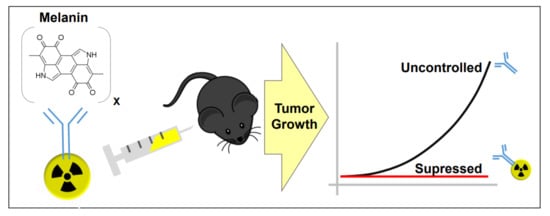
Comparative Radioimmunotherapy of Experimental Melanoma with Novel Humanized Antibody to Melanin Labeled with 213Bismuth and 177Lutetium
Abstract
:1. Introduction
2. Materials and Methods
3. Results
3.1. Humanized 8C3 mAb Specifically Localized in the Tumors, but not in Healthy Melanized Tissues
3.2. microSPECT/CT Imaging and Detailed Biodistribution Revealed Prolonged Retention of 111In-h8C3 in B16-F10 in the Tumors
3.3. Mouse and Human Dosimetry Calculations Point at Differences Between 177Lu-h8C3 and 213Bi-h8C3 in Doses Delivered to the Tumor and Normal Organs
3.4. 213Bi-h8C3 was More Effective and Safer than 177Lu-h8C3 in Slowing Down B16-F10 Tumor Growth
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- American Cancer Society. Skin Cancer—Melanoma. Available online: http://www.cancer.org/cancer/skincancer-melanoma/detailedguide/melanoma-skin-cancer-key-statistics (accessed on 22 June 2019).
- Ribas, A.; Flaherty, K.T. Gauging the Long-Term Benefits of Ipilimumab in Melanoma. J. Clin. Oncol. 2015, 33, 1865–1866. [Google Scholar] [CrossRef] [PubMed]
- Schadendorf, D.; Hodi, F.S.; Robert, C.; Weber, J.S.; Margolin, K.; Hamid, O.; Patt, D.; Chen, T.T.; Berman, D.M.; Wolchok, J.D. Pooled analysis of long-term survival data from phase II and phase III trials of ipilimumab in unresectable or metastatic melanoma. J. Clin. Oncol. 2015, 33, 1889–1894. [Google Scholar] [CrossRef] [PubMed]
- Hernandez-Davies, J.E.; Tran, T.Q.; Reid, M.A.; Rosales, K.R.; Lowman, X.H.; Pan, M.; Moriceau, G.; Yang, Y.; Wu, J.; Lo, R.S.; et al. Vemurafenib resistance reprograms melanoma cells towards glutamine dependence. J. Transl. Med. 2015, 13, 210–221. [Google Scholar] [CrossRef] [PubMed]
- Hodi, F.S.; O’Day, S.J.; McDermott, D.F.; Weber, R.W.; Sosman, J.A.; Haanen, J.B.; Gonzalez, R.; Robert, C.; Schadendorf, D.; Hassel, J.C.; et al. Improved survival with ipilimumab in patients with metastatic melanoma. N. Engl. J. Med. 2010, 363, 711–723. [Google Scholar] [CrossRef] [PubMed]
- Robert, C.; Thomas, L.; Bondarenko, I.; O’Day, S.; Weber, J.; Garbe, C.; Lebbe, C.; Baurain, J.F.; Testori, A.; Grob, J.J.; et al. Ipilimumab plus dacarbazine for previously untreated metastatic melanoma. N. Engl. J. Med. 2011, 364, 2517–2526. [Google Scholar] [CrossRef] [PubMed]
- Robert, C.; Schachter, J.; Long, G.V.; Arance, A.; Grob, J.J.; Mortier, L.; Daud, A.; Carlino, M.S.; McNeil, C.; Lotem, M.; et al. Pembrolizumab versus Ipilimumab in Advanced Melanoma. N. Engl. J. Med. 2015, 372, 2521–2532. [Google Scholar] [CrossRef] [PubMed]
- Philips, G.K.; Atkins, M. Therapeutic uses of anti-PD-1 and anti-PD-L1 antibodies. Int. Immunol. 2015, 27, 39–46. [Google Scholar] [CrossRef] [PubMed]
- Fellner, C. Ipilimumab (Yervoy) Prolongs Survival in Advanced Melanoma: Serious Side Effects and a Hefty Price Tag May Limit Its Use. Pharm. Ther. 2012, 27, 503–511. [Google Scholar]
- Weber, J.S.; Kohler, K.C.; Hauschild, A. Management of immune-related adverse events and kinetics of response with ipilimumab. J. Clin. Oncol. 2012, 30, 2691–2697. [Google Scholar] [CrossRef] [PubMed]
- Norain, A.; Dadachova, E. Review of Targeted Radionuclide Therapy of Melanoma. Semin. Nucl. Med. 2016, 46, 250–259. [Google Scholar] [CrossRef]
- Nosanchuk, J.D.; Jeyakumar, A.; Ray, A.; Revskaya, E.; Jiang, Z.; Bryan, R.A.; Allen, K.J.H.; Jiao, R.; Malo, M.E.; Gómez, B.L.; et al. Structure-function analysis and therapeutic efficacy of antibodies to fungal melanin for melanoma radioimmunotherapy. Sci. Rep. 2018, 8, 5466. [Google Scholar] [CrossRef] [PubMed]
- Melanin Antibodies and Uses Thereof. U.S. Patent 62,558,230, 22 July 2008.
- Miller, W.H.; Hartmann-Siantar, C.; Fisher, D.R.; Descalle, M.-A.; Daly, T.; Lehmann, J.; Lewis, M.R.; Hoffman, T.; Smith, J.; Situ, P.D.; et al. Evaluation of Beta Absorbed Fractions in a Mouse Model for 90Y, 188Re, 166Ho, 149Pm, 64Cu, and 177Lu Radionuclides. Cancer Biother. Radiopharm. 2005, 20, 436–449. [Google Scholar] [CrossRef] [PubMed]
- Eckerman, K.F.; Endo, A. MIRD Radionuclide Data and Decay Schemes, 2nd ed.; Society of Nuclear Medicine: Reston, VA, USA, 2008. [Google Scholar]
- Kirschner, A.S.; Ice, R.D.; Beierwaltes, W.H. Radiation-dosimetry of 131I-19-iodocholesterol: The pitfalls of using tissue concentration data—Reply. J. Nucl. Med. 1975, 16, 248–249. [Google Scholar]
- Sgouros, G.; Ballangrud, A.M.; Jurcic, J.G.; McDevitt, M.R.; Humm, J.L.; Erdi, Y.E.; Mehta, B.M.; Finn, R.D.; Larson, S.M.; Scheinberg, D.A. Pharmacokinetics and dosimetry of an alpha-particle emitter labeled antibody: 213Bi-HuM195 (anti-CD33) in patients with leukemia. J. Nucl. Med. 1999, 40, 1935–1946. [Google Scholar] [PubMed]
- Jurcic, J.G.; Larson, S.M.; Sgouros, G.; McDevitt, M.R.; Finn, R.D.; Divgi, C.R.; Ballangrud, A.M.; Hamacher, K.A.; Ma, D.; Humm, J.L.; et al. Targeted α-particle immunotherapy for myeloid leukemia. Blood 2002, 100, 1233–1239. [Google Scholar] [CrossRef] [PubMed]
- Allen, K.J.H.; Jiao, R.; Malo, M.E.; Dadachova, E. Evaluation of N-Succinimidyl S-Acetylthioacetate Ligand for Radiolabeling of Humanized Antibodies with 188Rhenium. Cancer Biother. Radiophar. 2018, 33, 349–355. [Google Scholar] [CrossRef]
- Kelly, M.P.; Lee, S.T.; Lee, F.T.; Smyth, F.E.; Davis, I.D.; Brechbiel, M.W.; Scott, A.M. Therapeutic efficacy of 177Lu-CHX-A″-DTPA-hu3S193 radioimmunotherapy in prostate cancer is enhanced by EGFR inhibition or docetaxel chemotherapy. Prostate 2009, 69, 92–104. [Google Scholar] [CrossRef]
- Kameswaran, M.; Pandey, U.; Dhakan, C.; Pathak, K.; Gota, V.; Vimalnath, K.V.; Dash, A.; Samuel, G. Synthesis and Preclinical Evaluation of 177Lu-CHX-A″-DTPA-Rituximab as a Radioimmunotherapeutic Agent for Non-Hodgkin’s Lymphoma. Cancer Biother. Radiopharm. 2015, 30, 240–246. [Google Scholar] [CrossRef]
- Dadachova, E.; Nosanchuk, J.D.; Shi, L.; Schweitzer, A.D.; Frenkel, A.; Nosanchuk, J.S.; Casadevall, A. Dead cells in melanoma tumors provide abundant antigen for targeted delivery of ionizing radiation by a monoclonal antibody to melanin. Proc. Natl. Acad. Sci. USA 2004, 101, 14865–14870. [Google Scholar] [CrossRef]
- Klein, M.; Lotem, M.; Peretz, T.; Zwas, S.T.; Mizrachi, S.; Liberman, Y.; Chisin, R.; Schachter, J.; Ron, I.G.; Iosilevsky, G.; et al. Safety and efficacy of 188-Rhenium-labeled antibody to melanin in patients with metastatic melanoma. J. Ski. Cancer 2013, 2013, 83–89. [Google Scholar] [CrossRef]
- Urán, M.E.; Nosanchuk, J.D.; Restrepo, A.; Hamilton, A.J.; Gómez, B.L.; Cano, L.E. Detection of antibodies against Paracoccidioides brasiliensis melanin in in vitro and in vivo studies during infection. Clin. Vaccine Immunol. 2011, 18, 1680–1688. [Google Scholar] [CrossRef] [PubMed]
- Larson, S.M.; Carrasquillo, J.A.; Cheung, N.V.; Press, O.W. Radioimmunotherapy of human tumours. Nature 2015, 15, 347–360. [Google Scholar] [CrossRef] [PubMed]
- Kraeber-Bodéré, F.; Bodet-Milin, C.; Rousseau, C.; Eugène, T.; Pallardy, A.; Frampas, E.; Carlier, T.; Ferrer, L.; Gaschet, J.; Davodeau, F.; et al. Radioimmunoconjugates for the treatment of cancer. Semin. Oncol. 2014, 41, 613–622. [Google Scholar] [CrossRef] [PubMed]
- Baidoo, K.E.; Yong, K.; Brechbiel, M.W. Molecular pathways: Targeted α-particle radiation therapy. Clin. Cancer Res. 2013, 19, 530–537. [Google Scholar] [CrossRef] [PubMed]
- Boll, R.A.; Kratochwil, C.; Giesel, F.L.; Mier, W.; Haberkorn, U.; Bruchertseifer, F.; Apostolidis, C.; Morgenstern, A. 213Bi-DOTATOC receptor-targeted alpha-radionuclide therapy induces remission in neuroendocrine tumours refractory to beta radiation: A first-in-human experience. Eur. J. Nucl. Med. Mol. Imaging 2014, 41, 2106–2119. [Google Scholar]
- Deshayes, E.; Ladjohounlou, R.; Le Fur, P.; Pichard, A.; Lozza, C.; Boudousq, V.; Sevestre, S.; Jarlier, M.; Kashani, R.; Koch, J.; et al. Radiolabeled Antibodies Against Müllerian-Inhibiting Substance Receptor, Type II: New Tools for a Theranostic Approach in Ovarian Cancer. J. Nucl. Med. 2018, 59, 1234–1242. [Google Scholar] [CrossRef] [PubMed]
- Jiao, R.; Allen, K.J.H.; Malo, M.E.; Helal, M.; Jiang, Z.; Smart, K.; Buhl, S.V.; Rickles, D.; Bryan, R.A.; Dadachova, E. Evaluation of novel highly specific antibodies to cancer testis antigen Centrin-1 for radioimmunoimaging and radioimmunotherapy of pancreatic cancer. Cancer Med. 2019. in print. [Google Scholar] [CrossRef] [PubMed]




| Target Organ | Bismuth-213 | Lutetium-177 | ||
|---|---|---|---|---|
| Absorbed Dose (cGy/37 kBq admin.) | Energy Absorbed Fraction | Absorbed Dose (cGy/37 kBq admin.) | Energy Absorbed Fraction | |
| Blood | 8.590 | 1.0 | 6.440 | 0.95 |
| Pancreas | 0.099 | 1.0 | 0.177 | 0.85 |
| Stomach | 0.389 | 1.0 | 0.346 | 0.96 |
| Small Intestine | 0.548 | 1.0 | 0.301 | 0.90 |
| Large intestine | 0.116 | 1.0 | 0.386 | 0.90 |
| Liver | 1.800 | 1.0 | 1.330 | 0.88 |
| Spleen | 1.409 | 1.0 | 1.707 | 0.87 |
| Kidney | 1.732 | 1.0 | 1.550 | 0.93 |
| Lungs | 2.010 | 1.0 | 1.079 | 0.89 |
| Heart | 2.453 | 1.0 | 1.822 | 0.93 |
| Tumor | 0.805 | 1.0 | 3.429 | 0.89 |
| Muscle | 0.158 | 1.0 | 0.298 | 0.99 |
| Bone | 0.502 | 1.0 | 0.679 | 0.50 |
| Brain | 0.113 | 1.0 | 0.159 | 0.95 |
| Eyes | 0.108 | 1.0 | 0.146 | 0.60 |
| Tail | 1.014 | 1.0 | 0.917 | 0.97 |
| Target Organ | Total 213Bi Dose | Total 177Lu Dose |
|---|---|---|
| Adrenals | 8.70 × 10−2 | 2.48 × 10−1 |
| Brain | 3.15 × 10−3 | 2.29 × 10−2 |
| Breasts | 8.65 × 10−2 | 2.38 × 10−1 |
| Gallbladder Wall | 8.72 × 10−2 | 2.50 × 10−1 |
| Lower Large Intestine Wall | 8.74 × 10−2 | 2.53 × 10−1 |
| Small Intestine | 8.76 × 10−2 | 2.56 × 10−1 |
| Stomach Wall | 8.72 × 10−2 | 2.48 × 10−1 |
| Upper Large Intestine Wall | 8.75 × 10−2 | 2.54 × 10−1 |
| Heart Wall | 6.74 × 10−3 | 3.65 × 10−2 |
| Kidneys | 2.36 × 10−2 | 9.00 × 10−2 |
| Liver | 5.68 × 10−2 | 1.69 × 10−1 |
| Lungs | 7.26 × 10−3 | 3.02 × 10−2 |
| Muscle | 3.94 × 10−3 | 3.51 × 10−2 |
| Ovaries | 8.75 × 10−2 | 2.54 × 10−1 |
| Pancreas | 1.76 × 10−3 | 2.59 × 10−2 |
| Red Marrow | 1.15 × 10−1 | 1.88 × 10−1 |
| Osteogenic Cells | 8.30 × 10−1 | 7.56 × 10−1 |
| Skin | 8.62 × 10−2 | 2.34 × 10−1 |
| Spleen | 2.91 × 10−3 | 2.68 × 10−2 |
| Testes | 8.68 × 10−2 | 2.42 × 10−1 |
| Thymus | 8.68 × 10−2 | 2.44 × 10−1 |
| Thyroid | 8.68 × 10−2 | 2.44 × 10−1 |
| Urinary Bladder Wall | 8.73 × 10−2 | 2.50 × 10−1 |
| Uterus | 8.75 × 10−2 | 2.55 × 10−1 |
| Total Body | 8.93 × 10−2 | 2.53 × 10−1 |
| Tumor | 2.98 × 10−1 | 3.36 × 10−1 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Allen, K.J.H.; Jiao, R.; Malo, M.E.; Frank, C.; Fisher, D.R.; Rickles, D.; Dadachova, E. Comparative Radioimmunotherapy of Experimental Melanoma with Novel Humanized Antibody to Melanin Labeled with 213Bismuth and 177Lutetium. Pharmaceutics 2019, 11, 348. https://doi.org/10.3390/pharmaceutics11070348
Allen KJH, Jiao R, Malo ME, Frank C, Fisher DR, Rickles D, Dadachova E. Comparative Radioimmunotherapy of Experimental Melanoma with Novel Humanized Antibody to Melanin Labeled with 213Bismuth and 177Lutetium. Pharmaceutics. 2019; 11(7):348. https://doi.org/10.3390/pharmaceutics11070348
Chicago/Turabian StyleAllen, Kevin J. H., Rubin Jiao, Mackenzie E. Malo, Connor Frank, Darrell R. Fisher, David Rickles, and Ekaterina Dadachova. 2019. "Comparative Radioimmunotherapy of Experimental Melanoma with Novel Humanized Antibody to Melanin Labeled with 213Bismuth and 177Lutetium" Pharmaceutics 11, no. 7: 348. https://doi.org/10.3390/pharmaceutics11070348
APA StyleAllen, K. J. H., Jiao, R., Malo, M. E., Frank, C., Fisher, D. R., Rickles, D., & Dadachova, E. (2019). Comparative Radioimmunotherapy of Experimental Melanoma with Novel Humanized Antibody to Melanin Labeled with 213Bismuth and 177Lutetium. Pharmaceutics, 11(7), 348. https://doi.org/10.3390/pharmaceutics11070348