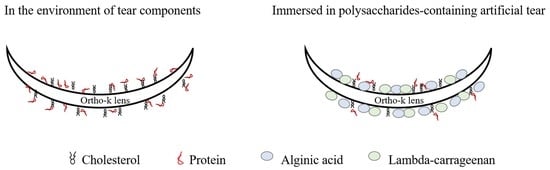
The Effect of Polysaccharides on Preventing Proteins and Cholesterol from Being Adsorbed on the Surface of Orthokeratology Lenses
Abstract
:1. Introduction
2. Materials and Methods
2.1. Orthokeratology Lenses, Polysaccharide-Containing Artificial Tear Solution, and Cleaning Solution
2.2. Cholesterol and Protein Adsorption Analysis
2.3. Measurement of Contact Lens
2.4. Statistical Data Analysis
3. Results
3.1. Low Concentration of Polysaccharides Could Prevent Cholesterol Adsorption Weakly
3.2. Distinct Effects of Polysaccharides on Lysozyme and Albumin Adsorption
3.3. Contact Angle of Lenses Was Reduced after the Treatment of Polysaccharides
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Van Meter, W.S.; Musch, D.C.; Jacobs, D.S.; Kaufman, S.C.; Reinhart, W.J.; Udell, I.J. Safety of overnight orthokeratology for myopia: A report by the american academy of ophthalmology. Ophthalmology 2008, 115, 2301–2313.e1. [Google Scholar] [CrossRef] [PubMed]
- Lipson, M.J.; Sugar, A.; Musch, D.C. Overnight corneal reshaping versus soft disposable contact lenses: Vision-related quality-of-life differences from a randomized clinical trial. Optom. Vis. Sci. 2005, 82, 886–891. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vincent, S.J.; Cho, P.; Chan, K.Y.; Fadel, D.; Ghorbani-Mojarrad, N.; Gonzalez-Meijome, J.M.; Johnson, L.; Kang, P.; Michaud, L.; Simard, P.; et al. Clear—Orthokeratology. Contact Lens Anterior Eye 2021, 44, 240–269. [Google Scholar] [CrossRef] [PubMed]
- Lipson, M.J.; Brooks, M.M.; Koffler, B.H. The role of orthokeratology in myopia control: A review. Eye Contact Lens 2018, 44, 224–230. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cheung, S.W.; Cho, P. Subjective and objective assessments of the effect of orthokeratology—A cross-sectional study. Curr. Eye Res. 2004, 28, 121–127. [Google Scholar] [CrossRef]
- Pucker, A.D. A review of the compatibility of topical artificial tears and rewetting drops with contact lenses. Contact Lens Anterior Eye 2020, 43, 426–432. [Google Scholar] [CrossRef]
- Sariri, R.; Ghafoori, H. Tear proteins in health, disease, and contact lens wear. Biochemistry 2008, 73, 381–392. [Google Scholar] [CrossRef]
- Su, C.Y.; Yeh, L.K.; Tsao, Y.F.; Lin, W.P.; Hou, C.H.; Huang, H.F.; Lai, C.C.; Fang, H.W. The effect of different cleaning methods on protein deposition and optical characteristics of orthokeratology lenses. Polymers 2021, 13, 4318. [Google Scholar] [CrossRef]
- Fleiszig, S.M.; Evans, D.J. Pathogenesis of contact lens-associated microbial keratitis. Optom. Vis. Sci. 2010, 87, 225–232. [Google Scholar] [CrossRef] [Green Version]
- Barniak, V.L.; Burke, S.E.; Venkatesh, S. Comparative evaluation of multi-purpose solutions in the stabilization of tear lysozyme. Contact Lens Anterior Eye 2010, 33 (Suppl. S1), S7–S11. [Google Scholar] [CrossRef]
- Cho, P.; Poon, H.Y.; Chen, C.C.; Yuon, L.T. To rub or not to rub?—Effective rigid contact lens cleaning. Ophthalmic Physiol. Opt. 2020, 40, 17–23. [Google Scholar] [CrossRef]
- Pucker, A.D.; Nichols, J.J. Impact of a rinse step on protein removal from silicone hydrogel contact lenses. Optom. Vis. Sci. 2009, 86, 943–947. [Google Scholar] [CrossRef] [Green Version]
- Su, C.Y.; Chen, C.C.; Huang, Y.L.; Chen, S.W.; Fang, H.W. Optimization of biomolecular additives for a reduction of friction in the artificial joint system. Tribol. Int. 2017, 111, 220–225. [Google Scholar] [CrossRef]
- Frediansyah, A. The antiviral activity of iota-, kappa-, and lambda-carrageenan against COVID-19: A critical review. Clin. Epidemiol. Glob Health 2021, 12, 100826. [Google Scholar] [CrossRef]
- Guo, X.; Wang, Y.; Qin, Y.; Shen, P.; Peng, Q. Structures, properties and application of alginic acid: A review. Int. J. Biol. Macromol. 2020, 162, 618–628. [Google Scholar] [CrossRef]
- Sanchez-Ballester, N.M.; Bataille, B.; Soulairol, I. Sodium alginate and alginic acid as pharmaceutical excipients for tablet formulation: Structure-function relationship. Carbohydr. Polym. 2021, 270, 118399. [Google Scholar] [CrossRef]
- Almutairi, F.M.; Adams, G.G.; Kok, M.S.; Lawson, C.J.; Gahler, R.; Wood, S.; Foster, T.J.; Rowe, A.J.; Harding, S.E. An analytical ultracentrifugation based study on the conformation of lambda carrageenan in aqueous solution. Carbohydr. Polym. 2013, 97, 203–209. [Google Scholar] [CrossRef]
- Lee, K.Y.; Mooney, D.J. Alginate: Properties and biomedical applications. Prog. Polym. Sci. 2012, 37, 106–126. [Google Scholar] [CrossRef] [Green Version]
- Guibet, M.; Colin, S.; Barbeyron, T.; Genicot, S.; Kloareg, B.; Michel, G.; Helbert, W. Degradation of lambda-carrageenan by pseudoalteromonas carrageenovora lambda-carrageenase: A new family of glycoside hydrolases unrelated to kappa- and iota-carrageenases. Biochem. J. 2007, 404, 105–114. [Google Scholar] [CrossRef] [Green Version]
- Hentati, F.; Delattre, C.; Ursu, A.V.; Desbrieres, J.; Le Cerf, D.; Gardarin, C.; Abdelkafi, S.; Michaud, P.; Pierre, G. Structural characterization and antioxidant activity of water-soluble polysaccharides from the tunisian brown seaweed cystoseira compressa. Carbohydr. Polym. 2018, 198, 589–600. [Google Scholar] [CrossRef]
- Rhein-Knudsen, N.; Ale, M.T.; Meyer, A.S. Seaweed hydrocolloid production: An update on enzyme assisted extraction and modification technologies. Mar. Drugs 2015, 13, 3340–3359. [Google Scholar] [CrossRef] [PubMed]
- Choy, C.K.; Cho, P.; Benzie, I.F.; Ng, V. Effect of one overnight wear of orthokeratology lenses on tear composition. Optom. Vis. Sci. 2004, 81, 414–420. [Google Scholar] [CrossRef] [PubMed]
- Sack, R.A.; Tan, K.O.; Tan, A. Diurnal tear cycle: Evidence for a nocturnal inflammatory constitutive tear fluid. Invest. Ophthalmol. Vis. Sci. 1992, 33, 626–640. [Google Scholar] [PubMed]
- Omali, N.B.; Subbaraman, L.N.; Heynen, M.; Ng, A.; Coles-Brennan, C.; Fadli, Z.; Jones, L. Surface versus bulk activity of lysozyme deposited on hydrogel contact lens materials in vitro. Contact Lens Anterior Eye 2018, 41, 329–334. [Google Scholar] [CrossRef]
- Perrigin, J.; Perrigin, D.; Quintero, S.; Grosvenor, T. Silicone-acrylate contact lenses for myopia control: 3-year results. Optom. Vis. Sci. 1990, 67, 764–769. [Google Scholar] [CrossRef]
- Bontempo, A.R.; Rapp, J. Protein-lipid interaction on the surface of a rigid gas-permeable contact lens in vitro. Curr. Eye Res. 1997, 16, 1258–1262. [Google Scholar] [CrossRef]
- Valachova, K.; Soltes, L. Versatile use of chitosan and hyaluronan in medicine. Molecules 2021, 26, 1195. [Google Scholar] [CrossRef]
- Omali, N.B.; Subbaraman, L.N.; Heynen, M.; Lada, M.; Canavan, K.; Fadli, Z.; Ngo, W.; Jones, L. Lipid deposition on contact lenses in symptomatic and asymptomatic contact lens wearers. Cont Lens Anterior Eye 2021, 44, 56–61. [Google Scholar] [CrossRef]
- Luensmann, D.; Jones, L. Albumin adsorption to contact lens materials: A review. Contact Lens Anterior Eye 2008, 31, 179–187. [Google Scholar] [CrossRef]
- Mession, J.L.; Assifaoui, A.; Lafarge, C.; Saurel, R.; Cayot, P. Protein aggregation induced by phase separation in a pea proteins-sodium alginate-water ternary system. Food Hydrocolloids 2012, 28, 333–343. [Google Scholar] [CrossRef]
- Omali, N.B.; Subbaraman, L.N.; Coles-Brennan, C.; Fadli, Z.; Jones, L.W. Biological and clinical implications of lysozyme deposition on soft contact lenses. Optom. Vis. Sci. 2015, 92, 750–757. [Google Scholar] [CrossRef]
- Ratner, B.D.; Bryant, S.J. Biomaterials: Where we have been and where we are going. Annu. Rev. Biomed Eng. 2004, 6, 41–75. [Google Scholar] [CrossRef]
- Chen, S.; Li, L.; Zhao, C.; Zheng, J. Surface hydration: Principles and applications toward low-fouling/nonfouling biomaterials. Polymer 2010, 51, 5283–5293. [Google Scholar] [CrossRef] [Green Version]
- Lin, W.; Klien, J. Control of surface forces through hydrated boundary layers. Curr. Opin. Colloid Interface Sci. 2019, 44, 94–106. [Google Scholar] [CrossRef]
- Hiraoka, T.; Yoshimitsu, M.; Santodomingo-Rubido, J.; Kondo, H.; Oshika, T. A novel quantitative evaluation of deposits adhered to worn orthokeratology contact lenses. Jpn J. Ophthalmol. 2021, 65, 855–863. [Google Scholar] [CrossRef]






| Artificial Tear Solution | Contact Angle (°) | |||
|---|---|---|---|---|
| 1 | 2 | 3 | Mean ± Standard Deviation | |
| Control (without polysaccharides) | 76.42 | 74.86 | 79.31 | 76.86 ± 2.26 |
| 2.25 mg/mL AA + 2.25 mg/mL CRG | 29.32 | 29.7 | 24.41 | 27.81 ± 2.95 |
| 4.5 mg/mL AA + 4.5 mg/mL CRG | 8.58 | 21.96 | 24.51 | 18.35 ± 8.56 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wu, T.-Y.; Yeh, L.-K.; Su, C.-Y.; Huang, P.-H.; Lai, C.-C.; Fang, H.-W. The Effect of Polysaccharides on Preventing Proteins and Cholesterol from Being Adsorbed on the Surface of Orthokeratology Lenses. Polymers 2022, 14, 4542. https://doi.org/10.3390/polym14214542
Wu T-Y, Yeh L-K, Su C-Y, Huang P-H, Lai C-C, Fang H-W. The Effect of Polysaccharides on Preventing Proteins and Cholesterol from Being Adsorbed on the Surface of Orthokeratology Lenses. Polymers. 2022; 14(21):4542. https://doi.org/10.3390/polym14214542
Chicago/Turabian StyleWu, Ting-Yao, Lung-Kun Yeh, Chen-Ying Su, Pin-Hsuan Huang, Chi-Chun Lai, and Hsu-Wei Fang. 2022. "The Effect of Polysaccharides on Preventing Proteins and Cholesterol from Being Adsorbed on the Surface of Orthokeratology Lenses" Polymers 14, no. 21: 4542. https://doi.org/10.3390/polym14214542
APA StyleWu, T. -Y., Yeh, L. -K., Su, C. -Y., Huang, P. -H., Lai, C. -C., & Fang, H. -W. (2022). The Effect of Polysaccharides on Preventing Proteins and Cholesterol from Being Adsorbed on the Surface of Orthokeratology Lenses. Polymers, 14(21), 4542. https://doi.org/10.3390/polym14214542