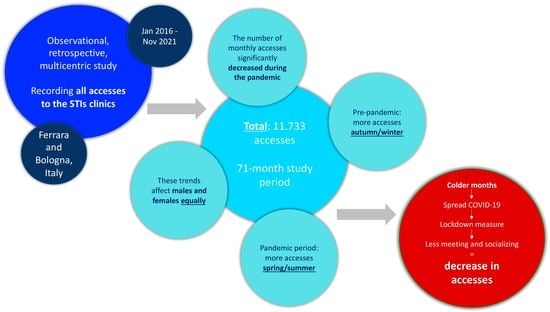
Visits to Sexually Transmitted Infection Clinics in Italy from January 2016 to November 2021: A Multicenter, Retrospective Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Setting
2.2. Population and Assessments
2.3. Statistical Analysis
3. Results
3.1. Study Population Features
3.2. Visits by Season
3.3. Further Variables Potentially Conditioning Accesses
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Garcia, M.R.; Leslie, S.W.; Wray, A.A. Sexually Transmitted Infections. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2022. Available online: http://www.ncbi.nlm.nih.gov/books/NBK560808/ (accessed on 14 December 2022).
- Unigwe, I.; Yang, S.; Song, H.J.; Lo-Ciganic, W.-H.; Hincapie-Castillo, J.; Cook, R.L.; Park, H. Trends in Sexually Transmitted Infections in United States Ambulatory Care Clinics from 2005–2016. J. Clin. Med. 2022, 11, 71. [Google Scholar] [CrossRef]
- Workowski, K.A.; Bolan, G.A.; Centers for Disease Control and Prevention. Sexually transmitted diseases treatment guidelines, 2015. Morb. Mortal. Wkly. Rep.: Recomm. Rep. 2015, 64, 1–137. [Google Scholar]
- Cegolon, L.; Bortolotto, M.; Bellizzi, S.; Cegolon, A.; Bubbico, L.; Pichierri, G.; Mastrangelo, G.; Xodo, C. A Survey on Knowledge, Prevention, and Occurrence of Sexually Transmitted Infections among Freshmen from Four Italian Universities. Int. J. Environ. Res. Public Health 2022, 19, 897. [Google Scholar] [CrossRef] [PubMed]
- Xu, X.; Ge, Z.; Chow, E.P.F.; Yu, Z.; Lee, D.; Wu, J.; Ong, J.J.; Fairley, C.K.; Zhang, L. A Machine-Learning-Based Risk-Prediction Tool for HIV and Sexually Transmitted Infections Acquisition over the Next 12 Months. J. Clin. Med. 2022, 11, 1818. [Google Scholar] [CrossRef] [PubMed]
- Salfa, M.; Ferri, M.; Suligoi, B.; Tagliaferro, L. Le Infezioni Sessualmente Trasmesse: Aggiornamento dei dati dei due Sistemi di sorveglianza sentinella attivi in Italia al 31 dicembre 2015. Ann. Ist. Super. Sanita 2017, 30, 3–27. [Google Scholar]
- European Centre for Disease Prevention and Control. Long-term Surveillance Strategy 2014–2020 (Revised). 2018. Available online: https://www.ecdc.europa.eu/en/publications-data/long-term-surveillance-strategy-2014-2020-revised (accessed on 14 December 2022).
- Cornelius, C.E., III. Seasonality of Gonorrhea in the United States. HSMHA Health Rep. 1971, 86, 157–160. [Google Scholar] [CrossRef] [Green Version]
- Wright, R.A.; Judson, F.N. Relative and seasonal incidences of the sexually transmitted diseases. A two-year statistical review. Br. J. Vener. Dis. 1978, 54, 433–440. [Google Scholar] [CrossRef] [Green Version]
- Schroeder, B.; Tetlow, P.; Sanfilippo, J.S.; Hertweck, S.P. Is There a Seasonal Variation in Gonorrhea and Chlamydia in Adolescents? J. Pediatr. Adolesc. Gynecol. 2001, 14, 25–27. [Google Scholar] [CrossRef]
- Ross, J.D.; Scott, G.R. Seasonal variation in gonorrhoea. Eur. J. Epidemiol. 1992, 8, 252–255. [Google Scholar] [CrossRef]
- Wellings, K.; Macdowall, W.; Catchpole, M.; Goodrich, J. Seasonal variations in sexual activity and their implications for sexual health promotion. J. R. Soc. Med. 1999, 92, 60–64. [Google Scholar] [CrossRef] [Green Version]
- Damiba, A.E.; Kelley, K.F.; Vermund, S.H. Rising trend of reported primary genital syphilis and genital ulcer disease in Burkina Faso. Int. J. Epidemiol. 1991, 20, 490–494. [Google Scholar] [CrossRef] [PubMed]
- Rodgers, J.L.; Harris, D.F.; Vickers, K.B. Seasonality of first coitus in the United States. Soc. Biol. 1992, 39, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Fortenberry, J.D.; Orr, D.P.; Zimet, G.D.; Blythe, M.J. Weekly and seasonal variation in sexual behaviors among adolescent women with sexually transmitted diseases. J. Adolesc. Health Off. Publ. Soc. Adolesc. Med. 1997, 20, 420–425. [Google Scholar] [CrossRef] [PubMed]
- Gamagedara, N.; Hocking, J.S.; Law, M.; Fehler, G.; Chen, M.Y.; Bradshaw, C.S.; Fairley, C.K. What are seasonal and meteorological factors are associated with the number of attendees at a sexual health service? An observational study between 2002–2012. Sex. Transm. Infect. 2014, 90, 635–640. [Google Scholar] [CrossRef]
- Bezzini, D.; Schiavetti, I.; Manacorda, T.; Franzone, G.; Battaglia, M.A. First Wave of COVID-19 Pandemic in Italy: Data and Evidence. Adv. Exp. Med. Biol. 2021, 1353, 91–113. [Google Scholar]
- Eddy, C.M. The social impact of COVID-19 as perceived by the employees of a UK mental health service. Int. J. Ment. Health Nurs. 2021, 30, 1366–1375. [Google Scholar] [CrossRef]
- Medda, E.; Gigantesco, A.; Picardi, A.; Carluccio, E.; D’Ippolito, C.; Ferri, M.; Brescianini, S.; Toccaceli, V.; Stazi, M.A. The COVID-19 pandemic in Italy: The impact on social life and mental health. Riv. Psichiatr. 2021, 56, 182–188. [Google Scholar]
- Kondo, K.K.; Williams, B.E.; Ayers, C.K.; Kansagara, D.; Smith, M.; Advani, S.M.; Young, S.; Somnath, S. Factors Associated with Health Inequalities in Infectious Disease Pandemics Predating COVID-19 in the United States: A Systematic Review. Health Equity 2022, 6, 254–269. [Google Scholar] [CrossRef]
- Tan, R.K.J.; Michielsen, K.; Campbell, L.; Tucker, J.D. Sexual and reproductive health during COVID-19—The I-SHARE multi-country survey. Nat. Rev. Urol. 2022, 19, 325–326. [Google Scholar] [CrossRef]
- Gaspari, V.; Orioni, G.; Viviani, F.; Raone, B.; Lanzoni, A.; Bardazzi, F. Does COVID-19 influence sexual behaviors? Dermatol. Ther. 2020, 33, e14004. [Google Scholar] [CrossRef]
- Ryu, H.; Blaque, E.; Stewart, M.; Anand, P.; Gómez-Ramírez, O.; MacKinnon, K.R.; Worthington, C.; Gilbert, M.; Grace, D. Disruptions of sexually transmitted and blood borne infections testing services during the COVID-19 pandemic: Accounts of service providers in Ontario, Canada. BMC Health Serv. Res. 2023, 23, 29. [Google Scholar] [CrossRef] [PubMed]
- de la Court, F.; Boyd, A.; Coyer, L.; Elshout, M.V.D.; de Vries, H.J.C.; Matser, A.; Hoornenborg, E.; Prins, M. The impact of COVID-19-related restrictions in 2020 on sexual healthcare use, pre-exposure prophylaxis use, and sexually transmitted infection incidence among men who have sex with men in Amsterdam, the Netherlands. HIV Med. 2023, 24, 212–223. [Google Scholar] [CrossRef] [PubMed]
- De Giorgi, A.; Storari, A.; Rodríguez-Muñoz, P.M.; Cappadona, R.; Lamberti, N.; Manfredini, F.; López-Soto, P.J.; Manfredini, R.; Fabbian, F. Seasonal pattern in elderly hospitalized with acute kidney injury: A retrospective nationwide study in Italy. Int. Urol. Nephrol. 2022, 54, 3243–3253. [Google Scholar] [CrossRef] [PubMed]
- Gallerani, M.; Manfredini, R. Seasonal variation in the occurrence of delirium in patients admitted to medical units of a general hospital in Italy. Acta Neuropsychiatr. 2013, 25, 179–183. [Google Scholar] [CrossRef]
- Manfredini, R.; Boari, B.; Manfredini, F.; Salmi, R.; Bossone, E.; Fabbri, D.; Contato, E.; Mascoli, F.; Gallerani, M. Seasonal variation in occurrence of aortic diseases: The database of hospital discharge data of the Emilia-Romagna region, Italy. J. Thorac. Cardiovasc. Surg. 2008, 135, 442–444. [Google Scholar] [CrossRef] [Green Version]
- Gallerani, M.; Boari, B.; Smolensky, M.H.; Salmi, R.; Fabbri, D.; Contato, E.; Manfredini, R. Seasonal variation in occurrence of pulmonary embolism: Analysis of the database of the Emilia-Romagna region, Italy. Chronobiol. Int. 2007, 24, 143–160. [Google Scholar] [CrossRef]
- Manfredini, R.; Imberti, D.; Gallerani, M.; Verso, M.; Pistelli, R.; Ageno, W.; Agnelli, G. Seasonal variation in the occurrence of venous thromboembolism: Data from the MASTER Registry. Clin. Appl. Thromb. Hemost. 2009, 15, 309–315. [Google Scholar] [CrossRef]
- Manfredini, R.; Manfredini, F.; Boari, B.; Bergami, E.; Mari, E.; Gamberini, S.; Salmi, R.; Gallerani, M. Seasonal and weekly patterns of hospital admissions for nonfatal and fatal myocardial infarction. Am. J. Emerg. Med. 2009, 27, 1097–1103. [Google Scholar] [CrossRef]
- Manfredini, R.; Manfredini, F.; Boari, B.; Malagoni, A.M.; Gamberini, S.; Salmi, R.; Gallerani, M. Temporal patterns of hospital admissions for transient ischemic attack: A retrospective population-based study in the Emilia-Romagna region of Italy. Clin. Appl. Thromb. Hemost. 2010, 16, 153–160. [Google Scholar] [CrossRef]
- Gallerani, M.; Boari, B.; Manfredini, F.; Manfredini, R. Seasonal variation in heart failure hospitalization. Clin. Cardiol. 2011, 34, 389–394. [Google Scholar] [CrossRef]
- Manfredini, R.; Fabbian, F.; Pala, M.; Tiseo, R.; De Giorgi, A.; Manfredini, F.; Malagoni, A.M.; Signani, F.; Andreati, C.; Boari, B.; et al. Seasonal and weekly patterns of occurrence of acute cardiovascular diseases: Does a gender difference exist? J. Womens Health 2011, 20, 1663–1668. [Google Scholar] [CrossRef] [PubMed]
- Salvi, F.; Bartolomei, I.; Smolensky, M.H.; Lorusso, A.; Barbarossa, E.; Malagoni, A.M.; Zamboni, P.; Manfredini, R. A seasonal periodicity in relapses of multiple sclerosis? A single-center, population-based, preliminary study conducted in Bologna, Italy. BMC Neurol. 2010, 10, 105. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Manfredini, R.; De Giorgio, R.; Smolensky, M.H.; Boari, B.; Salmi, R.; Fabbri, D.; Contato, E.; Serra, M.; Barbara, G.; Stanghellini, V.; et al. Seasonal pattern of peptic ulcer hospitalizations: Analysis of the hospital discharge data of the Emilia-Romagna region of Italy. BMC Gastroenterol. 2010, 10, 37. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Manfredini, R.; Vergine, G.; Boari, B.; Faggioli, R.; Borgna-Pignatti, C. Circadian and seasonal variation of first febrile seizures. J. Pediatr. 2004, 145, 838–839. [Google Scholar] [CrossRef] [PubMed]
- Gallerani, M.; Boari, B.; Salmi, R.; Manfredini, R. Seasonal variation in the onset of acute pancreatitis. World J. Gastroenterol. 2004, 10, 3328–3331. [Google Scholar] [CrossRef]
- Manfredini, R.; Gallerani, M.; Portaluppi, F. Seasonal variation in the occurrence of epistaxis. Am. J. Med. 2000, 108, 759–760. [Google Scholar] [CrossRef]
- Gallerani, M.; Manfredini, R. Seasonal variation in herpes zoster infection. Br. J. Dermatol. 2000, 142, 588–589. [Google Scholar] [CrossRef]
- Gallerani, M.; Govoni, M.; Mucinelli, M.; Bigoni, M.; Trotta, F.; Manfredini, R. Seasonal variation in the onset of acute microcrystalline arthritis. Rheumatology 1999, 38, 1003–1006. [Google Scholar] [CrossRef] [Green Version]
- Gallerani, M.; Delli Gatti, C.; Salmi, R.; Kuwornu Afi, H.; la Cecilia, O.; Manfredini, R. Seasonal variations in the incidence of cranial nerve paralysis. J. Int. Med. Res. 1999, 27, 130–133. [Google Scholar] [CrossRef] [Green Version]
- Soriani, S.; Fiumana, E.; Manfredini, R.; Boari, B.; Battistella, P.A.; Canetta, E.; Pedretti, S.; Borgna-Pignatti, C. Circadian and seasonal variation of migraine attacks in children. Headache 2006, 46, 1571–1574. [Google Scholar] [CrossRef]
- Degli Atti, M.C.; Rizzo, C.; D’Amore, C.; Ravà, L.; Reale, A.; Barbieri, M.A.; Bernaschi, P.; Russo, C.; Villani, A.; Perno, C.F.; et al. Acute respiratory infection emergency access in a tertiary care children hospital in Italy, prior and after the SARS-CoV-2 emergence. Influenza Other Respir. Viruses 2023, 17, e13102. [Google Scholar] [CrossRef]
- Demotier, S.; Gornet, M.; Belli, A.; Huguenin, A.; N’Guyen, Y. Malaria diagnosis in an emergency department before and after the COVID-19 pandemic: A retrospective study. Trans. R. Soc. Trop. Med. Hyg. 2023, 117, 64–66. [Google Scholar] [CrossRef]
- Rodríguez-Cortés, F.J.; Jiménez-Hornero, J.E.; Alcalá-Diaz, J.F.; Moral, R.M.M.-D.; Romero-Cabrera, J.L.; Manfredini, R.; Rodríguez-Borrego, M.A.; López-Soto, P.J. COVID-19 pandemic on coronary artery and cerebrovascular diseases in Southern Spain: Interrupted time series analysis. Eur. Rev. Med. Pharmacol. Sci. 2023, 27, 3208–3217. [Google Scholar] [CrossRef] [PubMed]
- Popovic, M.; Fiano, V.; Moirano, G.; Chiusa, L.; Conway, D.I.; Demo, P.G.; Gilardetti, M.; Iorio, G.C.; Moccia, C.; Ostellino, O.; et al. The Impact of the COVID-19 Pandemic on Head and Neck Cancer Diagnosis in the Piedmont Region, Italy: Interrupted Time-Series Analysis. Front. Public Health 2022, 10, 809283. [Google Scholar] [CrossRef]
- Linjawi, M.; Shakoor, H.; Hilary, S.; Ali, H.I.; Al-Dhaheri, A.S.; Ismail, L.C.; Apostolopoulos, V.; Stojanovska, L. Cancer Patients during COVID-19 Pandemic: A Mini-Review. Healthcare 2023, 11, 248. [Google Scholar] [CrossRef]
- Hacker, K.A.; Briss, P.A.; Richardson, L.; Wright, J.; Petersen, R. COVID-19 and Chronic Disease: The Impact Now and in the Future. Prev. Chronic Dis. 2021, 18, E62. [Google Scholar] [CrossRef] [PubMed]
- Reschen, M.E.; Bowen, J.; Novak, A.; Giles, M.; Singh, S.; Lasserson, D.; O’callaghan, C.A. Impact of the COVID-19 pandemic on emergency department attendances and acute medical admissions. BMC Emerg. Med. 2021, 21, 143. [Google Scholar] [CrossRef] [PubMed]
- Czeisler, M.; Marynak, K.; Clarke, K.E.; Salah, Z.; Shakya, I.; Thierry, J.M.; Ali, N.; McMillan, H.; Wiley, J.F.; Weaver, M.D.; et al. Delay or Avoidance of Medical Care Because of COVID-19-Related Concerns—United States, June 2020. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 1250–1257. [Google Scholar] [CrossRef]
- Li, T.; Nickel, B.; Ngo, P.; McFadden, K.; Brennan, M.; Marinovich, M.L.; Houssami, N. A systematic review of the impact of the COVID-19 pandemic on breast cancer screening and diagnosis. Breast 2023, 67, 78–88. [Google Scholar] [CrossRef]
- Mazidimoradi, A.; Hadavandsiri, F.; Momenimovahed, Z.; Salehiniya, H. Impact of the COVID-19 Pandemic on Colorectal Cancer Diagnosis and Treatment: A Systematic Review. J. Gastrointest. Cancer 2021. Epub ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Maddock, J.; Parsons, S.; Gessa, G.D.; Green, M.J.; Thompson, E.J.; Stevenson, A.J.; Kwong, A.S.; McElroy, E.; Santorelli, G.; Silverwood, R.J.; et al. Inequalities in healthcare disruptions during the COVID-19 pandemic: Evidence from 12 UK population-based longitudinal studies. BMJ Open 2022, 12, e064981. [Google Scholar] [CrossRef] [PubMed]
- Topriceanu, C.C.; Wong, A.; Moon, J.C.; Hughes, A.D.; Bann, D.; Chaturvedi, N.; Patalay, P.; Conti, G.; Captur, G. Evaluating access to health and care services during lockdown by the COVID-19 survey in five UK national longitudinal studies. BMJ Open 2021, 11, e045813. [Google Scholar] [CrossRef] [PubMed]
- Dema, E.; Gibbs, J.; Clifton, S.; Copas, A.J.; Tanton, C.; Riddell, J.; Pérez, R.B.; Reid, D.; Bonell, C.; Unemo, M.; et al. Initial impacts of the COVID-19 pandemic on sexual and reproductive health service use and unmet need in Britain: Findings from a quasi-representative survey (Natsal-COVID). Lancet Public Health 2022, 7, e36–e47. [Google Scholar] [CrossRef] [PubMed]
- Dema, E.; Sonnenberg, P.; Gibbs, J.; Conolly, A.; Willis, M.; Riddell, J.; Pérez, R.B.; Copas, A.J.; Tanton, C.; Bonell, C.; et al. How did the COVID-19 pandemic affect access to condoms, chlamydia and HIV testing, and cervical cancer screening at a population level in Britain? (Natsal-COVID). In Sex Transm Infect; BMJ Publishing: London, UK, 2022; Available online: https://sti.bmj.com/content/early/2022/08/17/sextrans-2022-055516 (accessed on 26 February 2023).

| Overall | Pre-Pandemic Period | Pandemic Period | p * | |
|---|---|---|---|---|
| N = 11,733 | N = 8484 | N = 3249 | ||
| Mean age in years (SD) | 34.5 (12.8) | 34.2 (12.4) | 35.3 (13.7) | <0.001 |
| Age class, % (n) | ||||
| - <20 yrs | 3.1 (361) | 3.1 (267) | 2.9 (94) | 0.6 |
| - 20–29 yrs | 42.2 (4950) | 42.5 (3605) | 41.4 (1345) | 0.3 |
| - 30–39 yrs | 23.9 (2800) | 23.7 (2009) | 24.3 (791) | 0.4 |
| - 40–49 yrs | 17.8 (2092) | 18.7 (1588) | 15.5 (504) | <0.01 |
| - 50–59 yrs | 8.4 (980) | 8.0 (678) | 9.3 (302) | 0.02 |
| - ≥60 yrs | 4.6 (550) | 4.0 (337) | 6.6 (213) | <0.001 |
| <0.001 | ||||
| Male gender, % (n) | 63.7 (7478) | 64.8 (5494) | 61.1 (1984) | |
| Female gender, % (n) | 36.3 (4255) | 35.2 (2990) | 38.9 (1265) | |
| Nationality, % (n) | <0.001 | |||
| - Italian | 82.3 (9656) | 81.1 (6877) | 85.5 (2779) | |
| - Others | 17.7 (2077) | 18.9 (1607) | 14.5 (470) | |
| Season, % (n) | ||||
| - Spring | 25.2 (2954) | 22.9 (1942) | 31.1 (1012) | <0.001 |
| - Summer | 25.0 (2934) | 22.2 (1886) | 32.3 (1048) | <0.001 |
| - Autumn | 25.2 (2953) | 26.0 (2205) | 23.0 (748) | <0.001 |
| - Winter | 24.6 (2892) | 28.9 (2451) | 13.6 (441) | <0.001 |
| b, c, d, e | b, c, d, e |
| Overall | Pre-Pandemic Period | Pandemic Period | p * | |
|---|---|---|---|---|
| N = 7478 | N = 5494 | N = 1984 | ||
| Mean age in years (SD) | 36.1 (12.5) | 36.1 (12.4) | 36.3 (12.9) | 0.5 |
| Age class, % (n) | ||||
| - <20 yrs | 2.3 (173) | 2.5 (135) | 1.9 (38) | 0.13 |
| - 20–29 yrs | 35.7 (2673) | 35.3 (1940) | 37.0 (733) | 0.2 |
| - 30–39 yrs | 25.0 (1872) | 24.9 (1365) | 25.6 (507) | 0.5 |
| - 40–49 yrs | 22.4 (1671) | 23.5 (1293) | 19.1 (378) | 0.001 |
| - 50–59 yrs | 9.6 (721) | 9.3 (511) | 10.6 (210) | 0.09 |
| - ≥60 yrs | 4.9 (368) | 4.6 (250) | 6.0 (118) | 0.014 |
| Nationality, % (n) | 0.7 | |||
| - Italian | 14.1 (1054) | 14.2 (780) | 13.8 (274) | |
| - Others | 85.9 (6424) | 85.8 (4714) | 86.2 (1710) | |
| Season, % (n) | ||||
| - Spring | 25.5 (1910) | 23.4 (1283) | 31.6 (627) | <0.001 |
| - Summer | 25.2 (1877) | 22.6 (1241) | 32.1 (636) | <0.001 |
| - Autumn | 25.2 (1886) | 25.8 (1417) | 23.6 (469) | 0.053 |
| - Winter | 24.1 (1805) | 28.3 (1553) | 12.7 (252) | <0.001 |
| b, c, d, e | b, c, d, e |
| Overall | Pre-Pandemic Period | Pandemic Period | p * | |
|---|---|---|---|---|
| N = 4255 | N = 2990 | N = 1265 | ||
| Mean age in years (SD) | 31.6 (12.7) | 30.8 (11.7) | 33.6 (14.7) | <0.001 |
| Age class, % (n) | ||||
| - <20 yrs | 4.4 (188) | 4.4 (132) | 4.4 (56) | 0.9 |
| - 20–29 yrs | 53.5 (2277) | 55.7 (1665) | 48.4 (612) | <0.001 |
| - 30–39 yrs | 21.8 (928) | 21.5 (644) | 22.5 (284) | 0.5 |
| - 40–49 yrs | 9.9 (421) | 9.9 (295) | 10.0 (126) | 0.9 |
| - 50–59 yrs | 6.1 (259) | 5.6 (167) | 7.3 (92) | 0.03 |
| - ≥60 yrs | 4.3 (182) | 2.9 (87) | 7.4 (95) | <0.001 |
| Nationality, % (n) | <0.001 | |||
| - Italian | 24.0 (1023) | 27.7 (827) | 15.5 (196) | |
| - Others | 75.9 (3232) | 72.3 (2163) | 84.5 (1096) | |
| Season, % (n) | ||||
| - Spring | 24.5 (1044) | 22.0 (659) | 30.4 (385) | <0.001 |
| - Summer | 24.8 (1057) | 21.6 (645) | 32.6 (412) | <0.001 |
| - Autumn | 25.1 (1067) | 26.4 (788) | 22.1 (279) | 0.003 |
| - Winter | 25.6 (1087) | 30.3 (898) | 14.9 (189) | <0.001 |
| b, c, d, e | b, c, d, e |
| Variables | Regression Coeff. (95% CI) | p |
|---|---|---|
| Pandemic vs. pre-pandemic period * | −16.3 (−18.9; −13.8) | <0.001 |
| Males vs. females | −2.19 (−4.62; 0.24) | 0.08 |
| Age-class: | ||
| - <20 yrs | 0 (ref. cat.) | -- |
| - 20–29 yrs | 4.12 (−2.57; 10.8) | 0.2 |
| - 30–39 yrs | 3.12 (−3.76; 10.0) | 0.4 |
| - 40–49 yrs | 3.91 (−3.14; 10.9) | 0.3 |
| - 50–59 yrs | 4.66 (−2.93; 12.3) | 0.2 |
| - ≥60 yrs | −2.30 (−10.; 6.01) | 0.6 |
| Season: | ||
| - Spring | 0 (ref. cat.) | -- |
| - Summer | −7.72 (−10.9; −4.52) | <0.001 |
| - Autumn | −2.30 (−5.50; 0.90) | 0.2 |
| - Winter | 7.04 (3.79; 10.3) | <0.001 |
| Foreign vs. Italian nationality | −1.06 (−4.08; 1.94) | 0.5 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Borghi, A.; Flacco, M.E.; Pacetti, L.; Orioni, G.; Marzola, E.; Cultrera, R.; Guerra, V.; Manfredini, R.; Gaspari, V.; Segala, D.; et al. Visits to Sexually Transmitted Infection Clinics in Italy from January 2016 to November 2021: A Multicenter, Retrospective Study. J. Pers. Med. 2023, 13, 731. https://doi.org/10.3390/jpm13050731
Borghi A, Flacco ME, Pacetti L, Orioni G, Marzola E, Cultrera R, Guerra V, Manfredini R, Gaspari V, Segala D, et al. Visits to Sexually Transmitted Infection Clinics in Italy from January 2016 to November 2021: A Multicenter, Retrospective Study. Journal of Personalized Medicine. 2023; 13(5):731. https://doi.org/10.3390/jpm13050731
Chicago/Turabian StyleBorghi, Alessandro, Maria Elena Flacco, Lucrezia Pacetti, Gionathan Orioni, Elisa Marzola, Rosario Cultrera, Valentina Guerra, Roberto Manfredini, Valeria Gaspari, Daniela Segala, and et al. 2023. "Visits to Sexually Transmitted Infection Clinics in Italy from January 2016 to November 2021: A Multicenter, Retrospective Study" Journal of Personalized Medicine 13, no. 5: 731. https://doi.org/10.3390/jpm13050731
APA StyleBorghi, A., Flacco, M. E., Pacetti, L., Orioni, G., Marzola, E., Cultrera, R., Guerra, V., Manfredini, R., Gaspari, V., Segala, D., & Corazza, M. (2023). Visits to Sexually Transmitted Infection Clinics in Italy from January 2016 to November 2021: A Multicenter, Retrospective Study. Journal of Personalized Medicine, 13(5), 731. https://doi.org/10.3390/jpm13050731