The Impact of Flavonols on Cardiovascular Risk
Abstract
:1. Introduction
2. Methods
3. General CVD Incidence and Mortality
3.1. Observational Study Data
3.2. Conclusions
4. Hypertension
4.1. Observational Studies Data
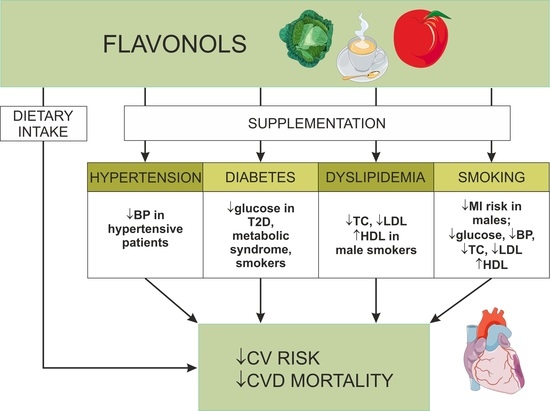
4.2. Interventional Study Data
4.3. Conclusions
5. Dyslipidemia
5.1. Interventional Study Data
5.2. Conclusions
6. Diabetes Mellitus
6.1. Observational Study Data
6.2. Interventional Study Data
6.3. Conclusions
7. Cigarette Smoking
7.1. Observational Study Data
7.2. Interventional Study Data
7.3. Conclusions
8. Limitations
9. Summary and Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| BP | Blood pressure |
| CV | Cardiovascular |
| CVD | Cardiovascular disease |
| CHD | Coronary heart disease |
| HDL-C | High-density lipoprotein cholesterol |
| LDL-C | Low-density lipoprotein cholesterol |
| MI | Myocardial infarction |
| T2D | Type 2 diabetes |
| TC | Total cholesterol |
References
- Pagidipati, N.J.; Gaziano, T.A. Estimating Deaths from Cardiovascular Disease: A Review of Global Methodologies of Mortality Measurement. Circulation 2013, 127, 749–756. [Google Scholar] [CrossRef] [PubMed]
- Lloyd-Jones, D.M.; Hong, Y.; Labarthe, D.; Mozaffarian, D.; Appel, L.J.; Van Horn, L.; Greenlund, K.; Daniels, S.; Nichol, G.; Tomaselli, G.F.; et al. Defining and Setting National Goals for Cardiovascular Health Promotion and Disease Reduction. Circulation 2010, 121, 586–613. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Arnett, D.K.; Blumenthal, R.S.; Albert, M.A.; Buroker, A.B.; Goldberger, Z.D.; Hahn, E.J.; Himmelfarb, C.D.; Khera, A.; Lloyd-Jones, D.; McEvoy, J.W.; et al. 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 2019, 74, e177–e232. [Google Scholar] [CrossRef] [PubMed]
- Panche, A.N.; Diwan, A.D.; Chandra, S.R. Flavonoids: An Overview. J. Nutr. Sci. 2016, 5, e47. [Google Scholar] [CrossRef] [Green Version]
- Sharma, A.; Sharma, P.; Singh Tuli, H.; Sharma, A.K. Phytochemical and Pharmacological Properties of Flavonols. eLS 2018, 2018, 1–12. [Google Scholar]
- Dabeek, W.M.; Marra, M.V. Dietary Quercetin and Kaempferol: Bioavailability and Potential Cardiovascular-Related Bioactivity in Humans. Nutrients 2019, 11, 2288. [Google Scholar] [CrossRef] [Green Version]
- Xiao, J.; Muzashvili, T.S.; Georgiev, M.I. Advances in the Biotechnological Glycosylation of Valuable Flavonoids. Biotechnol. Adv. 2014, 32, 1145–1156. [Google Scholar] [CrossRef]
- Kumar, S.; Pandey, A.K. Chemistry and Biological Activities of Flavonoids: An Overview. Sci. World J. 2013, 2013, 162750. [Google Scholar] [CrossRef] [Green Version]
- Aherne, S.A.; O’Brien, N.M. Dietary Flavonols: Chemistry, Food Content, and Metabolism. Nutrition 2002, 18, 75–81. [Google Scholar] [CrossRef]
- Day, A.J.; Dupont, M.S.; Ridley, S.; Rhodes, M.; Rhodes, M.J.C.; Morgan, M.R.A.; Williamson, G. Deglycosylation of Flavonoid and Isoflavonoid Glycosides by Human Small Intestine and Liver β-Glucosidase Activity. FEBS Lett. 1998, 436, 71–75. [Google Scholar] [CrossRef] [Green Version]
- Manach, C.; Regerat, F.; Texier, O.; Agullo, G.; Demigne, C.; Remesy, C. Bioavailability, Metabolism and Physiological Impact of 4-Oxo-Flavonoids. Nutr. Res. 1996, 16, 517–544. [Google Scholar] [CrossRef]
- Cassidy, A.; O’Reilly, É.J.; Kay, C.; Sampson, L.; Franz, M.; Forman, J.; Curhan, G.; Rimm, E.B. Habitual Intake of Flavonoid Subclasses and Incident Hypertension in Adults. Am. J. Clin. Nutr. 2011, 93, 338–347. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zamora-Ros, R.; Knaze, V.; Luján-Barroso, L.; Slimani, N.; Romieu, I.; Fedirko, V.; Santucci de Magistris, M.; Ericson, U.; Amiano, P.; Trichopoulou, A.; et al. Estimated Dietary Intakes of Flavonols, Flavanones and Flavones in the European Prospective Investigation into Cancer and Nutrition (EPIC) 24 Hour Dietary Recall Cohort. Br. J. Nutr. 2011, 106, 1915–1925. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zamora-Ros, R.; Andres-Lacueva, C.; Lamuela-Raventós, R.M.; Berenguer, T.; Jakszyn, P.; Barricarte, A.; Ardanaz, E.; Amiano, P.; Dorronsoro, M.; Larrañaga, N.; et al. Estimation of Dietary Sources and Flavonoid Intake in a Spanish Adult Population (EPIC-Spain). J. Am. Diet. Assoc. 2010, 110, 390–398. [Google Scholar] [CrossRef]
- Sampson, L.; Rimm, E.; Hollman, P.C.H.; de Vries, J.H.M.; Katan, M.B. Flavonol and Flavone Intakes in US Health Professionals. J. Am. Diet. Assoc. 2002, 102, 1414–1420. [Google Scholar] [CrossRef]
- Chen, X.; Qian, J.; Wang, L.; Li, J.; Zhao, Y.; Han, J.; Khan, Z.; Chen, X.; Wang, J.; Liang, G. Kaempferol Attenuates Hyperglycemia-Induced Cardiac Injuries by Inhibiting Inflammatory Responses and Oxidative Stress. Endocrine 2018, 60, 83–94. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, Y.; Oue, E. Antihypertensive Effect of Quercetin in Rats Fed with a High-Fat High-Sucrose Diet. Biosci. Biotechnol. Biochem. 2006, 70, 933–939. [Google Scholar] [CrossRef] [Green Version]
- Hettihewa, S.K.; Hemar, Y.; Vasantha Rupasinghe, H.P. Flavonoid-Rich Extract of Actinidia Macrosperma (a Wild Kiwifruit) Inhibits Angiotensin-Converting Enzyme in Vitro. Foods 2018, 7, 146. [Google Scholar] [CrossRef] [Green Version]
- Lescano, C.H.; de Lima, F.F.; Mendes-Silvério, C.B.; Justo, A.F.O.; da Silva Baldivia, D.; Vieira, C.P.; Sanjinez-Argandoña, E.J.; Cardoso, C.A.L.; Mónica, F.Z.; de Oliveira, I.P. Effect of Polyphenols from Campomanesia Adamantium on Platelet Aggregation and Inhibition of Cyclooxygenases: Molecular Docking and in Vitro Analysis. Front. Pharmacol. 2018, 9, 617. [Google Scholar] [CrossRef] [Green Version]
- Stainer, A.R.; Sasikumar, P.; Bye, A.P.; Unsworth, A.J.; Holbrook, L.M.; Tindall, M.; Lovegrove, J.A.; Gibbins, J.M. The Metabolites of the Dietary Flavonoid Quercetin Possess Potent Antithrombotic Activity, and Interact with Aspirin to Enhance Antiplatelet Effects. TH Open 2019, 3, e244–e258. [Google Scholar] [CrossRef]
- Li, W.; Yang, C.; Mei, X.; Huang, R.; Zhang, S.; Tang, Y.; Dong, Q.; Zhou, C. Effect of the Polyphenol-Rich Extract from Allium Cepa on Hyperlipidemic Sprague-Dawley Rats. J. Food Biochem. 2021, 45, e13565. [Google Scholar] [CrossRef]
- Hertog, M.G.; Feskens, E.J.; Kromhout, D.; Hertog, M.G.; Hollman, P.C.; Hertog, M.G.; Katan, M. Dietary Antioxidant Flavonoids and Risk of Coronary Heart Disease: The Zutphen Elderly Study. Lancet 1993, 342, 1007–1011. [Google Scholar] [CrossRef]
- Hertog, M.G.L.; Feskens, E.J.M.; Kromhout, D. Antioxidant Flavonols and Coronary Heart Disease Risk. Lancet 1997, 349, 699. [Google Scholar] [CrossRef]
- Knekt, P.; Jarvinen, R.; Reunanen, A.; Maatela, J. Flavonoid Intake and Coronary Mortality in Finland: A Cohort Study. BMJ 1996, 312, 478–481. [Google Scholar] [CrossRef] [Green Version]
- Rimm, E.B. Relation between Intake of Flavonoids and Risk for Coronary Heart Disease in Male Health Professionals. Ann. Intern. Med. 1996, 125, 384. [Google Scholar] [CrossRef] [PubMed]
- Hertog, M.G.L.; Sweetnam, P.M.; Fehily, A.M.; Elwood, P.C.; Kromhout, D. Antioxidant Flavonols and Ischemic Heart Disease in a Welsh Population of Men: The Caerphilly Study. Am. J. Clin. Nutr. 1997, 65, 1489–1494. [Google Scholar] [CrossRef]
- Yochum, L.; Kushi, L.H.; Meyer, K.; Folsom, A.R. Dietary Flavonoid Intake and Risk of Cardiovascular Disease in Postmenopausal Women. Am. J. Epidemiol. 1999, 149, 943–949. [Google Scholar] [CrossRef]
- Geleijnse, J.M.; Launer, L.J.; van der Kuip, D.A.; Hofman, A.; Witteman, J.C.M. Inverse Association of Tea and Flavonoid Intakes with Incident Myocardial Infarction: The Rotterdam Study. Am. J. Clin. Nutr. 2002, 75, 880–886. [Google Scholar] [CrossRef] [PubMed]
- Knekt, P.; Kumpulainen, J.; Järvinen, R.; Rissanen, H.; Heliövaara, M.; Reunanen, A.; Hakulinen, T.; Aromaa, A. Flavonoid Intake and Risk of Chronic Diseases. Am. J. Clin. Nutr. 2002, 76, 560–568. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sesso, H.D.; Gaziano, J.M.; Liu, S.; Buring, J.E. Flavonoid Intake and the Risk of Cardiovascular Disease in Women. Am. J. Clin. Nutr. 2003, 77, 1400–1408. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marniemi, J.; Alanen, E.; Impivaara, O.; Seppänen, R.; Hakala, P.; Rajala, T.; Rönnemaa, T. Dietary and Serum Vitamins and Minerals as Predictors of Myocardial Infarction and Stroke in Elderly Subjects. Nutr. Metab. Cardiovasc. Dis. 2005, 15, 188–197. [Google Scholar] [CrossRef] [PubMed]
- Lin, J.; Rexrode, K.M.; Hu, F.; Albert, C.M.; Chae, C.U.; Rimm, E.B.; Stampfer, M.J.; Manson, J.E. Dietary Intakes of Flavonols and Flavones and Coronary Heart Disease in US Women. Am. J. Epidemiol. 2007, 165, 1305–1313. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Huxley, R.R.; Neil, H.A.W. The Relation between Dietary Flavonol Intake and Coronary Heart Disease Mortality: A Meta-Analysis of Prospective Cohort Studies. Eur. J. Clin. Nutr. 2003, 57, 904–908. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Micek, A.; Godos, J.; Del Rio, D.; Galvano, F.; Grosso, G. Dietary Flavonoids and Cardiovascular Disease: A Comprehensive Dose–Response Meta-Analysis. Mol. Nutr. Food Res. 2021, 65, 2001019. [Google Scholar] [CrossRef] [PubMed]
- Conquer, J.A.; Maiani, G.; Azzini, E.; Raguzzini, A.; Holub, B.J. Supplementation with Quercetin Markedly Increases Plasma Quercetin Concentration without Effect on Selected Risk Factors for Heart Disease in Healthy Subjects. J. Nutr. 1998, 128, 593–597. [Google Scholar] [CrossRef] [PubMed]
- Edwards, R.L.; Lyon, T.; Litwin, S.E.; Rabovsky, A.; Symons, J.D.; Jalili, T. Quercetin Reduces Blood Pressure in Hypertensive Subjects. J. Nutr. 2007, 137, 2405–2411. [Google Scholar] [CrossRef]
- Egert, S.; Bosy-Westphal, A.; Seiberl, J.; Kürbitz, C.; Settler, U.; Plachta-Danielzik, S.; Wagner, A.E.; Frank, J.; Schrezenmeir, J.; Rimbach, G.; et al. Quercetin Reduces Systolic Blood Pressure and Plasma Oxidised Low-Density Lipoprotein Concentrations in Overweight Subjects with a High-Cardiovascular Disease Risk Phenotype: A Double-Blinded, Placebo-Controlled Cross-over Study. Br. J. Nutr. 2009, 102, 1065–1074. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, K.-H.; Park, E.; Lee, H.-J.; Kim, M.-O.; Cha, Y.-J.; Kim, J.-M.; Lee, H.; Shin, M.-J. Effects of Daily Quercetin-Rich Supplementation on Cardiometabolic Risks in Male Smokers. Nutr. Res. Pract. 2011, 5, 28. [Google Scholar] [CrossRef] [Green Version]
- Larson, A.; Witman, M.A.H.; Guo, Y.; Ives, S.; Richardson, R.S.; Bruno, R.S.; Jalili, T.; Symons, J.D. Acute, Quercetin-Induced Reductions in Blood Pressure in Hypertensive Individuals Are Not Secondary to Lower Plasma Angiotensin-Converting Enzyme Activity or Endothelin-1: Nitric Oxide. Nutr. Res. 2012, 32, 557–564. [Google Scholar] [CrossRef]
- Brüll, V.; Burak, C.; Stoffel-Wagner, B.; Wolffram, S.; Nickenig, G.; Müller, C.; Langguth, P.; Alteheld, B.; Fimmers, R.; Naaf, S.; et al. Effects of a Quercetin-Rich Onion Skin Extract on 24 h Ambulatory Blood Pressure and Endothelial Function in Overweight-to-Obese Patients with (Pre-)Hypertension: A Randomised Double-Blinded Placebo-Controlled Cross-over Trial. Br. J. Nutr. 2015, 114, 1263–1277. [Google Scholar] [CrossRef] [Green Version]
- Zahedi, M.; Ghiasvand, R.; Feizi, A.; Asgari, G.; Darvish, L. Does Quercetin Improve Cardiovascular Risk Factors and Inflammatory Biomarkers in Women with Type 2 Diabetes: A Double-Blind Randomized Controlled Clinical Trial. Int. J. Prev. Med. 2013, 4, 777–785. [Google Scholar]
- Pfeuffer, M.; Auinger, A.; Bley, U.; Kraus-Stojanowic, I.; Laue, C.; Winkler, P.; Rüfer, C.E.; Frank, J.; Bösch-Saadatmandi, C.; Rimbach, G.; et al. Effect of Quercetin on Traits of the Metabolic Syndrome, Endothelial Function and Inflammation in Men with Different APOE Isoforms. Nutr. Metab. Cardiovasc. Dis. 2013, 23, 403–409. [Google Scholar] [CrossRef] [PubMed]
- Bondonno, N.P.; Bondonno, C.P.; Rich, L.; Mas, E.; Shinde, S.; Ward, N.C.; Hodgson, J.M.; Croft, K.D. Acute Effects of Quercetin-3-O-Glucoside on Endothelial Function and Blood Pressure: A Randomized Dose-Response Study. Am. J. Clin. Nutr. 2016, 104, 97–103. [Google Scholar] [CrossRef] [PubMed]
- Kondratiuk, V.E.; Synytsia, Y.P. Effect of Quercetin on the Echocardiographic Parameters of Left Ventricular Diastolic Function in Patients with Gout and Essential Hypertension. Wiad. Lek. 2018, 71, 1554–1559. [Google Scholar] [PubMed]
- Burak, C.; Wolffram, S.; Zur, B.; Langguth, P.; Fimmers, R.; Alteheld, B.; Stehle, P.; Egert, S. Effect of Alpha-Linolenic Acid in Combination with the Flavonol Quercetin on Markers of Cardiovascular Disease Risk in Healthy, Non-Obese Adults: A Randomized, Double-Blinded Placebo-Controlled Crossover Trial. Nutrition 2019, 58, 47–56. [Google Scholar] [CrossRef] [PubMed]
- Serban, M.; Sahebkar, A.; Zanchetti, A.; Mikhailidis, D.P.; Howard, G.; Antal, D.; Andrica, F.; Ahmed, A.; Aronow, W.S.; Muntner, P.; et al. Effects of Quercetin on Blood Pressure: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. J. Am. Heart Assoc. 2016, 5, e002713. [Google Scholar] [CrossRef] [Green Version]
- Tamtaji, O.R.; Milajerdi, A.; Dadgostar, E.; Kolahdooz, F.; Chamani, M.; Amirani, E.; Mirzaei, H.; Asemi, Z. The Effects of Quercetin Supplementation on Blood Pressures and Endothelial Function among Patients with Metabolic Syndrome and Related Disorders: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Curr. Pharm. Des. 2019, 25, 1372–1384. [Google Scholar] [CrossRef]
- Suomela, J.P.; Ahotupa, M.; Yang, B.; Vasankari, T.; Kallio, H. Absorption of Flavonols Derived from Sea Buckthorn (Hippophaë Rhamnoides L.) and Their Effect on Emerging Risk Factors for Cardiovascular Disease in Humans. J. Agric. Food Chem. 2006, 54, 7364–7369. [Google Scholar] [CrossRef]
- Talirevic, E.; Sehovic, J. Quercetin in the Treatment of Dyslipidemia. Med. Arch. 2012, 66, 87. [Google Scholar] [CrossRef] [Green Version]
- Sahebkar, A. Effects of Quercetin Supplementation on Lipid Profile: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Crit. Rev. Food Sci. Nutr. 2017, 57, 666–676. [Google Scholar] [CrossRef]
- Tabrizi, R.; Tamtaji, O.R.; Mirhosseini, N.; Lankarani, K.B.; Akbari, M.; Heydari, S.T.; Dadgostar, E.; Asemi, Z. The Effects of Quercetin Supplementation on Lipid Profiles and Inflammatory Markers among Patients with Metabolic Syndrome and Related Disorders: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Crit. Rev. Food Sci. Nutr. 2020, 60, 1855–1868. [Google Scholar] [CrossRef] [PubMed]
- Song, Y.; Manson, J.E.; Buring, J.E.; Sesso, H.D.; Liu, S. Associations of Dietary Flavonoids with Risk of Type 2 Diabetes, and Markers of Insulin Resistance and Systemic Inflammation in Women: A Prospective Study and Cross-Sectional Analysis. J. Am. Coll. Nutr. 2005, 24, 376–384. [Google Scholar] [CrossRef] [PubMed]
- Yao, Z.; Gu, Y.; Zhang, Q.; Liu, L.; Meng, G.; Wu, H.; Xia, Y.; Bao, X.; Shi, H.; Sun, S.; et al. Estimated Daily Quercetin Intake and Association with the Prevalence of Type 2 Diabetes Mellitus in Chinese Adults. Eur. J. Nutr. 2019, 58, 819–830. [Google Scholar] [CrossRef]
- Abidov, M.; Ramazanov, A.; Jimenez Del Rio, M.; Chkhikvishvili, I. Effect of Blueberin on Fasting Glucose, C-Reactive Protein and Plasma Aminotransferases, in Female Volunteers with Diabetes Type 2: Double-Blind, Placebo Controlled Clinical Study. Georgian Med. News 2006, 66–72. [Google Scholar]
- Ahrens, M.J.; Thompson, D.L. Effect of Emulin on Blood Glucose in Type 2 Diabetics. J. Med. Food 2013, 16, 211–215. [Google Scholar] [CrossRef]
- Ostadmohammadi, V.; Milajerdi, A.; Ayati, E.; Kolahdooz, F.; Asemi, Z. Effects of Quercetin Supplementation on Glycemic Control among Patients with Metabolic Syndrome and Related Disorders: A Systematic Review and Meta-analysis of Randomized Controlled Trials. Phyther. Res. 2019, 33, 1330–1340. [Google Scholar] [CrossRef]
- Martin, M.A.; Goya, L.; Ramos, S. Protective Effects of Tea, Red Wine and Cocoa in Diabetes. Evidences from Human Studies. Food Chem. Toxicol. 2017, 109, 302–314. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hirvonen, T.; Pietinen, P.; Virtanen, M.; Ovaskainen, M.-L.; Häkkinen, S.; Albanes, D.; Virtamo, J. Intake of Flavonols and Flavones and Risk of Coronary Heart Disease in Male Smokers. Epidemiology 2001, 12, 62–67. [Google Scholar] [CrossRef]

| Study Group | Compound or Group | Outcome | Significant Association |
|---|---|---|---|
| men aged 65–84 years [22,23]; | flavonoids | CHD mortality | yes |
| postmenopausal women aged 55–69 years [27]; | |||
| healthy women aged 30–69 years [24] | |||
| men aged 40–75 years with CHD [25]; | flavonoids | CHD mortality | no |
| healthy men aged 30–69 years [24] | |||
| healthy men aged 45–59 years [26] | flavonols | CHD mortality | no |
| healthy women aged 30–55 years [32] | kaempferol | CHD mortality | yes |
| healthy mixed population [29] | kaempferol and myricetin | CHD mortality | no |
| healthy mixed population [29] | quercetin | CHD mortality | yes |
| healthy women aged 30–55 years [32] | flavonols | nonfatal MI, CHD mortality | no |
| healthy subjects aged ≥ 55 years [28] | flavonols | fatal MI | yes |
| healthy subjects aged ≥ 55 years [28] | flavonols | all events of MI | no |
| healthy women aged 30–55 years [32] | quercetin, kaempferol, myricetin | nonfatal MI | no |
| healthy men aged 45–59 years [26] | flavonols | CHD incidence | no |
| men aged 40–75 years [25]; | flavonoids, quercetin, kaempferol, myricetin | CHD incidence | no |
| healthy women [30] | |||
| healthy mixed population aged 65–99 years [31] | kaempferol | acute MI | yes |
| healthy mixed population aged 65–99 years [31] | quercetin, myricetin | acute MI | no |
| Study Group | Compound or Group | Outcome | Significant Association |
|---|---|---|---|
| Hypertension | |||
| healthy mixed population [12] | flavonoids, quercetin, kaempferol, isorhamnetin, and myricetin | hypertension incidence | no |
| healthy mixed population [35]; | quercetin | BP level | no |
| prehypertensive patients [36]; | |||
| healthy volunteers [45]; | |||
| normotensive male patients [39] | |||
| pre-hypertensive obese-to-overweight patients [40] | |||
| first stage of hypertension [36]; | quercetin | BP level | yes |
| metabolic syndrome patients (with and without hypertension) [37]; | |||
| hypertensive obese-to-overweight patients [40]; | |||
| first stage hypertensive male patients [39]; | |||
| healthy male smokers [38] | |||
| female T2D patients [41] | quercetin | systolic BP level | yes |
| female T2D patients [41] | quercetin | diastolic BP level | no |
| healthy male patients with different apolipoprotein E genotypes [42] | quercetin | postprandial systolic BP level | yes |
| male patients with essential hypertension and gout [44] | quercetin | systolic and diastolic BP level | unknown |
| healthy volunteers [43] | quercetin | BP level 60 min after administration | no |
| Dyslipidemia | |||
| healthy mixed population [35] | quercetin | LDL-C, HDL-C, TC, and triglycerides | no |
| metabolic syndrome patients [37] | quercetin | HDL-C, oxidized LDL | yes |
| metabolic syndrome patients [37] | quercetin | TC, triglyceride, and LDL-C/HDL-C, TC/HDL-C, triglycerides/HDL-C ratio | no |
| diabetic patients [41] | quercetin | TC, LDL-C, triglycerides, triglycerides/HDL-C, and LDL-C/HDL-C ratio | no |
| healthy male smokers [38] | quercetin | TC, LDL-C, HDL-C | yes |
| healthy men with different apolipoprotein E genotypes [42] | quercetin | postprandial triglycerides and HDL-C | yes |
| patients with dyslipidemia [49] | quercetin | LDL-C, HDL-C, TC, and triglycerides | unknown |
| healthy volunteers [45] | quercetin | TC and LDL-C | no |
| healthy male nonsmokers [48] | quercetin, kaempferol, isorhamnetin | TC, LDL-C, and HDL-C | no |
| Diabetes | |||
| healthy mixed population [29] | quercetin, myricetin | T2D risk | no |
| women free of CVD and diabetes [52] | flavonols, quercetin, kaempferol and myricetin | T2D risk, fasting insulin, glycated hemoglobin | no |
| Chinese population [53] | quercetin | T2D prevalence | yes |
| healthy male smokers [38] | quercetin | glucose concentration | yes |
| patients with metabolic syndrome and related disorders [56] | quercetin | fasting plasma glucose | yes |
| T2D female patients [54] | myricetin | fasting plasma glucose | yes |
| T2D mixed population [55] | myricetin, quercetin, chlorogenic acid | acute glycemic impact of foods, chronic blood glucose | yes |
| patients with metabolic syndrome aged <45 years [56] | quercetin | insulin concentration | yes |
| healthy male nonsmokers [48] | quercetin, kaempferol, isorhamnetin | glucose concentration | no |
| Smoking | |||
| healthy male smokers aged 50–69 years [58] | flavonols | nonfatal MI | yes |
| healthy male smokers [38] | quercetin | glucose concentration | yes |
| healthy male smokers [38] | quercetin | BP level | yes |
| healthy male smokers [38] | quercetin | TC, LDL-C, HDL-C | yes |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Popiolek-Kalisz, J.; Fornal, E. The Impact of Flavonols on Cardiovascular Risk. Nutrients 2022, 14, 1973. https://doi.org/10.3390/nu14091973
Popiolek-Kalisz J, Fornal E. The Impact of Flavonols on Cardiovascular Risk. Nutrients. 2022; 14(9):1973. https://doi.org/10.3390/nu14091973
Chicago/Turabian StylePopiolek-Kalisz, Joanna, and Emilia Fornal. 2022. "The Impact of Flavonols on Cardiovascular Risk" Nutrients 14, no. 9: 1973. https://doi.org/10.3390/nu14091973
APA StylePopiolek-Kalisz, J., & Fornal, E. (2022). The Impact of Flavonols on Cardiovascular Risk. Nutrients, 14(9), 1973. https://doi.org/10.3390/nu14091973