Food Environment around Schools: A Systematic Scope Review
Abstract
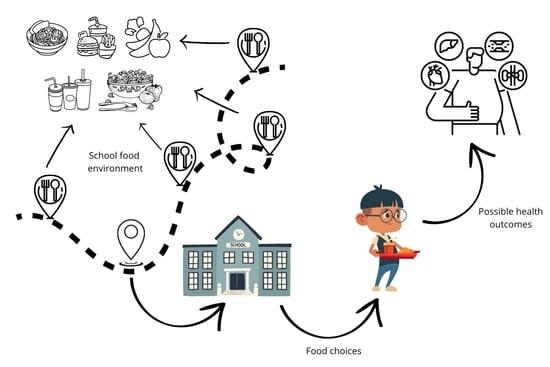
:1. Introduction
2. Materials and Methods
2.1. Search Strategy
2.2. Eligibility Criteria
2.3. Studies Selection and Data Collection
3. Results and Discussion
3.1. Characteristics of the Schools Studied
3.2. Availability and Proximity of Food around Schools
3.3. Food-School Environment Exposure and Associated Dietary-Nutritional-Health Implications
4. Strengths, Limitations, and Closing Remarks
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Machado Azeredo, C.; Fornias, L.; De Rezende, M.; Canella, D.S.; Claro, R.M.; Rugani, I.; De Castro, R.; Do, O.; Luiz, C.; Levy, R.B. Dietary Intake of Brazilian Adolescents. Public Health Nutr. 2014, 18, 1215–1224. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tang, X.; Ohri-Vachaspati, P.; Abbott, J.K.; Aggarwal, R.; Tulloch, D.L.; Lloyd, K.; Yedidia, M.J. Associations between Food Environment around Schools and Professionally Measured Weight Status for Middle and High School Students. Child. Obes. 2014, 10, 511–517. [Google Scholar] [CrossRef] [Green Version]
- Leite, M.A.; Azeredo, C.M.; Peres, M.F.T.; Escuder, M.M.L.; Levy, R.B. Disponibilidade e Consumo de Ultraprocessados Em Escolas Do Município de São Paulo, Brasil: Resultados Do SP-Proso. Cad. Saude Publica 2021, 37, e00162920. [Google Scholar] [CrossRef] [PubMed]
- von Philipsborn, P.; Stratil, J.M.; Burns, J.; Busert, L.K.; Pfadenhauer, L.M.; Polus, S.; Holzapfel, C.; Hauner, H.; Rehfuess, E. Environmental Interventions to Reduce the Consumption of Sugar-Sweetened Beverages and Their Effects on Health. Cochrane Database Syst. Rev. 2019, 6, CD012292. [Google Scholar] [CrossRef] [PubMed]
- Rocha, L.L.; Pessoa, M.C.; Gratão, L.H.A.; do Carmo, A.S.; Cordeiro, N.G.; de Freitas Cunha, C.; de Oliveira, T.R.P.R.; Mendes, L.L. Characteristics of the School Food Environment Affect the Consumption of Sugar-Sweetened Beverages Among Adolescents. Front. Nutr. 2021, 8, 742744. [Google Scholar] [CrossRef]
- Rocha, L.L.; Gratão, L.H.A.; do Carmo, A.S.; Costa, A.B.P.; de Freitas Cunha, C.; de Oliveira, T.R.P.R.; Mendes, L.L. School Type, Eating Habits, and Screen Time Are Associated With Ultra-Processed Food Consumption Among Brazilian Adolescents. J. Acad. Nutr. Diet. 2021, 121, 1136–1142. [Google Scholar] [CrossRef]
- Marien Da Costa Peres, C.; Soares Gardone, D.; Vieira De Lima Costa, B.; Kü Mmel Duarte, C.; Pessoa, C.; Mendes, L.L. Retail Food Environment around Schools and Overweight: A Systematic Review. Nutr. Rev. 2020, 78, 841–856. [Google Scholar] [CrossRef]
- He, M.; Tucker, P.; Gilliland, J.; Irwin, J.D.; Larsen, K.; Hess, P. The Influence of Local Food Environments on Adolescents’ Food Purchasing Behaviors. Int. J. Environ. Res. Public Health 2012, 9, 1458–1471. [Google Scholar] [CrossRef] [Green Version]
- Mackenbach, J.D.; Nelissen, K.G.; Dijkstra, S.C.; Poelman, M.P.; Daams, J.G.; Leijssen, J.B.; Nicolaou, M. A Systematic Review on Socioeconomic Differences. Nutrients 2019, 11, 2215. [Google Scholar] [CrossRef] [Green Version]
- Carmo, A.S.D.; Assis, M.M.D.; Cunha, C.D.F.; Oliveira, T.R.P.R.D.; Mendes, L.L. The Food Environment of Brazilian Public and Private Schools. Cad. Saude Publica 2018, 34, e00014918. [Google Scholar] [CrossRef]
- Day, P.L.; Pearce, J. Obesity-Promoting Food Environments and the Spatial Clustering of Food Outlets Around Schools. Am. J. Prev. Med. 2011, 40, 113–121. [Google Scholar] [CrossRef] [PubMed]
- Fitzpatrick, C.; Datta, G.; Henderson, M.; Gray-Donald, K.; Kestens, Y.; Barnett, T. School Food Environments Associated with Adiposity in Canadian Children. Int. J. Obes. 2017, 41, 1005–1010. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Saavedra-Garcia, L.; Meza-Hernández, M.; Yabiku-Soto, K.; Hernández-Vásquez, A.; Kesar, H.V.; Mejia-Victorio, C.; Diez-Canseco, F. Oferta y Publicidad de Alimentos y Bebidas En Instituciones Educativas y Entornos Escolares de Lima Metropolitana. Un Estudio Exploratorio. Rev. Peru. Med. Exp. Salud Publica 2021, 37, 726–732. [Google Scholar] [CrossRef] [PubMed]
- Buck, C.; Börnhorst, C.; Pohlabeln, H.; Huybrechts, I.; Pala, V.; Reisch, L.; Pigeot, I. Clustering of Unhealthy Food around German Schools and Its Influence on Dietary Behavior in School Children: A Pilot Study. Int. J. Behav. Nutr. Phys. Act. 2013, 10, 65. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lorenzo, P.M.; Izquierdo, A.G.; Rodriguez-Carnero, G.; Fernández-Pombo, A.; Iglesias, A.; Carreira, M.C.; Tejera, C.; Bellido, D.; Martinez-Olmos, M.A.; Leis, R.; et al. Epigenetic Effects of Healthy Foods and Lifestyle Habits from the Southern European Atlantic Diet Pattern: A Narrative Review. Adv. Nutr. 2022, 13, 1725–1747. [Google Scholar] [CrossRef] [PubMed]
- Landecker, H. Food as Exposure: Nutritional Epigenetics and the New Metabolism. Biosocieties 2011, 6, 167–194. [Google Scholar] [CrossRef] [Green Version]
- Borges, C.A.; Jaime, P.C. Development and Evaluation of Food Environment Audit Instrument: AUDITNOVA. Rev. Saude Publica 2019, 53, 91. [Google Scholar] [CrossRef] [Green Version]
- Martins, P.; Cremm, E.; Leite, F.; Maron, L.; Scagliusi, F.; Oliveira, M. Validation of an Adapted Version of the Nutrition Environment Measurement Tool for Stores (NEMS-S) in an Urban Area of Brazil. J. Nutr. Educ. Behav. 2013, 45, 785–792. [Google Scholar] [CrossRef]
- Honório, O.S.; Horta, P.M.; Pessoa, M.C.; Jardim, M.Z.; do Carmo, A.S.; Mendes, L.L. Food Deserts and Food Swamps in a Brazilian Metropolis: Comparison of Methods to Evaluate the Community Food Environment in Belo Horizonte. Food Secur. 2021, 14, 695–707. [Google Scholar] [CrossRef]
- Hager, E.R.; Cockerham, A.; O’Reilly, N.; Harrington, D.; Harding, J.; Hurley, K.M.; Black, M.M. Food Swamps and Food Deserts in Baltimore City, MD, USA: Associations with Dietary Behaviours among Urban Adolescent Girls. Public Health Nutr. 2017, 20, 2598–2607. [Google Scholar] [CrossRef]
- Charreire, H.; Casey, R.; Salze, P.; Simon, C.; Chaix, B.; Banos, A.; Badariotti, D.; Weber, C.; Oppert, J.M. Measuring the Food Environment Using Geographical Information Systems: A Methodological Review. Public Health Nutr. 2010, 13, 1773–1785. [Google Scholar] [CrossRef] [PubMed]
- Matsuzaki, M.; Sanchez, B.; Acosta, M.; Botkin, J.; Sanchez-Vaznaugh, E. Food Environment near Schools and Body Weight-A Systematic Review of Associations by Race/Ethnicity, Gender, Grade, and Socio-Economic Factors. Obes. Rev. 2020, 21, e12997. [Google Scholar] [CrossRef] [PubMed]
- Addis, S.; Murphy, S. “There Is Such a Thing as Too Healthy!” The Impact of Minimum Nutritional Guidelines on School Food Practices in Secondary Schools. J. Hum. Nutr. Diet 2019, 32, 31–40. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Smith, D.; Cummins, S.; Clark, C.; Stansfeld, S. Does the Local Food Environment around Schools Affect Diet? Longitudinal Associations in Adolescents Attending Secondary Schools in East London. BMC Public Health 2013, 13, 70. [Google Scholar] [CrossRef] [Green Version]
- Moraeus, L.; Lindroos, A.K.; Warensjö Lemming, E.; Mattisson, I. Diet Diversity Score and Healthy Eating Index in Relation to Diet Quality and Socio-Demographic Factors: Results from a Cross-Sectional National Dietary Survey of Swedish Adolescents. Public Health Nutr. 2020, 23, 1754–1765. [Google Scholar] [CrossRef] [Green Version]
- Davis, B.; Carpenter, C. Proximity of Fast-Food Restaurants to Schools and Adolescent Obesity. Am. J. Public Health 2009, 99, 505–510. [Google Scholar] [CrossRef]
- Nasreddine, L.; Naja, F.; Akl, C.; Chamieh, M.C.; Karam, S.; Sibai, A.M.; Hwalla, N. Dietary, Lifestyle and Socio-Economic Correlates of Overweight, Obesity and Central Adiposity in Lebanese Children and Adolescents. Nutrients 2014, 6, 1038–1062. [Google Scholar] [CrossRef]
- Brown, H.; Kirkman, S.; Albani, V.; Goffe, L.; Akhter, N.; Hollingsworth, B.; von Hinke, S.; Lake, A.; D’Souza, E.; Vandevijvere, S.; et al. Home and Neighbourhood Built Environment Features in Family-Based Treatment for Childhood Obesity. Obes. Rev. 2022, 32, 112323. [Google Scholar] [CrossRef]
- Peters, M.D.J.; Godfrey, C.M.; Khalil, H.; McInerney, P.; Parker, D.; Soares, C.B. Guidance for Conducting Systematic Scoping Reviews. Int. J. Evid. Based. Healthc. 2015, 13, 141–146. [Google Scholar] [CrossRef] [Green Version]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
- Institute, J.B. Critical Appraisal Tools for Use in JBI Systematic Reviews Checklist for Prevalence Studies. Adel. SA Joanna Briggs Inst. 2016. Available online: https://jbi.global/sites/default/files/2019-05/JBI_Critical_Appraisal-Checklist_for_Prevalence_Studies2017_0.pdf (accessed on 2 November 2022).
- Austin, S.B.; Melly, S.J.; Sanchez, B.N.; Patel, A.; Buka, S.; Gortmaker, S.L. Clustering of Fast-Food Restaurants around Schools: A Novel Application of Spatial Statistics to the Study of Food Environments. Am. J. Public Health 2005, 95, 1575–1581. [Google Scholar] [CrossRef] [PubMed]
- Frank, L.; Glanz, K.; Mccarron, M.; Sallis, J.; Saelens, B.; Chapman, J. The Spatial Distribution of Food Outlet Type and Quality around Schools in Differing Built Environment and Demographic Contexts. Berkeley Plan. J. 2006, 19, 79–95. [Google Scholar] [CrossRef]
- Kipke, M.D.; Iverson, E.; Moore, D.; Booker, C.; Ruelas, V.; Peters, A.L.; Kaufman, F. Food and Park Environments: Neighborhood-Level Risks for Childhood Obesity in East Los Angeles. J. Adolesc. Health 2007, 40, 325–333. [Google Scholar] [CrossRef] [PubMed]
- Simon, P.A.; Kwan, D.; Angelescu, A.; Shih, M.; Fielding, J.E. Proximity of Fast Food Restaurants to Schools: Do Neighborhood Income and Type of School Matter? Prev. Med. 2008, 47, 284–288. [Google Scholar] [CrossRef]
- Sturm, R. Disparities in the Food Environment Surrounding US Middle and High Schools. Public Health 2008, 122, 681–690. [Google Scholar] [CrossRef] [Green Version]
- Zenk, S.N.; Powell, L.M. US Secondary Schools and Food Outlets. Health Place 2008, 14, 336–346. [Google Scholar] [CrossRef]
- Kestens, Y.; Daniel, M. Social Inequalities in Food Exposure Around Schools in an Urban Area. Am. J. Prev. Med. 2010, 39, 33–40. [Google Scholar] [CrossRef]
- Kwate, N.O.A.; Loh, J.M. Separate and Unequal: The Influence of Neighborhood and School Characteristics on Spatial Proximity between Fast Food and Schools. Prev. Med. 2010, 51, 153–156. [Google Scholar] [CrossRef]
- Laska, M.N.; Hearst, M.O.; Forsyth, A.; Pasch, K.E.; Lytle, L. Neighbourhood Food Environments: Are They Associated with Adolescent Dietary Intake, Food Purchases and Weight Status? Public Health Nutr. 2010, 13, 1757–1763. [Google Scholar] [CrossRef] [Green Version]
- Neckerman, K.M.; Bader, M.D.M.; Richards, C.A.; Purciel, M.; Quinn, J.W.; Thomas, J.S.; Warbelow, C.; Weiss, C.C.; Lovasi, G.S.; Rundle, A. Disparities in the Food Environments of New York City Public Schools. Am. J. Prev. Med. 2010, 39, 195–202. [Google Scholar] [CrossRef]
- Robitaille, E.; Bergeron, P.; Lasnier, B.; Institut national de santé publique du Québec; Gibson Library Connections. Analyse Géographique de l’accessibilité Des Restaurants-Minute et Des Dépanneurs Autour Des Écoles Publiques Québécoises: Rapport; Institut National de santé Publique du Québec: Québec City, QC, Canada, 2010. [Google Scholar]
- Tester, J.M.; Yen, I.H.; Laraia, B. Mobile Food Vending and the After-School Food Environment. Am. J. Prev. Med. 2010, 38, 70–73. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nixon, H.; Doud, L. Do Fast Food Restaurants Cluster around High Schools? A Geospatial Analysis of Proximity of Fast Food Restaurants to High Schools and the Connection to Childhood Obesity Rates. J. Agric. Food Syst. Community Dev. 2011, 2, 181–194. [Google Scholar] [CrossRef] [Green Version]
- Gebauer, H.; Laska, M.N. Convenience Stores Surrounding Urban Schools: An Assessment of Healthy Food Availability, Advertising and Product Placement. J. Urban Health 2011, 88, 616–622. [Google Scholar] [CrossRef] [Green Version]
- Sanchez, B.; Sanchez-Vaznaugh, E.; Uscilka, A.; Baek, J.; Zhang, L. Differential Associations Between the Food Environment Near Schools and Childhood Overweight Across Race/Ethnicity, Gender, and Grade. Am. J. Epidemiol. 2012, 175, 1284–1293. [Google Scholar] [CrossRef] [PubMed]
- An, R.; Sturm, R. School and Residential Neighborhood Food Environment and Diet among California Youth. Am. J. Prev. Med. 2012, 42, 129–135. [Google Scholar] [CrossRef] [Green Version]
- Black, J.L.; Day, M. Availability of Limited Service Food Outlets Surrounding Schools InBritish Columbia. Can. J. Public Health 2012, 103, 255–259. [Google Scholar] [CrossRef]
- Ellaway, A.; Macdonald, L.; Lamb, K.; Thornton, L.; Day, P.; Pearce, J. Do Obesity-Promoting Food Environments Cluster around Socially Disadvantaged Schools in Glasgow, Scotland? Health Place 2012, 18, 1335–1340. [Google Scholar] [CrossRef] [Green Version]
- Forsyth, A.; Wall, M.; Larson, N.; Story, M.; Neumark-Sztainer, D. Do Adolescents Who Live or Go to School near Fast-Food Restaurants Eat More Frequently from Fast-Food Restaurants? Health Place 2012, 18, 1261–1269. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Heroux, M.; Iannotti, R.; Currie, D.; Pickett, W.; Janssen, I. The Food Retail Environment in School Neighborhoods and Its Relation to Lunchtime Eating Behaviors in Youth from Three Countries. Health Place 2012, 18, 1240–1247. [Google Scholar] [CrossRef] [Green Version]
- Leite, F.H.M.; De Oliveira, M.A.; Cremm, E.D.C.; De Abreu, D.S.C.; Maron, L.R.; Martins, P.A. Availability of Processed Foods in the Perimeter of Public Schools in Urban Areas. J. Pediatr. 2012, 88, 328–334. [Google Scholar] [CrossRef]
- Seliske, L.; Pickett, W.; Rosu, A.; Janssen, I. Identification of the Appropriate Boundary Size to Use When Measuring the Food Retail Environment Surrounding Schools. Int. J. Environ. Res. Public Health 2012, 9, 2715–2727. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Day, P.L.; Pearce, J.R.; Pearson, A.L. A Temporal Analysis of the Spatial Clustering of Food Outlets around Schools in Christchurch, New Zealand, 1966 to 2006. Public Health Nutr. 2013, 18, 135–142. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Grier, S.; Davis, B. Are All Proximity Effects Created Equal? Fast Food Near Schools and Body Weight Among Diverse Adolescents. J. Public Policy Mark. 2013, 32, 1547–7207. [Google Scholar] [CrossRef]
- Richmond, T.K.; Spadano-Gasbarro, J.L.; Walls, C.E.; Austin, S.B.; Greaney, M.L.; Wang, M.L.; Mezegebu, S.; Peterson, K.E. Middle School Food Environments and Racial/Ethnic Differences in Sugar-Sweetened Beverage Consumption: Findings from the Healthy Choices Study. Prev. Med. 2013, 57, 735–738. [Google Scholar] [CrossRef] [Green Version]
- Engler-Stringer, R.; Shah, T.; Bell, S.; Muhajarine, N. Geographic Access to Healthy and Unhealthy Food Sources for Children in Neighbourhoods and from Elementary Schools in a Mid-Sized Canadian City. Spat. Spatiotemporal. Epidemiol. 2014, 11, 23–32. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Laxer, R.E.; Janssen, I. The Proportion of Excessive Fast-Food Consumption Attributable to the Neighbourhood Food Environment among Youth Living within 1 Km of Their School. Appl. Physiol. Nutr. Metab. 2014, 39, 480–486. [Google Scholar] [CrossRef] [PubMed]
- Clark, E.; Quigg, R.; Wong, J.; Richards, R.; Black, K.; Skidmore, P. Is the Food Environment Surrounding Schools Associated with the Diet Quality of Adolescents in Otago, New Zealand? Health Place 2014, 30, 78–85. [Google Scholar] [CrossRef]
- Cutumisu, N.; Traoré, I.; Paquette, M.C.; Cazale, L.; Camirand, H.; Lalonde, B.; Robitaille, E. Association between Junk Food Consumption and Fast-Food Outlet Access near School among Quebec Secondary-School Children: Findings from the Quebec Health Survey of High School Students (QHSHSS) 2010–2011. Public Health Nutr. 2017, 20, 927–937. [Google Scholar] [CrossRef] [Green Version]
- Soltero, E.G.; Ortiz Hernández, L.; Jauregui, E.; Lévesque, L.; Lopez Y Taylor, J.; Barquera, S.; Lee, R.E. Characterization of the School Neighborhood Food Environment in Three Mexican Cities. Ecol. Food Nutr. 2017, 56, 139–151. [Google Scholar] [CrossRef]
- Li, Y.; Du, T.; Huff-Corzine, L.; Johnson, K.; Noyongoyo, B. Where Is the Fruit? Multidimensional Inequalities in Food Retail Environments around Public Elementary Schools. Child Care Health Dev 2019, 45, 500–508. [Google Scholar] [CrossRef]
- Lourenço, A.E.P.; Vieira, J.L.; da Rocha, C.M.M.; Lima, F.F. Influência Da Ambiência Escolar No Estado Nutricional de Pré-Escolares de Macaé, Rio de Janeiro, Brasil. Cien. Saude Colet. 2019, 24, 2399–2410. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rummo, P.; Wu, E.; McDermott, Z.; Schwartz, A.; Elbel, B. Relationship between Retail Food Outlets near Public Schools and Adolescent Obesity in New York City. Health Place 2020, 65, 102408. [Google Scholar] [CrossRef] [PubMed]
- Chew, A.; Moran, A.; Barnoya, J. Food Swamps Surrounding Schools in Three Areas of Guatemala. Prev. Chronic. Dis. 2020, 17, E75. [Google Scholar] [CrossRef] [PubMed]
- Henriques, P.; de Alvarenga, C.R.T.; Ferreira, D.M.; Dias, P.C.; da Silva Bastos Soares, D.; Barbosa, R.M.S.; Burlandy, L. Ambiente Alimentar Do Entorno de Escolas Públicas e Privadas: Oportunidade Ou Desafio Para Alimentação Saudável? Cien. Saude Colet. 2021, 26, 3135–3145. [Google Scholar] [CrossRef]
- da Costa Peres, C.M.; de Lima Costa, B.V.; Pessoa, M.C.; Honório, O.S.; do Carmo, A.S.; da Silva, T.P.R.; Gardone, D.S.; Meireles, A.L.; Mendes, L.L. O Ambiente Alimentar Comunitário e a Presença de Pântanos Alimentares No Entorno Das Escolas de Uma Metrópole Brasileira. Cad. Saude Publica 2021, 37, e00205120. [Google Scholar] [CrossRef]
- Rundle, A.; Neckerman, K.M.; Freeman, L.; Lovasi, G.S.; Purciel, M.; Quinn, J.; Richards, C.; Sircar, N.; Weiss, C. Neighborhood Food Environment and Walkability Predict Obesity in New York City. Environ. Health Perspect. 2009, 117, 442–447. [Google Scholar] [CrossRef]
- Ooi, J.; Wolfenden, L.; Yoong, S.; Janssen, L.; Reilly, K.; Nathan, N.; Sutherland, R. A Trial of a Six-Month Sugar-Sweetened Beverage Intervention in Secondary Schools from a Socio-Economically Disadvantaged Region in Australia. Aust. N. Z. J. Public Health 2021, 45, 599–607. [Google Scholar] [CrossRef]
- Bardin, S.; Gola, A.A. Analyzing the Association between Student Weight Status and School Meal Participation: Evidence from the School Nutrition and Meal Cost Study. Nutrients 2020, 13, 17. [Google Scholar] [CrossRef]
- Dantas, R.R.; da Silva, G.A.P. The Role of the Obesogenic Environment and Parental Lifestyles in Infant Feeding Behavior. Rev. Paul. Pediatr. 2019, 37, 363–371. [Google Scholar] [CrossRef]
- Leite, M.A.; De Assis, M.M.; Do Carmo, A.S.; Da Silva, T.P.R.; Nogueira, M.C.; Netto, M.P.; Levy, R.B.; Mendes, L.L. Disparities in Food Availability around Schools in a Large Brazilian City. Child. Youth Environ. 2021, 31, 146–164. [Google Scholar] [CrossRef]
- Ralston, K.; Newman, C.; Clauson, A.; Guthrie, J.; Buzby, J. The National School Lunch Program: Background, Trends, and Issues. Economic Research Report Number 61; US Department of Agriculture: Washington, DC, USA, 2008.
- Brasil. Fundo Nacional de Desenvolvimento da Educação. FNDE. Lei No 11.947, de 16 de Junho de 2009. Available online: http://www.planalto.gov.br/ccivil_03/_ato2007-2010/2009/lei/l11947.htm (accessed on 23 March 2022).
- Jin, H.; Lu, Y. Evaluating Consumer Nutrition Environment in Food Deserts and Food Swamps. J. Environ. Res. Public Health 2021, 18, 2675. [Google Scholar] [CrossRef]
- Ferdinand, K.C.; Mahata, I. Food Deserts Limited Healthy Foods in the Land of Plenty Editorial. Circ. Cardiovasc. Qual. Outcomes 2017, 10, e004131. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jiao, J. Measuring Vulnerable Population’s Healthy and Unhealthy Food Access in Austin, Texas. AIMS Public Health 2016, 3, 722. [Google Scholar] [CrossRef] [PubMed]
- Pai, S.; Bahadur, K. The Impact of Food Insecurity on Child Health. Pediatr. Clin. N. Am. 2020, 67, 387–396. [Google Scholar] [CrossRef] [PubMed]



| Authors | Year | Risk of Bias |
|---|---|---|
| Austin et al. [32] | 2005 | Moderate |
| Frank et al. [33] | 2006 | Moderate |
| Kipke et al. [34] | 2007 | Moderate |
| Simon et al. [35] | 2008 | Moderate |
| Sturm [36] | 2008 | Moderate |
| Zenk; Powell [37] | 2008 | Moderate |
| Davis; Carpenter [26] | 2009 | Low |
| Kestens; Daniel [38] | 2010 | Moderate |
| Kwate; Loh [39] | 2010 | Moderate |
| Laska et al. [40] | 2010 | Low |
| Neckerman et al. [41] | 2010 | High |
| Robitaille; Bergeron, Lasnier [42] | 2010 | High |
| Tester; Yen; Laraia [43] | 2010 | High |
| Nixon; Doud [44] | 2011 | Moderate |
| Day; Pearce [11] | 2011 | Low |
| Gebauer; Laska [45] | 2011 | Moderate |
| Sanchez et al. [46] | 2012 | High |
| An; Sturm [47] | 2012 | Moderate |
| Black; Day [48] | 2012 | Moderate |
| Ellaway et al. [49] | 2012 | Moderate |
| Forsyth et al. [50] | 2012 | Moderate |
| He et al. [8] | 2012 | Low |
| Héroux et al. [51] | 2012 | Moderate |
| Leite et al. [52] | 2012 | Moderate |
| Seliske et al. [53] | 2012 | Moderate |
| Buck et al. [14] | 2013 | Moderate |
| Day; Pearce; Pearson [54] | 2013 | Moderate |
| Grier; Davis [55] | 2013 | Moderate |
| Richmond et al. [56] | 2013 | High |
| Smith et al. [24] | 2013 | Moderate |
| Engler-Stringer et al. [57] | 2014 | Moderate |
| Laxer; Janssen [58] | 2014 | Moderate |
| Clark et al. [59] | 2014 | Moderate |
| Tang et al. [2] | 2014 | Low |
| Cutumisu et al. [60] | 2017 | Moderate |
| Fitzpatrick et al. [12] | 2017 | Moderate |
| Soltero et al. [61] | 2017 | Moderate |
| do Carmo et al. [10] | 2018 | Moderate |
| Li et al. [62] | 2019 | Moderate |
| Lourenço et al. [63] | 2019 | Moderate |
| Rummo et al. [64] | 2020 | Moderate |
| Chew; Moran; Barnoya [65] | 2020 | Moderate |
| Henriques et al. [66] | 2021 | Moderate |
| Saavedra-Garcia et al. [13] | 2021 | Moderate |
| Leite et al. [3] | 2021 | Moderate |
| Peres et al. [67] | 2021 | Moderate |
| Authors | Year | Local | Sample Size | Unit of Analysis | Types of Food Establishments Evaluated |
|---|---|---|---|---|---|
| Austin et al. [32] | 2005 | Chicago (U.S.) | 1292 schools and 613 food establishments | Density of food establishments on a buffer of 400 and 800 m | Fast-food restaurants |
| Frank et al. [33] | 2006 | Atlanta (U.S.) | 302 food establishments around schools | Density and proximity of food establishments on a buffer of 400, 800, 1200, 1600, and 2000 m | Restaurants, grocery stores, convenience stores, and fast-food restaurants |
| Kipke et al. [34] | 2007 | California (U.S.) | 11 schools and 190 food establishments | Density of food establishments on a buffer of 300 and 500 m | Fast-food restaurants, bakeries, ice cream parlors, convenience stores, butchers and fishmongers, grocery stores/supermarkets |
| Simon et al. [35] | 2008 | California (U.S.) | 1684 schools and 2712 food establishments | Density of food establishments on a buffer of 400 and 800 m on school territory | Fast-food restaurants |
| Sturm [36] | 2008 | US | 31,622 schools | Density of food establishments on buffers of 400 and 800 m | Restaurants (including fast-food outlets), snack and non-alcoholic beverage stores, convenience stores, liquor distributors, and liquor stores |
| Zenk; Powell [37] | 2008 | US | 31,243 schools | Density of food establishments on buffers of 800 m | Convenience stores and fast-food restaurants |
| Davis; Carpenter [26] | 2009 | California (US) | >500,000 students | Density of food establishments on buffer of 800 m | Fast-food restaurants |
| Kestens; Daniel [38] | 2010 | Montreal (Canada) | 1168 schools and 7368 food establishments | Density of food establishments on a buffer of 750 m on school territory | Fast-food restaurants, fruit and vegetable stores, and full-service restaurants |
| Kwate; Loh [39] | 2010 | New York (U.S.) | 2096 schools and 817 food establishments | Density of food establishments on a buffer of 400 m on school territory | Fast-food restaurants |
| Laska et al. [40] | 2010 | Minneapolis (U.S.) | 349 adolescents | Density of food establishments on a buffer of 800, 1600, and 3000 m | Restaurants, fast-food restaurants, convenience stores, grocery stores, and other food establishments |
| Neckerman et al. [41] | 2010 | New York (U.S.) | 1089 schools | Density of food establishments on a buffer of 400 and 800 m | Restaurants, fast-food restaurants, convenience stores, grocery stores, and other food establishments |
| Robitaille; Bergeron, Lasnier [42] | 2010 | Quebec (Canada) | 2302 schools and 5233 food establishments | Density of food establishments on a buffer of 400 and 640 m | Convenience stores and fast-food restaurants |
| Tester; Yen; Laraia [43] | 2010 | California (U.S.) | 6 schools | Density of food establishments on a buffer of 400 m | Street vendors |
| Nixon; Doud [44] | 2011 | California(US) | 41 schools | Density of food establishments on a buffer of 400 and 800 m | Fast-food restaurants |
| Day; Pearce [11] | 2011 | New Zealand | 406 schools 1849 food establishments | Density of food establishments on a buffer of 400 and 800 m | Convenience stores and fast-food restaurants |
| Gebauer; Laska [45] | 2011 | Minneapolis (U.S.) | 36 schools and 63 food establishments | Density of food establishments on a buffer of 800 m | Convenience stores |
| Sanchez et al. [46] | 2012 | California (U.S.) | 926,018 children from 6362 schools | Proximity of food establishments to schools | Fast-food restaurants and convenience stores |
| An; Sturm [47] | 2012 | California (U.S.) | 8226 children and 5236 adolescents | Density and proximity of food establishments on a buffer of 160, 800, 1600, and 2400 m on school territory | Fast-food restaurants, convenience stores, mini-markets, grocery stores, and supermarkets |
| Black; Day [48] | 2012 | British Columbia (Canada) | 1392 schools | Density of food establishments on a buffer of 800 m | Fast-food restaurants, liquor stores, eateries, delis, and convenience stores |
| Ellaway et al. [49] | 2012 | Glasgow (Reino Unido) | 29 schools and 2236 food establishments | Density of food establishments on a buffer of 400 and 800 m | Cafes, takeaways (food for off-site consumption), fast-food restaurants, general stores (such as kiosks and supermarkets), trailers |
| Forsyth et al. [50] | 2012 | Minneapolis (U.S.) | 2724 adolescents in 20 schools | Density of food establishments on a buffer of 800 and 1600 m in school territory | Fast-food restaurants |
| He et al. [8] | 2012 | Ontario (Canada) | 632 adolescents in 21 schools | Density of food establishments on a buffer of 1 km | Convenience stores and fast-food restaurants |
| Héroux et al. [51] | 2012 | Canada, Escócia, and U.S. | 26,778 students of 687 schools and 46 food establishments | Density of food establishments on a buffer of 1 km | Convenience stores, coffee shops, and fast-food restaurants |
| Leite et al. [52] | 2012 | Santos (Brazil) | 3 schools and 82 food establishments | Density of food establishments on a buffer of 500 m | Food establishments classified in the predominant sale of minimally processed and ultra-processed foods |
| Seliske et al. [53] | 2012 | Canada | 6971 students from 158 schools | Density of food establishments on a buffer of 500, 750, 1000, 1500, 2000, and 5000 m | Convenience stores, fast-food restaurants, and coffee shops |
| Buck et al. [14] | 2013 | Delmenhorst (Germany) | 384 children and 188 food establishments | Density of food establishments on a buffer of 1.5 km in school territory | Fast-food restaurants, snack bars, kebab shops, bakeries, kiosks, grocery stores, and supermarkets |
| Day; Pearce; Pearson [54] | 2013 | Christchurch (New Zealand) | Schools and food establishments from 1966 to 2006 | Density of food establishments on a buffer of 800 m | Supermarkets/grocery stores, convenience stores, fast-food restaurants |
| Grier; Davis [55] | 2013 | California (U.S.) | Schools | Proximity of food establishments to schools | Fast-food restaurants |
| Richmond et al. [56] | 2013 | Massachusetts (U.S.) | 18,281 students from 47 schools | Density of food establishments on a buffer of 1.5 km | Convenience stores and fast-food restaurants |
| Smith et al. [24] | 2013 | London (England) | 757 students from 30 schools | Density of food establishments on a buffer of 400 and 800 m | Grocery stores, convenience stores, and takeaways (food for off-site consumption) |
| Engler-Stringer et al. [57] | 2014 | Saskatoon (Canada) | 76 schools, 375 food establishments | Density of food establishments on a buffer of 750 m | Grocery stores, convenience stores, and fast-food restaurants |
| Laxer; Janssen [58] | 2014 | Canada | 6099 adolescents from 255 schools | Density of food establishments on a buffer of 1 km | Fast-food restaurants |
| Clark et al. [59] | 2014 | Otago (New Zealand) | 730 students from 11 schools | Density of food establishments on a buffer of 800 m and 1500 m in school territory | Supermarkets, grocery stores, convenience stores, fast-food restaurants |
| Tang et al. [2] | 2014 | Camden, New Brunswick, Newark e Trenton (New Zealand) | 8 schools | Density of food establishments on a buffer of 400 m | Supermarkets, grocery stores, convenience stores, fast-food restaurants |
| Cutumisu et al. [60] | 2017 | Quebec (Canada) | 374 schools | Density of food establishments on buffer of 750 m | Fast-food restaurants |
| Fitzpatrick et al. [12] | 2017 | Quebec (Canada) | 246 schools | Density of food establishments on a buffer of 750 m | Convenience stores and fast-food restaurants |
| Soltero et al. [61] | 2017 | Guadalajara, Puerto Vallarta, and Mexico City (Mexico) | 32 schools | Density of food establishments on a buffer of 800 m | Supermarkets, grocery stores, convenience stores, table service restaurants, fast-food restaurants, street vendors, taco stands |
| do Carmo et al. [10] | 2018 | Brazil | 1247 schools | Direct observation of food establishments in and around schools | Canteens and street vendors |
| Li et al. [62] | 2019 | US | 52,375 schools | Density of food establishments on a buffer of 800 m | Supermarkets, grocery stores, convenience stores, restaurants |
| Lourenço et al. [63] | 2019 | Brazil | 962 children from 4 schools | Direct observation of food establishments in and around schools | Canteens and street vendors |
| Rummo et al. [64] | 2020 | New York (US) | 361,942 students from 706 schools | Density of food establishments on a buffer of 400 and 800 m | Fast-food restaurants, a la carte restaurants, corner stores, supermarkets |
| Chew; Moran; Barnoya [65] | 2020 | Guatemala | 60 schools | Density of food establishments on a buffer of 150 m | Fast-food restaurants, corner stores, supermarkets, farmer’s stores |
| Henriques et al. [66] | 2021 | Niterói, Brazil | 56 schools | Direct observation of establishments in and around schools (up to 500 m) | Formal and informal food trade |
| Saavedra-Garcia et al. [13] | 2021 | Lima | 15 schools | Direct observation of establishments in and around schools | Canteens and street vendors |
| Leite et al. [3] | 2021 | Juiz de Fora (Minas Gerais- Brazil) | 316 schools and 4690 food establishments | Density of food establishments on a buffer of 250 m, 500 m, and 1000 m | Establishments that sell only or mainly in natural or minimally processed foods; mixed establishments; establishments that sell only or primarily ultra-processed foods; supermarkets and hypermarkets |
| Peres et al. [67] | 2021 | Belo Horizonte (Minas Gerais- Brazil) | 1436 schools | Density of food establishments on a buffer of 250 m | Supermarkets, hypermarkets, grocery stores, snack bars, candy stores, bars, restaurants, bakeries |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
França, F.C.O.d.; Andrade, I.d.S.; Zandonadi, R.P.; Sávio, K.E.; Akutsu, R.d.C.C.d.A. Food Environment around Schools: A Systematic Scope Review. Nutrients 2022, 14, 5090. https://doi.org/10.3390/nu14235090
França FCOd, Andrade IdS, Zandonadi RP, Sávio KE, Akutsu RdCCdA. Food Environment around Schools: A Systematic Scope Review. Nutrients. 2022; 14(23):5090. https://doi.org/10.3390/nu14235090
Chicago/Turabian StyleFrança, Fabiana Chagas Oliveira de, Iziane da Silva Andrade, Renata Puppin Zandonadi, Karin Eleonora Sávio, and Rita de Cassia Coelho de Almeida Akutsu. 2022. "Food Environment around Schools: A Systematic Scope Review" Nutrients 14, no. 23: 5090. https://doi.org/10.3390/nu14235090
APA StyleFrança, F. C. O. d., Andrade, I. d. S., Zandonadi, R. P., Sávio, K. E., & Akutsu, R. d. C. C. d. A. (2022). Food Environment around Schools: A Systematic Scope Review. Nutrients, 14(23), 5090. https://doi.org/10.3390/nu14235090