Differential Growth Characteristics of Crimean-Congo Hemorrhagic Fever Virus in Kidney Cells of Human and Bovine Origin
Abstract
:1. Introduction
2. Materials and Methods
2.1. Ethical Statement
2.2. Cells and Culture Conditions
2.3. Virus and Analysis of Growth Kinetics in the Cell Lines
2.4. Quantitative Real-Time Polymerase Chain Reaction (qRT-PCR)
2.5. Indirect Immunofluorescence Assay (IIFA)
2.6. LDH Assay
2.7. Statistical Analysis
3. Results
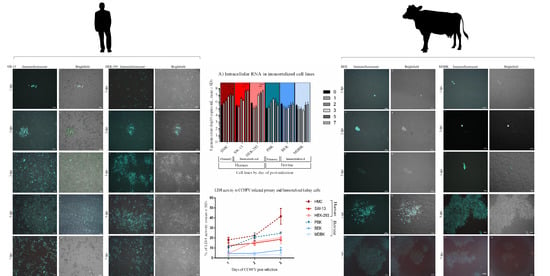
3.1. Bovine Kidney Cells Display Islet-Like Infection Pattern while Human Kidney Cells Show Overall Virus Infection and More Pronounced CPE
3.2. Viral Genome Load in Human but Not in Bovine Kidney Cells Increased Significantly with Time
3.3. Human Kidney Cells Display Higher Cytotoxicity
4. Discussion
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A
| HMC | IF score | CPE score | ||||||
| Day p.i | Mean | SD | N | Mean | SD | N | ||
| 1 | 1 | 0 | 3 | 0.333 | 0.577 | 3 | ||
| 2 | 1.333 | 0.577 | 3 | 1 | 0 | 3 | ||
| 3 | 1.333 | 0.577 | 3 | 2 | 0 | 3 | ||
| 5 | 2.333 | 0.577 | 3 | 3.333 | 0.577 | 3 | ||
| 7 | 4 | 0 | 3 | 4 | 0 | 3 | ||
| SW-13 | IF score | CPE score | ||||||
| Day p.i | Mean | SD | N | Mean | SD | N | ||
| 1 | 1 | 0 | 3 | 0.666 | 0.577 | 3 | ||
| 2 | 1.333 | 0.577 | 3 | 1.667 | 0.577 | 3 | ||
| 3 | 3.333 | 1.154 | 3 | 2.667 | 0.577 | 3 | ||
| 5 | 4 | 0 | 3 | 4 | 0 | 3 | ||
| 7 | 4 | 0 | 3 | 4 | 0 | 3 | ||
| HEK-293 | IF score | CPE score | ||||||
| Day p.i | Mean | SD | N | Mean | SD | N | ||
| 1 | 1.333 | 0.577 | 3 | 0 | 0 | 3 | ||
| 2 | 1.333 | 0.577 | 3 | 1 | 0 | 3 | ||
| 3 | 2.667 | 0.577 | 3 | 2.333 | 0.577 | 3 | ||
| 5 | 3.333 | 0.577 | 3 | 2.667 | 0.577 | 3 | ||
| 7 | 3.333 | 0.577 | 3 | 3.333 | 0.577 | 3 | ||
| PBK | IF score | CPE score | ||||||
| Day p.i | Mean | SD | N | Mean | SD | N | ||
| 1 | 1 | 0 | 3 | 0 | 0 | 3 | ||
| 2 | 1 | 0 | 3 | 0 | 0 | 3 | ||
| 3 | 1 | 0 | 3 | 1 | 0 | 3 | ||
| 5 | 1.333 | 0.577 | 3 | 1.333 | 0.577 | 3 | ||
| 7 | 1.333 | 0.577 | 3 | 2 | 0 | 3 | ||
| BEK | IF score | CPE score | ||||||
| Day p.i | Mean | SD | N | Mean | SD | N | ||
| 1 | 1 | 0 | 3 | 0 | 0 | 3 | ||
| 2 | 1 | 0 | 3 | 0 | 0 | 3 | ||
| 3 | 1 | 0 | 3 | 0.667 | 0.577 | 3 | ||
| 5 | 1.667 | 0.577 | 3 | 2 | 0 | 3 | ||
| 7 | 2.333 | 0.577 | 3 | 2 | 0 | 3 | ||
| MDBK | IF score | CPE score | ||||||
| Day p.i | Mean | SD | N | Mean | SD | N | ||
| 1 | 1 | 0 | 3 | 0 | 0 | 3 | ||
| 2 | 1 | 0 | 3 | 0 | 0 | 3 | ||
| 3 | 1 | 0 | 3 | 0.667 | 0.577 | 3 | ||
| 5 | 1.667 | 0.577 | 3 | 2 | 0 | 3 | ||
| 7 | 1.667 | 0.577 | 3 | 2 | 0 | 3 | ||
| HMC | IF stained cell number/well | PBK | IF stained cell number/well | |||||
| Day p.i | Mean | SD | N | Day p.i | Mean | SD | N | |
| 1 | 95 | 7.071 | 3 | 1 | 700 | 28.284 | 3 | |
| 2 | 2530 | 98.994 | 3 | 2 | 1100 | 84.852 | 3 | |
| 3 | 2735 | 91.923 | 3 | 3 | 1340 | 367.695 | 3 | |
| 5 | 5860 | 197.989 | 3 | 5 | 1420 | 311.127 | 3 | |
| 7 | 15,675 | 459.619 | 3 | 7 | 1440 | 226.274 | 3 | |
| SW-13 | IF stained cell number/well | BEK | IF stained cell number/well | |||||
| Day p.i | Mean | SD | N | Day p.i | Mean | SD | N | |
| 1 | 720 | 141.421 | 3 | 1 | 380 | 113.137 | 3 | |
| 2 | 3580 | 113.137 | 3 | 2 | 310 | 226.274 | 3 | |
| 3 | 12,200 | 1131.371 | 3 | 3 | 1090 | 268.7 | 3 | |
| 5 | 31,610 | 551.543 | 3 | 5 | 3740 | 1046.518 | 3 | |
| 7 | 13,900 | 5656.855 | 3 | 7 | 51,900 | 4101.219 | 3 | |
| HEK-293 | IF stained cell number/well | MDBK | IF stained cell number/well | |||||
| Day p.i | Mean | SD | N | Day p.i | Mean | SD | N | |
| 1 | 250 | 282.842 | 3 | 1 | 250 | 70.71 | 3 | |
| 2 | 2320 | 452.548 | 3 | 2 | 200 | 141.421 | 3 | |
| 3 | 16,500 | 707.106 | 3 | 3 | 415 | 304.055 | 3 | |
| 5 | 17,420 | 593.969 | 3 | 5 | 29,450 | 6293.251 | 3 | |
| 7 | 19,000 | 1414.214 | 3 | 7 | 28,440 | 3450.681 | 3 | |

References
- Spengler, J.R.; Patel, J.R.; Chakrabarti, A.K.; Zivcec, M.; García-Sastre, A.; Spiropoulou, C.F.; Bergeron, É. RIG-I Mediates an Antiviral Response to Crimean-Congo Hemorrhagic Fever Virus. J. Virol. 2015, 89, 10219–10229. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mertens, M.; Schmidt, K.; Ozkul, A.; Groschup, M.H. The impact of Crimean-Congo hemorrhagic fever virus on public health. Antivir. Res. 2013, 98, 248–260. [Google Scholar] [CrossRef] [PubMed]
- Elliott, R.M. Orthobunyaviruses: Recent genetic and structural insights. Nat. Rev. Microbiol. 2014, 12, 673. [Google Scholar] [CrossRef] [PubMed]
- Zivcec, M.; Metcalfe, M.G.; Albariño, C.G.; Guerrero, L.W.; Pegan, S.D.; Spiropoulou, C.F.; Bergeron, É. Assessment of Inhibitors of Pathogenic Crimean-Congo Hemorrhagic Fever Virus Strains Using Virus-Like Particles. PLoS Negl. Trop. Dis. 2015, 9, e0004259. [Google Scholar] [CrossRef] [Green Version]
- Haddock, E.; Feldmann, F.; Hawman, D.W.; Zivcec, M.; Hanley, P.W.; Saturday, G.; Scott, D.P.; Thomas, T.; Korva, M.; Avšič-Županc, T.; et al. A cynomolgus macaque model for Crimean–Congo haemorrhagic fever. Nat. Microbiol. 2018, 3, 556–562. [Google Scholar] [CrossRef]
- Spengler, J.R.; Estrada-Pena, A.; Garrison, A.R.; Schmaljohn, C.; Spiropoulou, C.F.; Bergeron, E.; Bente, D.A. A chronological review of experimental infection studies of the role of wild animals and livestock in the maintenance and transmission of Crimean-Congo hemorrhagic fever virus. Antivir. Res. 2016, 135, 31–47. [Google Scholar] [CrossRef] [Green Version]
- Cobo, F. Viruses Causing Hemorrhagic Fever. Safety Laboratory Procedures. Open Virol. J. 2016, 10, 1–9. [Google Scholar] [CrossRef]
- Spengler, J.R.; Estrada-Peña, A. Host preferences support the prominent role of Hyalomma ticks in the ecology of Crimean-Congo hemorrhagic fever. PLoS Negl. Trop. Dis. 2018, 12, e0006248. [Google Scholar] [CrossRef] [Green Version]
- Leblebicioglu, H.; Sunbul, M.; Memish, Z.A.; Al-Tawfiq, J.A.; Bodur, H.; Ozkul, A.; Gucukoglu, A.; Chinikar, S.; Hasan, Z. Consensus report: Preventive measures for Crimean-Congo Hemorrhagic Fever during Eid-al-Adha festival. Int. J. Infect. Dis. 2015, 38, 9–15. [Google Scholar] [CrossRef] [Green Version]
- Bente, D.A.; Alimonti, J.B.; Shieh, W.-J.; Camus, G.; Ströher, U.; Zaki, S.; Jones, S.M. Pathogenesis and immune response of Crimean-Congo hemorrhagic fever virus in a STAT-1 knockout mouse model. J. Virol. 2010, 84, 11089–11100. [Google Scholar] [CrossRef] [Green Version]
- Bereczky, S.; Lindegren, G.; Karlberg, H.; Akerstrom, S.; Klingstrom, J.; Mirazimi, A. Crimean-Congo hemorrhagic fever virus infection is lethal for adult type I interferon receptor-knockout mice. J. Gen. Virol. 2010, 91, 1473–1477. [Google Scholar] [CrossRef]
- Spengler, J.R.; Kelly Keating, M.; McElroy, A.K.; Zivcec, M.; Coleman-McCray, J.D.; Harmon, J.R.; Bollweg, B.C.; Goldsmith, C.S.; Bergeron, É.; Keck, J.G.; et al. Crimean-Congo Hemorrhagic Fever in Humanized Mice Reveals Glial Cells as Primary Targets of Neurological Infection. J. Infect. Dis. 2017, 216, 1386–1397. [Google Scholar] [CrossRef] [Green Version]
- Dowall, S.D.; Carroll, M.W.; Hewson, R. Development of vaccines against Crimean-Congo haemorrhagic fever virus. Vaccine 2017, 35, 6015–6023. [Google Scholar] [CrossRef] [PubMed]
- Lindquist, M.E.; Zeng, X.; Altamura, L.A.; Daye, S.P.; Delp, K.L.; Blancett, C.; Coffin, K.M.; Koehler, J.W.; Coyne, S.; Shoemaker, C.J.; et al. Exploring Crimean-Congo Hemorrhagic Fever Virus-Induced Hepatic Injury Using Antibody-Mediated Type I Interferon Blockade in Mice. J. Virol. 2018, 92, e01083-18. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Garrison, R.A.; Smith, R.D.; Golden, W.J. Animal Models for Crimean-Congo Hemorrhagic Fever Human Disease. Viruses 2019, 11, 590. [Google Scholar] [CrossRef] [Green Version]
- World Organization for Animal Helath. Chapter 3.1.5 Crimean-Congo Hemorrhagic Fever. In OIE Terrestrial Manual; World Organization for Animal Helath: Paris, France, 2018; pp. 399–406. Available online: https://www.oie.int/standard-setting/terrestrial-manual/access-online/ (accessed on 18 June 2020).
- Bartolini, B.; Gruber, C.E.; Koopmans, M.; Avšič, T.; Bino, S.; Christova, I.; Grunow, R.; Hewson, R.; Korukluoglu, G.; Lemos, C.M.; et al. Laboratory management of Crimean-Congo haemorrhagic fever virus infections: Perspectives from two European networks. Eurosurveillance 2019, 24, 1800093. [Google Scholar] [CrossRef] [Green Version]
- Bertolotti-Ciarlet, A.; Smith, J.; Strecker, K.; Paragas, J.; Altamura, L.A.; McFalls, J.M.; Frias-Stäheli, N.; García-Sastre, A.; Schmaljohn, C.S.; Doms, R.W. Cellular localization and antigenic characterization of crimean-congo hemorrhagic fever virus glycoproteins. J. Virol. 2005, 79, 6152–6161. [Google Scholar] [CrossRef] [Green Version]
- Burt, F.J.; Swanepoel, R.; Shieh, W.J.; Smith, J.F.; Leman, P.A.; Greer, P.W.; Coffield, L.M.; Rollin, P.E.; Ksiazek, T.G.; Peters, C.J.; et al. Immunohistochemical and in situ localization of Crimean-Congo hemorrhagic fever (CCHF) virus in human tissues and implications for CCHF pathogenesis. Arch. Pathol. Lab. Med. 1997, 121, 839–846. [Google Scholar]
- Ardalan, M.R.; Shane Tubbs, R.; Chinikar, S.; Shoja, M.M. Crimean–Congo haemorrhagic fever presenting as thrombotic microangiopathy and acute renal failure. Nephrol. Dial. Transplant. 2006, 21, 2304–2307. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Deveci, K.; Uysal, E.B.; Kaya, A.; Sancakdar, E.; Alkan, F. Evaluation of Renal Involvement in Children with Crimean-Congo Hemorrhagic Fever. Jpn. J. Infect. Dis. 2013, 66, 493–496. [Google Scholar] [CrossRef]
- Khazaei, Z.; Darvishi, I.; Amiri, M.; Sohrabivafa, M.; Kamran, S. Crimean Congo hemorrhagic fever: A brief report regarding kidney involvement. J. Ren. Inj. Prev. 2018, 7, 129–131. [Google Scholar] [CrossRef] [Green Version]
- Hölzer, M.; Krähling, V.; Amman, F.; Barth, E.; Bernhart, S.H.; Carmelo, V.A.O.; Collatz, M.; Doose, G.; Eggenhofer, F.; Ewald, J.; et al. Differential transcriptional responses to Ebola and Marburg virus infection in bat and human cells. Sci. Rep. 2016, 6, 34589. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sattentau, Q. Avoiding the void: Cell-to-cell spread of human viruses. Nat. Rev. Microbiol. 2008, 6, 815. [Google Scholar] [CrossRef] [PubMed]
- Sigal, A.; Kim, J.T.; Balazs, A.B.; Dekel, E.; Mayo, A.; Milo, R.; Baltimore, D. Cell-to-cell spread of HIV permits ongoing replication despite antiretroviral therapy. Nature 2011, 477, 95. [Google Scholar] [CrossRef] [PubMed]
- Valente, M.J.; Henrique, R.; Costa, V.L.; Jerónimo, C.; Carvalho, F.; Bastos, M.L.; de Pinho, P.G.; Carvalho, M. A rapid and simple procedure for the establishment of human normal and cancer renal primary cell cultures from surgical specimens. PLoS ONE 2011, 6, e19337. [Google Scholar] [CrossRef] [Green Version]
- Aligholipour Farzani, T.; Hanifehnezhad, A.; Földes, K.; Ergünay, K.; Yilmaz, E.; Hashim Mohamed Ali, H.; Ozkul, A. Co-Delivery Effect of CD24 on the Immunogenicity and Lethal Challenge Protection of a DNA Vector Expressing Nucleocapsid Protein of Crimean Congo Hemorrhagic Fever Virus. Viruses 2019, 11, 75. [Google Scholar] [CrossRef] [Green Version]
- Aligholipour Farzani, T.; Földes, K.; Hanifehnezhad, A.; Yener Ilce, B.; Bilge Dagalp, S.; Amirzadeh Khiabani, N.; Ergünay, K.; Alkan, F.; Karaoglu, T.; Bodur, H.; et al. Bovine Herpesvirus Type 4 (BoHV-4) Vector Delivering Nucleocapsid Protein of Crimean-Congo Hemorrhagic Fever Virus Induces Comparable Protective Immunity against Lethal Challenge in IFNα/β/γR−/− Mice Models. Viruses 2019, 11, 237. [Google Scholar] [CrossRef] [Green Version]
- Bhattacharjee, P.S.; Naylor, C.J.; Jones, R.C. A simple method for immunofluorescence staining of tracheal organ cultures for the rapid identification of infectious bronchitis virus. Avian Pathol. 1994, 23, 471–480. [Google Scholar] [CrossRef] [Green Version]
- Rizzardi, A.E.; Johnson, A.T.; Vogel, R.I.; Pambuccian, S.E.; Henriksen, J.; Skubitz, A.P.; Metzger, G.J.; Schmechel, S.C. Quantitative comparison of immunohistochemical staining measured by digital image analysis versus pathologist visual scoring. Diagn. Pathol. 2012, 7, 42. [Google Scholar] [CrossRef] [Green Version]
- Li, X.; Yang, H.; Huang, H.; Zhu, T. CELLCOUNTER: Novel Open-Source Software for Counting Cell Migration and Invasion In Vitro. Biomed. Res. Int. 2014, 2014, 863564. [Google Scholar] [CrossRef]
- Mehand, M.S.; Al-Shorbaji, F.; Millett, P.; Murgue, B. The WHO R&D Blueprint: 2018 review of emerging infectious diseases requiring urgent research and development efforts. Antivir. Res. 2018, 159, 63–67. [Google Scholar] [PubMed]
- Mazzola, L.T.; Kelly-Cirino, C. Diagnostic tests for Crimean-Congo haemorrhagic fever: A widespread tickborne disease. BMJ Glob. Heal. 2019, 4, e001114. [Google Scholar] [CrossRef] [Green Version]
- Longdon, B.; Brockhurst, M.A.; Russell, C.A.; Welch, J.J.; Jiggins, F.M. The evolution and genetics of virus host shifts. PLoS Pathog. 2014, 10, e1004395. [Google Scholar] [CrossRef] [Green Version]
- Coffey, L.L.; Vasilakis, N.; Brault, A.C.; Powers, A.M.; Tripet, F.; Weaver, S.C. Arbovirus evolution in vivo is constrained by host alternation. Proc. Natl. Acad. Sci. USA 2008, 105, 6970–6975. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Coffey, L.L.; Vignuzzi, M. Host alternation of chikungunya virus increases fitness while restricting population diversity and adaptability to novel selective pressures. J. Virol. 2011, 85, 1025–1035. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moutailler, S.; Roche, B.; Thiberge, J.-M.; Caro, V.; Rougeon, F.; Failloux, A.-B. Host alternation is necessary to maintain the genome stability of rift valley fever virus. PLoS Negl. Trop. Dis. 2011, 5, e1156. [Google Scholar] [CrossRef] [Green Version]
- Akinci, E.; Bodur, H.; Leblebicioglu, H. Pathogenesis of Crimean-Congo hemorrhagic fever. Vector Borne Zoonotic Dis. 2013, 13, 429–437. [Google Scholar] [CrossRef]
- Welch, S.R.; Ritter, J.M.; McElroy, A.K.; Harmon, J.R.; Coleman-McCray, J.D.; Scholte, F.E.M.; Kobinger, G.P.; Bergeron, É.; Zaki, S.R.; Nichol, S.T.; et al. Fluorescent Crimean-Congo hemorrhagic fever virus illuminates tissue tropism patterns and identifies early mononuclear phagocytic cell targets in IFNAR-/- mice. PLoS Pathog. 2019, 15, e1008183. [Google Scholar] [CrossRef] [Green Version]
- López-Montero, N.; Risco, C. Self-protection and survival of arbovirus-infected mosquito cells. Cell. Microbiol. 2011, 13, 300–315. [Google Scholar] [CrossRef]
- Cifuentes-Muñoz, N.; Dutch, R.E.; Cattaneo, R. Direct cell-to-cell transmission of respiratory viruses: The fast lanes. PLoS Pathog. 2018, 14, e1007015. [Google Scholar] [CrossRef] [Green Version]
- Chang, K.; Baginski, J.; Hassan, S.F.; Volin, M.; Shukla, D.; Tiwari, V. Filopodia and Viruses: An Analysis of Membrane Processes in Entry Mechanisms. Front. Microbiol. 2016, 7, 300. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhong, P.; Agosto, L.M.; Munro, J.B.; Mothes, W. Cell-to-cell transmission of viruses. Curr. Opin. Virol. 2013, 3, 44–50. [Google Scholar] [CrossRef] [Green Version]
- Mothes, W.; Sherer, N.M.; Jin, J.; Zhong, P. Virus cell-to-cell transmission. J. Virol. 2010, 84, 8360–8368. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hawman, D.W.; Feldmann, H. Recent advances in understanding Crimean-Congo hemorrhagic fever virus. F1000Research 2018, 7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bailey, M.; Christoforidou, Z.; Lewis, M.C. The evolutionary basis for differences between the immune systems of man, mouse, pig and ruminants. Vet. Immunol. Immunopathol. 2013, 152, 13–19. [Google Scholar] [CrossRef]
- Hasanoglu, I.; Guner, R.; Carhan, A.; Kocak Tufan, Z.; Yagci-Caglayik, D.; Guven, T.; Yilmaz, G.R.; Tasyaran, M.A. Crucial parameter of the outcome in Crimean Congo hemorrhagic fever: Viral load. J. Clin. Virol. 2016, 75, 42–46. [Google Scholar] [CrossRef]
- Ergunay, K.; Kocak Tufan, Z.; Bulut, C.; Kinikli, S.; Demiroz, A.P.; Ozkul, A. Antibody responses and viral load in patients with Crimean-Congo hemorrhagic fever: A comprehensive analysis during the early stages of the infection. Diagn. Microbiol. Infect. Dis. 2014, 79, 31–36. [Google Scholar] [CrossRef]
- Duh, D.; Saksida, A.; Petrovec, M.; Ahmeti, S.; Dedushaj, I.; Panning, M.; Drosten, C.; Avsic-Zupanc, T. Viral load as predictor of Crimean-Congo hemorrhagic fever outcome. Emerg. Infect. Dis. 2007, 13, 1769–1772. [Google Scholar] [CrossRef]
- Saksida, A.; Duh, D.; Wraber, B.; Dedushaj, I.; Ahmeti, S.; Avsic-Zupanc, T. Interacting roles of immune mechanisms and viral load in the pathogenesis of crimean-congo hemorrhagic fever. Clin. Vaccine Immunol. 2010, 17, 1086–1093. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kubar, A.; Haciomeroglu, M.; Ozkul, A.; Bagriacik, U.; Akinci, E.; Sener, K.; Bodur, H. Prompt administration of Crimean-Congo hemorrhagic fever (CCHF) virus hyperimmunoglobulin in patients diagnosed with CCHF and viral load monitorization by reverse transcriptase-PCR. Jpn. J. Infect. Dis. 2011, 64, 439–443. [Google Scholar] [PubMed]
- Hasanoglu, I.; Guner, R.; Carhan, A.K.; Tufan, Z.Y.; Caglayik, D.; Yilmaz, G.R.; Tasyaran, M.A. Dynamics of viral load in Crimean Congo hemorrhagic fever. J. Med. Virol. 2018, 90, 639–643. [Google Scholar] [CrossRef]
- Haferkamp, S.; Fernando, L.; Schwarz, T.F.; Feldmann, H.; Flick, R. Intracellular localization of Crimean-Congo Hemorrhagic Fever (CCHF) virus glycoproteins. Virol. J. 2005, 2, 42. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ergonul, O.; Battal, I. Potential Sexual Transmission of Crimean-Congo Hemorrhagic Fever Infection. Jpn. J. Infect. Dis. 2014, 67, 137–138. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pshenichnaya, N.Y.; Sydenko, I.S.; Klinovaya, E.P.; Romanova, E.B.; Zhuravlev, A.S. Possible sexual transmission of Crimean-Congo hemorrhagic fever. Int. J. Infect. Dis. 2016, 45, 109–111. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Leblebicioglu, H.; Ozaras, R.; Sunbul, M. Crimean-Congo hemorrhagic fever: A neglected infectious disease with potential nosocomial infection threat. Am. J. Infect. Control. 2017, 45, 815–816. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yadav, P.D.; Patil, D.Y.; Shete, A.M.; Kokate, P.; Goyal, P.; Jadhav, S.; Sinha, S.; Zawar, D.; Sharma, S.K.; Kapil, A.; et al. Nosocomial infection of CCHF among health care workers in Rajasthan, India. BMC Infect. Dis. 2016, 16, 624. [Google Scholar] [CrossRef] [Green Version]










| Cell Line | Abbreviation | Culture Requirements | Resources |
|---|---|---|---|
| Human | |||
| Human primary mesangial cell line | HMC | Eagle’s minimum essential medium | Hacettepe University, Ankara, Turkey |
| Human adrenal gland/cortex Scott and White No. 13 | SW-13 | Leibovitz’s L-15 medium | National Public Health and Medical Officer Service, Hungary |
| Human embryonic kidney | HEK-293 | Minimum essential medium alpha | Departmental culture collection: ATCC no. CRL-1573 |
| Bovine | |||
| Primary bovine kidney cortex cell | PBK | Eagle’s minimum essential medium | In-house |
| Madin–Darby bovine kidney | MDBK | Eagle’s minimum essential medium | Departmental culture collection: ATCC no. CCL-22 |
| Bovine embryonic kidney | BEK | Eagle’s minimum essential medium | Dipartimento di Salute Animale, Sezione di Malattie Infettive, Facoltà di Medicina Veterinaria, via del Taglio 8, 43100 Parma, Italy |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Földes, K.; Aligholipour Farzani, T.; Ergünay, K.; Ozkul, A. Differential Growth Characteristics of Crimean-Congo Hemorrhagic Fever Virus in Kidney Cells of Human and Bovine Origin. Viruses 2020, 12, 685. https://doi.org/10.3390/v12060685
Földes K, Aligholipour Farzani T, Ergünay K, Ozkul A. Differential Growth Characteristics of Crimean-Congo Hemorrhagic Fever Virus in Kidney Cells of Human and Bovine Origin. Viruses. 2020; 12(6):685. https://doi.org/10.3390/v12060685
Chicago/Turabian StyleFöldes, Katalin, Touraj Aligholipour Farzani, Koray Ergünay, and Aykut Ozkul. 2020. "Differential Growth Characteristics of Crimean-Congo Hemorrhagic Fever Virus in Kidney Cells of Human and Bovine Origin" Viruses 12, no. 6: 685. https://doi.org/10.3390/v12060685
APA StyleFöldes, K., Aligholipour Farzani, T., Ergünay, K., & Ozkul, A. (2020). Differential Growth Characteristics of Crimean-Congo Hemorrhagic Fever Virus in Kidney Cells of Human and Bovine Origin. Viruses, 12(6), 685. https://doi.org/10.3390/v12060685