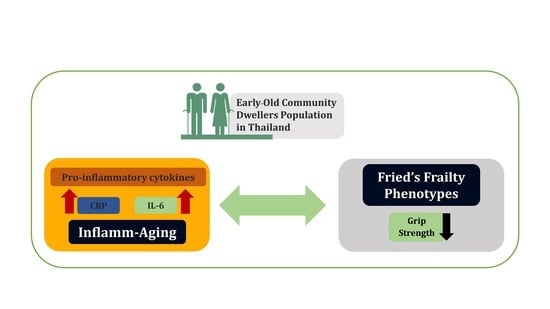
The Association between Frailty Indicators and Blood-Based Biomarkers in Early-Old Community Dwellers of Thailand
Abstract
:1. Introduction
2. Methods
2.1. Study Design and Participants
2.2. Frailty Measurement
2.3. Blood-Based Frailty Biomarker Measurement
2.4. Statistical Analysis
2.5. Ethical Consideration
3. Results
3.1. Assessment of Frailty Among a Population of Early-Old Community Dwellers
3.2. Assessment of Blood-Based Frailty Biomarkers
3.3. Frailty Phenotypes and Frailty Biomarkers within the Context of Gender Differences
3.4. Association between Frailty Phenotypes and Inflammatory Biomarkers
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- National Statistical Office. Report on the 2017 Survey of the Older Persons in Thailand; Statistical Forecasting Division, National Statistical Office: Bangkok, Thailand, 2018; p. 266.
- Gavrilov, L.A.; Heuveline, P. Aging of population. Encycl. Popul. 2003, 1, 32–37. [Google Scholar]
- Institute for Population and Social Research M.U. Situation of Thai Elderly 2015; Foundation of Thai Gerontology Research and Development Institute: Bangkok, Thailand, 2015; p. 132. [Google Scholar]
- Siriwardhana, D.D.; Weerasinghe, M.C.; Rait, G.; Falcaro, M.; Scholes, S.; Walters, K.R. Prevalence of frailty in rural community-dwelling older adults in Kegalle district of Sri Lanka: A population-based cross-sectional study. BMJ Open 2019, 9, bmjopen-2018. [Google Scholar] [CrossRef]
- Chen, X.; Mao, G.; Leng, S.X. Frailty syndrome: An overview. Clin. Interv. Aging 2014, 9, 433–441. [Google Scholar]
- Hubbard, R.E.; Woodhouse, K.W. Frailty, inflammation and the elderly. Biogerontology 2010, 11, 635–641. [Google Scholar] [CrossRef]
- Fried, L.P.; Ferrucci, L.; Darer, J.; Williamson, J.D.; Anderson, G. Untangling the concepts of disability, frailty, and comorbidity: Implications for improved targeting and care. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2004, 59, M255–M263. [Google Scholar] [CrossRef]
- Bektas, A.; Schurman, S.H.; Sen, R.; Ferrucci, L. Human T cell immunosenescence and inflammation in aging. J. Leukoc. Biol. 2017, 102, 977–988. [Google Scholar] [CrossRef] [Green Version]
- Wou, F.; Conroy, S. The frailty syndrome. Medicine 2013, 41, 13–15. [Google Scholar] [CrossRef]
- Fried, L.P.; Tangen, C.M.; Walston, J.; Newman, A.B.; Hirsch, C.; Gottdiener, J.; Seeman, T.; Tracy, R.; Kop, W.J.; Burke, G.; et al. Frailty in older adults: Evidence for a phenotype. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2001, 56, M146–M157. [Google Scholar] [CrossRef]
- Rockwood, K.; Song, X.; MacKnight, C.; Bergman, H.; Hogan, D.B.; McDowell, I.; Mitnitski, A. A global clinical measure of fitness and frailty in elderly people. CMAJ 2005, 173, 489–495. [Google Scholar] [CrossRef] [Green Version]
- Martin-Ruiz, C.; Jagger, C.; Kingston, A.; Collerton, J.; Catt, M.; Davies, K.; Dunn, M.; Hilkens, C.; Keavney, B.; Pearce, S.H.; et al. Assessment of a large panel of candidate biomarkers of ageing in the Newcastle 85+ study. Mech. Ageing Dev. 2011, 132, 496–502. [Google Scholar] [CrossRef]
- Wagner, K.H.; Cameron-Smith, D.; Wessner, B.; Franzke, B. Biomarkers of aging: From function to molecular biology. Nutrients 2016, 8, 338. [Google Scholar] [CrossRef]
- Xia, X.; Chen, W.; McDermott, J.; Han, J.D.J. Molecular and phenotypic biomarkers of aging. F1000Research 2017, 6, 860–869. [Google Scholar] [CrossRef]
- Siriwardhana, D.D.; Hardoon, S.; Rait, G.; Weerasinghe, M.C.; Walters, K.R. Prevalence of frailty and prefrailty among community-dwelling older adults in low-income and middle-income countries: A systematic review and meta-analysis. BMJ Open 2018, 8, e018195. [Google Scholar] [CrossRef]
- Doba, N.; Tokuda, Y.; Goldstein, N.E.; Kushiro, T.; Hinohara, S. A pilot trial to predict frailty syndrome: The Japanese Health Research Volunteer Study. Exp. Gerontol. 2012, 47, 638–643. [Google Scholar] [CrossRef] [Green Version]
- Mohd Hamidin, F.A.; Adznam, S.N.A.; Ibrahim, Z.; Chan, Y.M.; Abdul Aziz, N.H. Prevalence of frailty syndrome and its associated factors among community-dwelling elderly in East Coast of Peninsular Malaysia. Sage Open Med. 2018, 6, 2050312118775581. [Google Scholar] [CrossRef]
- Buckinx, F.; Rolland, Y.; Reginster, J.Y.; Ricour, C.; Petermans, J.; Bruyère, O. Burden of frailty in the elderly population: Perspectives for a public health challenge. Arch. Public Health 2015, 73, 19–25. [Google Scholar] [CrossRef]
- Xue, Q.L. The frailty syndrome: Definition and natural history. Clin. Geriatr. Med. 2011, 27, 1–15. [Google Scholar] [CrossRef]
- Srinonprasert, V.; Chalermsri, C.; Aekplakorn, W. Frailty index to predict all-cause mortality in Thai community-dwelling older population: A result from a National Health Examination Survey cohort. Arch. Gerontol. Geriatr. 2018, 77, 124–128. [Google Scholar] [CrossRef]
- Kingston, A.; Comas-Herrera, A.; Jagger, C. Forecasting the care needs of the older population in England over the next 20 years: Estimates from the Population Ageing and Care Simulation (PACSim) modelling study. Lancet Public Health 2018, 3, e447–e455. [Google Scholar] [CrossRef]
- House, J.S.; Kessler, R.C.; Herzog, A.R.; Mero, R.P.; Kinney, A.M.; Breslow, M.J. Age, socioeconomic status, and health. Milbank Q. 1990, 68, 383–411. [Google Scholar] [CrossRef]
- Silpakit, O.; Silpakit, C.; Pukdeenaul, P. A comparison study of cognitive impairment screening tools: CDT, IQCODE VS MMSE. Siriraj. Med. J. 2007, 59, 361–363. [Google Scholar]
- Lemieux, I.; Lamarche, B.; Couillard, C.; Pascot, A.; Cantin, B.; Bergeron, J.; Dagenais, G.R.; Després, J.P. Total cholesterol/HDL cholesterol ratio vs LDL cholesterol/HDL cholesterol ratio as indices of ischemic heart disease risk in men: The Quebec Cardiovascular Study. Arch. Intern. Med. 2001, 161, 2685–2692. [Google Scholar] [CrossRef]
- United Nation The Department of Economic and Social Affairs. Population Division. In World Population Ageing 2017; The United Nations: New York, NY, USA, 2017; p. 46. [Google Scholar]
- Hongthong, D.; Somrongthong, R. Factors influencing the Quality of Life (Qol) among Thai older people in a rural area of Thailand. Iran. J. Public Health 2015, 44, 479–485. [Google Scholar]
- Manasatchakun, P.; Roxberg, Å.; Asp, M. Conceptions of healthy aging held by relatives of older persons in Isan-Thai culture: A phenomenographic study. J. Aging Res. 2018, 2018, 3734645. [Google Scholar] [CrossRef]
- Knodel, J.; Chayovan, N. Family support and living arrangements of Thai elderly. Asia Pac. Popul. J. 1997, 12, 51–68. [Google Scholar] [CrossRef]
- Rockwood, K.; Fox, R.A.; Stolee, P.; Robertson, D.; Beattie, B.L. Frailty in elderly people: An evolving concept. CMAJ Can. Med. Assoc. J. 1994, 150, 489–495. [Google Scholar]
- Fulop, T.; Larbi, A.; Witkowski, J.M.; McElhaney, J.; Loeb, M.; Mitnitski, A.; Pawelec, G. Aging, frailty and age-related diseases. Biogerontology 2010, 11, 547–563. [Google Scholar] [CrossRef]
- Lang, P.O.; Michel, J.P.; Zekry, D. Frailty syndrome: A transitional state in a dynamic process. Gerontology 2009, 55, 539–549. [Google Scholar] [CrossRef]
- Salvioli, S.; Capri, M.; Valensin, S.; Tieri, P.; Monti, D.; Ottaviani, E.; Franceschi, C. Inflamm-aging, cytokines and aging: State of the art, new hypotheses on the role of mitochondria and new perspectives from systems biology. Curr. Pharm. Des. 2006, 12, 3161–3171. [Google Scholar] [CrossRef]
- Franceschi, C.; Capri, M.; Garagnani, P.; Ostan, R.; Santoro, A.; Monti, D.; Salvioli, S. Inflammaging. In Handbook of Immunosenescence: Basic Understanding and Clinical Implications; Springer: Basel, Switzerland, 2018; pp. 1–31. [Google Scholar]
- Limtrakul, P.; Yodkeeree, S.; Pitchakarn, P.; Punfa, W. Suppression of inflammatory responses by black rice extract in RAW 264.7 macrophage cells via downregulation of NF-kB and AP-1 signaling pathways. Asian Pac. J. Cancer Prev. 2015, 16, 4277–4283. [Google Scholar] [CrossRef]
- Franceschi, C.; Bonafè, M.; Valensin, S.; Olivieri, F.; De Luca, M.; Ottaviani, E.; De Benedictis, G. Inflamm-aging: An evolutionary perspective on immunosenescence. Ann. N. Y. Acad. Sci. 2000, 908, 244–254. [Google Scholar] [CrossRef]
- Miquel, J. An update of the oxidation-inflammation theory of aging: The involvement of the immune system in oxi-inflamm-aging. Curr. Pharm. Des. 2009, 15, 3003–3026. [Google Scholar]
- Fulop, T.; Larbi, A.; Dupuis, G.; Le Page, A.; Frost, E.H.; Cohen, A.A.; Witkowski, J.M.; Franceschi, C. Immunosenescence and inflamm-aging as two sides of the same coin: Friends or foes? Front. Immunol. 2018, 8, 1960. [Google Scholar] [CrossRef]
- Ferrucci, L.; Fabbri, E. Inflammageing: Chronic inflammation in ageing, cardiovascular disease, and frailty. Nat. Rev. Cardiol. 2018, 15, 505–522. [Google Scholar] [CrossRef]
- Röhrig, G. Anemia in the frail, elderly patient. Clin. Interv. Aging 2016, 11, 319. [Google Scholar] [CrossRef]
- Morley, J.E.; Malmstrom, T.K. Frailty, sarcopenia, and hormones. Endocrinol. Metab. Clin. 2013, 42, 391–405. [Google Scholar] [CrossRef]
- Leng, S.X.; Xue, Q.L.; Tian, J.; Walston, J.D.; Fried, L.P. Inflammation and frailty in older women. J. Am. Geriatr. Soc. 2007, 55, 864–871. [Google Scholar] [CrossRef]
- Collerton, J.; Martin-Ruiz, C.; Davies, K.; Hilkens, C.M.; Isaacs, J.; Kolenda, C.; Parker, C.; Dunn, M.; Catt, M.; Jagger, C.; et al. Frailty and the role of inflammation, immunosenescence and cellular ageing in the very old: Cross-sectional findings from the Newcastle 85+ Study. Mech. Ageing Dev. 2012, 133, 456–466. [Google Scholar] [CrossRef]
- Yang, Y.; Hao, Q.; Flaherty, J.H.; Cao, L.; Zhou, J.; Su, L.; Shen, Y.; Dong, B. Comparison of procalcitonin, a potentially new inflammatory biomarker of frailty, to interleukin-6 and C-reactive protein among older Chinese hospitalized patients. Aging Clin. Exp. Res. 2018, 30, 1459–1464. [Google Scholar] [CrossRef]
- De Martinis, M.; Franceschi, C.; Monti, D.; Ginaldi, L. Inflammation markers predicting frailty and mortality in the elderly. Exp. Mol. Pathol. 2006, 80, 219–227. [Google Scholar] [CrossRef]
- Hubbard, R.E.; O’Mahony, M.S.; Savva, G.M.; Calver, B.L.; Woodhouse, K.W. Inflammation and frailty measures in older people. J. Cell. Mol. Med. 2009, 13, 3103–3109. [Google Scholar] [CrossRef] [Green Version]
- Darvin, K.; Randolph, A.; Ovalles, S.; Halade, D.; Breeding, L.; Richardson, A.; Espinoza, S.E. Plasma protein biomarkers of the geriatric syndrome of frailty. J. Gerontol. Ser. A Biomed. Sci. Med. Sci. 2013, 69, 182–186. [Google Scholar] [CrossRef]
- Pereira, L.S.M.; Narciso, F.M.S.; Oliveira, D.M.G.; Coelho, F.M.; de Souza, D.D.G.; Dias, R.C. Correlation between manual muscle strength and interleukin-6 (IL-6) plasma levels in elderly community-dwelling women. Arch. Gerontol. Geriatr. 2009, 48, 313–316. [Google Scholar] [CrossRef]
- Legrand, D.; Adriaensen, W.; Vaes, B.; Matheï, C.; Wallemacq, P.; Degryse, J. The relationship between grip strength and muscle mass (MM), inflammatory biomarkers and physical performance in community-dwelling very old persons. Arch. Gerontol. Geriatr. 2013, 57, 345–351. [Google Scholar] [CrossRef]
- Leng, S.; Chaves, P.; Koenig, K.; Walston, J. Serum interleukin-6 and hemoglobin as physiological correlates in the geriatric syndrome of frailty: A pilot study. J. Am. Geriatr. Soc. 2002, 50, 1268–1271. [Google Scholar] [CrossRef]
- Ershler, W.B. Biological interactions of aging and anemia: A focus on cytokines. J. Am. Geriatr. Soc. 2003, 51, 18–21. [Google Scholar] [CrossRef]
- Gale, C.R.; Baylis, D.; Cooper, C.; Sayer, A.A. Inflammatory markers and incident frailty in men and women: The English Longitudinal Study of Ageing. Age 2013, 35, 2493–2501. [Google Scholar] [CrossRef]
- Puts, M.T.; Visser, M.; Twisk, J.W.; Deeg, D.J.; Lips, P. Endocrine and inflammatory markers as predictors of frailty. Clin. Endocrinol. 2005, 63, 403–411. [Google Scholar] [CrossRef] [Green Version]
- Baylis, D.; Bartlett, D.B.; Syddall, H.E.; Ntani, G.; Gale, C.R.; Cooper, C.; Lord, J.M.; Sayer, A.A. Immune-endocrine biomarkers as predictors of frailty and mortality: A 10-year longitudinal study in community-dwelling older people. Age 2013, 35, 963–971. [Google Scholar] [CrossRef]
- Barzilay, J.I.; Blaum, C.; Moore, T.; Xue, Q.L.; Hirsch, C.H.; Walston, J.D.; Fried, L.P. Insulin resistance and inflammation as precursors of frailty: The Cardiovascular Health Study. Arch. Intern. Med. 2007, 167, 635–641. [Google Scholar] [CrossRef]
- Gruver, A.; Hudson, L.; Sempowski, G. Immunosenescence of ageing. J. Pathol. A J. Pathol. Soc. Great Br. Irel. 2007, 211, 144–156. [Google Scholar] [CrossRef]
- Pawelec, G.; Adibzadeh, M.; Pohla, H.; Schaudt, K. Immunosenescence: Ageing of the immune system. Immunol. Today 1995, 16, 420–422. [Google Scholar] [CrossRef]
- Correa, B.L.; Ornaghi, A.P.; Muller, G.C.; Engroff, P.; Lopes, R.P.; da Silva Filho, I.G.; Bosch, J.A.; Bonorino, C.; Bauer, M.E. The inverted CD4: CD8 ratio is associated with cytomegalovirus, poor cognitive and functional states in older adults. Neuroimmunomodulation 2014, 21, 206–212. [Google Scholar] [CrossRef]
- Leng, S.X.; Cappola, A.R.; Andersen, R.E.; Blackman, M.R.; Koenig, K.; Blair, M.; Walston, J.D. Serum levels of insulin-like growth factor-I (IGF-I) and dehydroepiandrosterone sulfate (DHEA-S), and their relationships with serum interleukin-6, in the geriatric syndrome of frailty. Aging Clin. Exp. Res. 2004, 16, 153–157. [Google Scholar] [CrossRef]

| Gender | Prevalence %, (95% CI) | ||
|---|---|---|---|
| Frail a | Pre-Frail b | Non-Frail c | |
| Overall (n = 526) | 15.0 (12.1, 18.4) | 69.6 (65.5, 73.5) | 15.4 (12.4, 18.8) |
| Men (n = 193) | 11.4 (7.3, 16.7) | 68.9 (61.9, 75.4) | 19.7 (14.3, 26.0) |
| Women (n = 333) | 17.1 (13.2, 21.6) | 70.0 (64.7, 74.8) | 12.9 (9.5, 17.0) |
| Data | Frail (n = 58) | Non-Frail (n = 60) | p-Value |
|---|---|---|---|
| Sociodemographic factors Age, mean ± SD | 68.9 ± 2.7 | 68.1 ± 2.5 | 0.06 |
| Female, n (%) | 41 (70.7) | 35 (58.3) | 0.23 |
| Married/living with partner, n (%) | 33 (56.9) | 41 (68.3) | 0.27 |
| Lifestyle characteristics | |||
| Smoking at present, n (%) | 4 (6.9) | 7 (11.7) | 0.57 |
| Alcohol at present, n (%) | 3 (5.2) | 11 (18.3) | 0.05 |
| Clinical health data | |||
| Body mass index (BMI), mean ± SD | 22.1 ± 4.1 | 22.2 ± 2.8 | 0.83 |
| History of illness, n (%) | |||
| Cardiovascular diseases | 4 (6.9) | 0 (0) | 0.12 |
| Diabetes | 10 (17.2) | 9 (15.0) | 0.94 |
| ** Osteoarthritis | 16 (27.6) | 4 (6.7) | <0.01 |
| Asthma or Chronic lung diseases | 1 (1.7) | 1 (1.7) | 1.00 |
| Hypercholesterolemia | 12 (20.7) | 10 (16.7) | 0.75 |
| Osteoporosis | 0 (0) | 2 (3.3) | 0.49 |
| Depression score ≥7, n (%) | 8 (13.8) | 3 (5.0) | 0.19 |
| * Cognitive function, mean ± SD | 23.1 ± 3.9 | 24.9 ± 3.7 | 0.02 |
| Hematological data, mean ± SD | |||
| * Hemoglobin (g/dL) | 12.5 ± 1.6 | 13.3 ± 1.6 | 0.01 |
| * Red blood cell count (106/µL) | 4.8 ± 0.8 | 5.1 ± 0.5 | <0.01 |
| * Hematocrit (%) | 39.2 ± 4.5 | 41.4 ± 4.0 | <0.01 |
| White blood cell count (103/µL) | 7.2 ± 1.8 | 6.9 ± 1.7 | 0.41 |
| Neutrophil (%) | 55.2 ± 8.8 | 52.9 ± 10.3 | 0.17 |
| Lymphocyte (%) | 31.5 ± 8.2 | 33.3 ± 8.5 | 0.21 |
| Monocyte (%) | 7.7 ± 2.0 | 7.7 ± 1.9 | 0.97 |
| Blood urea nitrogrn (mg/dL) | 14.5 ± 4.6 | 13.9 ± 4.6 | 0.44 |
| Creatinine (mg/dL) | 0.9 ± 0.3 | 0.9 ± 0.2 | 0.68 |
| ** AST (U/L) | 20.4 ± 6.0 | 24.7 ± 10.8 | <0.01 |
| ** ALT (U/L) | 15.8 ± 7.0 | 20.9 ± 12.7 | <0.01 |
| Fasting blood glucose (mg/dL) | 101.0 ± 26.5 | 105.5 ± 27.7 | 0.35 |
| Lipid profile, mean ± SD | |||
| Total cholesterol | 200.8 ± 50.9 | 203.6 ± 38.1 | 0.73 |
| Triglycerides (mg/dL) | 142.2 ± 79.0 | 125.0 ± 57.7 | 0.08 |
| ** HDL-C (mg/dL) | 49.4 ± 10.4 | 54.1 ± 11.4 | <0.01 |
| LDL-C (mg/dL) | 123.0 ± 42.7 | 124.5 ± 32.4 | 0.83 |
| LDL-c/ HDL-c Ratio | 2.56 ± 0.9 | 2.37 ± 0.7 | 0.09 |
| TC/ HDL-c Ratio | 4.19 ± 1.2 | 3.88 ± 0.9 | 0.05 |
| Parameters | Frail (n = 58) | Non-Frail (n = 60) | p-Value |
|---|---|---|---|
| Frailty indicators | |||
| Self-reported weight loss, n (%) | 18 (31.0) | 0 (0) | - |
| ** Weight difference (∆w, kg) | −2.23 ± 4.3 | 0.55 ± 1.7 | <0.01 |
| Self-reported exhaustion, n (%) | 40 (69.0) | 0 (0) | - |
| ** Exhaustion sum score | 2.14 ± 1.6 | 0.18 ± 0.4 | <0.01 |
| Weakness, n (%) | 50 (86.2) | 0 (0) | - |
| ** Grip strength, kg | 15.89 ± 5.69 | 25.76 ± 7.09 | <0.01 |
| Slow walking speed, n (%) | 37 (63.8) | 0 (0) | - |
| ** Walking speed, s | 7.28 ± 1.98 | 4.30 ± 0.80 | <0.01 |
| Decreased activity, n (%) | 50 (86.2) | 0 (0) | - |
| ** Physical activity, Kcal | 215.3 ± 470.1 | 1192.1 ± 1397.7 | < 0.01 |
| ** Frailty score | 3.36 ± 0.52 | 0 | < 0.01 |
| Biomarkers | Frail (n = 58) | Non-Frail (n = 60) | p-Value |
|---|---|---|---|
| Inflammatory Biomarkers | |||
| * C-reactive protein, mg/L | 0.67 ± 0.13 | 0.40 ± 0.05 | 0.033 |
| * Interleukin-6, pg/mL | 20.01 ± 8.14 | 5.80 ± 0.55 | 0.044 |
| Endocrine biomarkers | |||
| Insulin-like growth factor-1, ng/mL | 29.96 ± 0.85 | 28.47 ± 0.80 | 0.103 |
| Immunosenescence biomarkers | |||
| % CD4+ T cell | 36.62 ± 1.07 | 33.88 ± 1.07 | 0.073 |
| % CD8+ T cell | 20.02 ± 0.96 | 19.67 ± 0.92 | 0.794 |
| CD4:CD8 Ratio | 2.13 ± 0.13 | 2.06 ± 1.19 | 0.735 |
| Parameters | Men | Women | ||||
|---|---|---|---|---|---|---|
| Frail (n = 17) | Non-Frail (n = 25) | p-Value | Frail (n = 41) | Non-Frail (n = 35) | p-Value | |
| Frailty indicators, n (%) Self-reported weight loss | 6 (35.3) | 0 | - | 12 (29.3) | 0 | - |
| ** Weight difference (∆w, kg) | −3.09 ± 4.0 | 0.59 ± 1.7 | <0.01 | −1.88 ± 4.4 | 0.53 ± 1.7 | <0.01 |
| Self-reported exhaustion | 13 (76.5) | 0 | - | 27 (65.9) | 0 | - |
| ** Exhaustion sum score | 2.65 ± 1.8 | 0.12 ± 0.3 | <0.01 | 1.93 ± 1.4 | 0.23 ± 0.4 | <0.01 |
| Weakness | 14 (82.4) | 0 | - | 36 (87.8) | 0 | - |
| ** Grip strength, kg | 20.6 ± 5.6 | 32.6 ± 5.7 | <0.01 | 13.9 ± 4.5 | 20.9 ± 2.3 | <0.01 |
| Slow walking speed | 6 (35.3) | 0 | - | 31 (75.6) | 0 | - |
| ** Walking speed, s | 6.2 ± 1.4 | 4.0 ± 0.7 | <0.01 | 7.7 ± 2.0 | 4.5 ± 0.8 | <0.01 |
| Decreased activity, kcal | 14 (82.4) | 0 | - | 36 (87.8) | 0 | - |
| ** Physical activity, Kcal | 363.8 ± 755.4 | 1481.2 ± 1382.9 | <0.01 | 153.7 ± 273.0 | 985.5 ± 1391.0 | <0.01 |
| ** Frailty score, mean ± SD | 3.1 ± 0.3 | 0 | <0.01 | 3.5 ± 0.6 | 0 | <0.01 |
| Frailty biomarkers, mean ± SE | ||||||
| ** C-reactive protein, mg/L | 0.47 ± 0.1 | 0.24 ± 0.04 | 0.005 | 0.75 ± 0.19 | 0.51 ± 0.07 | 0.001 |
| * Interleukin-6, pg/mL | 10.44 ± 3.7 | 5.69 ± 0.8 | 0.033 | 23.98 ± 11.4 | 5.88 ± 0.8 | 0.034 |
| IGF-1, ng/mL | 32.57 ± 1.0 | 29.57 ± 1.2 | 0.072 | 28.88 ± 1.1 | 27.69 ± 1.0 | 0.432 |
| % CD4 + T cell | 31.64 ± 8.1 | 36.86 ± 7.2 | 0.023* | 34.66 ± 8.6 | 36.74 ± 9.6 | 0.309 |
| % CD8 + T cell | 18.63 ± 10.4 | 19.20 ± 7.1 | 0.822 | 21.11 ± 7.3 | 19.47 ± 6.1 | 0.286 |
| CD4:CD8 Ratio | 2.19 ± 1.2 | 2.27 ± 1.2 | 0.834 | 1.90 ± 1.0 | 2.14 ± 1.1 | 0.315 |
| Frailty category (non-frail, frail) | Interleukin-6 | C-reactive Protein | ||
|---|---|---|---|---|
| OR (95% CI) | p-Value | OR (95% CI) | p-Value | |
| ** Overall | 1.554 (1.229, 1.966) | <0.001 | 1.011 (1.006, 1.016) | <0.001 |
| * Men | 1.927 (1.138, 3.262) | 0.015 | 1.004 (1.001, 1.007) | 0.020 |
| ** Women | 1.806 (1.215, 2.683) | 0.003 | 1.011 (1.003, 1.018) | 0.005 |
| Frailty indicators | Interleukin-6 | C-reactive Protein | ||
|---|---|---|---|---|
| OR (95% CI) | p-Value | OR (95% CI) | p-Value | |
| Overall | ||||
| Weight difference (∆w, kg) | 0.996 (0.976, 1.016) | 0.683 | 1.000 (0.999, 1.001) | 0.530 |
| Exhaustion sum score | 1.006 (0.995, 1.016) | 0.278 | 1.000 (0.999, 1.000) | 0.512 |
| ** Grip strength (kg) | 1.470 (1.200, 1.801) | <0.01 ** | 1.008 (1.004, 1.011) | <0.01 ** |
| Walking speed (s) | 1.017 (0.993, 1.042) | 0.165 | 1.001 (1.000, 1.001) | 0.074 |
| Physical activity (Kcal) | 1.001 (0.993, 1.009) | 0.797 | 1.001 (1.000, 1.002) | 0.054 |
| Men | ||||
| Weight difference (∆w, kg) | 1.038 (0.973, 1.107) | 0.256 | 1.000 (0.997, 1.002) | 0.850 |
| Exhaustion sum score | 1.061 (0.979, 1.151) | 0.149 | 1.002 (1.000, 1.005) | 0.037 * |
| Grip strength (kg) | 1.075 (0.974, 1.186) | 0.150 | 1.014 (1.003, 1.026) | 0.012 * |
| Walking speed (s) | 0.859 (0.624, 1.183) | 0.352 | 1.001 (0.999, 1.003) | 0.417 |
| Physical activity (Kcal) | 1.089 (0.969, 1.225) | 0.153 | 1.002 (1.000, 1.005) | 0.044 * |
| Women | ||||
| Weight difference (∆w, kg) | 0.989 (0.948, 1.032) | 0.616 | 1.000 (0.999, 1.001) | 0.523 |
| Exhaustion sum score | 1.004 (0.995, 1.014) | 0.368 | 0.999 (0.998, 1.000) | 0.195 |
| ** Grip strength (kg) | 1.393 (1.088, 1.782) | <0.01 ** | 1.009 (1.002, 1.015) | <0.01 ** |
| Walking speed (s) | 1.028 (0.983, 1.075) | 0.225 | 1.000 (1.000, 1.001) | 0.197 |
| Physical activity (Kcal) | 0.999 (0.991, 1.008) | 0.888 | 1.000 (1.000, 1.001) | 0.182 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Semmarath, W.; Seesen, M.; Yodkeeree, S.; Sapbamrer, R.; Ayood, P.; Malasao, R.; Siviroj, P.; Limtrakul, P. The Association between Frailty Indicators and Blood-Based Biomarkers in Early-Old Community Dwellers of Thailand. Int. J. Environ. Res. Public Health 2019, 16, 3457. https://doi.org/10.3390/ijerph16183457
Semmarath W, Seesen M, Yodkeeree S, Sapbamrer R, Ayood P, Malasao R, Siviroj P, Limtrakul P. The Association between Frailty Indicators and Blood-Based Biomarkers in Early-Old Community Dwellers of Thailand. International Journal of Environmental Research and Public Health. 2019; 16(18):3457. https://doi.org/10.3390/ijerph16183457
Chicago/Turabian StyleSemmarath, Warathit, Mathuramat Seesen, Supachai Yodkeeree, Ratana Sapbamrer, Pisittawoot Ayood, Rungnapa Malasao, Penprapa Siviroj, and Pornngarm Limtrakul (Dejkriengkraikul). 2019. "The Association between Frailty Indicators and Blood-Based Biomarkers in Early-Old Community Dwellers of Thailand" International Journal of Environmental Research and Public Health 16, no. 18: 3457. https://doi.org/10.3390/ijerph16183457
APA StyleSemmarath, W., Seesen, M., Yodkeeree, S., Sapbamrer, R., Ayood, P., Malasao, R., Siviroj, P., & Limtrakul, P. (2019). The Association between Frailty Indicators and Blood-Based Biomarkers in Early-Old Community Dwellers of Thailand. International Journal of Environmental Research and Public Health, 16(18), 3457. https://doi.org/10.3390/ijerph16183457