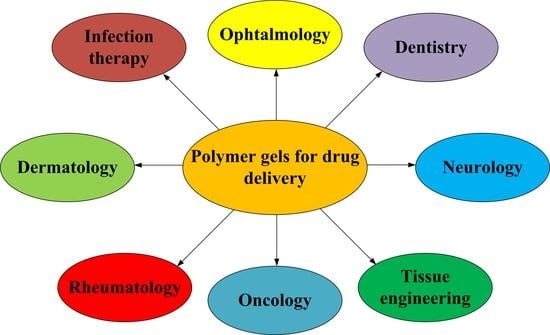
Polymeric Gel Systems Cytotoxicity and Drug Release as Key Features for their Effective Application in Various Fields of Addressed Pharmaceuticals Delivery
Abstract
:1. Introduction
2. Gels for the Treatment of Diseases of the Intestines and Skin
3. Gels in Ophthalmology
4. Gels in Cancer Treatment
5. Gels in Dentistry
6. Gels in Tissue Engineering
7. Gels for the Treatment of Joint Diseases
8. Gels for the Treatment of Neurodegenerative Diseases
9. Gels for the Delivery of Antimicrobial and Antipyretic Drugs
10. Synthetic and Natural Polymers for Gels Drug Delivery Systems
11. Crosslinkers for Gels Preparation
12. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Loukelis, K.; Helal, Z.A.; Mikos, A.G.; Chatzinikolaidou, M. Nanocomposite Bioprinting for Tissue Engineering Applications. Gels 2023, 9, 103. [Google Scholar] [CrossRef] [PubMed]
- Preda, P.; Enciu, A.M.; Adiaconita, B.; Mihalache, I.; Craciun, G.; Boldeiu, A.; Aricov, L.; Romanitan, C.; Stan, D.; Marculescu, C.; et al. New Amorphous Hydrogels with Proliferative Properties as Potential Tools in Wound Healing. Gels 2022, 8, 604. [Google Scholar] [CrossRef] [PubMed]
- Ding, Y.W.; Zhang, X.W.; Mi, C.H.; Qi, X.Y.; Zhou, J.; Wei, D.X. Recent advances in hyaluronic acid-based hydrogels for 3D bioprinting in tissue engineering applications. Smart Mater. Med. 2022, 4, 59–68. [Google Scholar] [CrossRef]
- Ran, C.; Wang, J.; He, Y.; Ren, Q.; Hu, H.; Zhu, J.; Gu, X.; Li, M.; Zheng, L.; Li, J. Recent Advances in Bioinspired Hydrogels with Environment-Responsive Characteristics for Biomedical Applications. Macromol. Biosci. 2022, 22, 2100474. [Google Scholar] [CrossRef]
- Luo, C.; Guo, A.; Li, J.; Tang, Z.; Luo, F. Janus hydrogel to mimic the structure and property of articular cartilage. ACS Appl. Mater. Interfaces 2022, 14, 35434–35443. [Google Scholar] [CrossRef]
- Abdel-Mageed, H.M.; Abd El Aziz, A.E.; Abdel Raouf, B.M.; Mohamed, S.A.; Nada, D. Antioxidant-biocompatible and stable catalase-based gelatin–alginate hydrogel scaffold with thermal wound healing capability: Immobilization and delivery approach. 3 Biotech 2022, 12, 1–12. [Google Scholar] [CrossRef]
- Xu, X.; Shen, S.; Mo, R. Bioresponsive nanogels for protein delivery. View 2022, 3, 20200136. [Google Scholar] [CrossRef]
- Nazir, F.; Tabish, T.A.; Tariq, F.; Iftikhar, S.; Wasim, R.; Shahnaz, G. Stimuli-sensitive drug delivery systems for site-specific antibiotic release. Drug Discov. Today 2022, 27, 1698–1705. [Google Scholar] [CrossRef]
- Alamoudi, A.A.; Alharbi, A.S.; Abdel-Naim, A.B.; Badr-Eldin, S.M.; Awan, Z.A.; Okbazghi, S.Z.; Ahmed, O.A.A.; Alhakamy, N.A.; Fahmy, U.A.; Esmat, A. Novel Nanoconjugate of Apamin and Ceftriaxone for Management of Diabetic Wounds. Life 2022, 12, 1096. [Google Scholar] [CrossRef]
- Ijaz, U.; Sohail, M.; Usman Minhas, M.; Khan, S.; Hussain, Z.; Kazi, M.; Shah, S.A.; Mahmood, A.; Maniruzzaman, M. Biofunctional Hyaluronic Acid/κ-Carrageenan Injectable Hydrogels for Improved Drug Delivery and Wound Healing. Polymers 2022, 14, 376. [Google Scholar] [CrossRef]
- Yuan, H.; Li, W.; Song, C.; Huang, R. An injectable supramolecular nanofiber-reinforced chitosan hydrogel with antibacterial and anti-inflammatory properties as potential carriers for drug delivery. Int. J. Biol. Macromol. 2022, 205, 563–573. [Google Scholar] [CrossRef]
- Du, Y.N.; Wei, Q.; Zhao, L.J.; Fan, C.Q.; Guo, L.R.; Ye, J.F.; Li, Y. Hydrogel-based co-delivery of CIK cells and oncolytic adenovirus armed with IL12 and IL15 for cancer immunotherapy. Biomed. Pharmacother. 2022, 151, 113110. [Google Scholar] [CrossRef]
- Hosny, N.M.; Abbass, M.; Ismail, F.; El-Din, H.M.N. Radiation synthesis and anticancer drug delivery of poly (acrylic acid/acrylamide) magnetite hydrogel. Polym. Bull. 2022, 1–16. [Google Scholar] [CrossRef]
- Zong, S.; Wen, H.; Lv, H.; Li, T.; Tang, R.; Liu, L.; Jiang, J.; Wang, S.; Duan, J. Intelligent hydrogel with both redox and thermo-response based on cellulose nanofiber for controlled drug delivery. Carbohydr. Polym. 2022, 278, 118943. [Google Scholar] [CrossRef]
- Li, L.; Lei, D.; Zhang, J.; Xu, L.; Li, J.; Jin, L.; Pan, L. Dual-Responsive Alginate Hydrogel Constructed by Sulfhdryl Dendrimer as an Intelligent System for Drug Delivery. Molecules 2022, 27, 281. [Google Scholar] [CrossRef]
- Liu, Y.; Ran, Y.; Ge, Y.; Raza, F.; Li, S.; Zafar, H.; Wu, Y.; Paiva-Santos, A.C.; Yu, C.; Sun, M.; et al. pH-Sensitive Peptide Hydrogels as a Combination Drug Delivery System for Cancer Treatment. Pharmaceutics 2022, 14, 652. [Google Scholar] [CrossRef]
- Kim, Y.; Hu, Y.; Jeong, J.P.; Jung, S. Injectable, self-healable and adhesive hydrogels using oxidized Succinoglycan/chitosan for pH-responsive drug delivery. Carbohydr. Polym. 2022, 284, 119195. [Google Scholar] [CrossRef]
- Nagaraja, K.; Rao, K.M.; Rao, K.K.; Han, S.S. Dual responsive tamarind gum-co-poly (N-isopropyl acrylamide-co-ethylene glycol vinyl ether) hydrogel: A promising device for colon specific anti-cancer drug delivery. Colloids Surf. A Physicochem. Eng. Asp. 2022, 641, 128456. [Google Scholar] [CrossRef]
- Wang, F.; Huang, K.; Xu, Z.; Shi, F.; Chen, C. Self-healable nanocellulose composite hydrogels combining multiple dynamic bonds for drug delivery. Int. J. Biol. Macromol. 2022, 203, 143–152. [Google Scholar] [CrossRef]
- Zhang, Q.; Yang, X.; Wu, Y.; Liu, C.; Xia, H.; Cheng, X.; Cheng, Y.; Xia, Y.; Wang, Y. In vitro evaluation of kaempferol-loaded hydrogel as pH-sensitive drug delivery systems. Polymers 2022, 14, 3205. [Google Scholar] [CrossRef]
- Gharehnazifam, Z.; Dolatabadi, R.; Baniassadi, M.; Shahsavari, H.; Kajbafzadeh, A.M.; Abrinia, K.; Gharehnazifam, K.; Baghani, M. Multiphysics modeling and experiments on ultrasound-triggered drug delivery from silk fibroin hydrogel for Wilms tumor. Int. J. Pharm. 2022, 621, 121787. [Google Scholar] [CrossRef] [PubMed]
- Ersen Dudu, T.; Alpaslan, D.; Aktas, N. Application of poly (Agar-co-glycerol-co-sweet almond oil) based organo-hydrogels as a drug delivery material. J. Polym. Environ. 2022, 30, 483–493. [Google Scholar] [CrossRef] [PubMed]
- Aslam, M.; Barkat, K.; Malik, N.S.; Alqahtani, M.S.; Anjum, I.; Khalid, I.; Tulain, U.R.; Gohar, N.; Zafar, H.; Paiva-Santos, A.C.; et al. pH Sensitive Pluronic Acid/Agarose-Hydrogels as Controlled Drug Delivery Carriers: Design, Characterization and Toxicity Evaluation. Pharmaceutics 2022, 14, 1218. [Google Scholar] [CrossRef] [PubMed]
- Wanjale, M.V.; Sunil Jaikumar, V.; Sivakumar, K.C.; Ann Paul, R.; James, J.; Kumar, G.V. Supramolecular hydrogel based post-surgical implant system for hydrophobic drug delivery against glioma recurrence. Int. J. Nanomed. 2022, 182, 2203–2224. [Google Scholar] [CrossRef]
- El-Zaafarany, G.M.; Nasr, M. Insightful exploring of advanced nanocarriers for the topical/transdermal treatment of skin diseases. Pharm. Dev. Technol. 2021, 26, 1136–1157. [Google Scholar] [CrossRef]
- Ojha, B.; Jain, V.K.; Gupta, S.; Talegaonkar, S.; Jain, K. Nanoemulgel: A promising novel formulation for treatment of skin ailments. Polym. Bull. 2022, 79, 4441–4465. [Google Scholar] [CrossRef]
- Ferrara, F.; Benedusi, M.; Cervellati, F.; Sguizzato, M.; Montesi, L.; Bondi, A.; Drechsler, M.; Pula, W.; Valacchi, G.; Esposito, E. Dimethyl Fumarate-Loaded Transethosomes: A Formulative Study and Preliminary Ex Vivo and In Vivo Evaluation. Int. J. Mol. Sci. 2022, 23, 8756. [Google Scholar] [CrossRef]
- Deng, W.; Yan, Y.; Zhuang, P.; Liu, X.; Tian, K.; Huang, W.; Li, C. Synthesis of nanocapsules blended polymeric hydrogel loaded with bupivacaine drug delivery system for local anesthetics and pain management. Drug Deliv. 2022, 29, 399–412. [Google Scholar] [CrossRef]
- Liu, Y.; Li, C.; Feng, Z.; Han, B.; Yu, D.-G.; Wang, K. Advances in the Preparation of Nanofiber Dressings by Electrospinning for Promoting Diabetic Wound Healing. Biomolecules 2022, 12, 1727. [Google Scholar] [CrossRef]
- Ceylan, S.; Küçükosman, R.; Yurt, F.; Özel, D.; Öztürk, İ.; Demir, D.; Ocakoglu, K. Antimicrobial activity enhancement of PVA/chitosan films with the additive of CZTS quantum dots. Polym. Bull. 2022, 1–21. [Google Scholar] [CrossRef]
- Kass, L.E.; Nguyen, J. Nanocarrier-hydrogel composite delivery systems for precision drug release. Wiley Interdiscip. Rev. Nanomed. Nanobiotechnol. 2022, 14, e1756. [Google Scholar] [CrossRef]
- Mazidi, Z.; Javanmardi, S.; Naghib, S.M.; Mohammadpour, Z. Smart stimuli-responsive implantable drug delivery systems for programmed and on-demand cancer treatment: An overview on the emerging materials. Chem. Eng. J. 2022, 433, 134569. [Google Scholar] [CrossRef]
- Khan, M.I.; Hossain, M.I.; Hossain, M.K.; Rubel, M.H.K.; Hossain, K.M.; Mahfuz, A.M.U.B.; Anik, M.I. Recent Progress in Nanostructured Smart Drug Delivery Systems for Cancer Therapy: A Review. ACS Appl. Bio Mater. 2022, 5, 971–1012. [Google Scholar] [CrossRef]
- Cascone, S.; Lamberti, G. Hydrogel-based commercial products for biomedical applications: A review. Int. J. Pharm. 2019, 573, 118803. [Google Scholar] [CrossRef]
- Ghasemiyeh, P.; Mohammadi-Samani, S. Hydrogels as drug delivery systems; pros and cons. Trends Pharmaceut. Sci. 2019, 5, 7–24. [Google Scholar]
- Minhas, M.U.; Khan, K.U.; Sarfraz, M.; Badshah, S.F.; Munir, A.; Barkat, K.; Basit, A.; Arafat, M. Polyvinylpyrrolidone K-30-Based Crosslinked Fast Swelling Nanogels: An Impeccable Approach for Drug’s Solubility Improvement. BioMed Res. Int. 2022, 2022, 5883239. [Google Scholar] [CrossRef]
- Amirova, A.; Rodchenko, S.; Kurlykin, M.; Tenkovtsev, A.; Krasnou, I.; Krumme, A.; Filippov, A. Synthesis and investigation of thermo-induced gelation of partially cross-linked poly-2-isopropyl-2-oxazoline in aqueous media. Polymers 2020, 12, 698. [Google Scholar] [CrossRef] [Green Version]
- Mahand, S.N.; Aliakbarzadeh, S.; Moghaddam, A.; Moghaddam, A.S.; Kruppke, B.; Nasrollahzadeh, M.; Khonakdar, H.A. Polyoxazoline: A review article from polymerization to smart behaviors and biomedical applications. Eur. Polym. J. 2022, 178, 111484. [Google Scholar] [CrossRef]
- Altinbasak, I.; Kocak, S.; Sanyal, R.; Sanyal, A. Fast-Forming Dissolvable Redox-Responsive Hydrogels: Exploiting the Orthogonality of Thiol-Maleimide and Thiol-Disulfide Exchange Chemistry. Biomacromolecules 2022, 23, 3525–3534. [Google Scholar] [CrossRef]
- Bahú, J.O.; de Andrade, L.R.M.; de Melo Barbosa, R.; Crivellin, S.; da Silva, A.P.; Souza, S.D.; Cardenas Concha, V.O.; Severino, P.; Souto, E.B. Plant polysaccharides in engineered pharmaceutical gels. Bioengineering 2022, 9, 376. [Google Scholar] [CrossRef]
- Tan, R.Y.H.; Lee, C.S.; Pichika, M.R.; Cheng, S.F.; Lam, K.Y. PH Responsive Polyurethane for the Advancement of Biomedical and Drug Delivery. Polymers 2022, 14, 1672. [Google Scholar] [CrossRef] [PubMed]
- Ansari, M.J.; Rajendran, R.R.; Mohanto, S.; Agarwal, U.; Panda, K.; Dhotre, K.; Manne, R.; Deepak, A.; Zafar, A.; Yasir, M.; et al. Poly (N-isopropylacrylamide)-based hydrogels for biomedical applications: A review of the state-of-the-art. Gels 2022, 8, 454. [Google Scholar] [CrossRef] [PubMed]
- Dalei, G.; Das, S. Polyacrylic acid-based drug delivery systems: A comprehensive review on the state-of-art. J. Drug Deliv. Sci. Technol. 2022, 78, 103988. [Google Scholar] [CrossRef]
- Baykara, D.; Pilavci, E.; Cesur, S.; Ilhan, E.; Ulag, S.; Sengor, M.; Kijeriska-Gawroriska, E.; Gunduz, O. Controlled Release of Gentamicin from Electrospun Poly (Vinyl Alcohol)/Gelatin Nanofibers: The Effect of Crosslinking Time Using Glutaraldehyde Vapor. ChemistrySelect 2023, 8. [Google Scholar] [CrossRef]
- Mozalewska, W.; Czechowska-Biskup, R.; Olejnik, A.K.; Wach, R.A.; Ulański, P.; Rosiak, J.M. Chitosan-containing hydrogel wound dressings prepared by radiation technique. Radiat. Phys. Chem. 2017, 134, 1–7. [Google Scholar] [CrossRef]
- Relleve, L.S.; Gallardo, A.K.R.; Tecson, M.G.; Luna, J.A. Biocompatible hydrogels of carboxymethyl hyaluronic acid prepared by radiation-induced crosslinking. Radiat. Phys. Chem. 2021, 179, 109194. [Google Scholar] [CrossRef]
- Demeter, M.; Meltzer, V.; Calina, J.; Scarisoreanu, A.; Micutz, M.; Kaya, M.G.A. Highly elastic superabsorbent collagen/PVP/PAA/PEO hydrogels crosslinked via e-beam radiation. Radiat. Phys. Chem. 2020, 174, 108898. [Google Scholar] [CrossRef]
- Qamruzzaman, M.; Ahmed, F.; Mondal, M.; Ibrahim, H. An overview on starch-based sustainable hydrogels: Potential applications and aspects. J. Polym. Environ. 2022, 30, 19–50. [Google Scholar] [CrossRef]
- Swilem, A.E.; Oyama, T.G.; Oyama, K.; Kimura, A.; Taguchi, M. Development of carboxymethyl cellulose/gelatin hybrid hydrogels via radiation-induced cross-linking as novel anti-adhesion barriers. Polym. Degrad. Stab. 2022, 197, 109856. [Google Scholar] [CrossRef]
- Mushtaq, F.; Raza, Z.A.; Batool, S.R.; Zahid, M.; Onder, O.C.; Rafique, A.; Nazeer, M.A. Preparation, properties, and applications of gelatin-based hydrogels (GHs) in the environmental, technological, and biomedical sectors. Int. J. Biol. Macromol. 2022, 218, 601–633. [Google Scholar] [CrossRef]
- Zeng, D.; Shen, S.; Fan, D. Molecular design, synthesis strategies and recent advances of hydrogels for wound dressing applications. Chin. J. Chem. Eng. 2021, 30, 308–320. [Google Scholar] [CrossRef]
- Stawicki, B.; Schacher, T.; Cho, H. Nanogels as a versatile drug delivery system for brain cancer. Gels 2021, 7, 63. [Google Scholar] [CrossRef]
- Baranov, N.; Popa, M.; Atanase, L.I.; Ichim, D.L. Polysaccharide-based drug delivery systems for the treatment of periodontitis. Molecules 2021, 26, 2735. [Google Scholar] [CrossRef]
- Okur, N.U.; Bulbul, E.O.; Yagcilar, A.P.; Siafaka, P.I. Current status of mucoadhesive gel systems for buccal drug delivery. Curr. Pharm. Des. 2021, 27, 2015–2025. [Google Scholar] [CrossRef]
- Agrawal, M.; Saraf, S.; Dubey, S.K.; Puri, A.; Gupta, U.; Alexander, A. Stimuli-responsive in situ gelling system for nose-to-brain drug delivery. J. Control. Release 2020, 327, 235–265. [Google Scholar] [CrossRef]
- Wang, H.; Deng, H.; Gao, M.; Zhang, W. Self-assembled nanogels based on ionic gelation of natural polysaccharides for drug delivery. Front. Bioeng. Biotechnol. 2021, 9, 703559. [Google Scholar] [CrossRef]
- Raina, N.; Pahwa, R.; Bhattacharya, J.; Paul, A.K.; Nissapatorn, V.; de Lourdes Pereira, M.; Oliveira, S.M.R.; Dolma, K.G.; Rahmatullah, M.; Wilairatana, P.; et al. Drug Delivery Strategies and Biomedical Significance of Hydrogels: Translational Considerations. Pharmaceutics 2022, 14, 574. [Google Scholar] [CrossRef]
- Song, F.; Gong, J.; Tao, Y.; Cheng, Y.; Lu, J.; Wang, H. A robust regenerated cellulose-based dual stimuli-responsive hydrogel as an intelligent switch for controlled drug delivery. Int. J. Biol. Macromol. 2021, 176, 448–458. [Google Scholar] [CrossRef]
- Zhang, S.; Kang, L.; Hu, S.; Hu, J.; Fu, Y.; Hu, Y.; Yang, X. Carboxymethyl chitosan microspheres loaded hyaluronic acid/gelatin hydrogels for controlled drug delivery and the treatment of inflammatory bowel disease. Int. J. Biol. Macromol. 2021, 167, 1598–1612. [Google Scholar] [CrossRef]
- Coentro, J.Q.; Di Nubila, A.; May, U.; Prince, S.; Zwaagstra, J.; Jarvinen, T.A.; Zeugolis, D.I. Dual drug delivery collagen vehicles for modulation of skin fibrosis in vitro. Biomed. Mater. 2022, 17, 025017. [Google Scholar] [CrossRef]
- Chatterjee, S.; Hui, P.C.L.; Siu, W.S.; Kan, C.W.; Leung, P.C.; Wanxue, C.; Chiou, J.C. Influence of pH-responsive compounds synthesized from chitosan and hyaluronic acid on dual-responsive (pH/temperature) hydrogel drug delivery systems of Cortex Moutan. Int. J. Biol. Macromol. 2021, 168, 163–174. [Google Scholar] [CrossRef] [PubMed]
- Sivasankarapillai, V.S.; Das, S.S.; Sabir, F.; Sundaramahalingam, M.A.; Colmenares, J.C.; Prasannakumar, S.; Rajan, M.; Rahdar, A.; Kyzas, G.Z. Progress in natural polymer engineered biomaterials for transdermal drug delivery systems. Mater. Today Chem. 2021, 19, 100382. [Google Scholar] [CrossRef]
- De Oliveira, M.J.A.; Villegas, G.M.E.; Motta, F.D.; Fabela-Sánchez, O.; Espinosa-Roa, A.; Fotoran, W.L.; Peixoto, J.C.; Tano, F.T.; Lugao, A.B.; Vásquez, P.A.S. Influence of gamma radiation on Amphotericin B incorporated in PVP hydrogel as an alternative treatment for cutaneous leishmaniosis. Acta Trop. 2021, 215, 105805. [Google Scholar] [CrossRef] [PubMed]
- Zare, M.R.; Khorram, M.; Barzegar, S.; Sarkari, B.; Asgari, Q.; Ahadian, S.; Zomorodian, K. Dissolvable carboxymethyl cellulose/polyvinylpyrrolidone microneedle arrays for transdermal delivery of Amphotericin B to treat cutaneous leishmaniasis. Int. J. Biol. Macromol. 2021, 182, 1310–1321. [Google Scholar] [CrossRef] [PubMed]
- Pradhan, M.; Yadav, K.; Singh, D.; Singh, M.R. Topical delivery of fluocinolone acetonide integrated NLCs and salicylic acid enriched gel: A potential and synergistic approach in the management of psoriasis. J. Drug. Deliv. Sci. Technol. 2021, 61, 102282. [Google Scholar] [CrossRef]
- Das, S.; Saha, D.; Majumdar, S.; Giri, L. Imaging Methods for the Assessment of a Complex Hydrogel as an Ocular Drug Delivery System for Glaucoma Treatment: Opportunities and Challenges in Preclinical Evaluation. Mol. Pharm. 2022, 19, 733–748. [Google Scholar] [CrossRef]
- Wen, Y.; Jia, H.; Mo, Z.; Zheng, K.; Chen, S.; Ding, Y.; Chen, Y. Cross-linked thermosensitive nanohydrogels for ocular drug delivery with a prolonged residence time and enhanced bioavailability. Mater. Sci. Eng. 2021, 119, 111445. [Google Scholar] [CrossRef]
- Ortiz, J.A.; Sepúlveda, F.A.; Panadero-Medianero, C.; Murgas, P.; Ahumada, M.; Palza, H.; Matsuhiro, B.; Zapata, P.A. Cytocompatible drug delivery hydrogels based on carboxymethylagarose/chitosan pH-responsive polyelectrolyte complexes. Int. J. Biol. Macromol. 2022, 199, 96–107. [Google Scholar] [CrossRef]
- Wang, L.; Pan, H.; Gu, D.; Sun, H.; Chen, K.; Tan, G.; Pan, W. A Novel Carbon Dots/Thermo-Sensitive in Situ Gel for a Composite Ocular Drug Delivery System: Characterization, Ex-Vivo Imaging, and In Vivo Evaluation. Int. J. Mol. Sci. 2021, 22, 9934. [Google Scholar] [CrossRef]
- Shukr, M.H.; Ismail, S.; El-Hossary, G.G.; El-Shazly, A.H. Design and evaluation of mucoadhesive in situ liposomal gel for sustained ocular delivery of travoprost using two steps factorial design. J. Drug. Deliv. Sci. Technol. 2021, 61, 102333. [Google Scholar] [CrossRef]
- Maxwell, C.J.; Soltisz, A.M.; Rich, W.W.; Choi, A.; Reilly, M.A.; Swindle-Reilly, K.E. Tunable alginate hydrogels as injectable drug delivery vehicles for optic neuropathy. J. Biomed. Mater. Res. A 2022, 110, 1621–1635. [Google Scholar] [CrossRef]
- Luo, L.J.; Nguyen, D.D.; Huang, C.C.; Lai, J.Y. Therapeutic hydrogel sheets programmed with multistage drug delivery for effective treatment of corneal abrasion. Chem. Eng. J. 2022, 429, 132409. [Google Scholar] [CrossRef]
- Choi, H.; Kwon, M.; Choi, H.E.; Hahn, S.K.; Kim, K.S. Non-Invasive Topical Drug-Delivery System Using Hyaluronate Nanogels Crosslinked via Click Chemistry. Materials 2021, 14, 1504. [Google Scholar] [CrossRef]
- Hermida-Merino, C.; Cabaleiro, D.; Lugo, L.; Valcarcel, J.; Vázquez, J.A.; Bravo, I.; Longo, A.; Salloum-Abour-Jaoude, G.; Solano, E.; Gracia-Fernandez, C.; et al. Characterization of Tuna Gelatin-Based Hydrogels as a Matrix for Drug Delivery. Gels 2022, 8, 237. [Google Scholar] [CrossRef]
- Fardous, J.; Omoso, Y.; Joshi, A.; Yoshida, K.; Patwary, M.K.; Ono, F.; Ijima, H. Development and characterization of gel-in-water nanoemulsion as a novel drug delivery system. Mater. Sci. Eng. C 2021, 124, 112076. [Google Scholar] [CrossRef]
- Moya-Lopez, C.; Juan, A.; Donizeti, M.; Valcarcel, J.; Vazquez, J.A.; Solano, E.; Hermida-Merino, D. Multifunctional PLA/Gelatin Bionanocomposites for Tailored Drug Delivery Systems. Pharmaceutics 2022, 14, 1138. [Google Scholar] [CrossRef]
- Yao, S.; Jin, X.; Wang, C.; Cao, A.; Hu, J.; Chen, B.; Wang, B. ICG/5-Fu coencapsulated temperature stimulus response nanogel drug delivery platform for chemo-photothermal/photodynamic synergetic therapy. J. Biomater. Appl. 2021, 36, 565–578. [Google Scholar] [CrossRef]
- Abd El-Sattar, N.E.; El-Hddad, S.E.S.; Ghobashy, M.M.; Zaher, A.A.; El-Adl, K. Nanogel-mediated drug delivery system for anticancer agent: pH stimuli responsive poly(ethylene glycol/acrylic acid) nanogel prepared by gamma irradiation. Bioorg. Chem. 2022, 127, 105972. [Google Scholar] [CrossRef]
- Liwinska, W.; Waleka-Bagiel, E.; Stojek, Z.; Karbarz, M.; Zabost, E. Enzyme-triggered-and tumor-targeted delivery with tunable, methacrylated poly (ethylene glycols) and hyaluronic acid hybrid nanogels. Drug Deliv. 2022, 29, 2561–2578. [Google Scholar] [CrossRef]
- Surikutchi, B.T.; Obenza-Otero, R.; Russo, E.; Zelzer, M.; Cancela, I.G.; Costoya, J.A.; Marlow, M. Development of a nanocapsule-loaded hydrogel for drug delivery for intraperitoneal administration. Int. J. Pharm. 2022, 622, 121828. [Google Scholar] [CrossRef]
- Chen, Z.; Song, S.; Ma, J.; Da Ling, S.; Wang, Y.D.; Kong, T.T.; Xu, J.H. Fabrication of magnetic core/shell hydrogels via microfluidics for controlled drug delivery. Chem. Eng. Sci. 2022, 248, 117216. [Google Scholar] [CrossRef]
- Derakhshankhah, H.; Haghshenas, B.; Eskandani, M.; Jahanban-Esfahlan, R.; Abbasi-Maleki, S.; Jaymand, M. Folate-conjugated thermal-and pH-responsive magnetic hydrogel as a drug delivery nano-system for “smart” chemo/hyperthermia therapy of solid tumors. Mater. Today Commun. 2022, 30, 103148. [Google Scholar] [CrossRef]
- Huang, T.H.; Hsu, S.H.; Chang, S.W. Molecular interaction mechanisms of glycol chitosan self-healing hydrogel as a drug delivery system for gemcitabine and doxorubicin. Comput. Struct. Biotechnol. J. 2022, 20, 700–709. [Google Scholar] [CrossRef] [PubMed]
- Ho, H.N.; Le, H.H.; Le, T.G.; Duong, T.H.A.; Ngo, V.Q.T.; Dang, C.T.; Nguyen, C.N. Formulation and characterization of hydroxyethyl cellulose-based gel containing metronidazole-loaded solid lipid nanoparticles for buccal mucosal drug delivery. Int. J. Biol. Macromol. 2022, 194, 1010–1018. [Google Scholar] [CrossRef]
- Soni, A.; Raj, S.; Kashyap, L.; Upadhyay, A.; Agrahari, V.C.; Sharma, A. Comparative effect of 1.2% atorvastatin gel and 1.2% rosuvastatin as a local drug delivery in treatment of intra-bony defects in chronic periodontitis. Indian J. Dent. Res. 2022, 33, 180. [Google Scholar] [CrossRef]
- Ding, Y.; Wang, Y.; Li, J.; Tang, M.; Chen, H.; Wang, G.; Gui, S. Microemulsion-thermosensitive gel composites as in situ-forming drug reservoir for periodontitis tissue repair through alveolar bone and collagen regeneration strategy. Pharm. Dev. Technol. 2023, 28, 1–13, 30–39. [Google Scholar] [CrossRef]
- Zhang, Y.; Dou, X.; Zhang, L.; Wang, H.; Zhang, T.; Bai, R.; Deng, X. Facile fabrication of a biocompatible composite gel with sustained release of aspirin for bone regeneration. Bioact. Mater. 2022, 11, 130–139. [Google Scholar] [CrossRef]
- Al-Baadani, M.A.; Yie, K.H.R.; Al-Bishari, A.M.; Alshobi, B.A.; Zhou, Z.; Fang, K.; Dai, B.; Shen, Y.; Ma, J.; Liu, J.; et al. Co-electrospinning polycaprolactone/gelatin membrane as a tunable drug delivery system for bone tissue regeneration. Mater. Des. 2021, 209, 109962. [Google Scholar] [CrossRef]
- Siefen, T.; Bjerregaard, S.; Plaksin, D.; Lokhnauth, J.; Liang, A.; Larsen, C.C.; Lamprecht, A. Co-formulations of adalimumab with hyaluronic acid/polyvinylpyrrolidone to combine intraarticular drug delivery and viscosupplementation. Eur. J. Pharm. Biopharm. 2022, 177, 39–49. [Google Scholar] [CrossRef]
- Park, S.Y.; Kang, J.H.; Kim, H.S.; Hwang, J.Y.; Shin, U.S. Electrical and thermal stimulus-responsive nanocarbon-based 3D hydrogel sponge for switchable drug delivery. Nanoscale 2022, 14, 2367–2382. [Google Scholar] [CrossRef]
- Hoang, H.T.; Vu, T.T.; Karthika, V.; Jo, S.H.; Jo, Y.J.; Seo, J.W.; Lim, K.T. Dual cross-linked chitosan/alginate hydrogels prepared by Nb-Tz ‘click’reaction for pH responsive drug delivery. Carbohydr. Polym. 2022, 288, 119389. [Google Scholar] [CrossRef]
- Manivong, S.; Garcia Ac, A.; Patten, S.A.; Fernandes, J.C.; Benderdour, M.; Banquy, X.; Moldovan, F.; Roullin, V.G. Chitosan-Based Nanogels: Synthesis and Toxicity Profile for Drug Delivery to Articular Joints. Nanomaterials 2022, 12, 1337. [Google Scholar] [CrossRef]
- Mi, B.; Chen, L.; Xiong, Y.; Yang, Y.; Panayi, A.C.; Xue, H.; Hu, Y.; Yan, C.; Hu, L.; Xie, X.; et al. Osteoblast/Osteoclast and Immune Cocktail Therapy of an Exosome/Drug Delivery Multifunctional Hydrogel Accelerates Fracture Repair. ACS Nano 2022, 16, 771–782. [Google Scholar] [CrossRef]
- Ji, X.; Shao, H.; Li, X.; Ullah, M.W.; Luo, G.; Xu, Z.; Zhang, Y. Injectable immunomodulation-based porous chitosan microspheres/HPCH hydrogel composites as a controlled drug delivery system for osteochondral regeneration. Biomaterials 2022, 285, 121530. [Google Scholar] [CrossRef]
- Motasadizadeh, H.; Tavakoli, M.; Damoogh, S.; Mottaghitalab, F.; Gholami, M.; Atyabi, F.; Farokhi, M.; Dinarvand, R. Dual drug delivery system of teicoplanin and phenamil based on pH-sensitive silk fibroin/sodium alginate hydrogel scaffold for treating chronic bone infection. Biomater. Adv. 2022, 139, 213032. [Google Scholar] [CrossRef]
- Rahmani, Z.; Ghaemy, M.; Olad, A. Preparation of nanogels based on kappa-carrageenan/chitosan and N-doped carbon dots: Study of drug delivery behavior. Polym. Bull. 2021, 78, 2709–2726. [Google Scholar] [CrossRef]
- Rahmani, S.; Olad, A.; Rahmani, Z. Preparation of self-healable nanocomposite hydrogel based on Gum Arabic/gelatin and graphene oxide: Study of drug delivery behavior. Polym. Bull. 2022, 1–22. [Google Scholar] [CrossRef]
- Baldelli, A.; Boraey, M.A.; Oguzlu, H.; Cidem, A.; Rodriguez, A.P.; Ong, H.X.; Jiang, F.; Bacca, M.; Thamboo, A.; Traini, D.; et al. Engineered nasal dry powder for the encapsulation of bioactive compounds. Drug Discov. Today. 2022, 27, 2300–2308. [Google Scholar] [CrossRef]
- Vigani, B.; Rossi, S.; Sandri, G.; Bonferoni, M.C.; Caramella, C.M.; Ferrari, F. Recent advances in the development of in situ gelling drug delivery systems for non-parenteral administration routes. Pharmaceutics 2020, 12, 859. [Google Scholar] [CrossRef]
- Lin, H.; Xie, L.; Lv, L.; Chen, J.; Feng, F.; Liu, W.; Han, L.; Liu, F. Intranasally administered thermosensitive gel for brain-targeted delivery of rhynchophylline to treat Parkinson’s disease. Colloids Surf. B 2023, 222, 113065. [Google Scholar] [CrossRef]
- Wang, J.T.W.; Rodrigo, A.C.; Patterson, A.K.; Hawkins, K.; Aly, M.M.; Sun, J.; Al Jamal, K.T.; Smith, D.K. Enhanced Delivery of Neuroactive Drugs via Nasal Delivery with a Self-Healing Supramolecular Gel. Adv. Sci. 2021, 8, 2101058. [Google Scholar] [CrossRef] [PubMed]
- Xu, X.; Sun, J.; Bing, L.; Cui, X.; Jia, B.; Bai, S. Fractal features of dual temperature/pH-sensitive poly (N-isopropylacrylamide-co-acrylic acid) hydrogels and resultant effects on the controlled drug delivery performances. Eur. Polym. J. 2022, 171, 111203. [Google Scholar] [CrossRef]
- Markovic, M.D.; Panic, V.V.; Savic, S.I.; Ugrinovic, V.D.; Pjanovic, R.V.; Spasojevic, M.M.; Spasojevic, P.M. Biobased thermo/pH sensitive poly (N-isopropylacrylamide-co-crotonic acid) hydrogels for targeted drug delivery. Microporous Mesoporous Mater. 2022, 335, 111817. [Google Scholar] [CrossRef]
- Andrade del Olmo, J.; Pérez-Álvarez, L.; Sáez Martínez, V.; Benito Cid, S.; Pérez González, R.; Vilas-Vilela, J.L.; Alonso, J.M. Drug Delivery from Hyaluronic Acid–BDDE Injectable Hydrogels for Antibacterial and Anti-Inflammatory Applications. Gels 2022, 8, 223. [Google Scholar] [CrossRef] [PubMed]
- Teodorescu, M.; Morariu, S. Drug delivery system based on PVA and clay for potential treatment of COVID-19. J. Polym. Res. 2022, 29, 1–13. [Google Scholar] [CrossRef]
- Jung, H. Hyaluronidase: An overview of its properties, applications, and side effects. Arch. Plast. Surg. 2020, 47, 297–300. [Google Scholar] [CrossRef]
- Kurakula, M.; Rao, G.K. Pharmaceutical assessment of polyvinylpyrrolidone (PVP): As excipient from conventional to controlled delivery systems with a spotlight on COVID-19 inhibition. J. Drug Deliv. Sci. Technol. 2020, 60, 102046. [Google Scholar] [CrossRef]
- Bludau, H.; Czapar, A.E.; Pitek, A.S.; Shukla, S.; Jordan, R.; Steinmetz, N.F. POxylation as an alternative stealth coating for biomedical applications. Eur. Polym. J. 2017, 88, 679–688. [Google Scholar] [CrossRef] [Green Version]
- Kim, J.O.; Sahay, G.; Kabanov, A.V.; Bronich, T.K. Polymeric micelles with ionic cores containing biodegradable cross-links for delivery of chemotherapeutic agents. Biomacromolecules 2010, 11, 919–926. [Google Scholar] [CrossRef] [Green Version]
- Yu, Y.; Xu, S.; Li, S.; Pan, H. Genipin-cross-linked hydrogels based on biomaterials for drug delivery: A review. Biomater. Sci. 2021, 9, 1583–1597. [Google Scholar] [CrossRef]
- Rehman, N.; Dilshad, M.R.; Islam, A.; Gull, N.; Riaz, T.; Khan, S.M.; Khan, R.U. Novel graphene oxide loaded sodium alginate hydrogels cross-linked with tetraethyl orthosilicate for cephradine release analysis. J. Drug Deliv. Sci. Technol. 2021, 66, 102784. [Google Scholar] [CrossRef]
- George, A.; Shrivastav, P.S. Preparation and optimization of tetraethyl orthosilicate cross-linked chitosan-guar gum-poly (vinyl alcohol) composites reinforced with montmorillonite for sustained release of sitagliptin. Int. J. Biol. Macromol. 2023, 229, 51–61. [Google Scholar] [CrossRef]
- Mashabela, L.T.; Maboa, M.M.; Miya, N.F.; Ajayi, T.O.; Chasara, R.S.; Milne, M.; Mokhele, S.; Demana, P.H.; Witika, B.A.; Siwe-Noundou, X.; et al. A Comprehensive Review of Cross-Linked Gels as Vehicles for Drug Delivery to Treat Central Nervous System Disorders. Gels 2022, 8, 563. [Google Scholar] [CrossRef]





| Cytokine | Concentration (Control), pg mL−1 | Concentration (Curcumin/Gel), pg mL−1 |
|---|---|---|
| IL-6 | 17.0070 ± 0.5005 | 10.3452 ± 1.6804 |
| TNF-α | 31.0771 ± 6.5353 | 11.9864 ± 5.3004 |
| Concentration, µg mL−1 | Relative Cell Viability, % |
|---|---|
| 0 (control) | 100 |
| 10 | 50 ± 5 |
| 30 | 47 ± 5 |
| 50 | 43 ± 5 |
| 80 | 41 ± 5 |
| 100 | 40 ± 5 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Smagina, V.; Yudaev, P.; Kuskov, A.; Chistyakov, E. Polymeric Gel Systems Cytotoxicity and Drug Release as Key Features for their Effective Application in Various Fields of Addressed Pharmaceuticals Delivery. Pharmaceutics 2023, 15, 830. https://doi.org/10.3390/pharmaceutics15030830
Smagina V, Yudaev P, Kuskov A, Chistyakov E. Polymeric Gel Systems Cytotoxicity and Drug Release as Key Features for their Effective Application in Various Fields of Addressed Pharmaceuticals Delivery. Pharmaceutics. 2023; 15(3):830. https://doi.org/10.3390/pharmaceutics15030830
Chicago/Turabian StyleSmagina, Veronika, Pavel Yudaev, Andrey Kuskov, and Evgeniy Chistyakov. 2023. "Polymeric Gel Systems Cytotoxicity and Drug Release as Key Features for their Effective Application in Various Fields of Addressed Pharmaceuticals Delivery" Pharmaceutics 15, no. 3: 830. https://doi.org/10.3390/pharmaceutics15030830
APA StyleSmagina, V., Yudaev, P., Kuskov, A., & Chistyakov, E. (2023). Polymeric Gel Systems Cytotoxicity and Drug Release as Key Features for their Effective Application in Various Fields of Addressed Pharmaceuticals Delivery. Pharmaceutics, 15(3), 830. https://doi.org/10.3390/pharmaceutics15030830