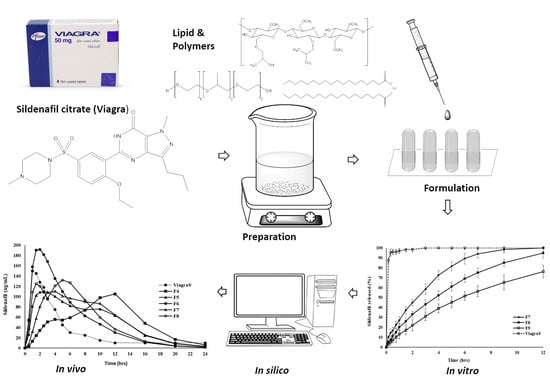
Development and In Vitro Evaluation of Controlled Release Viagra® Containing Poloxamer-188 Using Gastroplus™ PBPK Modeling Software for In Vivo Predictions and Pharmacokinetic Assessments
Abstract
:1. Introduction
2. Results
2.1. In Vitro Drug Release
2.2. Mechanism of Drug Release from Polymer Matrix
2.3. In Silico PK of SDF Using PBPK Model Simulations
3. Discussion
4. Material and Methods
4.1. Chemicals
4.2. Preparation of Poloxamer 188 Polymer Matrix Containing Sildenafil Citrate
4.3. Preparation of Controlled Release Polymer Matrices Containing Various Drug to Polymer Ratios
4.4. Dissolution Studies
4.5. Mechanism of Release
4.6. Simulation Studies
4.7. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Miranda, C.; Pérez-Rodríguez, Z.; Hernández-Armengol, R.; Quiñones-García, Y.; Betancourt-Purón, T.; Cabrera-Pérez, M.Á. Biowaiver or Bioequivalence: Ambiguity in Sildenafil Citrate BCS Classification. AAPS Pharm. Sci. Tech. 2018, 19, 1693–1698. [Google Scholar] [CrossRef]
- Kim, T.H.; Shin, S.; Jeong, S.W.; Lee, J.B.; Shin, B.S. Physiologically Relevant In Vitro-In Vivo Correlation (IVIVC) Approach for Sildenafil with Site-Dependent Dissolution. Pharmaceutics 2019, 11, 251. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hyland, R.; Roe, E.G.; Jones, B.C.; Smith, D.A. Identification of the cytochrome P450 enzymes involved in the N-demethylation of sildenafil. Br. J. Clin. Pharmacol. 2001, 51, 239–248. [Google Scholar] [CrossRef] [Green Version]
- Zayed, R.; Kamel, A.O.; Shukr, M.; Shamy, A. An in vitro and in vivo comparative study of directly compressed solid dispersions and freeze dried sildenafil citrate sublingual tablets for management of pulmonary arterial hypertension. Acta Pharm. 2012, 62, 411–432. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nichols, D.J.; Muirhead, G.J.; Harness, J.A. Pharmacokinetics of sildenafil after single oral doses in healthy male subjects: Absolute bioavailability, food effects and dose proportionality. Br. J. Clin. Pharmacol. 2002, 53 (Suppl. 1), 5S–12S. [Google Scholar] [CrossRef] [Green Version]
- Radicioni, M.; Castiglioni, C.; Giori, A.; Cupone, I.; Frangione, V.; Rovati, S. Bioequivalence study of a new sildenafil 100 mg orodispersible film compared to the conventional film-coated 100 mg tablet administered to healthy male volunteers. Drug Des. Devel. Ther. 2017, 11, 1183–1192. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McCullough, A.R. Four-year review of sildenafil citrate. Rev. Urol. 2002, 4 (Suppl. 3), S26–S38. [Google Scholar] [PubMed]
- Dalla-Bona, A.C.; Stoisiek, K.; Oesterheld, N.; Schmehl, T.; Gessler, T.; Seeger, W.; Beck-Broichsitter, M. Characterization of lung-delivered in-situ forming controlled release formulations. J. Pharm. Pharmacol. 2015, 67, 1349–1354. [Google Scholar] [CrossRef] [PubMed]
- Değim, I.T.; Tuğcu-Demiröz, F.; Tamer-Ilbasmis, S.; Acartürk, F. Development of controlled release sildenafil formulations for vaginal administration. Drug Deliv. 2008, 15, 259–265. [Google Scholar] [CrossRef] [PubMed]
- Chunhachaichana, C.; Sritharadol, R.; Sawatdee, S.; Heng, P.W.S.; Srichana, T. Development of nanodispersion-based sildenafil metered-dose inhalers stabilized by poloxamer 188: A potential candidate for the treatment of pulmonary arterial hypertension. Pharm. Dev. Technol. 2019, 24, 1218–1228. [Google Scholar] [CrossRef]
- Hosny, K.M.; Aljaeid, B.M. Sildenafil citrate as oral solid lipid nanoparticles: A novel formula with higher bioavailability and sustained action for treatment of erectile dysfunction. Expert Opin. Drug Deliv. 2014, 11, 1015–1022. [Google Scholar] [CrossRef] [PubMed]
- Shahin, H.I.; Vinjamuri, B.P.; Mahmoud, A.A.; Shamma, R.N.; Mansour, S.M.; Ammar, H.O.; Ghorab, M.M.; Chougule, M.B.; Chablani, L. Design and evaluation of novel inhalable sildenafil citrate spray-dried microparticles for pulmonary arterial hypertension. J. Control Release 2019, 302, 126–139. [Google Scholar] [CrossRef] [PubMed]
- Beck-Broichsitter, M.; Bohr, A.; Aragão-Santiago, L.; Klingl, A.; Kissel, T. Formulation and process considerations for the design of sildenafil-loaded polymeric microparticles by vibrational spray-drying. Pharm. Dev. Technol. 2017, 22, 691–698. [Google Scholar] [CrossRef] [PubMed]
- Atipairin, A.; Chunhachaichana, C.; Nakpheng, T.; Changsan, N.; Srichana, T.; Sawatdee, S. Development of a Sildenafil Citrate Microemulsion-Loaded Hydrogel as a Potential System for Drug Delivery to the Penis and Its Cellular Metabolic Mechanism. Pharmaceutics 2020, 12, 1055. [Google Scholar] [CrossRef] [PubMed]
- Bodratti, A.M.; Sarkar, B.; Alexandridis, P. Adsorption of poly(ethylene oxide)-containing amphiphilic polymers on solid-liquid interfaces: Fundamentals and applications. Adv. Colloid Interface Sci. 2017, 244, 132–163. [Google Scholar] [CrossRef] [PubMed]
- Sarkar, B.; Venugopal, V.; Bodratti, A.M.; Tsianou, M.; Alexandridis, P. Nanoparticle surface modification by amphiphilic polymers in aqueous media: Role of polar organic solvents. J. Colloid Interface Sci. 2013, 397, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Bostanudin, M.F.; Arafat, M.; Sarfraz, M.; Górecki, D.C.; Barbu, E. Butylglyceryl Pectin Nanoparticles: Synthesis, Formulation and Characterization. Polymers 2019, 11, 789. [Google Scholar] [CrossRef] [Green Version]
- Kamal, T.; Sarfraz, M.; Arafat, M.; Mikov, M.; Rahman, N. Cross-linked guar gum and sodium borate based microspheres as colon-targeted anticancer drug delivery systems for 5-fluorouracil. Pak. J. Pharm. Sci. 2017, 30, 2329–2336. [Google Scholar] [PubMed]
- Khalid, N.; Sarfraz, M.; Arafat, M.; Akhtar, M.; Löbenberg, R.; Rehman, N. Nano-sized Droplets of Self-Emulsifying System for Enhancing Oral Bioavailability of Chemotherapeutic Agent VP-16 in Rats: A Nano Lipid Carrier for BCS Class IV Drugs. J. Pharm. Pharm. Sci. 2018, 21, 398–408. [Google Scholar] [CrossRef]
- Tanbour, R.; Martins, A.M.; Pitt, W.G.; Husseini, G.A. Drug Delivery Systems Based on Polymeric Micelles and Ultrasound: A Review. Curr. Pharm. Des. 2016, 21, 398–408. [Google Scholar] [CrossRef] [PubMed]
- Arafat, M.; Kirchhoefer, C.; Mikov, M. Mixed Micelles Loaded with Bile Salt: An Approach to Enhance Intestinal Transport of the BCS Class III Drug Cefotaxime in Rats. Eur. J. Drug Metab. Pharm. 2017, 42, 635–645. [Google Scholar] [CrossRef] [PubMed]
- Duttagupta, A.S.; Chaudhary, H.M.; Jadhav, K.R.; Kadam, V.J. Cubosomes: Innovative Nanostructures for Drug Delivery. Curr. Drug Deliv. 2016, 13, 482–493. [Google Scholar] [CrossRef] [PubMed]
- Almeida, H.; Amaral, M.H.; Lobão, P.; Lobo, J.M.S. Applications of poloxamers in ophthalmic pharmaceutical formulations: An overview. Expert Opin. Drug Deliv. 2013, 10, 1223–1237. [Google Scholar] [CrossRef]
- Al Hanbali, O.A.; Khan, H.M.S.; Sarfraz, M.; Arafat, M.; Ijaz, S.; Hameed, A. Transdermal patches: Design and current approaches to painless drug delivery. Acta Pharm. 2019, 69, 197–215. [Google Scholar] [CrossRef] [Green Version]
- Kunjachan, S.; Rychlik, B.; Storm, G.; Kiessling, F.; Lammers, T. Multidrug resistance: Physiological principles and nanomedical solutions. Adv. Drug Deliv. Rev. 2013, 65, 1852–1865. [Google Scholar] [CrossRef] [Green Version]
- Al Hanbali, O.A.; Hamed, R.; Arafat, M.; Bakkour, Y.; Al-Matubsi, H.; Mansour, R.; Al-Bataineh, Y.; Aldhoun, M.; Sarfraz, M.; Dardas, A.K. Formulation and evaluation of diclofenac controlled release matrix tablets made of HPMC and Poloxamer 188 polymer: An assessment on mechanism of drug release. Pak. J. Pharm. Sci. 2018, 31, 345–351. [Google Scholar]
- Jannin, V.; Pochard, E.; Chambin, O. Influence of poloxamers on the dissolution performance and stability of controlled-release formulations containing Precirol ATO 5. Int. J. Pharm. 2006, 309, 6–15. [Google Scholar] [CrossRef] [PubMed]
- Moura, S.; Noro, J.; Cerqueira, P.; Silva, C.; Cavaco-Paulo, A.; Loureiro, A. Poloxamer 407 based-nanoparticles for controlled release of methotrexate. Int. J. Pharm. 2020, 575, 118924. [Google Scholar] [CrossRef] [Green Version]
- Jansen, M.M.P.M.; Verzijl, J.M.; Burger, D.M.; Hekster, Y.A. Controlled release of morphine from a poloxamer 407 gel. Int. J. Pharm. 2013, 452, 266–269. [Google Scholar] [CrossRef] [PubMed]
- Veyriesa, M.L.; Couarrazeb, G.; Geigerb, S.; Gnelyb, F.A.; Massiasc, L.; Kunzlic, B.; Faurissona, F.; Rouveixd, B. Controlled release of vancomycin from Poloxamer 407 gels. Int. J. Pharm. 2000, 192, 183–193. [Google Scholar] [CrossRef]
- Xia, H.; Jin, H.; Cheng, Y.; Cheng, Z.; Xu, Y. The Controlled Release and Anti-Inflammatory Activity of a Tetramethylpyrazine-Loaded Thermosensitive Poloxamer Hydrogel. Pharm. Res. 2019, 36, 52. [Google Scholar] [CrossRef]
- Kuroiwa, Y.; Higashi, K.; Ueda, K.; Yamamoto, K.; Moribe, K. Nano-scale and molecular-level understanding of wet-milled indomethacin/poloxamer 407 nanosuspension with TEM, suspended-state NMR, and Raman measurements. Int. J. Pharm. 2018, 537, 30–39. [Google Scholar] [CrossRef] [PubMed]
- Paavola, A.; Bernards, C.M.; Rosenberg, P.H. Controlled release ibuprofen-poloxamer gel for epidural use-A pharmacokinetic study using microdialysis in pigs. Eur. J. Pharm. Biopharm. 2016, 108, 180–186. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Orasugh, J.T.; Dutta, S.; Das, D.; Pal, C.; Zaman, A.; Das, S. Sustained release of ketorolac tromethamine from poloxamer 407/cellulose nanofibrils graft nanocollagen based ophthalmic formulations. Int. J. Biol. Macromol. 2019, 140, 441–453. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.H.; Choi, G.; Oh, Y.J.; Park, J.W.; Choy, Y.B.; Park, M.C.; Yoon, Y.J.; Lee, H.J.; Chang, H.C.; Choy, J.H. A nanohybrid system for taste masking of sildenafil. Int. J. Nanomed. 2012, 7, 1635–1649. [Google Scholar] [CrossRef] [Green Version]
- Golocorbin-Kon, S.; Mikov, M.; Arafat, M.; Lepojevic, Z.; Mikov, I.; Sahman-Zaimovic, M.; Tomic, Z. Cefotaxime pharmacokinetics after oral application in the form of 3alpha,7alpha-dihydroxy-12-keto-5beta-cholanate microvesicles in rat. Eur. J. Drug Metab. Pharmacokinet. 2009, 34, 31–36. [Google Scholar] [CrossRef] [PubMed]
- Sarfraz, M.K.; Rehman, N.U.; Mohsin, S. Naproxen release from sustained release matrix system and effect of cellulose derivatives. Pak. J. Pharm. Sci. 2006, 19, 251–255. [Google Scholar]
- Uzunović, A.; Vranić, E. Effect of magnesium stearate concentration on dissolution properties of ranitidine hydrochloride coated tablets. Bosn. J. Basic Med. Sci. 2007, 7, 279–283. [Google Scholar] [CrossRef] [PubMed]
- Ariyasu, A.; Hattori, Y.; Otsuka, M. Delay effect of magnesium stearate on tablet dissolution in acidic medium. Int. J. Pharm. 2016, 511, 757–764. [Google Scholar] [CrossRef]
- Arafat, M.; Fahelelbom, K.M.; Sarfraz, M.K.; Bostanudin, M.F.; Sharif, Q.U.; Esmaeil, A.; Al Hanbali, O.A.; Aburuz, S. Comparison between Branded and Generic Furosemide 40 mg Tablets Using Thermal Gravimetric Analysis and Fourier Transform Infrared Spectroscopy. J. Pharm. Bioallied. Sci. 2020, 12, 489–498. [Google Scholar] [CrossRef]
- Arafat, M.; Kirchhoefer, C.; Mikov, M.; Sarfraz, M.; Löbenberg, R. Nanosized Liposomes Containing Bile Salt: A Vesicular Nanocarrier for Enhancing Oral Bioavailability of BCS Class III Drug. J. Pharm. Pharm. Sci. 2017, 20, 305–318. [Google Scholar] [CrossRef] [PubMed]
- Rashid, M.; Sarfraz, M.; Arafat, M.; Hussain, A.; Abbas, N.; Sadiq, M.W.; Rasool, M.F.; Bukhari, N.I. Prediction of lisinopril pediatric dose from the reference adult dose by employing a physiologically based pharmacokinetic model. BMC Pharmacol. Toxicol. 2020, 21, 56. [Google Scholar] [CrossRef] [PubMed]
- Bolger, M.B.; Macwan, J.S.; Sarfraz, M.; Almukainzi, M.; Löbenberg, R. The Irrelevance of In Vitro Dissolution in Setting Product Specifications for Drugs Like Dextromethorphan That are Subject to Lysosomal Trapping. J. Pharm. Sci. 2019, 108, 268–278. [Google Scholar] [CrossRef] [PubMed] [Green Version]





| Model Name | r2 of F7 | r2 of F8 | r2 of F9 |
|---|---|---|---|
| Zero Order Model | 0.9883 | 0.9825 | 0.9754 |
| First Order Model | 0.6394 | 0.5738 | 0.5769 |
| Hixson–Crowell Model | 0.9850 | 0.9907 | 0.9875 |
| Higuchi Model | 0.9601 | 0.9685 | 0.9696 |
| Korsmeyer–Peppas Model | 0.4203 | 0.3309 | 0.3290 |
| Parameter | Values |
|---|---|
| Log P | a 2.27 |
| Molecular Weight (g/mol) | a 474.59 |
| Ionization Constant | (pKa) 6.5 |
| Solubility (mg/mL) | a 6.965 (pH = 3) |
| Diffusion Coefficient (cm2 /sec × 10−5) | a 0.58 × 10−5 |
| Papp (Caco-2) | a 7.077 (pH = 4) |
| Jejunal Effective Permeability (Peff) (×10−4 cm/s) | a 3.48 × 10−4 |
| Unbound Percent in Human Plasma (Fup %) | a 28.10 |
| Human Blood-to-Plasma Concentration Ratio (Rbp) | 1.65 |
| PK | Viagra® | F1 | F2 | F3 | F4 | F5 | F6 | F7 | F8 |
|---|---|---|---|---|---|---|---|---|---|
| Cmax (ng mL−1) | 159 | 120.9 * | 96.2 * | 93.9 * | 105.1 * | 109.3 * | 193.2 * | 113.7 * | 132.4 * |
| tmax (h) | 1.46 | 3.68 * | 9.44 * | 11.2 * | 12.08 * | 2.48 * | 1.76 | 3.61 * | 5.28 * |
| t1/2 (h) | 4.07 | 5.65 * | 8.12 * | 9.85 * | 11.8 * | 7.75 * | 6.10 * | 8.12 * | 6.51 * |
| AUC0-∞(ng mL−1h) | 530 | 128 * | 1267 * | 1258 * | 1252.2 * | 1272.2 * | 1288.7 * | 1237.7 * | 1289.9 * |
| AUC0-t (ng mL−1h) | 528 | 1271 * | 1252 * | 1238 * | 1224.6 * | 1259.5 * | 1283.2 * | 1262.1 * | 1276.5 * |
| Formulations | SDF (mg) | P-188 (mg) | HPMC (mg) | Total Weight (mg) | Ratio 1:5 |
|---|---|---|---|---|---|
| F1 | 50 | 250 | 0 | 275 | 1:5:0 |
| F2 | 50 | 225 | 25 | 275 | 1:4.5:0.5 |
| F3 | 50 | 200 | 50 | 275 | 1:4:1 |
| F4 | 50 | 175 | 75 | 275 | 1:3.5:1.5 |
| F5 | 50 | 150 | 100 | 275 | 1:3:2 |
| F6 | 50 | 125 | 125 | 275 | 1:2.5:2.5 |
| Formulations | SDF (mg) | P-188 (mg) | HPMC (mg) | STA (mg) | MGS (mg) |
|---|---|---|---|---|---|
| F7 | 50 | 300 | 200 | 50 | 0 |
| F8 | 50 | 300 | 200 | 50 | 37.5 |
| F9 | 50 | 300 | 200 | 50 | 75 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Arafat, M.; Sarfraz, M.; AbuRuz, S. Development and In Vitro Evaluation of Controlled Release Viagra® Containing Poloxamer-188 Using Gastroplus™ PBPK Modeling Software for In Vivo Predictions and Pharmacokinetic Assessments. Pharmaceuticals 2021, 14, 479. https://doi.org/10.3390/ph14050479
Arafat M, Sarfraz M, AbuRuz S. Development and In Vitro Evaluation of Controlled Release Viagra® Containing Poloxamer-188 Using Gastroplus™ PBPK Modeling Software for In Vivo Predictions and Pharmacokinetic Assessments. Pharmaceuticals. 2021; 14(5):479. https://doi.org/10.3390/ph14050479
Chicago/Turabian StyleArafat, Mosab, Muhammad Sarfraz, and Salahdein AbuRuz. 2021. "Development and In Vitro Evaluation of Controlled Release Viagra® Containing Poloxamer-188 Using Gastroplus™ PBPK Modeling Software for In Vivo Predictions and Pharmacokinetic Assessments" Pharmaceuticals 14, no. 5: 479. https://doi.org/10.3390/ph14050479
APA StyleArafat, M., Sarfraz, M., & AbuRuz, S. (2021). Development and In Vitro Evaluation of Controlled Release Viagra® Containing Poloxamer-188 Using Gastroplus™ PBPK Modeling Software for In Vivo Predictions and Pharmacokinetic Assessments. Pharmaceuticals, 14(5), 479. https://doi.org/10.3390/ph14050479