Therapeutic Efficacy of Polymeric Biomaterials in Treating Diabetic Wounds—An Upcoming Wound Healing Technology
Abstract
:1. Introduction
2. Wound Healing—Physiology
3. Wound Healing in Diabetes
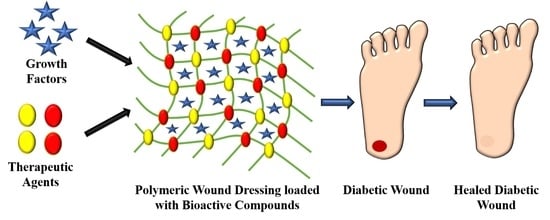
4. Types of Diabetic Wound Dressings
5. Polymeric Biomaterials
5.1. Natural Polymers
5.1.1. Collagen
5.1.2. Gelatin
5.1.3. Fibrin
5.1.4. Silk Proteins
5.2. Synthetic Polymers for Diabetic Wounds
5.2.1. Polycaprolactone (PCL)
5.2.2. Poly(vinyl alcohol) (PVA)
5.2.3. Poly(2-Hydroxyethyl Methacrylate) (pHEMA)
5.2.4. Polylactide (PLA) and Polyglycolic Acid (PGA)
6. Future Perspectives and Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Patel, S.; Srivastava, S.; Singh, M.R.; Singh, D. Mechanistic insight into diabetic wounds: Pathogenesis, molecular targets and treatment strategies to pace wound healing. Biomed. Pharmacother. 2019, 112, 108615. [Google Scholar] [CrossRef] [PubMed]
- Selle, J.J.; Aminuddin, A.; Chellappan, K. Benefit of Foot Thermogram Analysis in the Treatment of Diabetic Foot Ulcer: A Systematic Review. Biomed. Res. Ther. 2022, 9, 5029–5042. [Google Scholar] [CrossRef]
- Alven, S.; Peter, S.; Mbese, Z.; Aderibigbe, B.A. Polymer-Based Wound Dressing Materials Loaded with Bioactive Agents: Potential Materials for the Treatment of Diabetic Wounds. Polymers 2022, 14, 724. [Google Scholar] [CrossRef] [PubMed]
- Okonkwo, U.A.; DiPietro, L.A. Diabetes and Wound Angiogenesis. Int. J. Mol. Sci. 2017, 18, 1419. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Spampinato, S.F.; Caruso, G.I.; De Pasquale, R.; Sortino, M.A.; Merlo, S. The Treatment of Impaired Wound Healing in Diabetes: Looking among Old Drugs. Pharmaceuticals 2020, 13, 60. [Google Scholar] [CrossRef] [Green Version]
- Singh, S.; Young, A.; McNaught, C.-E. The physiology of wound healing. Surgery 2017, 35, 473–477. [Google Scholar] [CrossRef]
- Guo, S.; DiPietro, L.A. Factors Affecting Wound Healing. J. Dent. Res. 2010, 89, 219–229. [Google Scholar] [CrossRef]
- Subramaniam, T.; Fauzi, M.; Lokanathan, Y.; Law, J. The Role of Calcium in Wound Healing. Int. J. Mol. Sci. 2021, 22, 6486. [Google Scholar] [CrossRef]
- Gosain, A.; DiPietro, L.A. Aging and Wound Healing. World J. Surg. 2004, 28, 321–326. [Google Scholar] [CrossRef]
- Broughton, G.; Janis, J.E.; Attinger, C.E. The Basic Science of Wound Healing. Plast. Reconstr. Surg. 2006, 117, 12S–34S. [Google Scholar] [CrossRef]
- Keylock, K.T.; Vieira-Potter, V.; Wallig, M.A.; DiPietro, L.A.; Schrementi, M.; Woods, J.A. Exercise accelerates cutaneous wound healing and decreases wound inflammation in aged mice. Am. J. Physiol. Integr. Comp. Physiol. 2008, 294, R179–R184. [Google Scholar] [CrossRef]
- Krzyszczyk, P.; Schloss, R.; Palmer, A.; Berthiaume, F. The Role of Macrophages in Acute and Chronic Wound Healing and Interventions to Promote Pro-wound Healing Phenotypes. Front. Physiol. 2018, 9, 419. [Google Scholar] [CrossRef] [PubMed]
- Mosser, D.M.; Edwards, J.P. Exploring the full spectrum of macrophage activation. Nat. Rev. Immunol. 2008, 8, 958–969. [Google Scholar] [CrossRef]
- Campos, A.C.; Groth, A.K.; Branco, A.B. Assessment and nutritional aspects of wound healing. Curr. Opin. Clin. Nutr. Metab. Care 2008, 11, 281–288. [Google Scholar] [CrossRef]
- Oro, F.B.; Sikka, R.S.; Wolters, B.; Graver, R.; Boyd, J.L.; Nelson, B.J.; Swiontkowski, M. Autograft Versus Allograft: An Economic Cost Comparison of Anterior Cruciate Ligament Reconstruction. Arthrosc. J. Arthrosc. Relat. Surg. 2011, 27, 1219–1225. [Google Scholar] [CrossRef] [PubMed]
- Flynn, M.; Tooke, J. Aetiology of Diabetic Foot Ulceration: A Role for the Microcirculation? Diabet. Med. 1992, 9, 320–329. [Google Scholar] [CrossRef] [PubMed]
- Tsourdi, E.; Barthel, A.; Rietzsch, H.; Reichel, A.; Bornstein, S.R. Current Aspects in the Pathophysiology and Treatment of Chronic Wounds in Diabetes Mellitus. BioMed Res. Int. 2013, 2013, 1–6. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Burgess, J.L.; Wyant, W.A.; Abdo Abujamra, B.; Kirsner, R.S.; Jozic, I. Diabetic Wound-Healing Science. Medicina 2021, 57, 1072. [Google Scholar] [CrossRef] [PubMed]
- Okizaki, S.-I.; Ito, Y.; Hosono, K.; Oba, K.; Ohkubo, H.; Amano, H.; Shichiri, M.; Majima, M. Suppressed recruitment of alternatively activated macrophages reduces TGF-β1 and impairs wound healing in streptozotocin-induced diabetic mice. Biomed. Pharmacother. 2015, 70, 317–325. [Google Scholar] [CrossRef]
- Loots, M.A.; Kenter, S.B.; Au, F.L.; van Galen, W.; Middelkoop, E.; Bos, J.D.; Mekkes, J.R. Fibroblasts derived from chronic diabetic ulcers differ in their response to stimulation with EGF, IGF-I, bFGF and PDGF-AB compared to controls. Eur. J. Cell Biol. 2002, 81, 153–160. [Google Scholar] [CrossRef] [Green Version]
- Hilton, J.R.; Williams, D.T.; Beuker, B.; Miller, D.R.; Harding, K.G. Wound Dressings in Diabetic Foot Disease. Clin. Infect. Dis. 2004, 39, S100–S103. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gianino, E.; Miller, C.; Gilmore, J. Smart Wound Dressings for Diabetic Chronic Wounds. Bioengineering 2018, 5, 51. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sood, A.; Granick, M.S.; Tomaselli, N.L. Wound Dressings and Comparative Effectiveness Data. Adv. Wound Care 2014, 3, 511–529. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Negut, I.; Grumezescu, V.; Grumezescu, A.M. Treatment Strategies for Infected Wounds. Molecules 2018, 23, 2392. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gupta, B.; Agarwal, R.; Alam, M. Textile-Based Smart Wound Dressings. Indian J. Fibre Text. Res. 2010, 35, 174–184. [Google Scholar]
- Tavakoli, S.; Klar, A.S. Advanced Hydrogels as Wound Dressings. Biomolecules 2020, 10, 1169. [Google Scholar] [CrossRef]
- Gupta, P.; Vermani, K.; Garg, S. Hydrogels: From controlled release to pH-responsive drug delivery. Drug Discov. Today 2002, 7, 569–579. [Google Scholar] [CrossRef] [PubMed]
- Xu, S.-C.; Qin, C.-C.; Yu, M.; Dong, R.-H.; Yan, X.; Zhao, H.; Han, W.-P.; Zhang, H.-D.; Long, Y.-Z. A battery-operated portable handheld electrospinning apparatus. Nanoscale 2015, 7, 12351–12355. [Google Scholar] [CrossRef]
- Hajilou, H.; Farahpour, M.R.; Hamishehkar, H. Polycaprolactone nanofiber coated with chitosan and Gamma oryzanol functionalized as a novel wound dressing for healing infected wounds. Int. J. Biol. Macromol. 2020, 164, 2358–2369. [Google Scholar] [CrossRef]
- Mulholland, E.J.; Ali, A.; Robson, T.; Dunne, N.J.; McCarthy, H.O. Delivery of RALA/siFKBPL nanoparticles via electrospun bilayer nanofibers: An innovative angiogenic therapy for wound repair. J. Control. Release 2019, 316, 53–65. [Google Scholar] [CrossRef]
- Zhao, Y.; Qiu, Y.; Wang, H.; Chen, Y.; Jin, S.; Chen, S. Preparation of Nanofibers with Renewable Polymers and Their Application in Wound Dressing. Int. J. Polym. Sci. 2016, 2016, 1–17. [Google Scholar] [CrossRef] [Green Version]
- Liu, M.; Duan, X.P.; Li, Y.M.; Yang, D.P.; Long, Y.Z. Electrospun nanofibers for wound healing. Mater. Sci. Eng. C 2017, 76, 1413–1423. [Google Scholar] [CrossRef] [PubMed]
- Heydari, P.; Varshosaz, J.; Kharazi, A.Z.; Karbasi, S. Preparation and evaluation of poly glycerol sebacate/poly hydroxy butyrate core-shell electrospun nanofibers with sequentially release of ciprofloxacin and simvastatin in wound dressings. Polym. Adv. Technol. 2018, 29, 1795–1803. [Google Scholar] [CrossRef]
- Dhivya, S.; Padma, V.V.; Santhini, E. Wound dressings—A review. BioMedicine 2015, 5, 22. [Google Scholar] [CrossRef]
- Morgan, D. Wounds—What Should a Dressing Formulary Include? Hosp. Pharm. 2002, 9, 216–261. [Google Scholar]
- Vijayan, A.; Nanditha, C.K.; Kumar, G.S.V. ECM-mimicking nanofibrous scaffold enriched with dual growth factor carrying nanoparticles for diabetic wound healing. Nanoscale Adv. 2021, 3, 3085–3092. [Google Scholar] [CrossRef]
- Ramos-E-Silva, M.; de Castro, M.C.R. New dressings, including tissue-engineered living skin. Clin. Dermatol. 2002, 20, 715–723. [Google Scholar] [CrossRef]
- Lipsky, B.A.; Hoey, C. Topical Antimicrobial Therapy for Treating Chronic Wounds. Clin. Infect. Dis. 2009, 49, 1541–1549. [Google Scholar] [CrossRef] [Green Version]
- Matthews, K.; Stevens, H.; Auffret, A.; Humphrey, M.; Eccleston, G. Formulation, stability and thermal analysis of lyophilised wound healing wafers containing an insoluble MMP-3 inhibitor and a non-ionic surfactant. Int. J. Pharm. 2008, 356, 110–120. [Google Scholar] [CrossRef]
- Yang, X.; Liu, W.; Xi, G.; Wang, M.; Liang, B.; Shi, Y.; Feng, Y.; Ren, X.; Shi, C. Fabricating antimicrobial peptide-immobilized starch sponges for hemorrhage control and antibacterial treatment. Carbohydr. Polym. 2019, 222, 115012. [Google Scholar] [CrossRef]
- Toleubayev, M.; Dmitriyeva, M.; Kozhakhmetov, S.; Sabitova, A. Efficacy of erythropoietin for wound healing: A systematic review of the literature. Ann. Med. Surg. 2021, 65, 102287. [Google Scholar] [CrossRef] [PubMed]
- Aramwit, P. Introduction to Biomaterials for Wound Healing. In Wound Healing Biomaterials; Elsevier: Amsterdam, The Netherlands, 2016; pp. 3–38. [Google Scholar]
- Ahmed, R.; Tariq, M.; Ali, I.; Asghar, R.; Khanam, P.N.; Augustine, R.; Hasan, A. Novel electrospun chitosan/polyvinyl alcohol/zinc oxide nanofibrous mats with antibacterial and antioxidant properties for diabetic wound healing. Int. J. Biol. Macromol. 2018, 120, 385–393. [Google Scholar] [CrossRef]
- Cam, M.E.; Yildiz, S.; Alenezi, H.; Cesur, S.; Ozcan, G.S.; Erdemir, G.; Edirisinghe, U.; Akakin, D.; Kuruca, D.S.; Kabasakal, L.; et al. Evaluation of burst release and sustained release of pioglitazone-loaded fibrous mats on diabetic wound healing: An in vitro and in vivo comparison study. J. R. Soc. Interface 2020, 17, 20190712. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Almasian, A.; Najafi, F.; Eftekhari, M.; Ardekani, M.R.S.; Sharifzadeh, M.; Khanavi, M. Polyurethane/carboxymethylcellulose nanofibers containing Malva sylvestris extract for healing diabetic wounds: Preparation, characterization, in vitro and in vivo studies. Mater. Sci. Eng. C 2020, 114, 111039. [Google Scholar] [CrossRef]
- Chen, X.; Zhou, W.; Zha, K.; Liu, G.; Yang, S.; Ye, S.; Liu, Y.; Xiong, Y.; Wu, Y.; Cao, F. Treatment of chronic ulcer in diabetic rats with self assembling nanofiber gel encapsulated-polydeoxyribonucleotide. Am. J. Transl. Res. 2016, 8, 3067–3076. [Google Scholar] [PubMed]
- Choi, J.S.; Leong, K.W.; Yoo, H.S. In vivo wound healing of diabetic ulcers using electrospun nanofibers immobilized with human epidermal growth factor (EGF). Biomaterials 2008, 29, 587–596. [Google Scholar] [CrossRef] [PubMed]
- Cui, S.; Sun, X.; Li, K.; Gou, D.; Zhou, Y.; Hu, J.; Liu, Y. Polylactide nanofibers delivering doxycycline for chronic wound treatment. Mater. Sci. Eng. C 2019, 104, 109745. [Google Scholar] [CrossRef]
- Grip, J.; Engstad, R.E.; Skjæveland, I.; Škalko-Basnet, N.; Isaksson, J.; Basnet, P.; Holsæter, A.M. Beta-glucan-loaded nanofiber dressing improves wound healing in diabetic mice. Eur. J. Pharm. Sci. 2018, 121, 269–280. [Google Scholar] [CrossRef] [Green Version]
- Kanji, S.; Das, M.; Joseph, M.; Aggarwal, R.; Sharma, S.M.; Ostrowski, M.; Pompili, V.J.; Mao, H.-Q.; Das, H. Nanofiber-expanded human CD34+ cells heal cutaneous wounds in streptozotocin-induced diabetic mice. Sci. Rep. 2019, 9, 8415. [Google Scholar] [CrossRef] [Green Version]
- Lee, C.-H.; Liu, K.-S.; Cheng, C.-W.; Chan, E.-C.; Hung, K.-C.; Hsieh, M.-J.; Chang, S.-H.; Fu, X.; Juang, J.-H.; Hsieh, I.-C.; et al. Codelivery of Sustainable Antimicrobial Agents and Platelet-Derived Growth Factor via Biodegradable Nanofibers for Repair of Diabetic Infectious Wounds. ACS Infect. Dis. 2020, 6, 2688–2697. [Google Scholar] [CrossRef]
- Lee, C.-H.; Hung, K.-C.; Hsieh, M.-J.; Chang, S.-H.; Juang, J.-H.; Hsieh, I.-C.; Wen, M.-S.; Liu, S.-J. Core-shell insulin-loaded nanofibrous scaffolds for repairing diabetic wounds. Nanomedicine 2020, 24, 102123. [Google Scholar] [CrossRef]
- Merrell, J.G.; McLaughlin, S.W.; Tie, L.; Laurencin, C.T.; Chen, A.F.; Nair, L.S. Curcumin loaded poly (ε-caprolactone) nanofibers: Diabetic wound dressing with antioxidant and anti-inflammatory properties. Clin. Exp. Pharmacol. Physiol. 2009, 36, 1149–1156. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- García, A.D.P.; Cassini-Vieira, P.; Ribeiro, C.C.; Jensen, C.E.D.M.; Barcelos, L.S.; Cortes, M.E.; Sinisterra, R.D. Efficient cutaneous wound healing using bixin-loaded PCL nanofibers in diabetic mice. J. Biomed. Mater. Res. Part B Appl. Biomater. 2017, 105, 1938–1949. [Google Scholar] [CrossRef] [PubMed]
- Ranjbar-Mohammadi, M.; Rabbani, S.; Bahrami, S.H.; Joghataei, M.; Moayer, F. Antibacterial performance and in vivo diabetic wound healing of curcumin loaded gum tragacanth/poly(ε-caprolactone) electrospun nanofibers. Mater. Sci. Eng. C 2016, 69, 1183–1191. [Google Scholar] [CrossRef] [PubMed]
- Shalaby, T.; Fekry, N.M.; El Sodfy, A.S.; Elsheredy, A.; Moustafa, M.E.S.S.A. Preparation and characterisation of antibacterial silver-containing nanofibers for wound healing in diabetic mice. Int. J. Nanoparticles 2015, 8, 82. [Google Scholar] [CrossRef]
- Zehra, M.; Zubairi, W.; Hasan, A.; Butt, H.; Ramzan, A.; Azam, M.; Mehmood, A.; Falahati, M.; Chaudhry, A.A.; Rehman, I.U.; et al. Oxygen Generating Polymeric Nano Fibers That Stimulate Angiogenesis and Show Efficient Wound Healing in a Diabetic Wound Model. Int. J. Nanomed. 2020, 15, 3511–3522. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.-H.; Chang, S.-H.; Chen, W.-J.; Hung, K.-C.; Lin, Y.-H.; Liu, S.-J.; Hsieh, M.-J.; Pang, J.-H.S.; Juang, J.-H. Augmentation of diabetic wound healing and enhancement of collagen content using nanofibrous glucophage-loaded collagen/PLGA scaffold membranes. J. Colloid Interface Sci. 2015, 439, 88–97. [Google Scholar] [CrossRef]
- Zheng, Z.; Liu, Y.; Huang, W.; Mo, Y.; Lan, Y.; Guo, R.; Cheng, B. Neurotensin-loaded PLGA/CNC composite nanofiber membranes accelerate diabetic wound healing. Artif. Cells, Nanomed. Biotechnol. 2018, 46, 493–501. [Google Scholar] [CrossRef] [Green Version]
- Liu, F.; Li, X.; Wang, L.; Yan, X.; Ma, D.; Liu, Z.; Liu, X. Sesamol incorporated cellulose acetate-zein composite nanofiber membrane: An efficient strategy to accelerate diabetic wound healing. Int. J. Biol. Macromol. 2020, 149, 627–638. [Google Scholar] [CrossRef]
- Lee, C.-H.; Hsieh, M.-J.; Chang, S.-H.; Lin, Y.-H.; Liu, S.-J.; Lin, T.-Y.; Hung, K.-C.; Pang, J.-H.S.; Juang, J.-H. Enhancement of Diabetic Wound Repair Using Biodegradable Nanofibrous Metformin-Eluting Membranes: In Vitro and in Vivo. ACS Appl. Mater. Interfaces 2014, 6, 3979–3986. [Google Scholar] [CrossRef]
- Ren, X.; Han, Y.; Wang, J.; Jiang, Y.; Yi, Z.; Xu, H.; Ke, Q. An aligned porous electrospun fibrous membrane with controlled drug delivery—An efficient strategy to accelerate diabetic wound healing with improved angiogenesis. Acta Biomater. 2018, 70, 140–153. [Google Scholar] [CrossRef] [PubMed]
- Lobmann, R.; Pittasch, D.; Mühlen, I.; Lehnert, H. Autologous human keratinocytes cultured on membranes composed of benzyl ester of hyaluronic acid for grafting in nonhealing diabetic foot lesions. J. Diabetes Its Complicat. 2003, 17, 199–204. [Google Scholar] [CrossRef] [PubMed]
- Augustine, R.; Hasan, A.; Patan, N.K.; Dalvi, Y.B.; Varghese, R.; Antony, A.; Unni, R.N.; Sandhyarani, N.; Al Moustafa, A.-E. Cerium Oxide Nanoparticle Incorporated Electrospun Poly(3-hydroxybutyrate-co-3-hydroxyvalerate) Membranes for Diabetic Wound Healing Applications. ACS Biomater. Sci. Eng. 2020, 6, 58–70. [Google Scholar] [CrossRef] [PubMed]
- Augustine, R.; Zahid, A.A.; Hasan, A.; Wang, M.; Webster, T.J. CTGF Loaded Electrospun Dual Porous Core-Shell Membrane for Diabetic Wound Healing. Int. J. Nanomed. 2019, 14, 8573–8588. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Arantes, V.T.; Faraco, A.A.; Ferreira, F.B.; Oliveira, C.A.; Martins-Santos, E.; Cassini-Vieira, P.; Barcelos, L.S.; Ferreira, L.A.; Goulart, G.A. Retinoic acid-loaded solid lipid nanoparticles surrounded by chitosan film support diabetic wound healing in in vivo study. Colloids Surf. B Biointerfaces 2020, 188, 110749. [Google Scholar] [CrossRef]
- Arul, V.; Kartha, R.; Jayakumar, R. A therapeutic approach for diabetic wound healing using biotinylated GHK incorporated collagen matrices. Life Sci. 2007, 80, 275–284. [Google Scholar] [CrossRef]
- Inpanya, P.; Faikrua, A.; Ounaroon, A.; Sittichokechaiwut, A.; Viyoch, J. Effects of the blended fibroin/aloe gel film on wound healing in streptozotocin-induced diabetic rats. Biomed. Mater. 2012, 7, 035008. [Google Scholar] [CrossRef]
- Kim, D.W.; Kim, K.S.; Seo, Y.G.; Lee, B.-J.; Park, Y.J.; Youn, Y.S.; Kim, J.O.; Yong, C.S.; Jin, S.G.; Choi, H.-G. Novel sodium fusidate-loaded film-forming hydrogel with easy application and excellent wound healing. Int. J. Pharm. 2015, 495, 67–74. [Google Scholar] [CrossRef]
- Mizuno, K.; Yamamura, K.; Yano, K.; Osada, T.; Saeki, S.; Takimoto, N.; Sakurai, T.; Nimura, Y. Effect of chitosan film containing basic fibroblast growth factor on wound healing in genetically diabetic mice. J. Biomed. Mater. Res. 2003, 64, 177–181. [Google Scholar] [CrossRef]
- Song, S.H.; Kim, J.E.; Koh, E.K.; Sung, J.E.; Lee, H.A.; Yun, W.B.; Hong, J.T.; Hwang, D.Y. Selenium-loaded cellulose film derived from Styela clava tunic accelerates the healing process of cutaneous wounds in streptozotocin-induced diabetic Sprague–Dawley rats. J. Dermatol. Treat. 2018, 29, 606–616. [Google Scholar] [CrossRef]
- Tan, W.S.; Arulselvan, P.; Ng, S.-F.; Taib, C.N.M.; Sarian, M.N.; Fakurazi, S. Improvement of diabetic wound healing by topical application of Vicenin-2 hydrocolloid film on Sprague Dawley rats. BMC Complement. Altern. Med. 2019, 19, 20. [Google Scholar] [CrossRef] [PubMed]
- Tong, W.Y.; bin Abdullah, A.Y.K.; binti Rozman, N.A.S.; bin Wahid, M.I.A.; Hossain, M.; Ring, L.C.; Lazim, Y.; Tan, W.-N. Antimicrobial wound dressing film utilizing cellulose nanocrystal as drug delivery system for curcumin. Cellulose 2018, 25, 631–638. [Google Scholar] [CrossRef]
- Voss, G.T.; Gularte, M.S.; Vogt, A.G.; Giongo, J.L.; Vaucher, R.A.; Echenique, J.V.; Soares, M.P.; Luchese, C.; Wilhelm, E.A.; Fajardo, A.R. Polysaccharide-based film loaded with vitamin C and propolis: A promising device to accelerate diabetic wound healing. Int. J. Pharm. 2018, 552, 340–351. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.-Y.; Jiao, Y.-P.; Xiao, L.-L.; Li, M.-M.; Liu, H.-W.; Li, S.-H.; Liao, X.; Chen, Y.-T.; Li, J.-X.; Zhang, Y. Experimental Study on Effects of Adipose-Derived Stem Cell–Seeded Silk Fibroin Chitosan Film on Wound Healing of a Diabetic Rat Model. Ann. Plast. Surg. 2018, 80, 572–580. [Google Scholar] [CrossRef] [Green Version]
- da Silva, L.P.; Santos, T.C.; Rodrigues, D.B.; Pirraco, R.P.; Cerqueira, M.T.; Reis, R.L.; Correlo, V.M.; Marques, A.P. Stem Cell-Containing Hyaluronic Acid-Based Spongy Hydrogels for Integrated Diabetic Wound Healing. J. Investig. Dermatol. 2017, 137, 1541–1551. [Google Scholar] [CrossRef] [Green Version]
- Lai, J.C.-Y.; Lai, H.-Y.; Rao, N.K.; Ng, S.-F. Treatment for diabetic ulcer wounds using a fern tannin optimized hydrogel formulation with antibacterial and antioxidative properties. J. Ethnopharmacol. 2016, 189, 277–289. [Google Scholar] [CrossRef]
- Li, M.; Ke, Q.-F.; Tao, S.-C.; Guo, S.-C.; Rui, B.-Y.; Guo, Y.-P. Fabrication of hydroxyapatite/chitosan composite hydrogels loaded with exosomes derived from miR-126-3p overexpressed synovial mesenchymal stem cells for diabetic chronic wound healing. J. Mater. Chem. B 2016, 4, 6830–6841. [Google Scholar] [CrossRef]
- Masood, N.; Ahmed, R.; Tariq, M.; Ahmed, Z.; Masoud, M.S.; Ali, I.; Asghar, R.; Andleeb, A.; Hasan, A. Silver nanoparticle impregnated chitosan-PEG hydrogel enhances wound healing in diabetes induced rabbits. Int. J. Pharm. 2019, 559, 23–36. [Google Scholar] [CrossRef]
- Shi, G.; Chen, W.; Zhang, Y.; Dai, X.; Zhang, X.; Wu, Z. An Antifouling Hydrogel Containing Silver Nanoparticles for Modulating the Therapeutic Immune Response in Chronic Wound Healing. Langmuir 2019, 35, 1837–1845. [Google Scholar] [CrossRef]
- Thangavel, P.; Ramachandran, B.; Chakraborty, S.; Kannan, R.; Lonchin, S.; Muthuvijayan, V. Accelerated Healing of Diabetic Wounds Treated with L-Glutamic acid Loaded Hydrogels Through Enhanced Collagen Deposition and Angiogenesis: An In Vivo Study. Sci. Rep. 2017, 7, 10701. [Google Scholar] [CrossRef] [Green Version]
- Zhang, L.; Ma, Y.; Pan, X.; Chen, S.; Zhuang, H.; Wang, S. A composite hydrogel of chitosan/heparin/poly (γ-glutamic acid) loaded with superoxide dismutase for wound healing. Carbohydr. Polym. 2018, 180, 168–174. [Google Scholar] [CrossRef] [PubMed]
- Choi, H.J.; Thambi, T.; Yang, Y.H.; Bang, S.I.; Kim, B.S.; Pyun, D.G.; Lee, D.S. AgNP and rhEGF-incorporating synergistic polyurethane foam as a dressing material for scar-free healing of diabetic wounds. RSC Adv. 2017, 7, 13714–13725. [Google Scholar] [CrossRef] [Green Version]
- Pyun, D.G.; Choi, H.J.; Yoon, H.S.; Thambi, T.; Lee, D.S. Polyurethane foam containing rhEGF as a dressing material for healing diabetic wounds: Synthesis, characterization, in vitro and in vivo studies. Colloids Surfaces B Biointerfaces 2015, 135, 699–706. [Google Scholar] [CrossRef] [PubMed]
- Atia, N.M.; Hazzah, H.A.; Gaafar, P.M.; Abdallah, O.Y. Diosmin Nanocrystal–Loaded Wafers for Treatment of Diabetic Ulcer: In Vitro and In Vivo Evaluation. J. Pharm. Sci. 2019, 108, 1857–1871. [Google Scholar] [CrossRef] [PubMed]
- Anisha, B.; Biswas, R.; Chennazhi, K.; Jayakumar, R. Chitosan–hyaluronic acid/nano silver composite sponges for drug resistant bacteria infected diabetic wounds. Int. J. Biol. Macromol. 2013, 62, 310–320. [Google Scholar] [CrossRef]
- Lipsky, B.A.; Kuss, M.; Edmonds, M.; Reyzelman, A.; Sigal, F. Topical Application of a Gentamicin-Collagen Sponge Combined with Systemic Antibiotic Therapy for the Treatment of Diabetic Foot Infections of Moderate Severity. J. Am. Podiatr. Med. Assoc. 2012, 102, 223–232. [Google Scholar] [CrossRef]
- Mohandas, A.; Anisha, B.; Chennazhi, K.; Jayakumar, R. Chitosan–hyaluronic acid/VEGF loaded fibrin nanoparticles composite sponges for enhancing angiogenesis in wounds. Colloids Surfaces B Biointerfaces 2015, 127, 105–113. [Google Scholar] [CrossRef]
- Shi, Q.; Qian, Z.; Liu, D.; Sun, J.; Wang, X.; Liu, H.; Xu, J.; Guo, X. GMSC-Derived Exosomes Combined with a Chitosan/Silk Hydrogel Sponge Accelerates Wound Healing in a Diabetic Rat Skin Defect Model. Front. Physiol. 2017, 8, 904. [Google Scholar] [CrossRef]
- Wang, W.; Lin, S.; Xiao, Y.; Huang, Y.; Tan, Y.; Cai, L.; Li, X. Acceleration of diabetic wound healing with chitosan-crosslinked collagen sponge containing recombinant human acidic fibroblast growth factor in healing-impaired STZ diabetic rats. Life Sci. 2008, 82, 190–204. [Google Scholar] [CrossRef]
- Xia, G.; Zhai, D.; Sun, Y.; Hou, L.; Guo, X.; Wang, L.; Li, Z.; Wang, F. Preparation of a novel asymmetric wettable chitosan-based sponge and its role in promoting chronic wound healing. Carbohydr. Polym. 2020, 227, 115296. [Google Scholar] [CrossRef]
- Kondo, S.; Niiyama, H.; Yu, A.; Kuroyanagi, Y. Evaluation of a Wound Dressing Composed of Hyaluronic Acid and Collagen Sponge Containing Epidermal Growth Factor in Diabetic Mice. J. Biomater. Sci. Polym. Ed. 2012, 23, 1729–1740. [Google Scholar] [CrossRef]
- Thattaruparambil Raveendran, N.; Mohandas, A.; Ramachandran Menon, R.; Somasekharan Menon, A.; Biswas, R.; Jayakumar, R. Ciprofloxacin- and Fluconazole-Containing Fibrin-Nanoparticle-Incorporated Chitosan Bandages for the Treatment of Polymicrobial Wound Infections. ACS Appl. Bio Mater. 2019, 2, 243–254. [Google Scholar] [CrossRef] [PubMed]
- Mohanty, C.; Pradhan, J. A human epidermal growth factor-curcumin bandage bioconjugate loaded with mesenchymal stem cell for in vivo diabetic wound healing. Mater. Sci. Eng. C 2020, 111, 110751. [Google Scholar] [CrossRef] [PubMed]
- Kumar, P.T.S.; Lakshmanan, V.-K.; Anilkumar, T.; Ramya, C.; Reshmi, P.; Unnikrishnan, A.; Nair, S.V.; Jayakumar, R. Flexible and Microporous Chitosan Hydrogel/Nano ZnO Composite Bandages for Wound Dressing: In Vitro and In Vivo Evaluation. ACS Appl. Mater. Interfaces 2012, 4, 2618–2629. [Google Scholar] [CrossRef]
- Kahan, V.; Andersen, M.; Tomimori, J.; Tufik, S. Stress, immunity and skin collagen integrity: Evidence from animal models and clinical conditions. Brain Behav. Immun. 2009, 23, 1089–1095. [Google Scholar] [CrossRef] [PubMed]
- Shoulders, M.D.; Raines, R.T. Collagen Structure and Stability. Annu. Rev. Biochem. 2009, 78, 929–958. [Google Scholar] [CrossRef] [Green Version]
- Naomi, R.; Fauzi, M.B. Cellulose/Collagen Dressings for Diabetic Foot Ulcer: A Review. Pharmaceutics 2020, 12, 881. [Google Scholar] [CrossRef]
- Davison-Kotler, E.; Marshall, W.S.; García-Gareta, E. Sources of Collagen for Biomaterials in Skin Wound Healing. Bioengineering 2019, 6, 56. [Google Scholar] [CrossRef] [Green Version]
- Ruszczak, Z. Effect of collagen matrices on dermal wound healing. Adv. Drug Deliv. Rev. 2003, 55, 1595–1611. [Google Scholar] [CrossRef]
- Chen, F.-M.; Liu, X. Advancing biomaterials of human origin for tissue engineering. Prog. Polym. Sci. 2016, 53, 86–168. [Google Scholar] [CrossRef] [Green Version]
- Sorushanova, A.; Delgado, L.M.; Wu, Z.; Shologu, N.; Kshirsagar, A.; Raghunath, R.; Mullen, A.M.; Bayon, Y.; Pandit, A.; Raghunath, M.; et al. The Collagen Suprafamily: From Biosynthesis to Advanced Biomaterial Development. Adv. Mater. 2019, 31, 1801651. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ricard-Blum, S. The Collagen Family. Cold Spring Harb. Perspect. Biol. 2011, 3, a004978. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Parenteau-Bareil, R.; Gauvin, R.; Berthod, F. Collagen-Based Biomaterials for Tissue Engineering Applications. Materials 2010, 3, 1863–1887. [Google Scholar] [CrossRef] [Green Version]
- Brodsky, B.; Eikenberry, E.F. [5] Characterization of Fibrous Forms of Collagen. In Methods in Enzymology; Academic Press: Cambridge, MA, USA, 1982; pp. 127–174. [Google Scholar]
- Haut, R.C. Age-Dependent Influence of Strain Rate on the Tensile Failure of Rat-Tail Tendon. J. Biomech. Eng. 1983, 105, 296–299. [Google Scholar] [CrossRef]
- Ferraro, V.; Gaillard-Martinie, B.; Sayd, T.; Chambon, C.; Anton, M.; Santé-Lhoutellier, V. Collagen type I from bovine bone. Effect of animal age, bone anatomy and drying methodology on extraction yield, self-assembly, thermal behaviour and electrokinetic potential. Int. J. Biol. Macromol. 2017, 97, 55–66. [Google Scholar] [CrossRef]
- Asghar, A.; Henrickson, R.L. Chemical, Biochemical, Functional, and Nutritional Characteristics of Collagen in Food Systems. In Advances in Food Research; Elsevier: Amsterdam, The Netherlands, 1982; pp. 231–372. [Google Scholar]
- Nehrer, S. Chondrocyte-seeded collagen matrices implanted in a chondral defect in a canine model. Biomaterials 1998, 19, 2313–2328. [Google Scholar] [CrossRef]
- Geesin, J.C.; Brown, L.J.; Liu, Z.; Berg, R.A. Development of a Skin Model Based on Insoluble Fibrillar Collagen. J. Biomed. Mater. Res. 1996, 33, 1–8. [Google Scholar] [CrossRef]
- Doillon, C.J.; Silver, F.H.; Berg, R.A. Fibroblast growth on a porous collagen sponge containing hyaluronic acid and fibronectin. Biomaterials 1987, 8, 195–200. [Google Scholar] [CrossRef]
- Rovira, A.; Amedee, J.; Bareille, R.; Rabaud, M. Colonization of a calcium phosphate/ elastin-solubilized peptide-collagen composite material by human osteoblasts. Biomaterials 1996, 17, 1535–1540. [Google Scholar] [CrossRef]
- Leipziger, L.S.; Glushko, V.; DiBernardo, B.; Shafaie, F.; Noble, J.; Nichols, J.; Alvarez, O.M. Dermal wound repair: Role of collagen matrix implants and synthetic polymer dressings. J. Am. Acad. Dermatol. 1985, 12, 409–419. [Google Scholar] [CrossRef]
- McPherson, J.M.; Sawamura, S.; Armstrong, R. An examination of the biologic response to injectable, glutaraldehyde cross-linked collagen implants. J. Biomed. Mater. Res. 1986, 20, 93–107. [Google Scholar] [CrossRef] [PubMed]
- Gerrits, L.; Hammink, R.; Kouwer, P.H.J. Semiflexible polymer scaffolds: An overview of conjugation strategies. Polym. Chem. 2021, 12, 1362–1392. [Google Scholar] [CrossRef]
- Chattopadhyay, S.; Raines, R.T. Collagen-based biomaterials for wound healing. Biopolymers 2014, 101, 821–833. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zaulyanov, L.; Kirsner, R.S. A review of a bi-layered living cell treatment (Apligraf) in the treatment of venous leg ulcers and diabetic foot ulcers. Clin. Interv. Aging 2007, 2, 93–98. [Google Scholar] [CrossRef] [PubMed]
- Rennert, R.C.; Rodrigues, M.; Wong, V.W.; Duscher, D.; Hu, M.; Maan, Z.; Sorkin, M.; Gurtner, G.C.; Longaker, M.T. Biological therapies for the treatment of cutaneous wounds: Phase III and launched therapies. Expert Opin. Biol. Ther. 2013, 13, 1523–1541. [Google Scholar] [CrossRef]
- Munish, T.; Ramneesh, G.; Sanjeev, S.; Jasdeep, S.; Jaspal, S.; Nikhil, G. Comparative Study of Collagen Based Dressing and Standard Dressing in Diabetic Foot Ulcer. J. Evol. Med. Dent. Sci. 2015, 4, 3614–3621. [Google Scholar] [CrossRef]
- Lee, D.S.; Lee, Y.N.; Han, S.K.; Namgoong, S. Effect of Collagen Dressing on Diabetic Wound Healing-A Pilot Study. J. Korean Wound Manag. Soc. 2015, 11, 1–10. [Google Scholar]
- Hauck, S.; Zager, P.; Halfter, N.; Wandel, E.; Torregrossa, M.; Kakpenova, A.; Rother, S.; Ordieres, M.; Räthel, S.; Berg, A.; et al. Collagen/hyaluronan based hydrogels releasing sulfated hyaluronan improve dermal wound healing in diabetic mice via reducing inflammatory macrophage activity. Bioact. Mater. 2021, 6, 4342–4359. [Google Scholar] [CrossRef]
- Shagdarova, B.; Konovalova, M.; Zhuikova, Y.; Lunkov, A.; Zhuikov, V.; Khaydapova, D.; Il’Ina, A.; Svirshchevskaya, E.; Varlamov, V. Collagen/Chitosan Gels Cross-Linked with Genipin for Wound Healing in Mice with Induced Diabetes. Materials 2021, 15, 15. [Google Scholar] [CrossRef]
- Michelacci, Y.M. Collagens and proteoglycans of the corneal extracellular matrix. Braz. J. Med. Biol. Res. 2003, 36, 1037–1046. [Google Scholar] [CrossRef] [Green Version]
- Duconseille, A.; Astruc, T.; Quintana, N.; Meersman, F.; Sante-Lhoutellier, V. Gelatin structure and composition linked to hard capsule dissolution: A review. Food Hydrocoll. 2015, 43, 360–376. [Google Scholar] [CrossRef]
- Rodríguez-Rodríguez, R.; Espinosa-Andrews, H.; Velasquillo-Martínez, C.; García-Carvajal, Z.Y. Composite Hydrogels based on gelatin, chitosan and polyvinyl alcohol to biomedical applications: A review. Int. J. Polym. Mater. Polym. Biomater. 2020, 69, 1–20. [Google Scholar] [CrossRef]
- Samadian, H.; Zamiri, S.; Ehterami, A.; Farzamfar, S.; Vaez, A.; Khastar, H.; Alam, M.; Ai, A.; Derakhshankhah, H.; Allahyari, Z.; et al. Electrospun cellulose acetate/gelatin nanofibrous wound dressing containing berberine for diabetic foot ulcer healing: In vitro and in vivo studies. Sci. Rep. 2020, 10, 8312. [Google Scholar] [CrossRef]
- Yu, H.; Gong, W.; Mei, J.; Qin, L.; Piao, Z.; You, D.; Gu, W.; Jia, Z. The efficacy of a paeoniflorin-sodium alginate-gelatin skin scaffold for the treatment of diabetic wound: An in vivo study in a rat model. Biomed. Pharmacother. 2022, 151, 113165. [Google Scholar] [CrossRef] [PubMed]
- Sadeghi, A.; Zare-Gachi, M.; Najjar-Asl, M.; Rajabi, S.; Fatemi, M.J.; Forghani, S.F.; Daemi, H.; Pezeshki-Modaress, M. Hybrid gelatin-sulfated alginate scaffolds as dermal substitutes can dramatically accelerate healing of full-thickness diabetic wounds. Carbohydr. Polym. 2023, 302, 120404. [Google Scholar] [CrossRef] [PubMed]
- Zheng, Y.; Yuan, W.; Liu, H.; Huang, S.; Bian, L.; Guo, R. Injectable supramolecular gelatin hydrogel loading of resveratrol and histatin-1 for burn wound therapy. Biomater. Sci. 2020, 8, 4810–4820. [Google Scholar] [CrossRef] [PubMed]
- Wolberg, A.S. Thrombin generation and fibrin clot structure. Blood Rev. 2007, 21, 131–142. [Google Scholar] [CrossRef]
- Uzunalli, G. Nanomaterials for Wound Healing. In Nanomaterials for Regenerative Medicine; Humana: Cham, Switzerland, 2019; pp. 81–117. [Google Scholar]
- Heher, P.; Mühleder, S.; Mittermayr, R.; Redl, H.; Slezak, P. Fibrin-based delivery strategies for acute and chronic wound healing. Adv. Drug Deliv. Rev. 2018, 129, 134–147. [Google Scholar] [CrossRef]
- Losi, P.; Briganti, E.; Errico, C.; Lisella, A.; Sanguinetti, E.; Chiellini, F.; Soldani, G. Fibrin-based scaffold incorporating VEGF- and bFGF-loaded nanoparticles stimulates wound healing in diabetic mice. Acta Biomater. 2013, 9, 7814–7821. [Google Scholar] [CrossRef]
- Al Kayal, T.; Losi, P.; Pierozzi, S.; Soldani, G. A New Method for Fibrin-Based Electrospun/Sprayed Scaffold Fabrication. Sci. Rep. 2020, 10, 5111. [Google Scholar] [CrossRef] [Green Version]
- Geer, D.J.; Swartz, D.D.; Andreadis, S.T. Fibrin Promotes Migration in a Three-Dimensional in Vitro Model of Wound Regeneration. Tissue Eng. 2002, 8, 787–798. [Google Scholar] [CrossRef] [PubMed]
- Falanga, V.; Iwamoto, S.; Chartier, M.; Yufit, T.; Butmarc, J.; Kouttab, N.; Shrayer, D.; Carson, P. Autologous Bone Marrow–Derived Cultured Mesenchymal Stem Cells Delivered in a Fibrin Spray Accelerate Healing in Murine and Human Cutaneous Wounds. Tissue Eng. 2007, 13, 1299–1312. [Google Scholar] [CrossRef]
- Crisci, A.; Marotta, G.; Licito, A.; Serra, E.; Benincasa, G.; Crisci, M. Use of Leukocyte Platelet (L-PRF) Rich Fibrin in Diabetic Foot Ulcer with Osteomyelitis (Three Clinical Cases Report). Diseases 2018, 6, 30. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Losi, P.; Al Kayal, T.; Buscemi, M.; Foffa, I.; Cavallo, A.; Soldani, G. Bilayered Fibrin-Based Electrospun-Sprayed Scaffold Loaded with Platelet Lysate Enhances Wound Healing in a Diabetic Mouse Model. Nanomaterials 2020, 10, 2128. [Google Scholar] [CrossRef] [PubMed]
- Chouhan, D.; Mandal, B.B. Silk biomaterials in wound healing and skin regeneration therapeutics: From bench to bedside. Acta Biomater. 2020, 103, 24–51. [Google Scholar] [CrossRef]
- Altman, G.H.; Diaz, F.; Jakuba, C.; Calabro, T.; Horan, R.L.; Chen, J.; Lu, H.; Richmond, J.; Kaplan, D.L. Silk-based biomaterials. Biomaterials 2003, 24, 401–416. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Park, Y.R.; Sultan, T.; Park, H.J.; Lee, J.M.; Ju, H.W.; Lee, O.J.; Lee, D.J.; Kaplan, D.L.; Park, C.H. NF-κB signaling is key in the wound healing processes of silk fibroin. Acta Biomater. 2018, 67, 183–195. [Google Scholar] [CrossRef]
- Capar, G.; Aygun, S.S.; Gecit, M.R. Separation of sericin from fatty acids towards its recovery from silk degumming wastewaters. J. Membr. Sci. 2009, 342, 179–189. [Google Scholar] [CrossRef]
- Tariq, M.; Tahir, H.M.; Butt, S.A.; Ali, S.; Ahmad, A.B.; Raza, C.; Summer, M.; Hassan, A.; Nadeem, J. Silk derived formulations for accelerated wound healing in diabetic mice. Peerj 2021, 9, e10232. [Google Scholar] [CrossRef]
- Sultan, M.T.; Lee, O.J.; Kim, S.H.; Ju, H.W.; Park, C.H. Silk Fibroin in Wound Healing Process. In Novel Biomaterials for Regenerative Medicine; Springer: Singapore, 2018; pp. 115–126. [Google Scholar]
- Liu, J.; Yan, L.; Yang, W.; Lan, Y.; Zhu, Q.; Xu, H.; Zheng, C.; Guo, R. Controlled-release neurotensin-loaded silk fibroin dressings improve wound healing in diabetic rat model. Bioact. Mater. 2019, 4, 151–159. [Google Scholar] [CrossRef]
- Guan, G.; Zhang, Q.; Jiang, Z.; Liu, J.; Wan, J.; Jin, P.; Lv, Q. Multifunctional Silk Fibroin Methacryloyl Microneedle for Diabetic Wound Healing. Small 2022, 18, 2203064. [Google Scholar] [CrossRef] [PubMed]
- Xu, X.; Wang, X.; Qin, C.; Khan, A.U.R.; Zhang, W.; Mo, X. Silk fibroin/poly-(L-lactide-co-caprolactone) nanofiber scaffolds loaded with Huangbai Liniment to accelerate diabetic wound healing. Colloids Surfaces B Biointerfaces 2021, 199, 111557. [Google Scholar] [CrossRef] [PubMed]
- Baptista-Silva, S.; Bernardes, B.G.; Borges, S.; Rodrigues, I.; Fernandes, R.; Gomes-Guerreiro, S.; Pinto, M.T.; Pintado, M.; Soares, R.; Costa, R.; et al. Exploring Silk Sericin for Diabetic Wounds: An In Situ-Forming Hydrogel to Protect against Oxidative Stress and Improve Tissue Healing and Regeneration. Biomolecules 2022, 12, 801. [Google Scholar] [CrossRef] [PubMed]
- El-Samad, L.M.; Hassan, M.A.; Basha, A.A.; El-Ashram, S.; Radwan, E.H.; Aziz, K.K.A.; Tamer, T.M.; Augustyniak, M.; El Wakil, A. Carboxymethyl cellulose/sericin-based hydrogels with intrinsic antibacterial, antioxidant, and anti-inflammatory properties promote re-epithelization of diabetic wounds in rats. Int. J. Pharm. 2022, 629, 122328. [Google Scholar] [CrossRef]
- Alven, S.; Nqoro, X.; Aderibigbe, B.A. Polymer-Based Materials Loaded with Curcumin for Wound Healing Applications. Polymers 2020, 12, 2286. [Google Scholar] [CrossRef]
- Mir, M.; Ali, M.N.; Barakullah, A.; Gulzar, A.; Arshad, M.; Fatima, S.; Asad, M. Synthetic polymeric biomaterials for wound healing: A review. Prog. Biomater. 2018, 7, 1–21. [Google Scholar] [CrossRef] [Green Version]
- Mondal, D.; Griffith, M.; Venkatraman, S.S. Polycaprolactone-based biomaterials for tissue engineering and drug delivery: Current scenario and challenges. Int. J. Polym. Mater. Polym. Biomater. 2016, 65, 255–265. [Google Scholar] [CrossRef]
- Huang, X.; Wang, Q.; Mao, R.; Wang, Z.; Shen, S.G.; Mou, J.; Dai, J. Two-dimensional nanovermiculite and polycaprolactone electrospun fibers composite scaffolds promoting diabetic wound healing. J. Nanobiotechnology 2022, 20, 343. [Google Scholar] [CrossRef]
- Lv, F.; Wang, J.; Xu, P.; Han, Y.; Ma, H.; Xu, H.; Chen, S.; Chang, J.; Ke, Q.; Liu, M.; et al. A conducive bioceramic/polymer composite biomaterial for diabetic wound healing. Acta Biomater. 2017, 60, 128–143. [Google Scholar] [CrossRef]
- Awasthi, A.; Gulati, M.; Kumar, B.; Kaur, J.; Vishwas, S.; Khursheed, R.; Porwal, O.; Alam, A.; Kr, A.; Corrie, L.; et al. Recent Progress in Development of Dressings Used for Diabetic Wounds with Special Emphasis on Scaffolds. BioMed Res. Int. 2022, 2022, 1–43. [Google Scholar] [CrossRef]
- Huang, X.; Guan, N.; Li, Q. A Marine-Derived Anti-Inflammatory Scaffold for Accelerating Skin Repair in Diabetic Mice. Mar. Drugs 2021, 19, 496. [Google Scholar] [CrossRef]
- Lin, W.-C.; Tang, C.-M. Evaluation of Polyvinyl Alcohol/Cobalt Substituted Hydroxyapatite Nanocomposite as a Potential Wound Dressing for Diabetic Foot Ulcers. Int. J. Mol. Sci. 2020, 21, 8831. [Google Scholar] [CrossRef]
- Zhu, H.; Xu, J.; Zhao, M.; Luo, H.; Lin, M.; Luo, Y.; Li, Y.; He, H.; Wu, J. Adhesive, injectable, and ROS-responsive hybrid polyvinyl alcohol (PVA) hydrogel co-delivers metformin and fibroblast growth factor 21 (FGF21) for enhanced diabetic wound repair. Front. Bioeng. Biotechnol. 2022, 10, 968078. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Gao, S.; Zhang, W.; Gong, H.; Xu, K.; Luo, C.; Zhi, W.; Chen, X.; Li, J.; Weng, J. Polyvinyl alcohol/chitosan composite hydrogels with sustained release of traditional Tibetan medicine for promoting chronic diabetic wound healing. Biomater. Sci. 2021, 9, 3821–3829. [Google Scholar] [CrossRef] [PubMed]
- Zare, M.; Bigham, A.; Zare, M.; Luo, H.; Ghomi, E.R.; Ramakrishna, S. pHEMA: An Overview for Biomedical Applications. Int. J. Mol. Sci. 2021, 22, 6376. [Google Scholar] [CrossRef] [PubMed]
- Khazaeli, P.; Alaei, M.; Khaksarihadad, M.; Ranjbar, M. Preparation of PLA/chitosan nanoscaffolds containing cod liver oil and experimental diabetic wound healing in male rats study. J. Nanobiotechnology 2020, 18, 176. [Google Scholar] [CrossRef] [PubMed]
- Zha, S.; Utomo, Y.K.S.; Yang, L.; Liang, G.; Liu, W. Mechanic-Driven Biodegradable Polyglycolic Acid/Silk Fibroin Nanofibrous Scaffolds Containing Deferoxamine Accelerate Diabetic Wound Healing. Pharmaceutics 2022, 14, 601. [Google Scholar] [CrossRef] [PubMed]










| Authors | Material/Dressings | Therapeutic Compounds | Applications | Ref. |
|---|---|---|---|---|
| Ahmed et al. | Polyvinyl alcohol—Chitosan nanofiber mats | Zinc oxide NP | Microbial-Infected DW Care | [43] |
| Cam et al. | Polyvinylpyrrolidone-Polycaprolactone nanofibrous mats | Pioglitazone | DW Healing | [44] |
| Almasian et al. | Polyurethane—Carboxymethylcellulose nanofibers | Plant extract of Malva sylvestris | DW Treatment | [45] |
| Chen et al. | Poly-N-acetylglucosamine nanofibers | Polydeoxyribonucleotide | Diabetic Skin Ulcer | [46] |
| Choi et al. | Polyethylene glycol—Polycaprolactone hybrid nanofibers | Human Epidermal Growth Factor | Diabetic Ulcer Treatment | [47] |
| Cui et al. | Polylactide-based nanofibers | Doxycycline | Chronic Wound Management | [48] |
| Grip et al. | Hydroxypropyl Methylcellulose/Polyethylene oxide nanofibers | β-Glucan | DW Care | [49] |
| Kanji et al. | Polyethersulfone nanofibers | Human umbilical cord blood-derived CD34+ cells | DW Management | [50] |
| Lee et al. | PLGA nanofibers | Platelet-derived growth factor, Vancomycin, and Gentamicin | Diabetic Infected Wound Care | [51] |
| Lee et al. | PLGA nanofibers | Insulin | DW Recovery | [52] |
| Merrel et al. | Polycaprolactone nanofibers | Curcumin | DW Management | [53] |
| Pinzón-García et al. | Polycaprolactone nanofibers | Bixin | DW Healing | [54] |
| Ranjbar-Mohammadi et al. | Polycaprolactone—Gum Tragacanth nanofibers | Curcumin | DW Care | [55] |
| Shalaby et al. | Cellulose acetate nanofibers | Silver NP | Microbial-Infected Diabetic Lesion Treatment | [56] |
| Zehra et al. | Polycaprolactone nanofibers | Sodium Percarbonate | DW Management | [57] |
| Lee et al. | PLGA—Collagen scaffold membranes | Glucophage | DW Management | [58] |
| Zheng et al. | PLGA—Cellulose nanocrystals nanofiber membranes | Neurotensin | DW Care | [59] |
| Liu et al. | Cellulose acetate—Zein composite nanofiber membranes | Sesamol | DW Treatment | [60] |
| Lee et al. | PLGA membranes | Metformin | DW Healing | [61] |
| Ren et al. | Poly-L-lactic acid fibrous membranes | Dimethyloxalylglycine-loaded mesoporous silica NP | DW Treatment | [62] |
| Lobmann et al. | Hyaluronic acid membranes | Human keratinocytes | Diabetic Foot Wounds | [63] |
| Augustine et al. | Poly(3- hydroxybutyrate-co-3-hydroxyvalerate) membranes | Cerium oxide NP/gelatin | DW Treatment | [64] |
| Augustine et al. | Polyvinyl alcohol—Polylactic acid hybrid membranes | Connective tissue growth factor | Wound Dressing Membranes For Diabetic Lesions And Chronic Ulcers | [65] |
| Arantes et al. | Chitosan films | Retinoic acid / solid lipid nanoparticles | DW Healing | [66] |
| Arul et al. | Collagen films | Biotinylated GHK peptide | DW Dressing | [67] |
| Inpanya et al. | Fibroin films | Aloe gel | DW Management | [68] |
| Kim et al. | Polyvinylpyrrolidone—Polyvinyl alcohol films | Sodium fusidate | Wound Healing | [69] |
| Mizuno et al. | Chitosan films | Fibroblast growth factors | DW Healing | [70] |
| Song et al. | Cellulose films | Selenium | Cutaneous DW Healing | [71] |
| Tan et al. | Sodium alginate hydrocolloid films | Vicenin-2 | DW Management | [72] |
| Tong et al. | Polyvinyl alcohol—Cellulose anocrystal films | Curcumin | DW Care | [73] |
| Voss et al. | Cellulose—Polyvinyl alcohol films | Propolis and/or Vitamin C | DW Management | [74] |
| Wu et al. | Silk Fibroin—Chitosan films | Adipose-derived stem cells | DW Care | [75] |
| Da Silva et al. | Hyaluronic acid spongy hydrogels | Human adipose stem cells | Diabetic Foot Ulcer | [76] |
| Lai et al. | Sodium carboxymethylcellulose hydrogels | Fern extracts (Blechnum orientale Linn.) | Diabetic Ulcer Treatment | [77] |
| Li et al. | Hydroxyapatite/Chitosan composite hydrogels | Exosomes (SMSCs-126) | DW Treatment | [78] |
| Masood et al. | Chitosan—Polyethylene glycol hybrid hydrogels | Silver NP | DW Healing | [79] |
| Shi et al. | Chitosan—Dextran hydrogels | Silver NP | DW Treatment | [80] |
| Thangavel et al. | Chitosan hydrogels | L-glutamic acid | DW Healing | [81] |
| Zhang et al. | Poly (γ-glutamic acid)—Heparin—Chitosan composite hydrogels | Superoxide dismutase | DW Treatment | [82] |
| Choi et al. | Polyurethane foams | Silver nanoparticles and Recombinant Human Epidermal Growth Factor | Bacteria-Infected DW Management | [83] |
| Pyun et al. | Polyurethane foams | Recombinant Human Epidermal Growth Factor | DW Treatment | [84] |
| Atia et al. | Sodium alginate—Gelatin wafers | Diosmin nanocrystals | DW Healing | [85] |
| Anisha et al. | Hyaluronic acid—Chitosan sponges | Silver nanoparticles | Wound Dressing for Diabetic Foot Ulcer | [86] |
| Lipsky et al. | Collagen sponges | Gentamicin | Diabetic Foot Ulcer | [87] |
| Mohandas et al. | Chitosan—Hyaluronic acid composite sponges | Fibrin nanoparticles incorporated with vascular endothelial growth factors | Wound Dressing For DW | [88] |
| Shi et al. | Chitosan—Silk hybrid sponges | Gingival mesenchymal stem cell-derived exosomes | DW Healing | [89] |
| Wang et al. | Chitosan—Collagen sponges | Recombinant Human Acidic Fibroblast Growth Factors | DW Healing | [90] |
| Xia et al. | Chitosan composite sponges | Quaternary ammonium chitosan nanoparticles | Wound DressingMaterial for Diabetic Chronic Injury | [91] |
| Kondo et al. | Hyaluronic acid—Collagen sponges | Epidermal growth factors | DW Healing | [92] |
| Raveendran et al. | Chitosan bandages | Ciprofloxacin and Fluconazole-containing Fibrin nanoparticles | DW Management | [93] |
| Mohanty et al. | Sodium alginate—Chitosan bandages | Epidermal growth factor, curcumin, and mesenchymal stem cells | DW Healing | [94] |
| Kumar et al. | Chitosan hydrogel composite bandages | Zinc oxide nanoparticles | Wound Dressing Material | [95] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sathyaraj, W.V.; Prabakaran, L.; Bhoopathy, J.; Dharmalingam, S.; Karthikeyan, R.; Atchudan, R. Therapeutic Efficacy of Polymeric Biomaterials in Treating Diabetic Wounds—An Upcoming Wound Healing Technology. Polymers 2023, 15, 1205. https://doi.org/10.3390/polym15051205
Sathyaraj WV, Prabakaran L, Bhoopathy J, Dharmalingam S, Karthikeyan R, Atchudan R. Therapeutic Efficacy of Polymeric Biomaterials in Treating Diabetic Wounds—An Upcoming Wound Healing Technology. Polymers. 2023; 15(5):1205. https://doi.org/10.3390/polym15051205
Chicago/Turabian StyleSathyaraj, Weslen Vedakumari, Lokesh Prabakaran, Jayavardhini Bhoopathy, Sankari Dharmalingam, Ramadoss Karthikeyan, and Raji Atchudan. 2023. "Therapeutic Efficacy of Polymeric Biomaterials in Treating Diabetic Wounds—An Upcoming Wound Healing Technology" Polymers 15, no. 5: 1205. https://doi.org/10.3390/polym15051205
APA StyleSathyaraj, W. V., Prabakaran, L., Bhoopathy, J., Dharmalingam, S., Karthikeyan, R., & Atchudan, R. (2023). Therapeutic Efficacy of Polymeric Biomaterials in Treating Diabetic Wounds—An Upcoming Wound Healing Technology. Polymers, 15(5), 1205. https://doi.org/10.3390/polym15051205