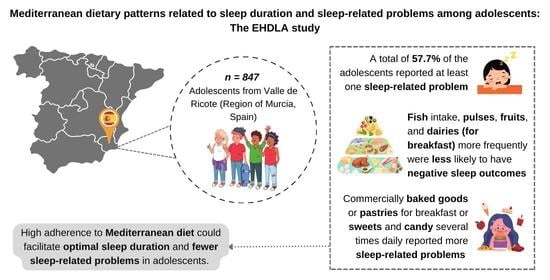
Mediterranean Dietary Patterns Related to Sleep Duration and Sleep-Related Problems among Adolescents: The EHDLA Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Population
2.2. Procedures
2.2.1. Adherence to the Mediterranean Diet
2.2.2. Sleep Recommendations and Sleep-Related Problems (Outcomes)
2.2.3. Covariates
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Zuraikat, F.M.; Wood, R.A.; Barragán, R.; St-Onge, M.-P. Sleep and Diet: Mounting Evidence of a Cyclical Relationship. Annu. Rev. Nutr. 2021, 41, 309–332. [Google Scholar] [CrossRef] [PubMed]
- Walker, M.P.; van der Helm, E. Overnight Therapy? The Role of Sleep in Emotional Brain Processing. Psychol. Bull. 2009, 135, 731–748. [Google Scholar] [CrossRef] [Green Version]
- Lundahl, A.; Nelson, T.D. Sleep and Food Intake: A Multisystem Review of Mechanisms in Children and Adults. J. Health Psychol. 2015, 20, 794–805. [Google Scholar] [CrossRef] [PubMed]
- Medic, G.; Wille, M.; Hemels, M. Short- and Long-Term Health Consequences of Sleep Disruption. Nat. Sci. Sleep 2017, 9, 151–161. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hirshkowitz, M.; Whiton, K.; Albert, S.M.; Alessi, C.; Bruni, O.; DonCarlos, L.; Hazen, N.; Herman, J.; Adams Hillard, P.J.; Katz, E.S.; et al. National Sleep Foundation’s Updated Sleep Duration Recommendations: Final Report. Sleep Health 2015, 1, 233–243. [Google Scholar] [CrossRef] [PubMed]
- Kansagra, S. Sleep Disorders in Adolescents. Pediatrics 2020, 145, S204–S209. [Google Scholar] [CrossRef] [PubMed]
- Sadeh, A.; Mindell, J.; Rivera, L. “My Child Has a Sleep Problem”: A Cross-Cultural Comparison of Parental Definitions. Sleep Med. 2011, 12, 478–482. [Google Scholar] [CrossRef]
- Schneider, N.; Mutungi, G.; Cubero, J. Diet and Nutrients in the Modulation of Infant Sleep: A Review of the Literature. Nutr. Neurosci. 2018, 21, 151–161. [Google Scholar] [CrossRef]
- Owens, J.A.; Weiss, M.R. Insufficient Sleep in Adolescents: Causes and Consequences. Minerva Pediatr. 2017, 69, 326–336. [Google Scholar] [CrossRef]
- Phillips, F.; Crisp, A.H.; Mcguinness, B.; Kalucy, E.C.; Chen, C.N.; Koval, J.; Kalucy, R.S.; Lacey, J.H. Isocaloric Diet Changes and Electroencephalographic Sleep. Lancet 1975, 306, 723–725. [Google Scholar] [CrossRef]
- Binks, H.; Vincent, G.E.; Gupta, C.; Irwin, C.; Khalesi, S. Effects of Diet on Sleep: A Narrative Review. Nutrients 2020, 12, 936. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- St-Onge, M.P.; Mikic, A.; Pietrolungo, C.E. Effects of Diet on Sleep Quality. Adv. Nutr. 2016, 7, 938–949. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhao, M.; Tuo, H.; Wang, S.; Zhao, L. The Effects of Dietary Nutrition on Sleep and Sleep Disorders. Mediat. Inflamm. 2020, 2020, 3142874. [Google Scholar] [CrossRef] [PubMed]
- Guasch-Ferré, M.; Willett, W.C. The Mediterranean Diet and Health: A Comprehensive Overview. J. Intern. Med. 2021, 290, 549–566. [Google Scholar] [CrossRef]
- Willett, W.C. The Mediterranean Diet: Science and Practice. Public Health Nutr. 2006, 9, 105–110. [Google Scholar] [CrossRef] [Green Version]
- Dernini, S.; Berry, E.; Serra-Majem, L.; La Vecchia, C.; Capone, R.; Medina, F.; Aranceta-Bartrina, J.; Belahsen, R.; Burlingame, B.; Calabrese, G.; et al. Med Diet 4.0: The Mediterranean Diet with Four Sustainable Benefits. Public Health Nutr. 2017, 20, 1322–1330. [Google Scholar] [CrossRef] [Green Version]
- Scoditti, E.; Tumolo, M.R.; Garbarino, S. Mediterranean Diet on Sleep: A Health Alliance. Nutrients 2022, 14, 2998. [Google Scholar] [CrossRef]
- Ferranti, R.; Marventano, S.; Castellano, S.; Giogianni, G.; Nolfo, F.; Rametta, S.; Matalone, M.; Mistretta, A. Sleep Quality and Duration Is Related with Diet and Obesity in Young Adolescent Living in Sicily, Southern Italy. Sleep Sci. 2016, 9, 117–122. [Google Scholar] [CrossRef] [Green Version]
- Rosi, A.; Giopp, F.; Milioli, G.; Melegari, G.; Goldoni, M.; Parrino, L.; Scazzina, F. Weight Status, Adherence to the Mediterranean Diet, Physical Activity Level, and Sleep Behavior of Italian Junior High School Adolescents. Nutrients 2020, 12, 478. [Google Scholar] [CrossRef] [Green Version]
- López-Gil, J.F. The Eating Healthy and Daily Life Activities (EHDLA) Study. Children 2022, 9, 370. [Google Scholar] [CrossRef]
- Serra-Majem, L.; Ribas, L.; Ngo, J.; Ortega, R.M.; García, A.; Pérez-Rodrigo, C.; Aranceta, J. Food, Youth and the Mediterranean Diet in Spain. Development of KIDMED, Mediterranean Diet Quality Index in Children and Adolescents. Public Health Nutr. 2004, 7, 931–935. [Google Scholar] [CrossRef]
- Owens, J.A.; Dalzell, V. Use of the ‘BEARS’ Sleep Screening Tool in a Pediatric Residents’ Continuity Clinic: A Pilot Study. Sleep Med. 2005, 6, 63–69. [Google Scholar] [CrossRef] [PubMed]
- Nunes, M.L.; Bruni, O. Insomnia in Childhood and Adolescence: Clinical Aspects, Diagnosis, and Therapeutic Approach. J. Pediatr. 2015, 91, S26–S35. [Google Scholar] [CrossRef] [PubMed]
- Currie, C.; Molcho, M.; Boyce, W.; Holstein, B.; Torsheim, T.; Richter, M. Researching Health Inequalities in Adolescents: The Development of the Health Behaviour in School-Aged Children (HBSC) Family Affluence Scale. Soc. Sci. Med. 2008, 66, 1429–1436. [Google Scholar] [CrossRef] [PubMed]
- Saint-Maurice, P.F.; Welk, G.J. Validity and Calibration of the Youth Activity Profile. PLoS ONE 2015, 10, e0143949. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Peduzzi, P.; Concato, J.; Kemper, E.; Holford, T.R.; Feinstein, A.R. A Simulation Study of the Number of Events per Variable in Logistic Regression Analysis. J. Clin. Epidemiol. 1996, 49, 1373–1379. [Google Scholar] [CrossRef] [PubMed]
- García-Hermoso, A.; Ezzatvar, Y.; López-Gil, J.F.; Ramírez-Vélez, R.; Olloquequi, J.; Izquierdo, M. Is Adherence to the Mediterranean Diet Associated with Healthy Habits and Physical Fitness? A Systematic Review and Meta-Analysis Including 565,421 Youths. Br. J. Nutr. 2020, 128, 1433–1444. [Google Scholar] [CrossRef]
- Iaccarino Idelson, P.; Scalfi, L.; Valerio, G. Adherence to the Mediterranean Diet in Children and Adolescents: A Systematic Review. Nutr. Metab. Cardiovasc. Dis. 2017, 27, 283–299. [Google Scholar] [CrossRef]
- St-Onge, M.-P.; Roberts, A.; Shechter, A.; Choudhury, A.R. Fiber and Saturated Fat Are Associated with Sleep Arousals and Slow Wave Sleep. J. Clin. Sleep Med. 2016, 12, 19–24. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Peuhkuri, K.; Sihvola, N.; Korpela, R. Diet Promotes Sleep Duration and Quality. Nutr. Res. 2012, 32, 309–319. [Google Scholar] [CrossRef]
- Grandner, M.A.; Jackson, N.; Gerstner, J.R.; Knutson, K.L. Dietary Nutrients Associated with Short and Long Sleep Duration. Data from a Nationally Representative Sample. Appetite 2013, 64, 71–80. [Google Scholar] [CrossRef] [Green Version]
- Otocka-Kmiecik, A.; Król, A. The Role of Vitamin C in Two Distinct Physiological States: Physical Activity and Sleep. Nutrients 2020, 12, 3908. [Google Scholar] [CrossRef] [PubMed]
- Doherty, R.; Madigan, S.; Warrington, G.; Ellis, J. Sleep and Nutrition Interactions: Implications for Athletes. Nutrients 2019, 11, 822. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tambalis, K.D.; Panagiotakos, D.B.; Psarra, G.; Sidossis, L.S. Breakfast Skipping in Greek Schoolchildren Connected to an Unhealthy Lifestyle Profile. Results from the National Action for Children’s Health Program. Nutr. Diet. 2019, 76, 328–335. [Google Scholar] [CrossRef]
- López-Gil, J.F.; Smith, L.; López-Bueno, R.; Tárraga-López, P.J. Breakfast and Psychosocial Behavioural Problems in Young Population: The Role of Status, Place, and Habits. Front. Nutr. 2022, 9, 871238. [Google Scholar] [CrossRef]
- Kortesoja, L.; Vainikainen, M.-P.; Hotulainen, R.; Rimpelä, A.; Dobewall, H.; Lindfors, P.; Karvonen, S.; Merikanto, I. Bidirectional Relationship of Sleep with Emotional and Behavioral Difficulties: A Five-Year Follow-up of Finnish Adolescents. J. Youth Adolesc. 2020, 49, 1277–1291. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Monteiro, C.A.; Cannon, G.; Moubarac, J.-C.; Levy, R.B.; Louzada, M.L.C.; Jaime, P.C. The UN Decade of Nutrition, the NOVA Food Classification and the Trouble with Ultra-Processing. Public Health Nutr. 2018, 21, 5–17. [Google Scholar] [CrossRef] [Green Version]
- Delpino, F.M.; Figueiredo, L.M.; Flores, T.R.; Silveira, E.A.; Silva dos Santos, F.; Werneck, A.O.; da Costa Louzada, M.L.; Arcêncio, R.A.; Nunes, B.P. Intake of Ultra-Processed Foods and Sleep-Related Outcomes: A Systematic Review and Meta-Analysis. Nutrition 2023, 106, 111908. [Google Scholar] [CrossRef] [PubMed]
- Sousa, R.D.S.; Bragança, M.L.B.M.; Oliveira, B.R.D.; Coelho, C.C.N.D.S.; Silva, A.A.M.D. Association between the Degree of Processing of Consumed Foods and Sleep Quality in Adolescents. Nutrients 2020, 12, 462. [Google Scholar] [CrossRef] [Green Version]
- Lane, K.E.; Davies, I.G.; Darabi, Z.; Ghayour-Mobarhan, M.; Khayyatzadeh, S.S.; Mazidi, M. The Association between Ultra-Processed Foods, Quality of Life and Insomnia among Adolescent Girls in Northeastern Iran. Int. J. Environ. Res. Public Health 2022, 19, 6338. [Google Scholar] [CrossRef]
- Irwin, M.R.; Olmstead, R.; Carroll, J.E. Sleep Disturbance, Sleep Duration, and Inflammation: A Systematic Review and Meta-Analysis of Cohort Studies and Experimental Sleep Deprivation. Biol. Psychiatry 2016, 80, 40–52. [Google Scholar] [CrossRef] [Green Version]
- Lane, J.M.; Vlasac, I.; Anderson, S.G.; Kyle, S.D.; Dixon, W.G.; Bechtold, D.A.; Gill, S.; Little, M.A.; Luik, A.; Loudon, A.; et al. Genome-Wide Association Analysis Identifies Novel Loci for Chronotype in 100,420 Individuals from the UK Biobank. Nat. Commun. 2016, 7, 10889. [Google Scholar] [CrossRef] [Green Version]
- Werneck, A.O.; Vancampfort, D.; Oyeyemi, A.L.; Stubbs, B.; Silva, D.R. Joint Association of Ultra-Processed Food and Sedentary Behavior with Anxiety-Induced Sleep Disturbance among Brazilian Adolescents. J. Affect. Disord. 2020, 266, 135–142. [Google Scholar] [CrossRef]
- Mesas, A.E.; González, A.D.; de Andrade, S.M.; Martínez-Vizcaíno, V.; López-Gil, J.F.; Jiménez-López, E. Increased Consumption of Ultra-Processed Food Is Associated with Poor Mental Health in a Nationally Representative Sample of Adolescent Students in Brazil. Nutrients 2022, 14, 5207. [Google Scholar] [CrossRef]
- Jansen, E.C.; Conroy, D.A.; Burgess, H.J.; O’Brien, L.M.; Cantoral, A.; Téllez-Rojo, M.M.; Peterson, K.E.; Baylin, A. Plasma DHA Is Related to Sleep Timing and Duration in a Cohort of Mexican Adolescents. J. Nutr. 2020, 150, 592–598. [Google Scholar] [CrossRef]
- Dai, Y.; Liu, J. Omega-3 Long-Chain Polyunsaturated Fatty Acid and Sleep: A Systematic Review and Meta-Analysis of Randomized Controlled Trials and Longitudinal Studies. Nutr. Rev. 2021, 79, 847–868. [Google Scholar] [CrossRef]
- Hartmann, J.A.; Wichers, M.; van Bemmel, A.L.; Derom, C.; Thiery, E.; Jacobs, N.; van Os, J.; Simons, C.J.P. The Serotonin Transporter 5-HTTLPR Polymorphism in the Association between Sleep Quality and Affect. Eur. Neuropsychopharmacol. 2014, 24, 1086–1090. [Google Scholar] [CrossRef]
- Young, S.N. The 1989 Borden Award Lecture. Some Effects of Dietary Components (Amino Acids, Carbohydrate, Folic Acid) on Brain Serotonin Synthesis, Mood, and Behavior. Can. J. Physiol. Pharmacol. 1991, 69, 893–903. [Google Scholar] [CrossRef]
- Layman, D.K.; Lönnerdal, B.; Fernstrom, J.D. Applications for α-Lactalbumin in Human Nutrition. Nutr. Rev. 2018, 76, 444–460. [Google Scholar] [CrossRef] [Green Version]
- Bravo, R.; Matito, S.; Cubero, J.; Paredes, S.D.; Franco, L.; Rivero, M.; Rodríguez, A.B.; Barriga, C. Tryptophan-Enriched Cereal Intake Improves Nocturnal Sleep, Melatonin, Serotonin, and Total Antioxidant Capacity Levels and Mood in Elderly Humans. AGE 2013, 35, 1277–1285. [Google Scholar] [CrossRef]
- Arendt, J.; Deacon, S.; English, J.; Hampton, S.; Morgan, L. Melatonin and Adjustment to Phase Shift. J. Sleep Res. 1995, 4, 74–79. [Google Scholar] [CrossRef] [PubMed]

| Variables | M ± SD/n (%) |
|---|---|
| Covariates | |
| Sex | |
| Boys | 379 (44.7) |
| Girls | 468 (55.3) |
| Age (years) | 14.1 ± 1.6 |
| FAS-III (score) | 8.2 ± 2.1 |
| Waist circumference (cm) | 73.0 ± 10.3 |
| Energy intake (kcal) | 3027 ± 1980 |
| YAP-S physical activity (score) | 2.6 ± 0.7 |
| YAP-S sedentary behavior (score) | 2.6 ± 0.6 |
| Adherence to the MD | |
| KIDMED (score) | 6.6 ± 2.5 |
| Low and moderate MD, n (%) | 524 (61.9) |
| High MD, n (%) | 323 (38.1) |
| Sleep duration | |
| Weekdays (min) | 466.0 ± 60.1 |
| Weekends (min) | 555.3 ± 83.7 |
| Overall (min) | 491.5 ± 53.7 |
| Meeting with sleep recommendations, n (%) | 210 (24.8) |
| Sleep-related problems | |
| Bedtime problems, n (%) | 195 (23.0) |
| Excessive day sleepiness, n (%) | 281 (33.2) |
| Awakening during night, n (%) | 128 (15.1) |
| Regularity and duration of sleep, n (%) | 247 (29.2) |
| Sleep-disordered breathing, n (%) | 56 (6.6) |
| At least one sleep-related problem, n (%) | 489 (57.7) |
| Variables | Not Meeting Sleep Recommendations (n = 637; 75.2%) | Meeting Sleep Recommendations (n = 210; 24.8%) | p | No Sleep-Related Problems (n = 358; 43.3%) | At Least One Sleep-Related Problem (n = 489; 57.7%) | p |
|---|---|---|---|---|---|---|
| Individual components | ||||||
| Takes a fruit or fruit juice every day | 459 (72.1) | 169 (80.5) | 0.016 | 279 (77.9) | 349 (71.4) | 0.031 |
| Has a second fruit every day | 238 (37.4) | 96 (45.7) | 0.032 | 149 (41.6) | 185 (37.8) | 0.265 |
| Has fresh or cooked vegetables regularly once a day | 450 (70.6) | 152 (72.4) | 0.630 | 261 (72.9) | 341 (69.7) | 0.315 |
| Has fresh or cooked vegetables more than once a day | 210 (33.0) | 75 (35.7) | 0.465 | 109 (30.4) | 176 (36.0) | 0.092 |
| Consumes fish regularly (at least 2–3 times per week) | 371 (58.2) | 136 (64.8) | 0.095 | 229 (64.0) | 278 (56.9) | 0.037 |
| Goes more than once a week to a fast-food (hamburger) restaurant | 445 (69.9) | 143 (68.1) | 0.631 | 255 (71.2) | 333 (68.1) | 0.329 |
| Likes pulses and eats them more than once a week | 477 (74.9) | 176 (83.8) | 0.008 | 285 (79.6) | 368 (75.3) | 0.136 |
| Consumes pasta or rice almost every day (5 or more times per week) | 369 (57.9) | 113 (53.8) | 0.296 | 193 (53.9) | 289 (59.1) | 0.132 |
| Has cereals or grains (bread, etc.) for breakfast | 374 (58.7) | 127 (60.5) | 0.652 | 213 (59.5) | 288 (58.9) | 0.860 |
| Consumes nuts regularly (at least 2–3 times per week) | 373 (58.6) | 122 (58.1) | 0.907 | 217 (60.6) | 278 (56.9) | 0.272 |
| Uses olive oil at home | 622 (97.6) | 335 (96.2) | 0.325 | 352 (98.3) | 472 (96.5) | 0.136 |
| Skips breakfast | 108 (17.0) | 19 (9.0) | 0.005 | 39 (10.9) | 88 (18.0) | 0.004 |
| Has a dairy product for breakfast (yogurt, milk, etc.) | 483 (75.8) | 164 (78.1) | 0.502 | 287 (80.2) | 360 (73.6) | 0.027 |
| Has commercially baked goods or pastries for breakfast | 104 (16.3) | 29 (13.8) | 0.385 | 35 (9.8) | 98 (20.0) | <0.001 |
| Takes two yogurts and/or some cheese (40 g) daily | 237 (37.2) | 85 (40.5) | 0.397 | 141 (39.4) | 181 (37.0) | 0.483 |
| Takes sweets and candy several times every day | 480 (75.4) | 176 (83.8) | 0.011 | 198 (55.3) | 326 (66.7) | 0.014 |
| Adherence to the MD | ||||||
| High MD (≥8 points) | 226 (35.5) | 97 (46.2) | 0.006 | 160 (44.7) | 163 (33.3) | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
López-Gil, J.F.; Smith, L.; Victoria-Montesinos, D.; Gutiérrez-Espinoza, H.; Tárraga-López, P.J.; Mesas, A.E. Mediterranean Dietary Patterns Related to Sleep Duration and Sleep-Related Problems among Adolescents: The EHDLA Study. Nutrients 2023, 15, 665. https://doi.org/10.3390/nu15030665
López-Gil JF, Smith L, Victoria-Montesinos D, Gutiérrez-Espinoza H, Tárraga-López PJ, Mesas AE. Mediterranean Dietary Patterns Related to Sleep Duration and Sleep-Related Problems among Adolescents: The EHDLA Study. Nutrients. 2023; 15(3):665. https://doi.org/10.3390/nu15030665
Chicago/Turabian StyleLópez-Gil, José Francisco, Lee Smith, Desirée Victoria-Montesinos, Héctor Gutiérrez-Espinoza, Pedro J. Tárraga-López, and Arthur Eumann Mesas. 2023. "Mediterranean Dietary Patterns Related to Sleep Duration and Sleep-Related Problems among Adolescents: The EHDLA Study" Nutrients 15, no. 3: 665. https://doi.org/10.3390/nu15030665
APA StyleLópez-Gil, J. F., Smith, L., Victoria-Montesinos, D., Gutiérrez-Espinoza, H., Tárraga-López, P. J., & Mesas, A. E. (2023). Mediterranean Dietary Patterns Related to Sleep Duration and Sleep-Related Problems among Adolescents: The EHDLA Study. Nutrients, 15(3), 665. https://doi.org/10.3390/nu15030665