The Use of Natural Polymers in Tissue Engineering: A Focus on Electrospun Extracellular Matrix Analogues
Abstract
:1. Introduction
1.1. The Native Extracellular Matrix
| Component | Location | Function |
|---|---|---|
| Collagen | Widely distributed | Key component of tissue architecture, provide tensile strength, cell-matrix interaction, matrix-matrix interaction |
| Elastin | Highly elastic tissues (lung, blood vessel, skin) | Key component of tissue architecture, provide elasticity |
| Proteoglycans | Widely distributed | Cell-matrix interaction, matrix-matrix interaction, cell proliferation, cell migration |
| Hyaluronan | Widely distributed | Cell-matrix interaction, matrix-matrix interaction, cell proliferation, cell migration |
| Laminin | Basement membranes | Basement membrane component, cell migration |
| Fibronectin | Widely distributed | Component of tissue architecture, cell-matrix interaction, matrix-matrix interaction, cell proliferation, cell migration |
| Fibrinogen | Blood, sites of wound healing | Cell proliferation, cell migration, hemostasis |
| Various Adhesion Molecules | Widely distributed | Mediate cell adhesion to matrix, mediate transmembrane signals |

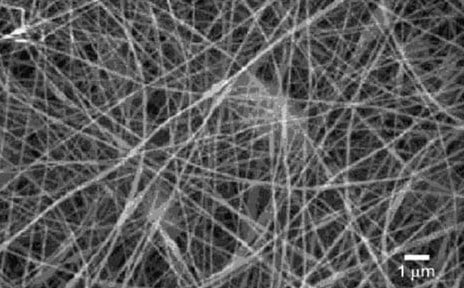
1.2. Electrospinning

2. Electrospun Natural Polymers
2.1. Collagen
2.1.1. Electrospinning Collagen

2.1.2. Electrospinning Collagen and Natural Polymer Blends
2.1.3. Electrospinning Collagen and Synthetic Polymer Blends
2.2. Gelatin
2.3. Elastin
2.3.1. Electrospinning Elastin

2.3.2. Electrospinning Elastin and Synthetic Polymer Blends

2.3.3. Electrospinning Collagen and Elastin

2.4. Fibrinogen
2.4.1. Electrospinning Fibrinogen


2.5. Silk Fibroin
2.5.1. Electrospinning Silk Fibroin

3. Current Challenges and Future Directions
4. Conclusions
References
- Barnes, C.P.; Sell, S.A.; Boland, E.D.; Simpson, D.G.; Bowlin, G.L. Nanofiber technology: designing the next generation of tissue engineering scaffolds. Adv. Drug Delivery Rev. 2007, 59, 1413–1433. [Google Scholar] [CrossRef]
- Martins-Green, M. The dynamics of Cell-ECM interactions with implications for tissue engineering. In Principles of Tissue Engineering; Lanza, R., Langer, R., Chick, W., Eds.; R.G. Landes Company: Austin, TX, USA, 1997; pp. 23–46. [Google Scholar]
- Palsson, B.O.; Bhatia, S.N. Tissue Engineering; Pearson Prentice Hall: Upper Sadle River, NJ, USA, 2004. [Google Scholar]
- Farach-Carson, M.C.; Wagner, R.C.; Kiick, K.L. Extracellular matrix: Structure, function, and applications to tissue engineering. In Tissue Engineering; Fisher, J.P., Mikos, A.G., Bronzino, J.D., Eds.; CRC Press: Boca Raton, FL, USA, 2007; p. 3-1-3-22. [Google Scholar]
- Boland, E.D.; Espy, P.G.; Bowlin, G.L. Tissue engineering scaffolds. In Encyclopedia of BioMaterials and Biomedical Engineering; Informa Healthcare: London, UK, 2004; pp. 1–7. [Google Scholar]
- Chew, S.Y.; Wen, Y.; Dzenis, Y.; Leong, K.W. The role of electrospinning in the emerging field of nanomedicine. Curr. Pharm. Des. 2006, 12, 4751–4570. [Google Scholar] [CrossRef] [PubMed]
- Lannutti, J.; Reneker, D.; Ma, T.; Tomasko, D.; Farson, D. Electrospinning for tissue engineering scaffolds. Mater. Sci. Eng. C Bio. Supramol. Syst. 2007, 27, 504–509. [Google Scholar] [CrossRef]
- Sell, S.; Barnes, C.; Smith, M.; McClure, M.; Madurantakam, P.; Grant, J.; McManus, M.; Bowlin, G. Extracellular matrix regenerated: tissue engineering via electrospun biomimetic nanofibers. Polym. Int. 2007, 56, 1349–1360. [Google Scholar]
- Kumbar, S.G.; James, R.; Nukavarapu, S.P.; Laurencin, C.T. Electrospun nanofiber scaffolds: engineering soft tissues. Biomed. Mater. 2008, 3, 034002. [Google Scholar] [CrossRef] [PubMed]
- Sill, T.J.; von Recum, H.A. Electrospinning: Applications in drug delivery and tissue engineering. Biomaterials 2008, 29, 1989–2006. [Google Scholar] [CrossRef] [PubMed]
- Sell, S.A.; McClure, M.J.; Garg, K.; Wolfe, P.S.; Bowlin, G.L. Electrospinning of collagen/biopolymers for regenerative medicine and cardiovascular tissue engineering. Adv. Drug Delivery Rev. 2009, 61, 1007–1019. [Google Scholar] [CrossRef]
- Jayaraman, K.; Kotaki, M.; Zhang, Y.; Mo, X.; Ramakrishna, S. Recent advances in polymer nanofibers. J. NanoSci. Nanotechnol. 2004, 4, 52–65. [Google Scholar] [PubMed]
- Engel, E.; Michiardi, A.; Navarro, M.; Lacroix, D.; Planell, J.A. Nanotechnology in regenerative medicine: the Mater. side. Trends Biotechn. 2007, 26, 39–47. [Google Scholar] [CrossRef]
- Mano, J.F.; Silva, G.A.; Azevedo, H.S.; Malafaya, P.B.; Sousa, R.A.; Silva, S.S.; Boesel, L.F.; Oliveira, J.; Santos, T.C.; Marques, A.P.; Neves, N.M.; Reis, R.L. Natural origin biodegradable systems in tissue engineering and regenerative medicine: present status and some moving trends. J. Royal Soc. Interface 2007, 4, 999–1030. [Google Scholar] [Green Version]
- Ramakrishna, S.; Fujihara, K.; Teo, W.E.; Lim, T.C.; Ma, Z. Introduction to Electrospinning and Nanofibers; World Scientific Publishing Company, Incorporated: Singapore, 2005. [Google Scholar]
- Kidoaki, S.; Kwon, I.K.; Matsuda, T. Mesoscopic spatial designs of nano- and microfiber meshes for tissue-engineering matrix and scaffold based on newly devised multilayering and mixing electrospinning techniques. Biomaterials 2005, 26, 37–46. [Google Scholar] [CrossRef] [PubMed]
- Hutmacher, D.; Woodfield, T.; Dalton, P.; Lewis, J. Scaffold design and fabrication. In Tissue Engineering; Blitterswijk, C.V., Ed.; Elsevier Inc.: San Diego, CA, USA, 2008; pp. 403–454. [Google Scholar]
- Stankus, J.J.; Soletti, L.; Fujimoto, K.; Hong, Y.; Vorp, D.A.; Wagner, W.R. Fabrication of cell microintegrated blood vessel constructs through electrohydrodynamic atomization. Biomaterials 2007, 28, 2738–2746. [Google Scholar] [CrossRef] [PubMed]
- Sell, S.A.; McClure, M.J.; Ayres, C.E.; Simpson, D.G.; Bowlin, G.L. Preliminary investigation of airgap electrospun silk fibroin-based structures for ligament analogue engineering. J. Biomater. Sci. Polym. Ed. 2010, in press. [Google Scholar]
- Konomi, H.; Hayashi, T.; Nakayasu, K.; Arima, M. Localization of type V collagen and type IV collagen in human cornea, lung, and skin. Immunohistochemical evidence by anti-collagen antibodies characterized by immunoelectroblotting. Am. of Pathol. 1984, 116, 417–426. [Google Scholar]
- Huang, L.; Nagapudi, K.; Apkarian, R.P.; Chaikof, E.L. Engineered collagen-PEO nanofibers and fabrics. J. Biomater. Sci. Polym. Ed. 2001, 12, 979–993. [Google Scholar] [CrossRef] [PubMed]
- Matthews, J.A.; Wnek, G.E.; Simpson, D.G.; Bowlin, G.L. Electrospinning of collagen nanofibers. Biomacromolecules 2002, 3, 232–238. [Google Scholar] [CrossRef] [PubMed]
- Matthews, J.A.; Boland, E.D.; Wnek, G.E.; Simpson, D.G.; Bowlin, G.L. Electrospinning of Collagen Type II: A Feasibility Study. J. Bioact. Compat. Polym. 2003, 18, 125–134. [Google Scholar] [CrossRef]
- Barnes, C.P.; Sell, S.A.; Knapp, D.C.; Walpoth, B.H.; Brand, D.D.; Bowlin, G.L. Preliminary investigation of electrospun collagen and polydioxanone for vascular tissue engineering applications. Int. J. Electrospun Nanofiber. Appl. 2007, 1, 73–87. [Google Scholar]
- Barnes, C.P.; Pemble, C.W.; Brand, D.D.; Simpson, D.G.; Bowlin, G.L. Cross-linking electrospun type II collagen tissue engineering scaffolds with carbodiimide in ethanol. Tissue Eng. 2007, 13, 1593–1605. [Google Scholar] [CrossRef] [PubMed]
- Dong, B.; Arnoult, O.; Smith, M.E.; Wnek, G.E. Electrospinning of Collagen Nanofiber Scaffolds from Benign Solvents. Macromol. Rapid Commun. 2009, 30, 539–542. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.S.; Lee, S.W.; Jeong, L.; Bae, S.H.; Min, B.C.; Youk, J.H.; Park, W.H. Effect of organosoluble salts on the nanofibrous structure of electrospun poly(3-hydroxybutyrate-co-3-hydroxyvalerate). Int. J. Biol. Macromol. 2004, 34, 249–256. [Google Scholar] [CrossRef] [PubMed]
- Zhong, S.; Teo, W.E.; Zhu, X.; Beuerman, R.; Ramakrishna, S.; Yung, L.Y. Formation of collagen-glycosaminoglycan blended nanofibrous scaffolds and their biological properties. Biomacromolecules 2005, 6, 2998–3004. [Google Scholar] [CrossRef] [PubMed]
- Thomas, V.; Dean, D.R.; Jose, M.V.; Mathew, B.; Chowdhury, S.; Vohra, Y.K. Nanostructured biocomposite scaffolds based on collagen coelectrospun with nanohydroxyapatite. Biomacromolecules 2007, 8, 631–637. [Google Scholar] [CrossRef] [PubMed]
- Chen, P.J.; Chang, G.Y.; Chen, J.K. Electrospun collagen/chitosan nanofibrous membrane as wound dressing. Colloids Surface. A 2008, 313, 183–188. [Google Scholar] [CrossRef]
- Chen, Z.G.; Wang, P.W.; Wei, B.; Mo, X.M.; Cui, F.Z. Electrospun collagen-chitosan nanofiber: A biomimetic extracellular matrix for endothelial cell and smooth muscle cell. Acta Biomater. 2009, 6, 372–382. [Google Scholar] [CrossRef]
- Yeo, I.S.; Oh, J.E.; Jeong, L.; Lee, T.S.; Lee, S.J.; Park, W.H.; Min, B.M. Collagen-based biomimetic nanofibrous scaffolds: preparation and characterization of collagen/silk fibroin bicomponent nanofibrous structures. Biomacromolecules 2008, 9, 1106–1116. [Google Scholar] [CrossRef] [PubMed]
- He, W.; Yong, T.; Teo, W.E.; Ma, Z.; Ramakrishna, S. Fabrication and endothelialization of collagen-blended biodegradable polymer nanofibers: potential vascular graft for blood vessel tissue engineering. Tissue Eng. 2005, 11, 1574–1588. [Google Scholar] [CrossRef] [PubMed]
- Kwon, I.K.; Matsuda, T. Co-electrospun nanofiber fabrics of poly(L-lactide-co-epsilon-caprolactone) with type I collagen or heparin. Biomacromolecules 2005, 6, 2096–2105. [Google Scholar] [CrossRef] [PubMed]
- Stitzel, J.D.; Pawlowski, K.J.; Wnek, G.E.; Simpson, D.G.; Bowlin, G.L. Arterial smooth muscle cell proliferation on a novel biomimicking, biodegradable vascular graft scaffold. J. Biomater. Appl. 2001, 16, 22–33. [Google Scholar] [CrossRef] [PubMed]
- Boland, E.D.; Coleman, B.D.; Barnes, C.P.; Simpson, D.G.; Wnek, G.E.; Bowlin, G.L. Electrospinning polydioxanone for biomedical applications. Acta Biomater. 2005, 1, 115–123. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.J.; Liu, J.; Oh, S.H.; Soker, S.; Atala, A.; Yoo, J.J. Development of a composite vascular scaffolding system that withstands physiological vascular conditions. Biomaterials 2008, 29, 2891–2898. [Google Scholar] [CrossRef] [PubMed]
- Tillman, B.W.; Yazdani, S.K.; Lee, S.J.; Geary, R.L.; Atala, A.; Yoo, J.J. The in vivo stability of electrospun polycaprolactone-collagen scaffolds in vascular reconstruction. Biomaterials 2009, 30, 583–588. [Google Scholar] [CrossRef] [PubMed]
- Venugopal, J.; Zhang, Y.Z.; Ramakrishna, S. Fabrication of modified and functionalized polycaprolactone nanofibre scaffolds for vascular tissue engineering. Nanotechnology 2005, 16, 2138–2142. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.S.; Lee, S.J.; Christ, G.J.; Atala, A.; Yoo, J.J. The influence of electrospun aligned poly(epsilon-caprolactone)/collagen nanofiber meshes on the formation of self-aligned skeletal muscle myotubes. Biomaterials 2008, 29, 2899–2906. [Google Scholar] [CrossRef] [PubMed]
- Schnell, E.; Klinkhammer, K.; Balzer, S.; Brook, G.; Klee, D.; Dalton, P.; Mey, J. Guidance of glial cell migration and axonal growth on electrospun nanofibers of poly-epsilon-caprolactone and a collagen/poly-epsilon-caprolactone blend. Biomaterials 2007, 28, 3012–3025. [Google Scholar] [CrossRef] [PubMed]
- Yoon, D.M.; Fisher, J.P. Polymeric Scaffolds for Tissue Engineering Applications. In Tissue Engineering; Fisher, J.P., Mikos, A.G., Bronzino, J.D., Eds.; Taylor and Francis Group, LLC: Boca Raton, FL, USA, 2007; p. 18. [Google Scholar]
- Li, M.; Mondrinos, M.J.; Gandhi, M.R.; Ko, F.K.; Weiss, A.S.; Lelkes, P.I. Electrospun protein fibers as matrices for tissue engineering. Biomaterials 2005, 26, 5999–6008. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Ouyang, H.; Lim, C.T.; Ramakrishna, S.; Huang, Z.-M. Electrospinning of Gelatin Fibers and Gelatin/PCL Composite Fibrous Scaffolds. J. Biomed. Mater. Res. B Appl. BioMater. 2005, 72B, 156–165. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.; Huang, Y.; Yang, X.; Mei, F.; Ma, Q.; Chen, G.; Ryu, S.; Deng, X. Gelatin nanofibrous membrane fabricated by electrospinning of aqueous gelatin solution for guided tissue regeneration. J. Biomed. Mater. Res. 2009. [Google Scholar] [CrossRef]
- Heydarkhan-Hagvall, S.; Schenke-Layland, K.; Dhanasopon, A.P.; Rofail, F.; Smith, H.; Wu, B.M.; Shemin, R.; Beygui, R.E.; MacLellan, W.R. Three-dimensional electrospun ECM-based hybrid scaffolds for cardiovascular tissue engineering. Biomaterials 2008, 29, 2907–2914. [Google Scholar] [CrossRef] [PubMed]
- Sisson, K.; Zhang, C.; Farach-Carson, M.C.; Chase, D.B.; Rabolt, J.F. Evaluation of cross-linking methods for electrospun gelatin on cell growth and viability. BioMacromolecules 2009, 10, 1675–1680. [Google Scholar] [CrossRef] [PubMed]
- Francis, L.; Venugopal, J.; Prabhakaran, M.P.; Thavasi, V.; Marsano, E.; Ramakrishna, S. Simultaneous electrospin-electrosprayed biocomposite nanofibrous scaffolds for bone tissue regeneration. Acta Biomater. 2010, 6, 4100–4109. [Google Scholar] [CrossRef] [PubMed]
- Ohkawa, K.; Hayashi, S.; Kameyama, N.; Yamamoto, H.; Yamaguchi, M.; Kimoto, S.; Kurata, S.; Shinji, H. Synthesis of collagen-like sequential polypeptides containing O-Phospho-L-hydroxyproline and preparation of electrospun composite fibers for possible dental application. Macromol. BioSci. 2009, 9, 79–92. [Google Scholar] [CrossRef] [PubMed]
- Sisson, K.; Zhang, C.; Farach-Carson, M.C.; Chase, D.B.; Rabolt, J.F. Fiber diameters control osteoblastic cell migration and differentiation in electrospun gelatin. J. Biomed. Mater. Res. A 2010, 94A, 1312–1320. [Google Scholar] [PubMed]
- Gauthaman, K.; Venugopal, J.R.; Yee, F.C.; Peh, G.S.L.; Ramakrishna, S.; Bongso, A. Nanofibrous substrates support colony formation and maintain stemness of human embryonic stem cells. J. Cell. Mol. Med. 2009, 13, 3475–3484. [Google Scholar] [CrossRef] [PubMed]
- Gupta, D.; Venugopal, J.; Prabhakaran, M.P.; Dev, V.R.G.; Low, S.; Choon, A.T.; Ramakrishna, S. Aligned and random nanofibrous substrate for the in vitro culture of Schwann cells for neural tissue engineering. Acta Biomater. 2009, 5, 2560–2569. [Google Scholar] [CrossRef] [PubMed]
- Songchotikunpan, P.; Tattiyakul, J.; Supaphol, P. Extraction and electrospinning of gelatin from fish skin. Int. J. Biol. Macromol. 2008, 42, 247–255. [Google Scholar] [CrossRef] [PubMed]
- Song, J.-H.; Kim, H.-E.; Kim, H.-W. Production of electrospun gelatin nanofiber by water-based co-solvent approach. J. Mater. Sci. Mater. Med. 2008, 19, 95–102. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; He, A.; Zheng, J.; Han, C.C. Gelatin and gelatin-hyaluronic acid nanofibrous membranes produced by electrospinning of their aqueous solutions. Biomacromolecules 2006, 7, 2243–2247. [Google Scholar] [CrossRef]
- Jiankang, H.; Dichen, L.; Yaxiong, L.; Bo, Y.; Hanxiang, Z.; Qin, L.; Bingheng, L.; Yi, L. Preparation of chitosan-gelatin hybrid scaffolds with well-organized microstructures for hepatic tissue engineering. Acta Biomater. 2008. in Press. [Google Scholar]
- Gupta, D.; Venugopal, J.; Mitra, S.; Dev, V.R.G.; Ramakrishna, S. Nanostructured biocomposite substrates by electrospinning and electrspraying for the mineralization of osteoblasts. Biomaterials 2009, 30, 2085–2094. [Google Scholar] [CrossRef] [PubMed]
- Gui-Bo, Y.; You-Zhu, Z.; Shu-Dong, W.; De-Bing, S.; Zhi-Hui, D.; Wei-Guo, F. Study of the electrospun PLA/silk fibroin-gelatin composite nanofibrous scaffold for tissue engineering. J. Biomed. Mater. Res. 2010, 93A, 158–163. [Google Scholar]
- Chong, E.J.; Phan, T.T.; Lim, I.J.; Zhang, Y.Z.; Bay, B.H.; Ramakrishna, S.; Lim, C.T. Evaluation of electrospun PCL/gelatin nanofibrous scaffold for wound healing and layered dermal reconstitution. Acta Biomater. 2007, 3, 321–330. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.E.; Heo, D.N.; Lee, J.B.; Kim, J.R.; Park, S.H.; Jeon, S.H.; Kwon, I.K. Electrospun gelatin/polyurethane blended nanofibers for wound healing. Biomed. Mater. 2009, 4, 1–11. [Google Scholar] [CrossRef]
- Ghasemi-Mobarakeh, L.; Prabhakaran, M.P.; Morshed, M.; Nasr-Esfahani, M.H.; Ramakrishna, S. Electrical Stimulation of nerve cells using conductive nanofibrous scaffolds for nerve tissue engineering. Tissue Eng. A 2009, 15, 3605–3619. [Google Scholar] [CrossRef]
- Ghasemi-Mobarakeh, L.; Prabhakaran, M.P.; Morshed, M.; Nasr-Esfahani, M.H.; Ramakrishna, S. Electrospun poly(epsilon-caprolactone)/gelatin nanofibrous scaffolds for nerve tissue engineering. BioMater. 2008, 29, 4532–4539. [Google Scholar] [CrossRef]
- Kim, H.-W.; Yu, H.-S.; Lee, H.-H. Nanofibrous matrices of poly(lactic acid) and gelatin polymeric blends for the improvement of cellular responses. J. Biomed. Mater. Res. 2008, 87A, 25–32. [Google Scholar] [CrossRef]
- Dhandayuthapani, B.; Krishnan, U.M.; Sethuraman, S. Fabrication and characterization of chitosan-gelatin blend nanofibers for skin tissue engineering. J. Biomed. Mater. Res. B Appl. BioMater. 2010, 94B, 264–272. [Google Scholar] [PubMed]
- Powell, H.M.; Boyce, S.T. Fiber density of electrospun gelatin scaffolds regulates morphogenesis of dermal-epidermal skin substitutes. J. Biomed. Mater. Res. 2008, 84A, 1078–1086. [Google Scholar] [CrossRef]
- Wang, S.; Zhang, Y.; Wang, H.; Yin, G.; Dong, Z. Fabrication and Properties of the Electrospun Polylactide/Silk Fibroin-Gelatin Composite Tubular Scaffold. Biomacromolecules 2009, 10, 2240–2244. [Google Scholar] [CrossRef] [PubMed]
- Li, M.; Guo, Y.; Wei, Y.; MacDiarmid, A.G.; Lelkes, P.I. Electrospinning polyaniline-contained gelatin nanofibers for tissue engineering applications. Biomaterials 2006, 27, 2705–2715. [Google Scholar] [CrossRef] [PubMed]
- Li, M.; Mondrinos, M.J.; Chen, X.; Gandhi, M.R.; Ko, F.K.; Lelkes, P.I. Co-electrospun poly(lactide-co-glycolide), gelatin, and elastin blends for tissue engineering scaffolds. J. Biomed. Mater. Res. 2006, 79A, 963–973. [Google Scholar] [CrossRef]
- Kejing, A.; Haiying, L.; Shidong, G.; Kumar, D.N.T.; Qingqing, W. Preparation of fish gelatin and fish gelatin/poly(L-lactide) nanofibers by electrospinning. Int. J. Biol. Macromol. 2010, 47, 380–388. [Google Scholar] [CrossRef] [PubMed]
- Rodgers, U.R.; Weiss, A.S. Cellular interactions with elastin. Pathol. Biol. 2005, 53, 390–398. [Google Scholar] [CrossRef] [PubMed]
- Debelle, L.; Tamburro, A.M. Elastin: molecular description and function. Int. J. Biochem. Cell Biol. 1999, 31, 261–272. [Google Scholar] [CrossRef] [PubMed]
- Duca, L.; Floquet, N.; Aliz, A.J.P.; Haye, B.; Debelle, L. Elastin as a matrikine. Crit. Rev. Oncol. Hematol. 2004, 49, 235–244. [Google Scholar] [CrossRef] [PubMed]
- Huang, L.; McMillan, R.A.; Apkarian, R.P.; Pourdeyhimi, B.; Conticello, V.P.; Chaikof, E.L. Generation of synthetic elastin-mimetic small diameter fibers and fiber networks. Macromolecules 2000, 33, 2989–2997. [Google Scholar] [CrossRef]
- Partridge, S.M.; Davis, H.F. The Chemistry of Connective Tissues 3. Composition of the soluble proteins derived from elastin. Biochem. J. 1955, 61, 21–30. [Google Scholar] [PubMed]
- Daamen, W.F.; Veerkamp, J.H.; van Hest, J.C.M.; van Kuppevelt, T.H. Elastin as a biomaterial for tissue engineering. Biomaterials 2007, 28, 4378–4398. [Google Scholar] [CrossRef] [PubMed]
- Lamme, E.N.; van Leeuwen, R.T.; Jonker, A.; van Marle, J.; Middelkoop, E. Living skin substitutes: Survival and function of fibroblasts seeded in a dermal substitute in experimental wounds. J. Invest. Dermatol. 1998, 111, 989–995. [Google Scholar] [CrossRef] [PubMed]
- Neuenschwander, S.; Hoerstrup, S.P. Heart valve tissue engineering. Transplant Immunol. 2004, 12, 359–365. [Google Scholar] [CrossRef]
- Xu, J.W.; Johnson, T.S.; Motarjem, P.M.; Peretti, G.M.; Randolph, M.A.; Yaremchuk, M.J. Tissue-engineered flexible ear-shaped cartilage. Plast. Reconstr. Sur. 2005, 115, 1633–1641. [Google Scholar] [CrossRef]
- Nivison-Smith, L.; Rnjak, J.; Weiss, A.S. Synthetic human elastin microfibers: Stable cross-linked tropoelastin and cell interactive constructs for tissue engineering applications. Acta Biomater. 2010, 6, 354–359. [Google Scholar] [CrossRef] [PubMed]
- McClure, M.; Sell, S.; Barnes, C.P.; Bowen, W.C.; Bowlin, G.L. Cross-linking Electrospun Polydioxanone-Soluble Elastin Blends: Material Characterization. J. Eng. Fiber. Fabr. 2008, 3, 1–10. [Google Scholar]
- Boland, E.D.; Matthews, J.A.; Pawlowski, K.J.; Simpson, D.G.; Wnek, G.E.; Bowlin, G.L. Electrospinning collagen and elastin: Preliminary vascular tissue engineering. Front. BioSci. 2004, 9, 1422–1432. [Google Scholar] [CrossRef] [PubMed]
- Buttafoco, L.; Kolkman, N.G.; Engbers-Buijtenhuijs, P.; Poot, A.A.; Dijkstra, P.J.; Vermes, I.; Feijen, J. Electrospinning of collagen and elastin for tissue engineering applications. Biomaterials 2006, 27, 724–734. [Google Scholar] [CrossRef] [PubMed]
- Sell, S.A.; McClure, M.J.; Barnes, C.P.; Knapp, D.C.; Walpoth, B.H.; Simpson, D.G.; Bowlin, G.L. Electrospun polydioxanone-elastin blends: potential for bioresorbable vascular grafts. Biomed. Mater. 2006, 1, 72–80. [Google Scholar] [CrossRef] [PubMed]
- Smith, M.J.; McClure, M.J.; Sell, S.A.; Barnes, C.P.; Walpoth, B.H.; Simpson, D.G.; Bowlin, G.L. Suture-reinforced electrospun polydioxanone-elastin small-diameter tubes for use in vascular tissue engineering: A feasibility study. Acta Biomater. 2008, 4, 58–66. [Google Scholar] [CrossRef] [PubMed]
- Thomas, V.; Zhang, X.; Vohra, Y.K. A Biomimetic tubular scaffold with spatially designed nanofibers of Protein/PDS bio-blends. Biotechnol. Bioeng. 2009, 104, 1025–1033. [Google Scholar] [CrossRef] [PubMed]
- Thomas, V.; Zhang, X.; Catledge, S.A.; Vohra, Y.K. Functionally graded electrospun scaffolds with tunable mechanical properties for vascular tissue regeneration. Biomed. Mater. 2007, 2, 224–232. [Google Scholar] [CrossRef]
- Stitzel, J.; Liu, J.; Lee, S.J.; Komura, M.; Berry, J.; Soker, S.; Lim, G.; Van Dyke, M.; Czerw, R.; Yoo, J.J.; Atala, A. Controlled fabrication of a biological vascular substitute. Biomaterials 2006, 27, 1088–1094. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.J.; Yoo, J.J.; Lim, G.J.; Atala, A.; Stitzel, J. In vitro evaluation of electrospun nanofiber scaffolds for vascular graft application. J. Biomed. Mater. Res. A 2007, 83, 999–1008. [Google Scholar] [CrossRef]
- El-Kurdi, M.S.; Hong, Y.; Stankus, J.J.; Soletti, L.; Wagner, W.R.; Vorp, D.A. Transient elastic support for vein grafts using a constricting microfibrillar polymer wrap. Biomaterials 2008, 29, 3213–3220. [Google Scholar] [CrossRef] [PubMed]
- Doolittle, R.F. Fibrinogen and fibrin. Annu. Rev. Biochem. 1984, 53, 195–229. [Google Scholar] [CrossRef] [PubMed]
- Fuss, C.; Palmaz, J.C.; Sprague, E.A. Fibrinogen: structure, function, and surface interactions. J. Vasc. Interv. Radiol. 2001, 12, 677–682. [Google Scholar] [CrossRef] [PubMed]
- Clark, R.A. Fibrin is a many splendored thing. J. Invest. Dermatol. 2003, 121, xxi–xxii. [Google Scholar] [CrossRef]
- Hanson, S. Blood coagulation and blood-materials interactions. In BioMaterials Science: An Introduction to Materials in Medicine; Elsevier Academic Press: San Diego, CA, USA, 2004; pp. 332–338. [Google Scholar]
- Mosesson, M.W.; Siebenlist, K.R.; Meh, D.A. The structure and biological features of fibrinogen and fibrin. Ann. N. Y. Acad. Sci. 2001, 936, 11–30. [Google Scholar] [CrossRef] [PubMed]
- Kollman, J.M.; Pandi, L.; Sawaya, M.R.; Riley, M.; Doolittle, R.F. Crystal structure of human fibrinogen. Biochemistry 2009, 48, 3877–3886. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Song, H.; Park, I.; Carlisle, C.R.; Bonin, K.; Guthold, M. Denaturing of single electrospun fibrinogen fibers studied by deep ultraviolet fluorescence microscopy. Microsc. Res. Tech. 2010. [Google Scholar] [CrossRef]
- Rybarczyk, B.J.; Lawrence, S.O.; Simpson-Haidaris, P.J. Matrix-fibrinogen enhances wound closure by increasing both cell proliferation and migration. Blood 2003, 102, 4035–4043. [Google Scholar] [CrossRef] [PubMed]
- Drew, A.F.; Liu, H.; Davidson, J.M.; Daugherty, C.C.; Degen, J.L. Wound-healing defects in mice lacking fibrinogen. Blood 2001, 97, 3691–3698. [Google Scholar] [CrossRef] [PubMed]
- Sahni, A.; Francis, C.W. Vascular endothelial growth factor binds to fibrinogen and fibrin and stimulates endothelial cell proliferation. Blood 2000, 96, 3772–3778. [Google Scholar] [PubMed]
- Wnek, G.E.; Carr, M.; Simpson, D.G.; Bowlin, G.L. Electrospinning of nanofiber fibrinogen structures. Nano Lett. 2003, 3, 213–216. [Google Scholar] [CrossRef]
- McManus, M.C.; Boland, E.D.; Simpson, D.G.; Barnes, C.P.; Bowlin, G.L. Electrospun fibrinogen: Feasibility as a tissue engineering scaffold in a rat cell culture model. J. Biomed. Mater. Res. A 2007, 81, 299–309. [Google Scholar] [CrossRef] [PubMed]
- McManus, M.; Boland, E.; Sell, S.; Bowen, W.; Koo, H.; Simpson, D.; Bowlin, G. Electrospun nanofibre fibrinogen for urinary tract tissue reconstruction. Biomed. Mater. 2007, 2, 257–262. [Google Scholar] [CrossRef] [PubMed]
- Carlisle, C.R.; Coulais, C.; Namboothiry, M.; Carroll, D.L.; Hantgan, R.R.; Guthold, M. The mechanical properties of individual, electrospun fibrinogen fibers. Biomaterials 2009, 30, 1205–1213. [Google Scholar] [CrossRef] [PubMed]
- McManus, M.C.; Boland, E.D.; Koo, H.P.; Barnes, C.P.; Pawlowski, K.J.; Wnek, G.E.; Simpson, D.G.; Bowlin, G.L. Mechanical properties of electrospun fibrinogen structures. Acta Biomater. 2006, 2, 19–28. [Google Scholar] [CrossRef] [PubMed]
- McManus, M.C.; Sell, S.A.; Bowen, W.C.; Koo, H.P.; Simpson, D.G.; Bowlin, G.L. Electrospun fibrinogen-polydioxanone composite matrix: Potential for in situ urologic tissue engineering. J. Eng. Fiber. Fabr. 2008, 3, 12–21. [Google Scholar]
- Sell, S.A.; Francis, M.P.; Garg, K.; McClure, M.J.; Simpson, D.G.; Bowlin, G.L. Cross-linking methods of electrospun fibrinogen scaffolds for tissue engineering applications. Biomed. Mater. 2008, 3. Epub. [Google Scholar] [CrossRef]
- Perez-Rigueiro, J.; Elices, M.; Llorca, J.; Viney, C. Tensile properties of silkworm silk obtained by forced silking. J. Appl. Polym. Sci. 2001, 82, 1928–1935. [Google Scholar] [CrossRef]
- Liu, H.; Ge, Z.; Wang, Y.; Toh, S.L.; Sutthikhum, V.; Goh, J.C.H. Modification of sericin-free silk fibers for ligament tissue engineering applications. J. Biomed. Mater. Res. B 2007, 82B, 129–138. [Google Scholar] [CrossRef]
- Nagarkar, S.; Patil, A.; Lele, A.; Bhat, S.; Bellare, J.; Mashelkar, R.A. Some mechanistic insights into the gelation of regenerated silk fibroin sol. Ind. Eng. Chem. Res. 2009, 48, 8014–8023. [Google Scholar] [CrossRef]
- Zhang, Q.; Yan, S.; Li, M. Silk fibroin based porous materials. Materials 2009, 2, 2276–2295. [Google Scholar]
- Altman, G.H.; Diaz, F.; Jakuba, C.; Calabro, T.; Horan, R.L.; Chen, J.; Lu, H.; Richmond, J.; Kaplan, D.L. Silk-based biomaterials. Biomaterials 2003, 24, 401–416. [Google Scholar] [CrossRef]
- Alessandrino, A.; Marelli, B.; Arosio, C.; Fare, S.; Tanzi, M.C.; Freddi, G. Electrospun silk fibroin mats for tissue engineering. Eng. Life Sci. 2008, 8, 219–225. [Google Scholar] [CrossRef]
- Bayraktar, O.; Malay, O.; Ozgarip, Y.; Batigun, A. Silk fibroin as a novel coating material for controlled release of theophylline. Eur. J. Pharm. Biopharm. 2005, 60, 373–381. [Google Scholar] [CrossRef] [PubMed]
- Liu, L.; Liu, J.; Wang, M.; Min, S.; Cai, Y.; Zhu, L.; Yao, J. Preparation and characterization of nano-hydroxyapatite/silk fibroin porous scaffolds. J. BioMater. Sci. Polym. Ed. 2008, 19, 325–338. [Google Scholar] [PubMed]
- Silva, S.S.; Maniglio, D.; Motta, A.; Mano, J.F.; Reis, R.L.; Migliaresi, C. Genipin-modified silk-fibroin nanometric nets. Macromol. BioSci. 2008, 8, 766–774. [Google Scholar] [CrossRef] [PubMed]
- Kearns, V.; Macintosh, A.C.; Crawford, A.; Hatton, P.V. Silk-based biomaterials for tissue engineering. In Topics in tissue engineering; Ashammakhi, N., Chiellini, R.R.F., Eds.; Biomaterials and Tissue Engineering Group: Finland, 2008; Volume 4, pp. 1–19. [Google Scholar]
- Altman, G.H.; Horan, R.L.; Lu, H.H.; Moreau, J.; Martin, I.; Richmond, J.C.; Kaplan, D.L. Silk matrix for tissue engineered anterior cruciate ligaments. Biomaterials 2002, 23, 4131–4141. [Google Scholar] [CrossRef] [PubMed]
- Wang, M.; Jin, H.-J.; Kaplan, D.L.; Rutledge, G.C. Mechanical properties of electrospun silk fibers. Macromolecules 2004, 37, 6856–6864. [Google Scholar] [CrossRef]
- Jeong, L.; Lee, K.Y.; Park, W.H. Effect of solvent on the characteristics of electrospun regenerated silk fibroin nanofibers. Key Eng. Mater. 2007, 342, 813–816. [Google Scholar] [CrossRef]
- Zarkoob, S.; Eby, R.K.; Reneker, D.H.; Hudson, S.D.; Ertley, D.; Adams, W.W. Structure and morphology of electrospun silk nanofibers. Polymers 2004, 45, 3973–3977. [Google Scholar] [CrossRef]
- Zarkoob, S. Structure and morphology of regenerated silk nano-fibers produced by electrospinning. Ph.D. Thesis, The University of Akron, Akron, OH, USA, 1998. [Google Scholar]
- Zarkoob, S.; Reneker, D.H.; Ertley, D.; Eby, R.K.; Hudson, S.D. Synthetically spun silk nanofibers and a process for making the same. U.S. Patent 6110590, August 2000. [Google Scholar]
- Sukigara, S.; Gandhi, M.; Ayutsede, J.; Micklus, M.; Ko, F. Regeneration of Bombyx mori silk by electrospinning—Part 1: Processing parameters and geometric properties. Polymers 2003, 44, 5721–5727. [Google Scholar] [CrossRef]
- Sukigara, S.; Gandhi, M.; Ayutesede, J.; Micklus, M.; Ko, F. Regeneration of Bombyx mori silk by electrospinning. Part 2. Process optimization and empirical modeling using response surface methodology. Polymers 2004, 45, 3701–3708. [Google Scholar] [CrossRef]
- Jin, H.-J.; Fridrikh, S.V.; Rutledge, G.C.; Kaplan, D.L. Electrospinning Bombyx mori silk with poly(ethylene oxide). Biomacromolecules 2002, 3, 1233–1239. [Google Scholar] [CrossRef] [PubMed]
- Jin, H.J.; Chen, J.; Karageorgiou, V.; Altman, G.H.; Kaplan, D.L. Human bone marrow stromal cell responses on electrospun silk fibroin mats. Biomaterials 2004, 25, 1039–1047. [Google Scholar] [CrossRef] [PubMed]
- Vepari, C.; Kaplan, D.L. Silk as a biomaterial. Progr. Polym. Sci. 2007, 32, 991–1007. [Google Scholar] [CrossRef]
- Wang, Y.; Rudym, D.D.; Walsh, A.; Abrahamsen, L.; Kim, H.-H.; Kim, H.S.; Kirker-Head, C.; Kaplan, D.L. In vivo degradation of three-dimensional silk fibroin scaffolds. Biomaterials 2008, 29, 3415–3428. [Google Scholar] [CrossRef] [PubMed]
- Ueda, H.; Hong, L.; Yamamoto, M.; Shigeno, K.; Inoue, M.; Toba, T. Use of collagen sponge incorporating transforming growth factor-beta 1 to promote bone repair in skull defects in rabbits. Biomaterials 2002, 23, 1003–1010. [Google Scholar] [CrossRef] [PubMed]
- Sun, H.; Mei, L.; Song, C.; Cui, X.; Wang, P. The in vivo degradation, absorption and excretion of PCL-based implant. Biomaterials 2006, 27, 1735–1740. [Google Scholar] [CrossRef] [PubMed]
- Ramchandani, M.; Pankaskie, M.; Robinson, D. The influence of manufacturing procedure on the degradation of poly(lactide-co-glycolide) 85:15 and 50:50 implants. J. Control. Release 1997, 43, 161–173. [Google Scholar] [CrossRef]
- Kister, G.; Cassanas, G.; Vert, M. Structure and morphology of solid lactide-gly-colide copolymers from C-13 nmr, infra-red and Raman Spectroscopy. Polymers 1998, 39, 3335–3340. [Google Scholar] [CrossRef]
- Liao, S.; Watari, F.; Zhu, Y.; Uo, M.; Akasaka, T.; Wang, W. The degradation of the three layered nano-carbonated hydroxyapatite/collagen/PLGA composite membrane in vitro. Dent. Mater. 2007, 23, 1120–1128. [Google Scholar] [CrossRef] [PubMed]
- Zhou, J.; Cao, C.; Ma, X. A novel three-dimensional tubular scaffold prepared from silk fibroin by electrospinning. Int. J. Biol. Macromol. 2009, 45, 504–510. [Google Scholar] [CrossRef] [PubMed]
- Marelli, B.; Alessandrino, A.; Fare, S.; Freddi, G.; Mantovani, D. Compliant electrospun silk fibroin tubes for small vessel bypass grafting. Acta Biomater. 2010. in Press. [Google Scholar]
- Soffer, L.; Wang, X.; Zhang, X.; Kluge, J.; Dorfmann, L.; Kaplan, D.L.; Leisk, G. Silk-based electrospun tubular scaffolds for tissue-engineered vascular grafts. J. BioMater. Sci. Polym. Ed. 2008, 19, 653–664. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Baughman, C.B.; Kaplan, D.L. In vitro evaluation of electrospun silk fibroin scaffolds for vascular cell growth. Biomaterials 2008, 29, 2217–2227. [Google Scholar] [CrossRef] [PubMed]
- Li, C.; Vepari, C.; Jin, H.J.; Kim, H.J.; Kaplan, D.L. Electrospun silk-BMP-2 scaffolds for bone tissue engineering. Biomaterials 2006, 27, 3115–3124. [Google Scholar] [CrossRef] [PubMed]
- Seo, Y.-K.; Choi, G.-M.; Kwon, S.-Y.; Lee, H.-S.; Park, Y.-S.; Song, K.-Y.; Kim, Y.-J.; Park, J.-K. The biocompatibility of silk scaffold for tissue engineered ligaments. Key Eng. Mater. 2007, 342, 73–76. [Google Scholar] [CrossRef]
- Liu, H.; Fan, H.; Wang, Y.; Toh, S.L.; Goh, J.C.H. The interaction between a combined knitted silk scaffold and microporous silk sponge with human mesenchymal stem cells for ligament tissue engineering. Biomaterials 2008, 29, 662–674. [Google Scholar] [CrossRef] [PubMed]
© 2010 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Sell, S.A.; Wolfe, P.S.; Garg, K.; McCool, J.M.; Rodriguez, I.A.; Bowlin, G.L. The Use of Natural Polymers in Tissue Engineering: A Focus on Electrospun Extracellular Matrix Analogues. Polymers 2010, 2, 522-553. https://doi.org/10.3390/polym2040522
Sell SA, Wolfe PS, Garg K, McCool JM, Rodriguez IA, Bowlin GL. The Use of Natural Polymers in Tissue Engineering: A Focus on Electrospun Extracellular Matrix Analogues. Polymers. 2010; 2(4):522-553. https://doi.org/10.3390/polym2040522
Chicago/Turabian StyleSell, Scott A., Patricia S. Wolfe, Koyal Garg, Jennifer M. McCool, Isaac A. Rodriguez, and Gary L. Bowlin. 2010. "The Use of Natural Polymers in Tissue Engineering: A Focus on Electrospun Extracellular Matrix Analogues" Polymers 2, no. 4: 522-553. https://doi.org/10.3390/polym2040522
APA StyleSell, S. A., Wolfe, P. S., Garg, K., McCool, J. M., Rodriguez, I. A., & Bowlin, G. L. (2010). The Use of Natural Polymers in Tissue Engineering: A Focus on Electrospun Extracellular Matrix Analogues. Polymers, 2(4), 522-553. https://doi.org/10.3390/polym2040522