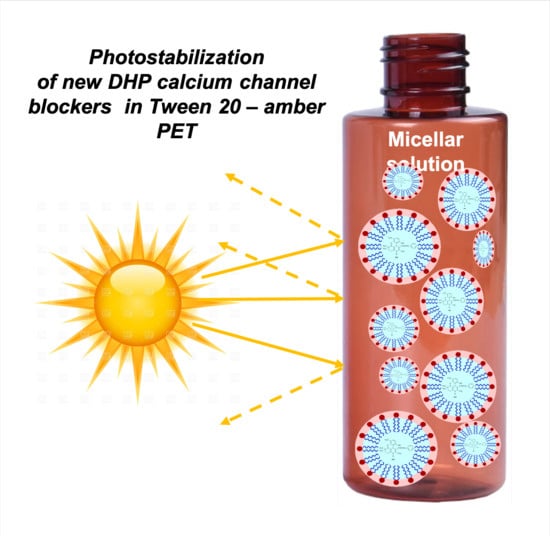
A New Generation of Dihydropyridine Calcium Channel Blockers: Photostabilization of Liquid Formulations Using Nonionic Surfactants
Abstract
:1. Introduction
2. Materials and Methods
2.1. Chemicals
2.2. Instruments
2.3. Standard Solutions
2.4. Preparation of the Drug–Cyclodextrin (CD) Complex
2.5. Preparation of Micellar Solutions
2.6. Photodegradation Studies
2.7. Chemometric Elaboration
3. Results
3.1. Photodegradation in Ethanol Solution
3.2. Photodegradation in Cyclodextrin Complex
3.3. Photodegradation in Micellar Solution
3.4. Photodegradation Studies of DHPs in PET Containers
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Zamponi, G.W.; Striessnig, J.; Koschak, A.; Dolphin, A.C. The Physiology, Pathology, and Pharmacology of Voltage-Gated Calcium Channels and Their Future Therapeutic Potential. Pharmacol. Rev. 2015, 67, 821–870. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Drapak, I.; Perekhoda, L.; Tsapko, T.; Berezniakova, N.; Tsapko, Y. Cardiovascular Calcium Channel Blockers: Historical Overview, Development and New Approaches in Design. J. Heterocycl. Chem. 2017, 54, 2117–2128. [Google Scholar] [CrossRef]
- Snutch, T.P.; Zamponi, G.W. Recent advances in the development of T-type calcium channel blockers for pain intervention. Br. J. Pharmacol. 2018, 175, 2375–2383. [Google Scholar] [CrossRef]
- Cain, S.M.; Snutch, T.P. Contributions of T-type calcium channel isoforms to neuronal firing. Channels 2010, 4, 475–482. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Carafoli, E. Special issue: Calcium signaling and disease. Biochem. Biophys. Res. Commun. 2004, 323, 1097. [Google Scholar] [CrossRef]
- Tsien, R.W.; Ellinor, P.T.; Horne, W.A. Molecular diversity of voltage dependent Ca2+ channels. Trends Pharmacol. Sci. 1991, 12, 349–354. [Google Scholar] [CrossRef]
- Bladen, C.; Gunduz, M.G.; Şimşek, R.; Şafak, C.; Zamponi, G.W. Synthesis and Evaluation of 1,4-Dihydropyridine Derivatives with Calcium Channel Blocking Activity. Pflugers Arch. Eur. J. Physiol. 2014, 466, 1355–1363. [Google Scholar] [CrossRef] [PubMed]
- Bladen, C.; Gadotti, V.M.; Gündüz, M.G.; Berger, N.D.; Şimşek, R.; Şafak, C.; Zamponi, G.W. 1,4-Dihydropyridine derivatives with T-type calcium channel blocking activity attenuate inflammatory and neuropathic pain. Pflugers Arch. Eur. J. Physiol. 2015, 467, 1237–1247. [Google Scholar] [CrossRef]
- Schaller, D.; Gündüz, M.G.; Zhang, F.X.; Zamponi, G.W.; Wolber, G. Binding mechanism investigations guiding the synthesis of novel condensed 1,4-dihydropyridine derivatives with L-/T-type calcium channel blocking activity. Eur. J. Med. Chem. 2018, 155, 1–12. [Google Scholar] [CrossRef]
- Gadotti, V.; Bladen, C.; Zhang, F.X.; Chen, L.; Gündüz, M.G.; Şimşek, R.; Şafak, C.; Zamponi, G.W. Analgesic effect of a broad spectrum dihydropyridine inhibitor of voltage gated calcium channels. Pflugers Arch. Eur. J. Physiol. 2015, 467, 2485–2493. [Google Scholar] [CrossRef]
- Maafi, W.; Maafi, M. Modelling nifedipine photodegradation, photostability and actinometric properties. Int. J. Pharm. 2013, 456, 153–164. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vetuschi, C.; Ragno, G.; Veronico, M.; Risoli, A.; Gianandrea, A. Comparative Evaluation of Analytical Methods for Simultaneous Determination of Nisoldipine and Its Photodegradation Products. Anal. Lett. 2002, 35, 1327–1339. [Google Scholar] [CrossRef]
- Fasani, E.; Albini, A.; Mella, M. Photochemistry of Hantzsch 1,4-dihydropyridines and pyridines. Tetrahedron 2008, 64, 3190–3196. [Google Scholar] [CrossRef]
- Ioele, G.; Gündüz, M.G.; De Luca, M.; Simone, R.; Şafak, C.; Muzzalupo, R.; Ragno, G. Photodegradation studies of 1,4-dihydropyridine compounds by MCR analysis on UV spectral data. Future Med. Chem. 2016, 8, 107–115. [Google Scholar] [CrossRef] [PubMed]
- Ioele, G.; Oliverio, F.; Andreu, I.; De Luca, M.; Miranda, M.A.; Ragno, G. Different photodegradation behavior of barnidipine under natural and forced irradiation. J. Photochem. Photobiol. A Chem. 2010, 215, 205–213. [Google Scholar] [CrossRef]
- Gündüz, M.G.; Ragno, G.; Şimşek, R.; De Luca, M.; Şafak, C.; Grande, F.; El Khouly, A.; İşli, F.; Yildirim, S.; Fincan, G.S.O.; Ioele, G. Synthesis and photodegradation studies of analogues of muscle relaxant 1,4-dihydropyridine compounds. Acta Pharm. 2017, 67, 341–355. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ragno, G.; Ioele, G.; De Luca, M.; Garofalo, A.; Grande, F.; Risoli, A. A critical study on the application of the zero-crossing derivative spectrophotometry to the photodegradation monitoring of lacidipine. J. Pharm. Biomed. Anal. 2006, 42, 39–45. [Google Scholar] [CrossRef] [PubMed]
- Dinç, E.; Ragno, G.; Ioele, G.; Baleanu, D. Fractional wavelet analysis for the simultaneous quantitative resolution of lacidipine and its photo-degradation product by continuous wavelet transform and multilinear regression calibration. J. AOAC Int. 2006, 89, 1538–1546. [Google Scholar] [PubMed]
- Ragno, G.; Vetuschi, C.; Risoli, A.; Ioele, G. Application of a classical least squares regression method to the assay of 1,4-dihydropyridine antihypertensives and their photoproducts. Talanta 2003, 59, 357–382. [Google Scholar] [CrossRef]
- Ragno, G.; Veronico, M.; Vetuschi, C. Analysis of nimodipine and its photodegradation product by derivative spectrophotometry and gas chromatography. Int. J. Pharm. 1995, 119, 115–119. [Google Scholar] [CrossRef]
- Ragno, G.; Veronico, M.; Vetuschi, C. Gaschromatographic and UV derivative determination of Nitrendipine and its photodegradation product. Int. J. Pharm. 1993, 99, 351–355. [Google Scholar] [CrossRef]
- Ioele, G.; De Luca, M.; Oliverio, F.; Ragno, G. Prediction of photosensitivity of 1,4-dihydropyridine antihypertensives by quantitative structure-property relationship. Talanta 2009, 79, 1418–1424. [Google Scholar] [CrossRef] [PubMed]
- Ioele, G.; De Luca, M.; Ragno, G. Photostability of barnidipine in combined cyclodextrin-in-liposome matrices. Future Med. Chem. 2014, 6, 35–43. [Google Scholar] [CrossRef] [PubMed]
- Ragno, G.; Cione, E.; Garofalo, A.; Genchi, G.; Ioele, G.; Risoli, A.; Spagnoletta, A. Design and monitoring of photostability systems for amlodipine dosage forms. Int. J. Pharm. 2003, 265, 125–132. [Google Scholar] [CrossRef] [PubMed]
- Ragno, G.; Risoli, A.; Ioele, G.; Cione, E.; De Luca, M. Photostabilization of 1,4-dihidropyridine antihypertensives by incorporation into β-cyclodextrin and liposomes. J. Nanosci. Nanotechnol. 2006, 6, 2979–2985. [Google Scholar] [CrossRef] [PubMed]
- Mohd-Maidin, N.; Oruna-Concha, M.J.; Jauregi, P. Surfactant TWEEN20 provides stabilisation effect on anthocyanins extracted from red grape pomace. Food Chem. 2019, 271, 224–231. [Google Scholar] [CrossRef] [PubMed]
- Gürbüz, G.; Kauntola, V.; Ramos Diaz, J.M.; Jouppila, K.; Heinonen, M. Oxidative and physical stability of oil-in-water emulsions prepared with quinoa and amaranth proteins. Eur. Food Res. Technol. 2018, 244, 469–479. [Google Scholar] [CrossRef]
- Naseef, M.A.; Ibrahim, H.K.; Nour, S.A.E.K. Solid form of lipid-based self-nanoemulsifying drug delivery systems for minimization of diacerein adverse effects: Development and bioequivalence evaluation in albino rabbits. AAPS PharmSciTech 2018, 19, 3097–3109. [Google Scholar] [CrossRef]
- Szymczyk, K.; Szaniawska, M.; Taraba, A. Micellar parameters of aqueous solutions of tween 20 and 60 at different temperatures: Volumetric and viscometric study. Colloids Int. 2018, 2, 34. [Google Scholar] [CrossRef]
- De Luca, M.; Ioele, G.; Spatari, C.; Ragno, G. Photostabilization studies of antihypertensive 1,4-dihydropyridines using polymeric containers. Int. J. Pharm. 2016, 505, 376–382. [Google Scholar] [CrossRef]
- International Conference on Harmonization. Stability Testing of New Drug Substances and Products; ICH Q1A(R2); IFPMA: Geneva, Switzerland, 2003. [Google Scholar]
- de Juan, A.; Rutan, S.C.; Maeder, M.; Tauler, R. Comprehensive Chemometrics; Elsevier: Amsterdam, The Netherlands, 2009; Volume 2. [Google Scholar]
- Rajko, R.; Istvan, K.J. Analytical solution for determining feasible regions of Self Modeling Curve Resolution (SMCR) method based on computational geometry. J. Chemom. 2005, 19, 448–463. [Google Scholar] [CrossRef]
- De Luca, M.; Mas, S.; Ioele, G.; Oliverio, F.; Ragno, G.; Tauler, R. Kinetic studies of nitrofurazone photodegradation by multivariate curve resolution applied to UV-spectral data. Int. J. Pharm. 2010, 386, 99–107. [Google Scholar] [CrossRef] [PubMed]
- De Luca, M.; Tauler, R.; Ioele, G.; Ragno, G. Study of photodegradation kinetics of melatonin by multivariate curve resolution (MCR) with estimation of feasible band boundaries. Drug Test. Anal. 2013, 5, 96–102. [Google Scholar] [CrossRef] [PubMed]
- Mas, S.; de Juan, A.; Lacorte, S.; Tauler, R. Photodegradation study of decabromodiphenyl ether by UV spectrophotometry and a hybrid hard- and soft-modelling approach. Anal. Chim. Acta 2008, 618, 18–28. [Google Scholar] [CrossRef] [PubMed]
- Marín-García, M.; Ioele, G.; Franquet-Griell, H.; Lacorte, S.; Ragno, G.; Tauler, R. Investigation of the photodegradation profile of tamoxifen using spectroscopic and chromatographic analysis and multivariate curve resolution. Chemom. Intell. Lab. Syst. 2018, 174, 128–141. [Google Scholar] [CrossRef]
- Ioele, G.; De Luca, M.; Tavano, L.; Ragno, G. The difficulties for a photolabile drug in topical formulations: The case of diclofenac. Int. J. Pharm. 2014, 465, 284–290. [Google Scholar] [CrossRef] [PubMed]
- Higuchi, T.; Connors, K. Phase solubility techniques. Adv. Anal. Chem. Instrum. 1965, 4, 127–212. [Google Scholar]







| Sample | Container | k (×10−3) | t0.1 (min) | t0.5 (min) | R2 |
|---|---|---|---|---|---|
| M3 free | quartz | 0.351 | 2.84 | 28.49 | 0.992 |
| blue PET | 0.132 | 7.58 | 75.76 | 0.999 | |
| amber PET | 0.008 | 125.00 | - | 0.999 | |
| covered amber PET | - | - | - | - | |
| M3-T20 | quartz | 0.198 | 5.05 | 50.51 | 0.969 |
| blue PET | 0.125 | 8.00 | 80.00 | 0.999 | |
| amber PET | 0.007 | 142.86 | - | 0.996 | |
| covered amber PET | - | - | - | - | |
| NIM free | quartz | 0.481 | 2.07 | 20.79 | 0.999 |
| blue PET | 0.291 | 3.44 | 34.36 | 0.996 | |
| amber PET | 0.184 | 5.44 | 54.35 | 0.999 | |
| covered amber PET | 0.066 | - | - | 0.989 | |
| NIM-T20 | quartz | 0.397 | 2.52 | 25.19 | 0.992 |
| blue PET | 0.241 | 4.15 | 41.49 | 0.991 | |
| amber PET | 0.181 | 5.52 | 55.25 | 0.991 | |
| covered amber PET | 0.006 | - | - | - |
| Samples | % Entrapment Efficiency | k (×10−3) | t0.1 (min) | R2 |
|---|---|---|---|---|
| M3 free | - | 0.351 | 2.84 | 0.992 |
| M3-mβCD | 15.9 | 0.184 | 5.43 | 0.992 |
| M3-hpβCD | 29.7 | 0.120 | 8.33 | 0.988 |
| M3-βCD | 18.3 | 0.167 | 5.98 | 0.985 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ioele, G.; Gündüz, M.G.; Spatari, C.; De Luca, M.; Grande, F.; Ragno, G. A New Generation of Dihydropyridine Calcium Channel Blockers: Photostabilization of Liquid Formulations Using Nonionic Surfactants. Pharmaceutics 2019, 11, 28. https://doi.org/10.3390/pharmaceutics11010028
Ioele G, Gündüz MG, Spatari C, De Luca M, Grande F, Ragno G. A New Generation of Dihydropyridine Calcium Channel Blockers: Photostabilization of Liquid Formulations Using Nonionic Surfactants. Pharmaceutics. 2019; 11(1):28. https://doi.org/10.3390/pharmaceutics11010028
Chicago/Turabian StyleIoele, Giuseppina, Miyase Gözde Gündüz, Claudia Spatari, Michele De Luca, Fedora Grande, and Gaetano Ragno. 2019. "A New Generation of Dihydropyridine Calcium Channel Blockers: Photostabilization of Liquid Formulations Using Nonionic Surfactants" Pharmaceutics 11, no. 1: 28. https://doi.org/10.3390/pharmaceutics11010028
APA StyleIoele, G., Gündüz, M. G., Spatari, C., De Luca, M., Grande, F., & Ragno, G. (2019). A New Generation of Dihydropyridine Calcium Channel Blockers: Photostabilization of Liquid Formulations Using Nonionic Surfactants. Pharmaceutics, 11(1), 28. https://doi.org/10.3390/pharmaceutics11010028