. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, T.; Ishigamori, R. Understanding carcinogenesis for fighting oral cancer. J. Oncol. 2011, 2011, 603740. [Google Scholar] [CrossRef] [PubMed]
- Eckert, A.W.; Wickenhauser, C.; Salins, P.C.; Kappler, M.; Bukur, J.; Seliger, B. Clinical relevance of the tumor microenvironment and immune escape of oral squamous cell carcinoma. J. Transl. Med. 2016, 14, 85. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shintani, S.; Li, C.; Ishikawa, T.; Mihara, M.; Nakashiro, K.; Hamakawa, H. Expression of vascular endothelial growth factor A, B, C, and D in oral squamous cell carcinoma. Oral Oncol. 2004, 40, 13–20. [Google Scholar] [CrossRef]
- Nakazato, T.; Shingaki, S.; Kitamura, N.; Saito, C.; Kuwano, R.; Tachibana, M. Expression level of vascular endothelial growth factor-C and -A in cultured human oral squamous cell carcinoma correlates respectively with lymphatic metastasis and angiogenesis when transplanted into nude mouse oral cavity. Oncol. Rep. 2006, 15, 825–830. [Google Scholar] [CrossRef]
- Margaritescu, C.; Pirici, D.; Simionescu, C.; Mogoanta, L.; Raica, M.; Stinga, A.; Ciurea, R.; Stepan, A.; Stinga, A.; Ribatti, D. VEGF and VEGFRs expression in oral squamous cell carcinoma. Rom. J. Morphol. Embryol. 2009, 50, 527–548. [Google Scholar]
- Raica, M.; Cimpean, A.M. Platelet-Derived Growth Factor (PDGF)/PDGF Receptors (PDGFR) Axis as Target for Antitumor and Antiangiogenic Therapy. Pharmaceuticals 2010, 3, 572–599. [Google Scholar] [CrossRef] [Green Version]
- Nie, D.; Yang, E.; Li, Z. Pretreatment thrombocytosis predict poor prognosis in patients with endometrial carcinoma: A systematic review and meta-analysis. BMC Cancer 2019, 19, 73. [Google Scholar] [CrossRef]
- Bailey, S.E.; Ukoumunne, O.C.; Shephard, E.; Hamilton, W. How useful is thrombocytosis in predicting an underlying cancer in primary care? a systematic review. Fam. Pract. 2017, 34, 4–10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shimada, H.; Oohira, G.; Okazumi, S.; Matsubara, H.; Nabeya, Y.; Hayashi, H.; Takeda, A.; Gunji, Y.; Ochiai, T. Thrombocytosis associated with poor prognosis in patients with esophageal carcinoma. J. Am. Coll. Surg. 2004, 198, 737–741. [Google Scholar] [CrossRef]
- Ikeda, M.; Furukawa, H.; Imamura, H.; Shimizu, J.; Ishida, H.; Masutani, S.; Tatsuta, M.; Satomi, T. Poor prognosis associated with thrombocytosis in patients with gastric cancer. Ann. Surg. Oncol. 2002, 9, 287–291. [Google Scholar] [CrossRef] [PubMed]
- Taucher, S.; Salat, A.; Gnant, M.; Kwasny, W.; Mlineritsch, B.; Menzel, R.C.; Schmid, M.; Smola, M.G.; Stierer, M.; Tausch, C.; et al. Impact of pretreatment thrombocytosis on survival in primary breast cancer. Thromb. Haemost. 2003, 89, 1098–1106. [Google Scholar] [PubMed]
- Lu, C.C.; Chang, K.W.; Chou, F.C.; Cheng, C.Y.; Liu, C.J. Association of pretreatment thrombocytosis with disease progression and survival in oral squamous cell carcinoma. Oral Oncol. 2007, 43, 283–288. [Google Scholar] [CrossRef] [PubMed]
- Arslan, C.; Coskun, H.S. Thrombocytosis in solid tumors: Review of the literature. Turk. J. Haematol. 2005, 22, 59–64. [Google Scholar] [PubMed]
- Rachidi, S.; Wallace, K.; Day, T.A.; Alberg, A.J.; Li, Z. Lower circulating platelet counts and antiplatelet therapy independently predict better outcomes in patients with head and neck squamous cell carcinoma. J. Hematol. Oncol. 2014, 7, 65. [Google Scholar] [CrossRef] [Green Version]
- Clara, C.A.; Marie, S.K.; de Almeida, J.R.; Wakamatsu, A.; Oba-Shinjo, S.M.; Uno, M.; Neville, M.; Rosemberg, S. Angiogenesis and expression of PDGF-C, VEGF, CD105 and HIF-1alpha in human glioblastoma. Neuropathology 2014, 34, 343–352. [Google Scholar]
- Nabors, L.B.; Suswam, E.; Huang, Y.; Yang, X.; Johnson, M.J.; King, P.H. Tumor necrosis factor alpha induces angiogenic factor up-regulation in malignant glioma cells: A role for RNA stabilization and HuR. Cancer Res. 2003, 63, 4181–4187. [Google Scholar]
- Li, H.; Fredriksson, L.; Li, X.; Eriksson, U. PDGF-D is a potent transforming and angiogenic growth factor. Oncogene 2003, 22, 1501–1510. [Google Scholar] [CrossRef] [Green Version]
- Demoulin, J.B.; Essaghir, A. PDGF receptor signaling networks in normal and cancer cells. Cytokine Growth Factor Rev. 2014, 25, 273–283. [Google Scholar] [CrossRef] [PubMed]
- Kohler, N.; Lipton, A. Platelets as a source of fibroblast growth-promoting activity. Exp. Cell Res. 1974, 87, 297–301. [Google Scholar] [CrossRef]
- Antoniades, H.N.; Galanopoulos, T.; Neville-Golden, J.; Kiritsy, C.P.; Lynch, S.E. Injury induces in vivo expression of platelet-derived growth factor (PDGF) and PDGF receptor mRNAs in skin epithelial cells and PDGF mRNA in connective tissue fibroblasts. Proc. Natl. Acad. Sci. USA 1991, 88, 565–569. [Google Scholar] [CrossRef] [Green Version]
- DiCorleto, P.E.; Bowen-Pope, D.F. Cultured endothelial cells produce a platelet-derived growth factor-like protein. Proc. Natl. Acad. Sci. USA 1983, 80, 1919–1923. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Evrova, O.; Buschmann, J. In vitro and in vivo effects of PDGF-BB delivery strategies on tendon healing: A review. Eur. Cells Mater. 2017, 34, 15–39. [Google Scholar] [CrossRef] [PubMed]
- Hoch, R.V.; Soriano, P. Roles of PDGF in animal development. Development 2003, 130, 4769–4784. [Google Scholar] [CrossRef] [Green Version]
- Gnessi, L.; Basciani, S.; Mariani, S.; Arizzi, M.; Spera, G.; Wang, C.; Bondjers, C.; Karlsson, L.; Betsholtz, C. Leydig cell loss and spermatogenic arrest in platelet-derived growth factor (PDGF)-A-deficient mice. J. Cell Biol. 2000, 149, 1019–1026. [Google Scholar] [CrossRef]
- Chen, J.; Yuan, W.; Wu, L.; Tang, Q.; Xia, Q.; Ji, J.; Liu, Z.; Ma, Z.; Zhou, Z.; Cheng, Y.; et al. PDGF-D promotes cell growth, aggressiveness, angiogenesis and EMT transformation of colorectal cancer by activation of Notch1/Twist1 pathway. Oncotarget 2017, 8, 9961–9973. [Google Scholar] [CrossRef] [Green Version]
- Farooqi, A.A.; Siddik, Z.H. Platelet-derived growth factor (PDGF) signalling in cancer: Rapidly emerging signalling landscape. Cell Biochem. Funct. 2015, 33, 257–265. [Google Scholar] [CrossRef] [Green Version]
- Hermanson, M.; Funa, K.; Hartman, M.; Claesson-Welsh, L.; Heldin, C.H.; Westermark, B.; Nister, M. Platelet-derived growth factor and its receptors in human glioma tissue: Expression of messenger RNA and protein suggests the presence of autocrine and paracrine loops. Cancer Res. 1992, 52, 3213–3219. [Google Scholar]
- Zhang, N.; Hu, H.; Fu, Y.; He, F.; Wang, L.; Zhuang, S.; Ding, M. The overexpression of PDGF-BB and its receptor is correlated with lymphatic metastasis in patients with non-small cell lung cancer. Int. J. Clin. Exp. Pathol. 2018, 11, 6010–6017. [Google Scholar] [PubMed]
- Zhang, M.; Liu, T.; Xia, B.; Yang, C.; Hou, S.; Xie, W.; Lou, G. Platelet-Derived Growth Factor D Is a Prognostic Biomarker and Is Associated With Platinum Resistance in Epithelial Ovarian Cancer. Int. J. Gynecol. Cancer 2018, 28, 323–331. [Google Scholar] [CrossRef] [PubMed]
- Heldin, C.H.; Lennartsson, J.; Westermark, B. Involvement of platelet-derived growth factor ligands and receptors in tumorigenesis. J. Intern. Med. 2018, 283, 16–44. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jain, R.K.; Lahdenranta, J.; Fukumura, D. Targeting PDGF signaling in carcinoma-associated fibroblasts controls cervical cancer in mouse model. PLoS Med. 2008, 5, e24. [Google Scholar] [CrossRef]
- Ozawa, T.; Brennan, C.W.; Wang, L.; Squatrito, M.; Sasayama, T.; Nakada, M.; Huse, J.T.; Pedraza, A.; Utsuki, S.; Yasui, Y.; et al. PDGFRA gene rearrangements are frequent genetic events in PDGFRA-amplified glioblastomas. Genes Dev. 2010, 24, 2205–2218. [Google Scholar] [CrossRef] [Green Version]
- Tu, H.F.; Chang, K.W.; Cheng, H.W.; Liu, C.J. Upregulation of miR-372 and -373 associates with lymph node metastasis and poor prognosis of oral carcinomas. Laryngoscope 2015, 125, E365–E370. [Google Scholar] [CrossRef]
- Lin, S.C.; Lin, L.H.; Yu, S.Y.; Kao, S.Y.; Chang, K.W.; Cheng, H.W.; Liu, C.J. FAT1 somatic mutations in head and neck carcinoma are associated with tumor progression and survival. Carcinogenesis 2018, 39, 1320–1330. [Google Scholar] [CrossRef]
- Liu, C.J.; Shen, W.G.; Peng, S.Y.; Cheng, H.W.; Kao, S.Y.; Lin, S.C.; Chang, K.W. miR-134 induces oncogenicity and metastasis in head and neck carcinoma through targeting WWOX gene. Int. J. Cancer 2014, 134, 811–821. [Google Scholar] [CrossRef]
- Hellstrom, M.; Kalen, M.; Lindahl, P.; Abramsson, A.; Betsholtz, C. Role of PDGF-B and PDGFR-beta in recruitment of vascular smooth muscle cells and pericytes during embryonic blood vessel formation in the mouse. Development 1999, 126, 3047–3055. [Google Scholar]
- Scher, C.D.; Stone, M.E.; Stiles, C.D. Platelet-derived growth factor prevents G0 growth arrest. Nature 1979, 281, 390–392. [Google Scholar] [CrossRef]
- Yu, J.; Liu, X.W.; Kim, H.R. Platelet-derived growth factor (PDGF) receptor-alpha-activated c-Jun NH2-terminal kinase-1 is critical for PDGF-induced p21WAF1/CIP1 promoter activity independent of p53. J. Biol. Chem. 2003, 278, 49582–49588. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vassbotn, F.S.; Havnen, O.K.; Heldin, C.H.; Holmsen, H. Negative feedback regulation of human platelets via autocrine activation of the platelet-derived growth factor alpha-receptor. J. Biol. Chem. 1994, 269, 13874–13879. [Google Scholar]
- Cao, R.; Brakenhielm, E.; Li, X.; Pietras, K.; Widenfalk, J.; Ostman, A.; Eriksson, U.; Cao, Y. Angiogenesis stimulated by PDGF-CC, a novel member in the PDGF family, involves activation of PDGFR-alphaalpha and -alphabeta receptors. FASEB J. 2002, 16, 1575–1583. [Google Scholar] [CrossRef] [PubMed]
- Watts, T.L.; Cui, R.; Szaniszlo, P.; Resto, V.A.; Powell, D.W.; Pinchuk, I.V. PDGF-AA mediates mesenchymal stromal cell chemotaxis to the head and neck squamous cell carcinoma tumor microenvironment. J. Transl. Med. 2016, 14, 337. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yao, R.; Cooper, G.M. Requirement for phosphatidylinositol-3 kinase in the prevention of apoptosis by nerve growth factor. Science 1995, 267, 2003–2006. [Google Scholar] [CrossRef] [PubMed]
- Ekman, S.; Thuresson, E.R.; Heldin, C.H.; Ronnstrand, L. Increased mitogenicity of an alphabeta heterodimeric PDGF receptor complex correlates with lack of RasGAP binding. Oncogene 1999, 18, 2481–2488. [Google Scholar] [CrossRef] [Green Version]
- Bran, B.; Bran, G.; Hormann, K.; Riedel, F. The platelet-derived growth factor receptor as a target for vascular endothelial growth factor-mediated anti-angiogenetic therapy in head and neck cancer. Int. J. Oncol. 2009, 34, 255–261. [Google Scholar] [CrossRef] [Green Version]
- Aebersold, D.M.; Froehlich, S.C.; Jonczy, M.; Beer, K.T.; Laissue, J.; Greiner, R.H.; Djonov, V. Expression of transforming growth factor-alpha, epidermal growth factor receptor and platelet-derived growth factors A and B in oropharyngeal cancers treated by curative radiation therapy. Radiother. Oncol. 2002, 63, 275–283. [Google Scholar] [CrossRef]
- Nissen, L.J.; Cao, R.; Hedlund, E.M.; Wang, Z.; Zhao, X.; Wetterskog, D.; Funa, K.; Brakenhielm, E.; Cao, Y. Angiogenic factors FGF2 and PDGF-BB synergistically promote murine tumor neovascularization and metastasis. J. Clin. Investig. 2007, 117, 2766–2777. [Google Scholar] [CrossRef] [Green Version]
- Petruzzelli, G.J.; Snyderman, C.H.; Johnson, J.T.; Myers, E.N. Angiogenesis induced by head and neck squamous cell carcinoma xenografts in the chick embryo chorioallantoic membrane model. Ann. Otol. Rhinol. Laryngol. 1993, 102, 215–221. [Google Scholar] [CrossRef]
- Rahbari, N.N.; Reissfelder, C.; Muhlbayer, M.; Weidmann, K.; Kahlert, C.; Buchler, M.W.; Weitz, J.; Koch, M. Correlation of circulating angiogenic factors with circulating tumor cells and disease recurrence in patients undergoing curative resection for colorectal liver metastases. Ann. Surg. Oncol. 2011, 18, 2182–2191. [Google Scholar] [CrossRef] [PubMed]
- Peterson, J.E.; Zurakowski, D.; Italiano, J.E., Jr.; Michel, L.V.; Connors, S.; Oenick, M.; D’Amato, R.J.; Klement, G.L.; Folkman, J. VEGF, PF4 and PDGF are elevated in platelets of colorectal cancer patients. Angiogenesis 2012, 15, 265–273. [Google Scholar] [CrossRef] [PubMed]
- Safi, A.; Sadmi, M.; Martinet, N.; Menard, O.; Vaillant, P.; Gallati, H.; Hosang, M.; Martinet, Y. Presence of elevated levels of platelet-derived growth factor (PDGF) in lung adenocarcinoma pleural effusions. Chest 1992, 102, 204–207. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gogus, C.; Baltaci, S.; Filiz, E.; Elhan, A.; Beduk, Y. Significance of thrombocytosis for determining prognosis in patients with localized renal cell carcinoma. Urology 2004, 63, 447–450. [Google Scholar] [CrossRef]
- Gu, D.; Szallasi, A. Thrombocytosis Portends Adverse Prognosis in Colorectal Cancer: A Meta-Analysis of 5,619 Patients in 16 Individual Studies. Anticancer Res. 2017, 37, 4717–4726. [Google Scholar]
- Mantur, M.; Snarska, J.; Sidorska, A.; Ostrowska, H.; Kruszewska-Wnorowska, K.; Wojszel, J. Changes in PDGF concentration in surgically treated colorectal carcinoma. Adv. Med. Sci. 2008, 53, 37–41. [Google Scholar] [CrossRef] [Green Version]
- Mantur, M.; Koper, O.; Snarska, J.; Sidorska, A.; Kruszewska-Wnorowska, K. Evaluation of PDGF-AB and sP-selectin concentrations in relation to platelet count in patients with colorectal cancer before and after surgical treatment. Pol. Arch. Med. Wewn. 2008, 118, 345–350. [Google Scholar] [CrossRef]
- Wang, Y.; Ji, M.; Wang, W.; Miao, Z.; Hou, P.; Chen, X.; Xu, F.; Zhu, G.; Sun, X.; Li, Y.; et al. Association of the T1799A BRAF mutation with tumor extrathyroidal invasion, higher peripheral platelet counts, and over-expression of platelet-derived growth factor-B in papillary thyroid cancer. Endocr. Relat. Cancer 2008, 15, 183–190. [Google Scholar] [CrossRef]
- Zhou, L.X.; Liang, E.Y.; Ye, J.Y.; Yang, M. Role of PDGF/PDGFR Pathway in Essential Thrombocythemia and Its Action Mechanism. Zhongguo Shi Yan Xue Ye Xue Za Zhi 2016, 24, 526–530. [Google Scholar]
- Väyrynen, J.P.; Väyrynen, S.A.; Sirniö, P.; Minkkinen, I.; Klintrup, K.; Karhu, T.; Mäkelä, J.; Herzig, K.-H.; Karttunen, T.J.; Tuomisto, A.; et al. Platelet count, aspirin use, and characteristics of host inflammatory responses in colorectal cancer. J. Transl. Med. 2019, 17, 199. [Google Scholar] [CrossRef]
- Papadopoulos, N.; Lennartsson, J. The PDGF/PDGFR pathway as a drug target. Mol. Asp. Med. 2018, 62, 75–88. [Google Scholar] [CrossRef] [PubMed]






| Variables | N | PDGFA | PDGFB | PDGFRA | PDGFRB | ||||
|---|---|---|---|---|---|---|---|---|---|
| Mean ± SEM | p-Value | Mean ± SEM | p-Value | Mean ± SE | p-Value | Mean ± SEM | p-Value | ||
| Gender | |||||||||
| Male | 117 | 9.63 ± 1.02 | 0.124 | 6.37 ± 0.77 | 0.502 | 3.25 ± 0.62 | 0.303 | 10.99 ± 1.29 | 0.615 |
| Female | 9 | 16.81 ± 10.59 | 8.29 ± 3.87 | 0.93 ± 0.34 | 13.47 ± 5.63 | ||||
| Age | |||||||||
| < 54 | 70 | 9.95 ± 1.30 | 0.858 | 7.46 ± 1.13 | 0.147 | 3.29 ± 0.91 | 0.696 | 11.55 ± 1.65 | 0.740 |
| ≥ 54 | 56 | 10.38 ± 2.17 | 5.32 ± 0.83 | 2.83 ± 0.64 | 10.70 ± 1.96 | ||||
| T stage | |||||||||
| T1-2 | 32 | 8.54 ± 2.12 | 0.440 | 5.70 ± 1.29 | 0.521 | 3.23 ± 1.06 | 0.884 | 9.93 ± 2.42 | 0.567 |
| T3-4 | 94 | 10.68 ± 1.44 | 6.78 ± 0.88 | 3.03 ± 0.69 | 11.59 ± 1.48 | ||||
| N status | |||||||||
| N0 | 80 | 7.34 ± 1.07 | 0.002 ** | 5.10 ± 0.90 | 0.011 * | 2.27 ± 0.42 | 0.064 | 9.05 ± 1.50 | 0.026 * |
| N+ | 46 | 15.00 ± 2.57 | 8.95 ± 1.17 | 4.49 ± 1.39 | 14.85 ± 2.17 | ||||
| Stage | |||||||||
| I-II | 21 | 6.41 ± 1.79 | 0.165 | 3.33 ± 0.81 | 0.051 | 1.39 ± 0.51 | 0.192 | 5.51 ± 2.45 | 0.045 * |
| III-IV | 105 | 10.89 ± 1.39 | 7.14 ± 0.85 | 3.42 ± 0.68 | 12.30 ± 1.41 | ||||
| Lymphovascular invasion | |||||||||
| No | 108 | 9.48 ± 1.28 | 0.185 | 6.33 ± 0.08 | 0.557 | 2.46 ± 0.43 | 0.445 | 10.31 ± 1.28 | 0.078 |
| Yes | 18 | 14.04 ± 3.37 | 7.57 ± 1.80 | 3.41 ± 1.62 | 16.32 ± 3.12 | ||||
| Perineural invasion | |||||||||
| No | 97 | 9.85 ± 1.46 | 0.664 | 6.01 ± 0.81 | 0.216 | 2.84 ± 0.48 | 0.438 | 10.22 ± 1.32 | 0.169 |
| Yes | 29 | 11.10 ± 1.85 | 8.16 ± 1.67 | 3.91 ± 1.95 | 14.35 ± 3.21 | ||||
| Variables | N | PDGF | PDGFRA | PDGFRB | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Low | High | p-Value | Low | High | p-Value | Low | High | p-Value | ||
| Gender | ||||||||||
| Male | 57 | 25 (43.9%) | 32 (56.1%) | 0.773 | 33 (57.9%) | 24 (42.1%) | 0.710 | 35 (61.4%) | 22 (38.6%) | 0.184 |
| Female | 6 | 3 (50.0%) | 3 (50.0%) | 3 (50.0%) | 3 (50.0%) | 2 (33.3%) | 4 (66.7%) | |||
| Age | ||||||||||
| <54 | 35 | 17 (48.6%) | 18 (51.4%) | 0.461 | 21 (60.0%) | 14 (40.0%) | 0.608 | 23 (65.7%) | 12 (34.3%) | 0.208 |
| ≥54 | 28 | 11 (39.9%) | 17 (60.7%) | 15 (53.6%) | 13 (46.4%) | 14 (50.0%) | 14 (50.0%) | |||
| T stage | ||||||||||
| T1-2 | 14 | 8 (57.1%) | 6 (42.9%) | 0.278 | 10 (71.4%) | 4 (28.6%) | 0.221 | 9 (64.3%) | 5 (35.7%) | 0.632 |
| T3-4 | 49 | 20 (40.8%) | 29 (59.2%) | 26 (53.1%) | 23 (46.9%) | 28 (57.1%) | 21 (42.9%) | |||
| N status | ||||||||||
| N0 | 36 | 21 (58.3%) | 15 (41.7%) | 0.010 * | 26 (72.2%) | 10 (27.8%) | 0.005 ** | 26 (72.2%) | 10 (27.8%) | 0.012 * |
| N+ | 27 | 7 (25.9%) | 20 (74.1%) | 10 (37.0%) | 17 (63.0%) | 11 (40.7%) | 16 (59.3%) | |||
| Stage | ||||||||||
| I-II | 7 | 4 (57.1%) | 3 (42.9%) | 0.473 | 5 (71.4%) | 2 (28.6%) | 0.418 | 5 (71.4%) | 2 (28.6%) | 0.469 |
| III-IV | 56 | 24 (42.9%) | 32 (57.1%) | 31 (55.4%) | 25 (44.6%) | 32 (57.1%) | 24 (42.9%) | |||
| Lymphovascular invasion | ||||||||||
| No | 51 | 24 (47.1%) | 27 (52.9%) | 0.389 | 31 (60.8%) | 20 (39.2%) | 0.229 | 33 (64.7%) | 18 (35.3%) | 0.047 * |
| Yes | 12 | 4 (33.3%) | 8 (66.7%) | 5 (41.7%) | 7 (58.3%) | 4 (33.3%) | 8 (66.7%) | |||
| Perineural invasion | ||||||||||
| No | 54 | 24 (44.4%) | 30 (55.6%) | 0.535 | 31 (60.8%) | 5 (39.2%) | 0.917 | 34 (63.0%) | 20 (37.0%) | 0.293 |
| Yes | 9 | 5 (55.6%) | 4 (44.4%) | 5 (55.6%) | 4 (44.4%) | 4 (44.4%) | 5 (55.6%) | |||
| Variables | N | PDGF-AA (pg/mL) | PDGF-BB (pg/mL) | Platelet Counts (Platelets/μL × 103) | |||
|---|---|---|---|---|---|---|---|
| Mean ± SEM | p-Value | Mean ± SEM | p-Value | Mean ± SEM | p-Value | ||
| Gender | |||||||
| Male | 129 | 4180.2 ± 107.2 | 0.247 | 2611.3 ± 148.5 | 0.789 | 267.9 ± 8.3 | 0.912 |
| Female | 20 | 3843.9 ± 244.6 | 2506.5 ± 257.2 | 265.5 ± 20.9 | |||
| Age | |||||||
| <54 | 73 | 4013.3 ± 143.3 | 0.228 | 2702.3 ± 191.8 | 0.440 | 270.8 ± 12.8 | 0.684 |
| ≥54 | 76 | 4252.0 ± 135.4 | 2496.3 ± 184.7 | 264.5 ± 8.8 | |||
| T stage | |||||||
| T1-2 | 67 | 3955.3 ± 136.6 | 0.100 | 2445.7 ± 192.9 | 0.304 | 259.0 ± 10.3 | 0.316 |
| T3-4 | 82 | 4281.9 ± 138.9 | 2721.0 ± 182.8 | 274.6 ± 11.2 | |||
| N status | |||||||
| N0 | 107 | 3971.0 ± 106.4 | 0.008 ** | 2323.5 ± 124.9 | 0.001 ** | 251.8 ± 89.9 | 0.001 ** |
| N+ | 42 | 4553.1 ± 210.1 | 3294.6 ± 326.6 | 307.8 ± 93.3 | |||
| Stage | |||||||
| I-II | 51 | 3816.0 ± 141.1 | 0.019* | 2346.0 ± 188.0 | 0.173 | 242.7 ± 10.6 | 0.019 * |
| III-IV | 98 | 4301.1 ± 128.1 | 2727.9 ± 175.9 | 280.6 ± 10.1 | |||
| Lymphovascular invasion | |||||||
| No | 130 | 4083.4 ± 101.6 | 0.172 | 2592.8 ± 145.5 | 0.932 | 264.1 ± 8.1 | 0.236 |
| Yes | 19 | 4488.4 ± 336.9 | 2627.2 ± 316.9 | 291.5 ± 23.7 | |||
| Perineural invasion | |||||||
| No | 130 | 4094.5 ± 100.9 | 0.284 | 2461.5 ± 135.7 | 0.007 ** | 267.7 ± 8.3 | 0.963 |
| Yes | 19 | 4412.5 ± 350.9 | 3525.7 ± 424.6 | 266.7 ± 20.9 | |||
| Univariate Analysis | Multivariate Analysis | ||||
|---|---|---|---|---|---|
| Variables | Subgroups | HR (95%CI) | p-Value | Adjusted HR (95%CI) | p-Value |
| PDGFA mRNA | High vs. Low | 2.943 (1.581−5.480) | 0.001 ** | 2.798 (1.501−5.216) | 0.003 * |
| PDGFB mRNA | High vs. Low | 3.661 (1.967−6.811) | <0.001 *** | 3.935 (2.080−7.444) | <0.001 *** |
| PDGFRA mRNA | High vs. Low | 1.711 (0.938−3.122) | 0.080 | 1.550 (0.846−2.838) | 0.156 |
| PDGFRB mRNA | High vs. Low | 3.775 (1.964−7.253) | 0.001 ** | 3.496 (1.801−6.786) | <0.001 *** |
| PDGF immunexpression | High vs. Low | 2.828 (1.194−6.699) | 0.018 * | 2.755 (1.161−6.541) | 0.022 * |
| PDGFRA immunexpression | High vs. Low | 2.108 (0.977−4.548) | 0.057 | 2.020 (0.931−4.383) | 0.075 |
| PDGFRB immunexpression | High vs. Low | 2.425 (1.130−5.204) | 0.023 * | 2.409 (1.100−5.275) | 0.028 * |
| Serum PDGF-AA | High vs. Low | 3.214 (1.508−6.851) | 0.002 ** | 2.394 (1.112−5.154) | 0.026 * |
| Serum PDGF-BB | High vs. Low | 2.311 (1.275−4.188) | 0.006 ** | 2.216 (1.218−4.033) | 0.009 ** |
| Platelet count | High vs. Low | 2.732 (1.533−4.870) | 0.001 ** | 2.207 (1.229−3.963) | 0.008 ** |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lin, L.-H.; Lin, J.-S.; Yang, C.-C.; Cheng, H.-W.; Chang, K.-W.; Liu, C.-J. Overexpression of Platelet-Derived Growth Factor and Its Receptor Are Correlated with Oral Tumorigenesis and Poor Prognosis in Oral Squamous Cell Carcinoma. Int. J. Mol. Sci. 2020, 21, 2360. https://doi.org/10.3390/ijms21072360
Lin L-H, Lin J-S, Yang C-C, Cheng H-W, Chang K-W, Liu C-J. Overexpression of Platelet-Derived Growth Factor and Its Receptor Are Correlated with Oral Tumorigenesis and Poor Prognosis in Oral Squamous Cell Carcinoma. International Journal of Molecular Sciences. 2020; 21(7):2360. https://doi.org/10.3390/ijms21072360
Chicago/Turabian StyleLin, Li-Han, Jiun-Sheng Lin, Cheng-Chieh Yang, Hui-Wen Cheng, Kuo-Wei Chang, and Chung-Ji Liu. 2020. "Overexpression of Platelet-Derived Growth Factor and Its Receptor Are Correlated with Oral Tumorigenesis and Poor Prognosis in Oral Squamous Cell Carcinoma" International Journal of Molecular Sciences 21, no. 7: 2360. https://doi.org/10.3390/ijms21072360
APA StyleLin, L. -H., Lin, J. -S., Yang, C. -C., Cheng, H. -W., Chang, K. -W., & Liu, C. -J. (2020). Overexpression of Platelet-Derived Growth Factor and Its Receptor Are Correlated with Oral Tumorigenesis and Poor Prognosis in Oral Squamous Cell Carcinoma. International Journal of Molecular Sciences, 21(7), 2360. https://doi.org/10.3390/ijms21072360