Application of Superabsorbent Spacer Fabrics as Exuding Wound Dressing
Abstract
:1. Introduction
2. Materials and Methods
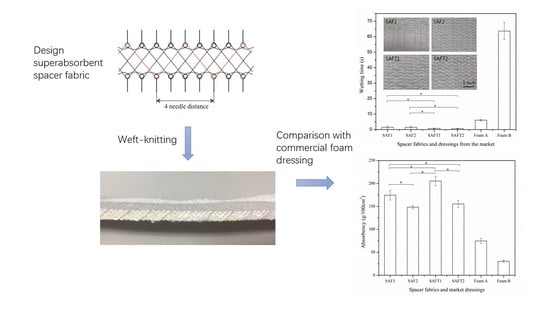
2.1. Fabrication of Superabsorbent Spacer Fabrics
2.2. Property Evaluation
2.2.1. Wettability Test
2.2.2. Absorbency Test
2.2.3. Air Permeability Test
2.2.4. Water Vapor Transmission Rate (WVTR) Test
A = πd2/4 (d = 0.083m)
2.2.5. Thermal Insulation Test
2.2.6. Conformability Test
2.2.7. Statistical Analysis
3. Results and Discussion
3.1. Wettability
3.2. Absorbency
3.3. Air Permeability
3.4. Water Vapor Permeability
3.5. Thermal Insulation
3.6. Conformability
4. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Winter, G.D. Formation of the scab and the rate of epithelization of superficial wounds in the skin of the young domestic pig. Nature 1962, 193, 293–294. [Google Scholar] [CrossRef] [PubMed]
- Watson, N.F.; Hodgkin, W. Wound dressings. Surgery 2005, 23, 52–55. [Google Scholar] [CrossRef]
- Abdelrahman, T.; Newton, H. Wound dressings: Principles and practice. Surgery 2011, 29, 491–495. [Google Scholar] [CrossRef]
- Ovington, L.G. Advances in wound dressings. Clin. Derm. 2007, 25, 33–38. [Google Scholar] [CrossRef] [PubMed]
- Seaman, S. Dressing selection in chronic wound management. J. Am. Podiat. Med. Assoc. 2002, 92, 24–33. [Google Scholar] [CrossRef]
- Prockop, D.J.; Kivirikko, K.I.; Tuderman, L.; Guzman, N.A. The biosynthesis of collagen and its disorders. N. Eng. J. Med. 1979, 301, 77–85. [Google Scholar] [CrossRef] [PubMed]
- Stephens, F.O.; Hunt, T.K. Effect of changes in inspired oxygen and carbon dioxide tensions on wound tensile strength: An experimental study. Ann. Surg. 1971, 173, 515–519. [Google Scholar] [CrossRef] [PubMed]
- Hunt, T.K.; Zederfeldt, B.; Goldstick, T.K. Oxygen and healing. Am. J. Surg. 1969, 118, 521–525. [Google Scholar] [CrossRef]
- Steed, D.L. Debridement. Am. J. Surg. 2004, 187, S71–S74. [Google Scholar] [CrossRef]
- Yager, D.R.; Cohen, I.K.; Diegelmann, R.F.; Montante, S.; Bertoniere, N.; Bopp, A.F. Modified cotton gauze dressings that selectively absorb neutrophil elastase activity in solution. Wound Rep. Reg. 2001, 9, 50–58. [Google Scholar] [CrossRef]
- Rajendran, S.; Anand, S. Hi-tech textiles for interactive wound therapies. In Handbook of Medical Textiles; Bartels, V.T., Ed.; Elsevier: Cambridge, UK, 2011; pp. 38–79. ISBN 978-0-85709-369-1. [Google Scholar]
- Barnea, Y.; Weiss, J.; Gur, E. A review of the applications of the hydrofiber dressing with silver (Aquacel Ag®) in wound care. Ther. Clin. Risk. Manag. 2010, 6, 21–27. [Google Scholar] [CrossRef] [PubMed]
- Kent, D.J. Introducing alginate dressings. Nurs. Made Incred. Easy 2009, 7, 26–27. [Google Scholar] [CrossRef]
- Davies, S.; Owen, P. Staying dry and keeping your cool: An in-depth survey of the methods and products currently available. Text. Month 1989, 87, 1481–1493. [Google Scholar]
- Donaghue, V.M.; Chrzan, J.S.; Rosenblum, B.I.; Giurini, J.M.; Habershaw, G.M.; Veves, A. Evaluation of a Collagen-Alginate Wound Dressing in the Management. Adv. Wound Care 1998, 11, 114–118. [Google Scholar] [PubMed]
- Torres, D.C.O.; Galindo, C.A. Pure calcium-sodium alginate dressing. Multicenter evaluation of chronic cutaneous lesions. Rev. Enferm. 1997, 20, 23–30. [Google Scholar]
- Chaby, G.; Senet, P.; Vaneau, M. Dressings for acute and chronic wounds: A systematic review. Arch. Dermatol. 2007, 143, 1297–1304. [Google Scholar] [CrossRef] [PubMed]
- Martini, L.; Reali, U.M.; Borgognoni, L.; Brandani, P.; Andriessen, A. Comparison of two dressings in the management of partial-thickness donor sites. J. Wound Care 1999, 8, 457–461. [Google Scholar] [CrossRef] [PubMed]
- Davies, A.; Williams, J. The Use of spacer fabrics for absorbent medical applications. J. Fib. Bioeng. Inform. 2009, 1, 321–330. [Google Scholar] [CrossRef]
- Tong, S.-F.; Yip, J.; Yick, K.-L.; Yuen, C.-W.M. Exploring use of warp-knitted spacer fabric as a substitute for the absorbent layer for advanced wound dressing. Text. Res. J. 2015, 85, 1258–1268. [Google Scholar] [CrossRef]
- Yang, Y.; Hu, H. Spacer fabric-based exuding wound dressing–Part I: Structural design, fabrication and property evaluation of spacer fabrics. Text. Res. J. 2016, 87, 1469–1480. [Google Scholar] [CrossRef]
- Yang, Y.; Hu, H. Spacer fabric-based exuding wound dressing–Part II: Comparison with commercial wound dressings. Text. Res. J. 2016, 87, 1481–1493. [Google Scholar] [CrossRef]
- Yang, Y.; Bechtold, T.; Redl, B.; Caven, B.; Hu, H. A novel silver-containing absorbent wound dressing based on spacer fabric. J. Mater. Chem. B 2017, 5, 6786–6793. [Google Scholar] [CrossRef]
- SAF™ (Super Absorbent Fiber). Available online: https://techabsorbents.com/uploads/files/Safety-Data-Sheet-%28SDS%29-eng.pdf (accessed on 22 February 2018).
- SAF™ (Super Absorbent Fiber). Available online: https://techabsorbents.com/en/products/saf (accessed on 22 February 2018).
- Wound Care. Available online: https://www.coloplast.com/Products/wound/#section=Painful-wounds_312727 (accessed on 22 February 2018).
- ALLEVYN Non-Adhesive. Available online: http://www.smith-nephew.com/key-products/advanced-wound-management/allevyn/allevyn-non-adhesive/ (accessed on 22 February 2018).
- Wahab, N. The Use of a Superabsorbent Three Layer Wicking Wound Dressing to Manage Diabetic Wounds in a Long-Term Care Facility. Available online: http://wce.lasvegaswebsolution.com/wp-content/uploads/2016/06/Qwick-2015-Wahab-LIT031WC.pdf (accessed on 22 February 2018).
- Schultz, G.S.; Sibbald, R.G.; Falanga, V.; Ayello, E.A.; Dowsett, C.; Harding, K.; Romanelli, M.; Stacey, M.C.; Teot, L.; Vanscheidt, W. Wound bed preparation: A systematic approach to wound management. Wound Repair Regen. 2003, 11, 1–28. [Google Scholar] [CrossRef]
- Bucalo, B.; Eaglstein, W.H.; Falanga, V. Inhibition of cell proliferation by chronic wound fluid. Wound Repair Regen. 1993, 1, 181–186. [Google Scholar] [CrossRef] [PubMed]
- Falanga, V.; Grinnell, F.; Gilchrest, B.; Maddox, Y.T.; Moshell, A. Workshop on the pathogenesis of chronic wounds. J. Investig. Dermatol. 1994, 102, 125–127. [Google Scholar] [CrossRef] [PubMed]
- Chakravarthy, D.; Roman, M. In vitro vertical wicking capacity of a three-layer wicking wound dressing. J. Wound Ost. Cont. Nurs. 2015, 42, S60. [Google Scholar]
- Gil, E.S.; Panilaitis, B.; Bellas, E.; Kap, D.L. Functionalized silk biomaterials for wound healing. Adv. Healthc. Mater. 2013, 2, 206–217. [Google Scholar] [CrossRef] [PubMed]
- Babior, B.M. Oxygen-dependent microbial killing by phagocytes. N. Eng. J. Med. 1978, 298, 659–668. [Google Scholar] [CrossRef] [PubMed]
- Holloway, S. Recognising and treating the causes of chronic malodorous wounds. Prof. Nurse 2004, 19, 380–384. [Google Scholar]
- Bolton, L.L.; Johnson, C.L.; Van Rijswijk, L. Occlusive dressings: Therapeutic agents and effects on drug delivery. Clin. Dermatol. 1991, 9, 573–583. [Google Scholar] [CrossRef]
- Lee, Y.M.; Kim, S.S.; Park, M.H.; Song, K.W.; Sung, Y.K.; Kang, I.K. β-Chitin-based wound dressing containing silver sulfurdiazine. J. Mater. Sci. Mater. Med. 2000, 11, 817–823. [Google Scholar] [CrossRef] [PubMed]
- Sussman, G. Technology update: Understanding foam dressings. Wounds Intern. 2010, 1, 2. [Google Scholar]













| Yarn designation | SAF | SAFT | |
|---|---|---|---|
| Absorbency (g/g) | 35 | 32 | |
| Linear density (dtex) | 2477 | 5071 | |
| Diameter (mm) | 0.85 | 1.45 | |
| Minimum breaking strength (N) | 18 | 100 | |
| Maximum breaking extension (%) | 15 | 15 | |
| Composition (%) | Superabsorbent fiber | 26.2 | 27.8 |
| PES fiber | 61.5 | 65.4 | |
| PA fiber | 12.3 | 6.8 | |
| Fabric Code | SAF1 | SAF2 | SAFT1 | SAFT2 | |
|---|---|---|---|---|---|
| Number of surface yarns | 1 | 2 | 1 | 2 | |
| Type of spacer yarn | SAF | SAF | SAFT | SAFT | |
| Fabric thickness (mm) | 6.271 (± 0.288) | 6.227 (± 0.187) | 6.423 (± 0.127) | 6.048 (± 0.257) | |
| Areal mass of fabric (g/cm2) | 0.159 (± 0.004) | 0.163 (± 0.014) | 0.211 (± 0.009) | 0.227 (± 0.004) | |
| Density (g/cm3) | 0.253 (± 0.006) | 0.261 (± 0.022) | 0.328 (± 0.013) | 0.376 (± 0.006) | |
| Porosity (%) | 79.7 (± 0.2) | 79.0 (± 0.5) | 73.8 (± 0.8) | 70.0 (± 0.4) | |
| Surface stitch density | Course direction (wales/cm) | 3.62 (± 0.08) | 3.96 (± 0.15) | 2.78 (± 0.08) | 2.94 (± 0.05) |
| Wale direction (courses/cm) | 7.62 (± 0.30) | 6.76 (± 0.22) | 5.86 (± 0.15) | 6.02 (± 0.04) | |
| Stitch density (loops/cm2) | 27.58 (± 1.16) | 26.75 (± 0.78) | 16.29 (± 0.55) | 17.7 (± 0.42) | |
| Code | Base material | Product name & brand | Areal mass (g/cm2) | Thickness (mm) |
|---|---|---|---|---|
| Foam A | Hydrophilic polyurethane foam | Biatain non-adhesive foam dressing from Coloplast | 0.0754 (± 0.0023) | 4.65 (± 0.06) |
| Foam B | Hydrocellular polyurethane foam | Allevyn non-adhesive foam dressing from Smith & Nephew | 0.0680 (± 0.0014) | 5.70 (± 0.05) |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yang, Y.; Hu, H. Application of Superabsorbent Spacer Fabrics as Exuding Wound Dressing. Polymers 2018, 10, 210. https://doi.org/10.3390/polym10020210
Yang Y, Hu H. Application of Superabsorbent Spacer Fabrics as Exuding Wound Dressing. Polymers. 2018; 10(2):210. https://doi.org/10.3390/polym10020210
Chicago/Turabian StyleYang, Yadie, and Hong Hu. 2018. "Application of Superabsorbent Spacer Fabrics as Exuding Wound Dressing" Polymers 10, no. 2: 210. https://doi.org/10.3390/polym10020210
APA StyleYang, Y., & Hu, H. (2018). Application of Superabsorbent Spacer Fabrics as Exuding Wound Dressing. Polymers, 10(2), 210. https://doi.org/10.3390/polym10020210