Face Masks and Respirators in the Fight Against the COVID-19 Pandemic: A Review of Current Materials, Advances and Future Perspectives
Abstract
:1. Introduction
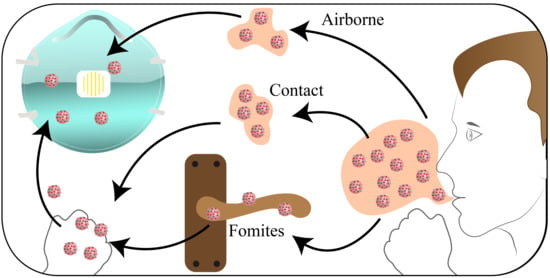
1.1. COVID-19 Pandemic
1.2. Face Masks
1.3. Respirators
2. Standards and Legislation
- Adequate control of inhalation exposure and to provide effective protection.
- Be suitable for the intended use.
- Must be ‘CE’ marked (RPE used must be manufactured according to the PPE Regulations 2002 (PE Directive 89/686/EEC) and the CE marks tell us that the equipment has met the legal requirements for the design [42]).
- Selected, used and checked regularly by trained people with proper records.
- Stored and appropriately cleaned.
3. Materials
4. Mathematical Modelling
5. Recent Advances
6. Reuse
7. Effectiveness and Fitting
8. Future Perspective and Conclusions
Funding
Conflicts of Interest
References
- Zheng, Y.-Y.; Ma, Y.-T.; Zhang, J.-Y.; Xie, X. COVID-19 and the cardiovascular system. Nat. Rev. Cardiol. 2020, 17, 259–260. [Google Scholar] [CrossRef] [Green Version]
- Sohrabi, C.; Alsafi, Z.; O’Neill, N.; Khan, M.; Kerwan, A.; Al-Jabir, A.; Iosifidis, C.; Agha, R. World Health Organization declares global emergency: A review of the 2019 novel coronavirus (COVID-19). Int. J. Surg. 2020, 76, 71–76. [Google Scholar] [CrossRef]
- Guo, Y.-R.; Cao, Q.-D.; Hong, Z.; Tan, Y.-Y.; Chen, S.; Jin, H.; Tan, K.S.; Wang, D.Y.; Yan, Y. The origin, transmission and clinical therapies on coronavirus disease 2019 (COVID-19) outbreak - an update on the status. Mil. Med. Res. 2020, 7, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Velavan, T.P.; Meyer, C.G. The COVID-19 epidemic. Trop. Med. Int. Health 2020, 25, 278–280. [Google Scholar] [CrossRef] [Green Version]
- WHO Director-General’s Remarks at the Media Briefing on 2019-nCoV on 11 February 2020. Available online: https://www.who.int/dg/speeches/detail/who-director-general-s-remarks-at-the-media-briefing-on-2019-ncov-on-11-february-2020 (accessed on 20 May 2020).
- COVID-19 Situation Update Worldwide, as of 17 July 2020. 2020. Available online: https://www.ecdc.europa.eu/en/geographical-distribution-2019-ncov-cases (accessed on 17 July 2020).
- Infection Prevention and Control during Health Care When Novel Coronavirus (nCoV) Infection Is Suspected. 2020. Available online: https://www.who.int/publications-detail/infection-prevention-and-control-during-health-care-when-novel-coronavirus-(ncov)-infection-is-suspected-20200125 (accessed on 20 May 2020).
- Huang, H.; Fan, C.; Li, M.; Nie, H.-L.; Wang, F.-B.; Wang, H.; Wang, R.; Xia, J.; Zheng, X.; Zuo, X.; et al. COVID-19: A Call for Physical Scientists and Engineers. ACS Nano 2020, 14, 3747–3754. [Google Scholar] [CrossRef] [Green Version]
- Prather, K.A.; Wang, C.C.; Schooley, R.T. Reducing transmission of SARS-CoV-2. Science 2020, 368, 1422–1424. [Google Scholar] [CrossRef]
- Advice on the Use of Masks in the Community, during Home Care and in Healthcare Settings in the Context of the Novel Coronavirus (COVID-19) Outbreak. 2020. Available online: https://www.who.int/publications/i/item/advice-on-the-use-of-masks-in-the-community-during-home-care-and-in-healthcare-settings-in-the-context-of-the-novel-coronavirus-(2019-ncov)-outbreak (accessed on 20 May 2020).
- Milton, D.K.; Fabian, M.P.; Cowling, B.J.; Grantham, M.L.; McDevitt, J.J. Influenza Virus Aerosols in Human Exhaled Breath: Particle Size, Culturability, and Effect of Surgical Masks. PLoS Pathog. 2013, 9, e1003205. [Google Scholar] [CrossRef] [Green Version]
- Anderson, E.L.; Turnham, P.; Griffin, J.R.; Clarke, C.C. Consideration of the Aerosol Transmission for COVID-19 and Public Health. Risk Anal. 2020, 40, 902–907. [Google Scholar] [CrossRef]
- Leung, N.H.L.; Chu, D.K.W.; Shiu, E.Y.C.; Chan, K.-H.; McDevitt, J.J.; Hau, B.J.P.; Yen, H.-L.; Li, Y.; Ip, D.K.M.; Peiris, J.S.M.; et al. Respiratory virus shedding in exhaled breath and efficacy of face masks. Nat. Med. 2020, 26, 676–680. [Google Scholar] [CrossRef] [Green Version]
- Gov.ie - Guidance on Safe Use of Face Coverings. 2020. Available online: https://www.gov.ie/en/publication/aac74c-guidance-on-safe-use-of-face-coverings/ (accessed on 22 May 2020).
- Use of Face Masks by the General Public - Health Protection Surveillance Centre. 2020. Available online: https://www.hpsc.ie/a-z/respiratory/coronavirus/novelcoronavirus/guidance/infectionpreventionandcontrolguidance/ppe/useoffacemasksbythegeneralpublic/ (accessed on 22 May 2020).
- PPE - Health Protection Surveillance Centre. 2020. Available online: https://www.hpsc.ie/a-z/respiratory/coronavirus/novelcoronavirus/guidance/infectionpreventionandcontrolguidance/ppe/ (accessed on 22 May 2020).
- @usatoday. Czech Government Implemented a Face Mask Requirement to Help Combat Covid-19. 2020. Available online: https://www.usatoday.com/story/opinion/2020/04/04/czech-government-implemented-face-mask-requirement-help-combat-coronavirus-column/2940393001/ (accessed on 22 May 2020).
- @BBCWorld, Germans don Compulsory Masks as Lockdown Eases. 2020. Available online: https://www.bbc.com/news/world-europe-52439926 (accessed on 22 May 2020).
- @BBCWorld, Spain Tightens Mask Rules for All Older Than Five. 2020. Available online: https://www.bbc.com/news/world-europe-52735166 (accessed on 22 May 2020).
- @CDCgov, Recommendation Regarding the Use of Cloth Face Coverings | CDC. 2020. Available online: https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/cloth-face-cover-guidance.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fcoronavirus%2F2019-ncov%2Fprevent-getting-sick%2Fcloth-face-cover.html (accessed on 22 May 2020).
- Tunevall, T.G. Postoperative wound infections and surgical face masks: A controlled study. World J. Surg. 1991, 15, 383–387. [Google Scholar] [CrossRef]
- Spooner, J.L. History of Surgical Face Masks. AORN J. 1967, 5, 76–80. [Google Scholar] [CrossRef]
- Rockwood, C.A.; O’Donoghue, D.H. The Surgical Mask: Its Development, Usage, and Efficiency. AMA Arch. Surg. 1960, 80, 963–971. [Google Scholar] [CrossRef] [PubMed]
- Belkin, N.L. The Evolution of the Surgical Mask: Filtering Efficiency Versus Effectiveness. Infect. Control Hosp. Epidemiol. 1997, 18, 49–57. [Google Scholar] [CrossRef] [PubMed]
- Schrader, E.S. From apron to gown: A history of OR attire. AORN J. 1976, 24, 52–67. [Google Scholar] [CrossRef]
- Cohen, H.J.; Birkner, J.S. Respiratory Protection. Clin. Chest Med. 2012, 33, 783–793. [Google Scholar] [CrossRef]
- Gosch, M.E.; Shaffer, R.E.; Eagan, A.E.; Roberge, R.J.; Davey, V.J.; Radonovich, L.J. B95: A new respirator for health care personnel. Am. J. Infect. Control 2013, 41, 1224–1230. [Google Scholar] [CrossRef]
- Oberg, T.; Brosseau, L.M. Surgical mask filter and fit performance. Am. J. Infect. Control 2008, 36, 276–282. [Google Scholar] [CrossRef]
- Lin, C.S. Surgical Masks - Premarket Notification [510(k)] Submissions. 2004; Center for Devices and Radiological Health. Available online: https://www.fda.gov/regulatory-information/search-fda-guidance-documents/surgical-masks-premarket-notification-510k-submissions (accessed on 26 May 2020).
- ASTM F2100-11(2018). Standard Specification for Performance of Materials Used in Medical Face Masks; ASTM International: West Conshohocken, PA, USA, 2018; Available online: https://www.astm.org/Standards/F2100.htm (accessed on 27 July 2020).
- Coronavirus: Harmonised Standards for Medical Devices. 2020. Available online: https://ec.europa.eu/commission/presscorner/detail/en/ip_20_522 (accessed on 6 July 2020).
- Rengasamy, A.; Zhuang, Z.; Berryann, R. Respiratory protection against bioaerosols: Literature review and research needs. Am. J. Infect. Control 2004, 32, 345–354. [Google Scholar] [CrossRef]
- Ippolito, M.; Vitale, F.; Accurso, G.; Iozzo, P.; Gregoretti, C.; Giarratano, A.; Cortegiani, A. Medical masks and Respirators for the Protection of Healthcare Workers from SARS-CoV-2 and other viruses. Pulmonology 2020, 26, 204–212. [Google Scholar] [CrossRef]
- British Standards Institution. Respiratory Protective Devices-Filtering Half Masks to Protect against Particles-Requirements, Testing, Marking; British Standards Institution: London, UK, 2020; Available online: https://books.google.ie/books/about/Respiratory_Protective_Devices_Filtering.html?id=4A3TAAAACAAJ&source=kp_book_description&redir_esc=y (accessed on 27 July 2020).
- Serfozo, N.; Ondracek, J.; Zíková, N.; Lazaridis, M.; Zdimal, V. Size-Resolved Penetration of Filtering Materials from CE-Marked Filtering Facepiece Respirators. Aerosol Air Qual. Res. 2017, 17, 1305–1315. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. Recommendation Regarding the Use of Cloth Face Coverings, Especially in Areas of Significant Community-Based Transmission. 2020. Available online: https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/cloth-face-cover.html (accessed on 22 May 2020).
- Konda, A.; Prakash, A.; Moss, G.A.; Schmoldt, M.; Grant, G.D.; Guha, S. Aerosol Filtration Efficiency of Common Fabrics Used in Respiratory Cloth Masks. ACS Nano 2020. [Google Scholar] [CrossRef]
- Nelson Labs. Respirator Precertification Tests – NIOSH. Available online: https://www.nelsonlabs.com/testing/respirator-pre-certification-tests-niosh/ (accessed on 19 May 2020).
- World Health Organization. Advice on the Use of Masks in the Context of COVID-19: Interim Guidance, 6 April 2020. 2020. Available online: https://apps.who.int/iris/handle/10665/331693 (accessed on 27 July 2020).
- HSE. Respiratory Protective Equipment at Work- A Practical Guide. 2013. Available online: https://www.hse.gov.uk/pUbns/priced/hsg53.pdf (accessed on 27 July 2020).
- HSE. Regulation 11 Health Surveillance. In Appendix A: Control of Substances Hazardous to Health Regulations; HSE: London, UK, 2002. Available online: https://www.hse.gov.uk/pUbns/priced/l5.pdf (accessed on 27 July 2020).
- HSE. Personal Protective Equipment at Work Personal Protective Equipment at Work Regulations 1992. 2015. Available online: https://www.hse.gov.uk/pUbns/priced/l25.pdf (accessed on 27 July 2020).
- Coia, J.; Ritchie, L.; Adisesh, A.; Booth, C.M.; Bradley, C.; Bunyan, D.; Carson, G.; Fry, C.; Hoffman, P.; Jenkins, D.; et al. Guidance on the use of respiratory and facial protection equipment. J. Hosp. Infect. 2013, 85, 170–182. [Google Scholar] [CrossRef]
- U.S. Food and Drug Administration. N95 Respirators and Surgical Masks (Face Masks). 2020. Available online: https://www.fda.gov/medical-devices/personal-protective-equipment-infection-control/n95-respirators-and-surgical-masks-face-masks (accessed on 27 July 2020).
- Health Protection Surveillance Centre. Guidance on the Use of Surgical Masks When Healthcare Is Being Provided in the Context of the COVID-19 Pandemic. 2020. Available online: https://www.hpsc.ie/a-z/respiratory/coronavirus/novelcoronavirus/guidance/infectionpreventionandcontrolguidance/ppe/useofsurgicalmasksinhealthcaresetting/ (accessed on 27 July 2020).
- Ireland Health Service Executive. Guidance on the Use of Personal Protective Equipment (PPE) in Disability Services. 2020. Available online: https://www.hse.ie/eng/services/news/newsfeatures/covid19-updates/partner-resources/guidance-on-the-use-of-ppe-in-disability-services.pdf (accessed on 27 July 2020).
- Centers for Disease Control and Prevention. Decontamination and Reuse of Filtering Facepiece Respirators. 2020. Available online: https://www.cdc.gov/coronavirus/2019-ncov/hcp/ppe-strategy/decontamination-reuse-respirators.html (accessed on 27 July 2020).
- Sutherland, K.; Chase, G. Section 2 - Filter Media. In Filters and Filtration Handbook, 5th ed.; Elsevier: Oxford, UK, 2008; pp. 41–95. [Google Scholar]
- Bien, C.; Revoir, W.H. Respiratory Protection Handbook; Taylor & Francis Limited: Oxforshire, UK, 2019. [Google Scholar]
- Davis, E.J. Introduction to Aerosol Science By Parker C. Reist, Macmillan, 1984, 299 pp., $38.00. AIChE J. 1986, 32, 175. [Google Scholar] [CrossRef]
- Kraemer, H.F.; Johnstone, H.F. Collection of Aerosol Particles in Presence of Electrostatic Fields. Ind. Eng. Chem. 1955, 47, 2426–2434. [Google Scholar] [CrossRef]
- Lee, K.W.; Liu, B.Y.H. Theoretical Study of Aerosol Filtration by Fibrous Filters. Aerosol Sci. Technol. 1982, 1, 147–161. [Google Scholar] [CrossRef]
- Fo, O.B.D.; Marra, W.D.; Kachan, G.C.; Coury, J.R. Filtration of Electrified Solid Particles. Ind. Eng. Chem. Res. 2000, 39, 3884–3895. [Google Scholar] [CrossRef]
- Zhu, C.; Lin, C.-H.; Cheung, C.S. Inertial impaction-dominated fibrous filtration with rectangular or cylindrical fibers. Powder Technol. 2000, 112, 149–162. [Google Scholar] [CrossRef]
- Van Turnhout, J. Electret filters for high-efficiency air cleaning? J. Electrost. 1980, 8, 369–379. [Google Scholar] [CrossRef]
- Li, S.-S.; Leggio, A.J.; Menzie, G.H.; Devore, D.; McNamara, J.J.; Yu, T.; Horsey, D.W. Process of Imparting Wettability to a Polyolefin Fiber. Justia Patent 20120270111, 4 March 2014. [Google Scholar]
- Klun, T.P.; Dunshee, W.K.; Schaffer, K.R.; Andrews, J.F.; Neu, D.M.; Scholz, M.T. Hydrophilic Polypropylene Fibers having Antimicrobial Activity. U.S. Patent US7879746B2, 13 July 2004. [Google Scholar]
- Liu, Z.; Yu, D.; Ge, Y.; Wang, L.; Zhang, J.; Li, H.; Liu, F.; Zhai, Z. Understanding the factors involved in determining the bioburdens of surgical masks. Ann. Transl. Med. 2019, 7, 754. [Google Scholar] [CrossRef]
- Zhou, S.S.; Lukula, S.; Chiossone, C.; Nims, R.W.; Suchmann, D.B.; Ijaz, M.K. Assessment of a respiratory face mask for capturing air pollutants and pathogens including human influenza and rhinoviruses. J. Thorac. Dis. 2018, 10, 2059–2069. [Google Scholar] [CrossRef] [Green Version]
- Tuite, A.R.; Fisman, D.N.; Greer, A.L. Mathematical modelling of COVID-19 transmission and mitigation strategies in the population of Ontario, Canada. Can. Med Assoc. J. 2020, 192, E497–E505. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Griffin, J.T.; Bhatt, S.; E Sinka, M.; Gething, P.W.; Lynch, M.; Patouillard, E.; Shutes, E.; Newman, R.D.; Alonso, P.; E Cibulskis, R.; et al. Potential for reduction of burden and local elimination of malaria by reducing Plasmodium falciparum malaria transmission: A mathematical modelling study. Lancet Infect. Dis. 2016, 16, 465–472. [Google Scholar] [CrossRef] [Green Version]
- Toda, A.A. Susceptible-infected-recovered (sir) dynamics of covid-19 and economic impact. arXiv 2020, arXiv:2003.11221. [Google Scholar]
- Biswas, K.; Khaleque, A.; Sen, P. Covid-19 spread: Reproduction of data and prediction using a SIR model on Euclidean network. arXiv 2020, arXiv:2003.07063. [Google Scholar]
- Bastos, S.B.; Cajueiro, D.O. Modeling and forecasting the Covid-19 pandemic in Brazil. arXiv 2020, arXiv:2003.14288. [Google Scholar]
- Chang, S.L.; Harding, N.; Zachreson, C.; Cliff, O.M.; Prokopenko, M. Modelling transmission and control of the COVID-19 pandemic in Australia. arXiv 2020, arXiv:2003.10218. [Google Scholar]
- Liu, D.; Clemente, L.; Poirier, C.; Ding, X.; Chinazzi, M.; Davis, J.T.; Vespignani, A.; Santillana, M. A machine learning methodology for real-time forecasting of the 2019-2020 COVID-19 outbreak using Internet searches, news alerts, and estimates from mechanistic models. arXiv 2020, arXiv:2004.04019. [Google Scholar]
- Mejía, S.; Wong, R. EMPIRICAL ISSUES IN THE STUDY OF COGNITIVE AGING THROUGH POPULATION-BASED STUDIES. Innov. Aging 2018, 2, 245–246. [Google Scholar] [CrossRef]
- Kiesling, E.; Günther, M.; Stummer, C.; Wakolbinger, L. Agent-based simulation of innovation diffusion: A review. Central Eur. J. Oper. Res. 2011, 20, 183–230. [Google Scholar] [CrossRef]
- Eikenberry, S.E.; Mancuso, M.; Iboi, E.; Phan, T.; Eikenberry, K.; Kuang, Y.; Kostelich, E.; Gumel, A.B. To mask or not to mask: Modeling the potential for face mask use by the general public to curtail the COVID-19 pandemic. Infect. Dis. Model. 2020, 5, 293–308. [Google Scholar] [CrossRef]
- Brienen, N.C.J.; Timen, A.; Wallinga, J.; Van Steenbergen, J.E.; Teunis, P.F.M. The Effect of Mask Use on the Spread of Influenza During a Pandemic. Risk Anal. 2010, 30, 1210–1218. [Google Scholar] [CrossRef] [PubMed]
- Schimit, P.; Monteiro, L. Who should wear mask against airborne infections? Altering the contact network for controlling the spread of contagious diseases. Ecol. Model. 2010, 221, 1329–1332. [Google Scholar] [CrossRef]
- Tracht, S.M.; Del Valle, S.Y.; Hyman, J.M. Mathematical Modeling of the Effectiveness of Facemasks in Reducing the Spread of Novel Influenza A (H1N1). PLoS ONE 2010, 5, e9018. [Google Scholar] [CrossRef]
- MacIntyre, C.R.; Cauchemez, S.; Dwyer, D.E.; Seale, H.; Cheung, P.; Browne, G.; Fasher, M.; Wood, J.; Gao, Z.; Booy, R.; et al. Face mask use and control of respiratory virus transmission in households. Emerging Infect. Dis. 2009, 15, 233–241. [Google Scholar] [CrossRef]
- Kai, D.; Goldstein, G.P.; Morgunov, A.; Nangalia, V.; Rotkirch, A. Universal Masking is Urgent in the COVID-19 Pandemic: SEIR and Agent Based Models, Empirical Validation, Policy Recommendations. arXiv 2020, arXiv:2004.13553. [Google Scholar]
- Li, Y.; Leung, P.H.; Yao, L.; Song, Q.; Newton, E. Antimicrobial effect of surgical masks coated with nanoparticles. J. Hosp. Infect. 2006, 62, 58–63. [Google Scholar] [CrossRef]
- Borkow, G.; Zhou, S.S.; Page, T.; Gabbay, J. A Novel Anti-Influenza Copper Oxide Containing Respiratory Face Mask. PLoS ONE 2010, 5, e11295. [Google Scholar] [CrossRef] [Green Version]
- Ratnesar-Shumate, S.; Wu, C.-Y.; Wander, J.; Lundgren, D.; Farrah, S.; Lee, J.-H.; Wanakule, P.; Blackburn, M.; Lan, M.-F. Evaluation of Physical Capture Efficiency and Disinfection Capability of an Iodinated Biocidal Filter Medium. Aerosol Air Qual. Res. 2008, 8, 1–18. [Google Scholar] [CrossRef]
- Lee, J.-H.; Wu, C.-Y.; Wysocki, K.M.; Farrah, S.; Wander, J. Efficacy of iodine-treated biocidal filter media against bacterial spore aerosols. J. Appl. Microbiol. 2008, 105, 1318–1326. [Google Scholar] [CrossRef]
- Pini, M.; Cedillo-González, E.I.; Neri, P.; Siligardi, C.; Ferrari, A.M. Assessment of Environmental Performance of TiO2 Nanoparticles Coated Self-Cleaning Float Glass. Coatings 2017, 7, 8. [Google Scholar] [CrossRef] [Green Version]
- Akduman, C.; Kumbasar, E.P.A. Nanofibers in face masks and respirators to provide better protection. IOP Conf. Series: Mater. Sci. Eng. 2018, 460, 012013. [Google Scholar] [CrossRef]
- Thavasi, V.; Singh, G.; Ramakrishna, S. Electrospun nanofibers in energy and environmental applications. Energy Environ. Sci. 2008, 1, 205. [Google Scholar] [CrossRef]
- Ramaseshan, R.; Sundarrajan, S.; Liu, Y.; Barhate, R.S.; Lala, N.L.; Ramakrishna, S. Functionalized polymer nanofibre membranes for protection from chemical warfare stimulants. Nanotechnology 2006, 17, 2947–2953. [Google Scholar] [CrossRef]
- Zhu, M.; Han, J.; Wang, F.; Shao, W.; Xiong, R.; Zhang, Q.; Pan, H.; Yang, Y.; Samal, S.K.; Zhang, F.; et al. Electrospun Nanofibers Membranes for Effective Air Filtration. Macromol. Mater. Eng. 2016, 302, 1600353. [Google Scholar] [CrossRef]
- Skaria, S.D.; Smaldone, G.C. Respiratory source control using surgical masks with nanofiber media. Ann. Occup. Hyg. 2014, 58, 771–781. [Google Scholar] [CrossRef] [Green Version]
- Suen, L.K.; Guo, Y.P.; Ho, S.S.; Au-Yeung, C.H.; Lam, S. Comparing mask fit and usability of traditional and nanofibre N95 filtering facepiece respirators before and after nursing procedures. J. Hosp. Infect. 2020, 104, 336–343. [Google Scholar] [CrossRef] [Green Version]
- Tong, H.W.; Kwok, S.K.C.; Kwok, H.C. Protective Masks with Coating Comprising Different Electrospun Fibers Interweaved with Each Other, Formulations Forming the Same, and Method of Producing Thereof. Patent WO2016101848A1, 30 June 2016. [Google Scholar]
- Wang, N.; Yang, Y.; Al-Deyab, S.S.; El-Newehy, M.; Yu, J.; Ding, B. Ultra-light 3D nanofibre-nets binary structured nylon 6–polyacrylonitrile membranes for efficient filtration of fine particulate matter. J. Mater. Chem. A 2015, 3, 23946–23954. [Google Scholar] [CrossRef]
- Akduman, C. Cellulose acetate and polyvinylidene fluoride nanofiber mats for N95 respirators. J. Ind. Text. 2019. [Google Scholar] [CrossRef]
- Wang, C.; Li, P.; Zong, Y.; Zhang, Y.; Li, S.; Wei, F. A high efficiency particulate air filter based on agglomerated carbon nanotube fluidized bed. Carbon 2014, 79, 424–431. [Google Scholar] [CrossRef]
- Li, X.; Wang, N.; Fan, G.; Yu, J.; Gao, J.; Sun, G.; Ding, B. Electreted polyetherimide–silica fibrous membranes for enhanced filtration of fine particles. J. Colloid Interface Sci. 2015, 439, 12–20. [Google Scholar] [CrossRef]
- Bortolassi, A.C.C.; Guerra, V.G.; Aguiar, M.L.; Soussan, L.; Cornu, D.; Miele, P.; Bechelany, M. Composites Based on Nanoparticle and Pan Electrospun Nanofiber Membranes for Air Filtration and Bacterial Removal. Nanomaterials 2019, 9, 1740. [Google Scholar] [CrossRef] [Green Version]
- Rubino, I.; Choi, H.-J. Respiratory Protection against Pandemic and Epidemic Diseases. Trends Biotechnol. 2017, 35, 907–910. [Google Scholar] [CrossRef]
- Kerry, R.G.; Malik, S.; Redda, Y.T.; Sahoo, S.; Patra, J.K.; Majhi, S. Nano-based approach to combat emerging viral (NIPAH virus) infection. Nanomed. Nanotechnol. Boil. Med. 2019, 18, 196–220. [Google Scholar] [CrossRef]
- Coronavirus: Nanotech Surface Sanitizes Milan with Nanomaterials Remaining Self-sterilized for Years. 2020. Available online: https://statnano.com//news/67531/Coronavirus-Nanotech-Surface-Sanitizes-Milan-with-Nanomaterials-Remaining-Self-sterilized-for-Years (accessed on 28 May 2020).
- Quan, F.-S.; Rubino, I.; Lee, S.-H.; Koch, B.; Choi, H.-J. Universal and reusable virus deactivation system for respiratory protection. Sci. Rep. 2017, 7, 39956. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Park, D.H.; Joe, Y.H.; Hwang, J. Dry Aerosol Coating of Anti-viral Particles on Commercial Air Filters Using a High-volume Flow Atomizer. Aerosol Air Qual. Res. 2019, 19, 1636–1644. [Google Scholar] [CrossRef]
- Abbasinia, M.; Karimie, S.; Haghighat, M.; Mohammadfam, I. Application of Nanomaterials in Personal Respiratory Protection Equipment: A Literature Review. Safety 2018, 4, 47. [Google Scholar] [CrossRef] [Green Version]
- Elechiguerra, J.L.; Burt, J.L.; Morones, J.R.; Camacho-Bragado, A.; Gao, X.; Lara, H.H.; Jose-Yacaman, M. Interaction of silver nanoparticles with HIV-1. J. Nanobiotechnol. 2005, 3, 6. [Google Scholar] [CrossRef] [Green Version]
- Hiragond, C.B.; Kshirsagar, A.S.; Dhapte, V.V.; Khanna, T.; Joshi, P.; More, P. Enhanced anti-microbial response of commercial face mask using colloidal silver nanoparticles. Vacuum 2018, 156, 475–482. [Google Scholar] [CrossRef]
- Vanangamudi, A.; Hamzah, S.; Singh, G. Synthesis of hybrid hydrophobic composite air filtration membranes for antibacterial activity and chemical detoxification with high particulate filtration efficiency (PFE). Chem. Eng. J. 2015, 260, 801–808. [Google Scholar] [CrossRef]
- Choi, J.; Yang, B.J.; Bae, G.-N.; Jung, J.H. Herbal Extract Incorporated Nanofiber Fabricated by an Electrospinning Technique and its Application to Antimicrobial Air Filtration. ACS Appl. Mater. Interfaces 2015, 7, 25313–25320. [Google Scholar] [CrossRef]
- Nicosia, A.; Gieparda, W.; Foksowicz-Flaczyk, J.; Walentowska, J.; Wesołek, D.; Vazquez, B.; Prodi, F.; Belosi, F. Air filtration and antimicrobial capabilities of electrospun PLA/PHB containing ionic liquid. Sep. Purif. Technol. 2015, 154, 154–160. [Google Scholar] [CrossRef]
- Ekabutr, P.; Chuysinuan, P.; Suksamrarn, S.; Sukhumsirichart, W.; Hongmanee, P.; Supaphol, P. Development of antituberculosis melt-blown polypropylene filters coated with mangosteen extracts for medical face mask applications. Polym. Bull. 2018, 76, 1985–2004. [Google Scholar] [CrossRef]
- Bhattacharjee, S.; Joshi, R.K.; Chughtai, A.A.; MacIntyre, C.R. Graphene Modified Multifunctional Personal Protective Clothing. Adv. Mater. Interfaces 2019, 6, 1900622. [Google Scholar] [CrossRef] [Green Version]
- Perreault, F.; Faria, A.F.; Nejati, S.; Elimelech, M. Antimicrobial Properties of Graphene Oxide Nanosheets: Why Size Matters. ACS Nano 2015, 9, 7226–7236. [Google Scholar] [CrossRef]
- Chen, Y.-N.; Hsueh, Y.-H.; Hsieh, C.-T.; Tzou, D.-Y.; Chang, P.-L. Antiviral Activity of Graphene–Silver Nanocomposites against Non-Enveloped and Enveloped Viruses. Int. J. Environ. Res. Public Health 2016, 13, 430. [Google Scholar] [CrossRef] [Green Version]
- Yang, A.; Cai, L.; Zhang, R.; Wang, J.; Hsu, P.-C.; Wang, H.; Zhou, G.; Xu, J.; Cui, Y. Thermal Management in Nanofiber-Based Face Mask. Nano Lett. 2017, 17, 3506–3510. [Google Scholar] [CrossRef]
- Liu, B.; Zhang, S.; Wang, X.; Yu, J.; Ding, B. Efficient and reusable polyamide-56 nanofiber/nets membrane with bimodal structures for air filtration. J. Colloid Interface Sci. 2015, 457, 203–211. [Google Scholar] [CrossRef]
- Rengasamy, S.; Eimer, B.; Shaffer, R.E. Simple Respiratory Protection—Evaluation of the Filtration Performance of Cloth Masks and Common Fabric Materials Against 20–1000 nm Size Particles. Ann. Occup. Hyg. 2010, 54, 789–798. [Google Scholar]
- Shakya, K.M.; Noyes, A.; Kallin, R.; E Peltier, R. Evaluating the efficacy of cloth facemasks in reducing particulate matter exposure. J. Expo. Sci. Environ. Epidemiol. 2016, 27, 352–357. [Google Scholar] [CrossRef]
- A Fischer, W.; Weber, D.J.; Wohl, D.A. Personal Protective Equipment: Protecting Health Care Providers in an Ebola Outbreak. Clin. Ther. 2015, 37, 2402–2410. [Google Scholar] [CrossRef] [Green Version]
- Viscusi, D.J.; Bergman, M.S.; Eimer, B.C.; Shaffer, R.E. Evaluation of Five Decontamination Methods for Filtering Facepiece Respirators. Ann. Occup. Hyg. 2009, 53, 815–827. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mills, D.; Harnish, D.A.; Lawrence, C.; Sandoval-Powers, M.; Heimbuch, B.K. Ultraviolet germicidal irradiation of influenza-contaminated N95 filtering facepiece respirators. Am. J. Infect. Control 2018, 46, e49–e55. [Google Scholar] [CrossRef]
- Lindsley, W.G.; Martin, S.B.; Thewlis, R.E.; Sarkisian, K.; Nwoko, J.O.; Mead, K.R.; Noti, J.D. Effects of Ultraviolet Germicidal Irradiation (UVGI) on N95 Respirator Filtration Performance and Structural Integrity. J. Occup. Environ. Hyg. 2015, 12, 509–517. [Google Scholar] [CrossRef]
- Grossman, J.; Pierce, A.; Mody, J.; Gagne, J.; Sykora, C.; Sayood, S.; Cook, S.; Shomer, N.; Liang, S.Y.; Eckhouse, S. Institution of a Novel Process for N95 Respirator Disinfection with Vaporized Hydrogen Peroxide in the Setting of the COVID-19 Pandemic at a Large Academic Medical Center. J. Am. Coll. Surg. 2020. [Google Scholar] [CrossRef]
- Lin, T.-H.; Chen, C.-C.; Huang, S.-H.; Kuo, C.-W.; Lai, C.-Y.; Lin, W.-Y. Filter quality of electret masks in filtering 14.6–594 nm aerosol particles: Effects of five decontamination methods. PLoS ONE 2017, 12, e0186217. [Google Scholar] [CrossRef] [Green Version]
- Li, D.F.; Cadnum, J.L.; Redmond, S.N.; Jones, L.D.; Donskey, C.J. It’s Not the Heat, It’s the Humidity: Effectiveness of a Rice Cooker-Steamer for Decontamination of Cloth and Surgical Face Masks and N95 Respirators. Am. J. Infect. Control 2020, 48, 854–855. [Google Scholar] [CrossRef]
- Bae, S.; Kim, M.-C.; Kim, J.Y.; Cha, H.-H.; Lim, J.S.; Jung, J.; Oh, D.K.; Lee, M.-K.; Choi, S.-H.; Sung, M.; et al. Effectiveness of Surgical and Cotton Masks in Blocking SARS–CoV-2: A Controlled Comparison in 4 Patients. Ann. Intern. Med. 2020, 173, 22. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dbouk, T.; Drikakis, D. On respiratory droplets and face masks. Phys. Fluids 2020, 32, 063303. [Google Scholar] [CrossRef]
- Derrick, J.; Gomersall, C.D. Protecting healthcare staff from severe acute respiratory syndrome: Filtration capacity of multiple surgical masks. J. Hosp. Infect. 2005, 59, 365–368. [Google Scholar] [CrossRef] [Green Version]
- Smereka, J.; Ruetzler, K.; Szarpak, L.; Filipiak, K.J.; Jaguszewski, M. Role of Mask/Respirator Protection Against SARS-CoV-2. Anesthesia Analg. 2020, 131, e33–e34. [Google Scholar] [CrossRef]
- Bar-On, Y.M.; Flamholz, A.; Phillips, R.; Milo, R. SARS-CoV-2 (COVID-19) by the numbers. eLife 2020, 9, 57309. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.-N. What Type of Face Mask is Appropriate for Everyone-Mask-Wearing Policy Amidst COVID-19 Pandemic? J. Korean Med. Sci. 2020, 35, e186. [Google Scholar] [CrossRef]
- Lam, S.C.; Lee, J.; Yau, S.; Charm, C. Sensitivity and specificity of the user-seal-check in determining the fit of N95 respirators. J. Hosp. Infect. 2011, 77, 252–256. [Google Scholar] [CrossRef] [PubMed]
- Morawska, L.; Cao, J. Airborne transmission of SARS-CoV-2: The world should face the reality. Environ. Int. 2020, 139, 105730. [Google Scholar] [CrossRef]
- Van Doremalen, N.; Bushmaker, T.; Morris, D.H.; Holbrook, M.G.; Gamble, A.; Williamson, B.N.; Tamin, A.; Harcourt, J.L.; Thornburg, N.J.; Gerber, S.I.; et al. Aerosol and Surface Stability of SARS-CoV-2 as Compared with SARS-CoV-1. New Engl. J. Med. 2020, 382, 1564–1567. [Google Scholar] [CrossRef]
- Ip, V.; Özelsel, T.J.P.; Sondekoppam, R.V.; Tsui, B.C.H. VID-19 pandemic: The 3R’s (reduce, refine, and replace) of personal protective equipment (PPE) sustainability. Can. J. Anesthesia 2020, 67, 1070–1071. [Google Scholar] [CrossRef]
- Starikovskiy, A.Y.; Usmanova, D.R. Medical mask with plasma sterilizing layer. arXiv 2020, arXiv:2004.00807. [Google Scholar]
- Eisenbrey, J.; Daecher, A. Temperature Sensitive Surgical Face Mask for Identifying at Risk Patients and Reducing Viral Infection. U.S. Patent US20190125011, 2 May 2019. [Google Scholar]
- Wang, R.; Li, Y.; Si, Y.; Wang, F.; Liu, Y.; Ma, Y.; Yu, J.; Yin, X.; Ding, B. Rechargeable polyamide-based N-halamine nanofibrous membranes for renewable, high-efficiency, and antibacterial respirators. Nanoscale Adv. 2019, 1, 1948–1956. [Google Scholar] [CrossRef] [Green Version]
- Rao, A.S.R.S.; Vazquez, J.A. Identification of COVID-19 can be quicker through artificial intelligence framework using a mobile phone–based survey when cities and towns are under quarantine. Infect. Control Hosp. Epidemiol. 2020, 1–5. [Google Scholar] [CrossRef] [Green Version]
- Javaid, M.; Haleem, A.; Vaishya, R.; Bahl, S.; Suman, R.; Vaish, A. Industry 4.0 technologies and their applications in fighting COVID-19 pandemic. Diabetes Metab. Syndr. Clin. Res. Rev. 2020, 14, 419–422. [Google Scholar] [CrossRef]
- Swennen, G.R.; Pottel, L.; Haers, P.E. Custom-made 3D-printed face masks in case of pandemic crisis situations with a lack of commercially available FFP2/3 masks. Int. J. Oral Maxillofacial Surg. 2020. [Google Scholar] [CrossRef]
- Nguyen, T.T. Artificial intelligence in the battle against coronavirus (COVID-19): A survey and future research directions. Preprint 2020. [Google Scholar] [CrossRef]
- Boulos, M.N.K.; Geraghty, E.M. Geographical tracking and mapping of coronavirus disease COVID-19/severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) epidemic andS associated events around the world: How 21st century GIS technologies are supporting the global fight against outbreaks and epidemics. Int. J. Health Geogr. 2020, 19, 8. [Google Scholar] [CrossRef] [Green Version]
- McCall, B. COVID-19 and artificial intelligence: Protecting health-care workers and curbing the spread. Lancet Digit. Health 2020, 2, e166–e167. [Google Scholar] [CrossRef]














© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
O’Dowd, K.; Nair, K.M.; Forouzandeh, P.; Mathew, S.; Grant, J.; Moran, R.; Bartlett, J.; Bird, J.; Pillai, S.C. Face Masks and Respirators in the Fight Against the COVID-19 Pandemic: A Review of Current Materials, Advances and Future Perspectives. Materials 2020, 13, 3363. https://doi.org/10.3390/ma13153363
O’Dowd K, Nair KM, Forouzandeh P, Mathew S, Grant J, Moran R, Bartlett J, Bird J, Pillai SC. Face Masks and Respirators in the Fight Against the COVID-19 Pandemic: A Review of Current Materials, Advances and Future Perspectives. Materials. 2020; 13(15):3363. https://doi.org/10.3390/ma13153363
Chicago/Turabian StyleO’Dowd, Kris, Keerthi M. Nair, Parnia Forouzandeh, Snehamol Mathew, Jamie Grant, Ruth Moran, John Bartlett, Jerry Bird, and Suresh C. Pillai. 2020. "Face Masks and Respirators in the Fight Against the COVID-19 Pandemic: A Review of Current Materials, Advances and Future Perspectives" Materials 13, no. 15: 3363. https://doi.org/10.3390/ma13153363
APA StyleO’Dowd, K., Nair, K. M., Forouzandeh, P., Mathew, S., Grant, J., Moran, R., Bartlett, J., Bird, J., & Pillai, S. C. (2020). Face Masks and Respirators in the Fight Against the COVID-19 Pandemic: A Review of Current Materials, Advances and Future Perspectives. Materials, 13(15), 3363. https://doi.org/10.3390/ma13153363