Numerical and Experimental Investigations of Humeral Greater Tuberosity Fractures with Plate Fixation under Different Shoulder Rehabilitation Activities
Abstract
:1. Introduction
2. Materials and Methods
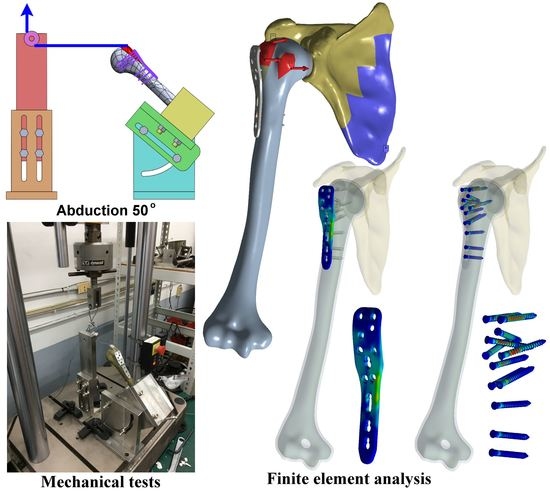
2.1. Numerical Modeling of Humerus GT Fracture with Plate Fixation under Mechanical Testing Loading
2.2. Mechanical Tests of Shoulder Rehabilitation Activities
2.3. Statistical Analysis
2.4. Numerical Modeling of Injured Shoulder Joint with Plate Fixation under Realistic Rotator Cuff Muscle Loading
3. Results
3.1. Finite Element Simulation under Mechanical Testing Loadings
3.2. Mechanical Testing Outcomes
3.3. Finite Element Simulation under the Realistic Rotator Cuff Muscle Loading
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gruson, K.I.; Ruchelsman, D.E.; Tejwani, N. Isolated tuberosity fractures of the proximal humerus: Current concepts. Injury 2008, 39, 284–298. [Google Scholar] [CrossRef] [PubMed]
- Mutch, J.; Laflamme, G.Y.; Hagemeister, N.; Cikes, A.; Rouleau, D.M. A new morphological classification for greater tuberosity fractures of the proximal humerus: Validation and clinical implications. Bone Jt. J. 2014, 96-B, 646–651. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bogdan, Y.; Gausden, E.B.; Zbeda, R.; Helfet, D.L.; Lorich, D.G.; Wellman, D.S. An alternative technique for greater tuberosity fractures: Use of the mesh plate. Arch. Orthop. Trauma. Surg. 2017, 137, 1067–1070. [Google Scholar] [CrossRef] [PubMed]
- Gillespie, R.J.; Johnston, P.S.; Gordon, V.A.; Ward, P.J.; Getz, C.L. Using Plate Osteosynthesis to Treat Isolated Greater Tuberosity Fractures. Am. J. Orthop. 2015, 44, E248–E251. [Google Scholar]
- Ma, J.; Zhao, L.; Liu, T.; Fu, Q.; Chen, A. A Retrospective Study in the Treatment of a 2-Part Greater Tuberosity Fracture Using the F3 Biomet Plate. Int. Surg. 2016, 101, 465–472. [Google Scholar] [CrossRef] [Green Version]
- Park, S.-E.; Jeong, J.-J.; Panchal, K.; Lee, J.-Y.; Min, H.-K.; Ji, J.-H. Arthroscopic-assisted plate fixation for displaced large-sized comminuted greater tuberosity fractures of proximal humerus: A novel surgical technique. Knee Surg. Sports Traumatol. Arthrosc. 2016, 24, 3892–3898. [Google Scholar] [CrossRef]
- Ji, J.-H.; Shafi, M.; Song, I.-S.; Kim, Y.-Y.; McFarland, E.G.; Moon, C.-Y. Arthroscopic Fixation Technique for Comminuted, Displaced Greater Tuberosity Fracture. Arthrosc. J. Arthrosc. Relat. Surg. 2010, 26, 600–609. [Google Scholar] [CrossRef]
- Brais, G.; Ménard, J.; Mutch, J.; Laflamme, G.-Y.; Petit, Y.; Rouleau, D.M. Transosseous braided-tape and double-row fixations are better than tension band for avulsion-type greater tuberosity fractures. Injury 2015, 46, 1007–1012. [Google Scholar] [CrossRef]
- Gaudelli, C.; Ménard, J.; Mutch, J.; Laflamme, G.-Y.; Petit, Y.; Rouleau, D.M. Locking plate fixation provides superior fixation of humerus split type greater tuberosity fractures than tension bands and double row suture bridges. Clin. Biomech. 2014, 29, 1003–1008. [Google Scholar] [CrossRef]
- Knierzinger, D.; Heinrichs, C.H.; Hengg, C.; Konschake, M.; Kralinger, F.; Schmoelz, W. Biomechanical evaluation of cable and suture cerclages for tuberosity reattachment in a 4-part proximal humeral fracture model treated with reverse shoulder arthroplasty. J. Shoulder Elb. Surg. 2018, 27, 1816–1823. [Google Scholar] [CrossRef]
- Lin, C.-L.; Yeh, M.-L.; Su, F.-C.; Wang, Y.-C.; Chiang, C.H.; Hong, C.-K.; Su, W.-R. Different suture anchor fixation techniques affect contact properties in humeral greater tuberosity fracture: A biomechanical study. BMC Musculoskelet. Disord. 2019, 20, 26. [Google Scholar] [CrossRef]
- Mihata, T.; Fukuhara, T.; Jun, B.J.; Watanabe, C.; Kinoshita, M. Effect of Shoulder Abduction Angle on Biomechanical Properties of the Repaired Rotator Cuff Tendons With 3 Types of Double-Row Technique. Am. J. Sports Med. 2010, 39, 551–556. [Google Scholar] [CrossRef] [PubMed]
- Palumbo, B.T.; Gutierrez, S.; Santoni, B.; Mighell, M. Biomechanical Investigation of Locked Plate Fixation with Suture Augmentation in a Comminuted Three-Part Proximal Humerus Fracture Model. Open J. Orthop. 2017, 7, 180–191. [Google Scholar] [CrossRef] [Green Version]
- St-Jean, B.L.; Ménard, J.; Hinse, S.; Petit, Y.; Rouleau, D.M.; Beauchamp, M. Braided tape suture provides superior bone pull-through strength than wire suture in greater tuberosity of the humerus. J. Orthop. 2015, 12, S14–S17. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Feerick, E.M.; Kennedy, J.; Mullett, H.; FitzPatrick, D.; McGarry, P. Investigation of metallic and carbon fibre PEEK fracture fixation devices for three-part proximal humeral fractures. Med. Eng. Phys. 2013, 35, 712–722. [Google Scholar] [CrossRef]
- Fletcher, J.W.A.; Windolf, M.; Richards, R.G.; Gueorguiev, B.; Buschbaum, J.; Varga, P. Importance of locking plate positioning in proximal humeral fractures as predicted by computer simulations. J. Orthop. Res. 2019, 37, 957–964. [Google Scholar] [CrossRef]
- Shen, L.; Zhang, W.; Wang, Q.; Chen, Y. Establishment of a three-dimensional finite element model and biomechanical analysis of three different internal fixation methods for humeral greater tuberosity fracture. Int. J. Clin. Exp. Med. 2018, 11, 3245–3254. [Google Scholar]
- Varga, P.; Inzana, J.A.; Gueorguiev, B.; Südkamp, N.P.; Windolf, M. Validated computational framework for efficient systematic evaluation of osteoporotic fracture fixation in the proximal humerus. Med. Eng. Phys. 2018, 57, 29–39. [Google Scholar] [CrossRef]
- Burke, N.G.; Kennedy, J.; Cousins, G.; FitzPatrick, D.; Mullett, H. Locking Plate Fixation with and without Inferomedial Screws for Proximal Humeral Fractures: A Biomechanical Study. J. Orthop. Surg. 2014, 22, 190–194. [Google Scholar] [CrossRef] [Green Version]
- Lee, C.-H.; Hsu, C.-C.; Huang, P.-Y. Biomechanical study of different fixation techniques for the treatment of sacroiliac joint injuries using finite element analyses and biomechanical tests. Comput. Biol. Med. 2017, 87, 250–257. [Google Scholar] [CrossRef]
- Osterhoff, G.; Baumgartner, D.; Favre, P.; Wanner, G.A.; Gerber, H.; Simmen, H.-P.; Werner, C.M. Medial support by fibula bone graft in angular stable plate fixation of proximal humeral fractures: An in vitro study with synthetic bone. J. Shoulder Elb. Surg. 2011, 20, 740–746. [Google Scholar] [CrossRef] [PubMed]
- Ausiello, P.; Ciaramella, S.; Di Rienzo, A.; Lanzotti, A.; Ventre, M.; Watts, D.C. Adhesive class I restorations in sound molar teeth incorporating combined resin-composite and glass ionomer materials: CAD-FE modeling and analysis. Dent. Mater. 2019, 35, 1514–1522. [Google Scholar] [CrossRef] [PubMed]
- Campaner, L.M.; Silveira, M.P.M.; de Andrade, G.S.; Borges, A.L.S.; Bottino, M.A.; de OliveiraDal Piva, A.M.; Lo Giudice, R.; Ausiello, P.; Tribst, J.P.M. Influence of polymeric restorative materials on the stress distribution in posterior fixed partial dentures: 3D finite element analysis. Polymers 2021, 13, 758. [Google Scholar] [CrossRef] [PubMed]
- Parizi, F.S.; Mehrabi, R.; Karamooz-Ravari, M.R. Finite element analysis of NiTi self-expandable heart valve stent. Proc. Inst. Mech. Eng. Part H J. Eng. Med. 2019, 233, 1042–1050. [Google Scholar] [CrossRef]
- Ye, Y.; You, W.; Zhu, W.; Cui, J.; Chen, K.; Wang, D. The Applications of Finite Element Analysis in Proximal Humeral Fractures. Comput. Math. Methods Med. 2017, 2017, 4879836. [Google Scholar] [CrossRef]
- Wu, W.; Lee, P.V.; Bryant, A.L.; Galea, M.; Ackland, D.C. Subject-specific musculoskeletal modeling in the evaluation of shoulder muscle and joint function. J. Biomech. 2016, 49, 3626–3634. [Google Scholar] [CrossRef]
- Lin, C.-L.; Su, F.-C.; Chang, C.-H.; Hong, C.-K.; Jou, I.-M.; Lin, C.-J.; Su, W.-R. Effect of shoulder abduction on the fixation of humeral greater tuberosity fractures: A biomechanical study for three types of fixation constructs. J. Shoulder Elb. Surg. 2015, 24, 547–554. [Google Scholar] [CrossRef]
- Curtis, A.S.; Burbank, K.M.; Tierney, J.J.; Scheller, A.D.; Curran, A.R. The Insertional Footprint of the Rotator Cuff: An Anatomic Study. Arthrosc. J. Arthrosc. Relat. Surg. 2006, 22, 603–609. [Google Scholar] [CrossRef]







| Rehabilitation Movement | Position (°) | Displacement at Fracture Site (mm) | Max. Bone Stress (MPa) | Max. Plate Stress (MPa) | Mean Screw Stress (MPa) |
|---|---|---|---|---|---|
| Abduction | 15 | 0.144 | 15.8 | 10.8 | 15.6 |
| 40 | 0.133 | 23.8 | 13.1 | 24.4 | |
| 65 | 0.075 | 22.2 | 12.1 | 22.0 | |
| 90 | 0.208 | 17.1 | 7.6 | 13.7 | |
| Flexion | 15 | 0.155 | 19.6 | 12.7 | 17.5 |
| 40 | 0.338 | 25.1 | 14.1 | 23.5 | |
| 65 | 0.573 | 23.4 | 17.8 | 21.3 | |
| 90 | 0.450 | 31.5 | 18.6 | 21.7 | |
| Horizontal flexion | 35 | 0.491 | 40.5 | 14.8 | 12.6 |
| 50 | 1.022 | 60.6 | 29.1 | 37.3 | |
| 70 | 1.163 | 56.1 | 29.0 | 34.0 | |
| 90 | 0.486 | 33.0 | 16.4 | 21.2 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Muthusamy, B.; Chao, C.-K.; Hsu, C.-C.; Lin, M.-H. Numerical and Experimental Investigations of Humeral Greater Tuberosity Fractures with Plate Fixation under Different Shoulder Rehabilitation Activities. Appl. Sci. 2022, 12, 6802. https://doi.org/10.3390/app12136802
Muthusamy B, Chao C-K, Hsu C-C, Lin M-H. Numerical and Experimental Investigations of Humeral Greater Tuberosity Fractures with Plate Fixation under Different Shoulder Rehabilitation Activities. Applied Sciences. 2022; 12(13):6802. https://doi.org/10.3390/app12136802
Chicago/Turabian StyleMuthusamy, Balraj, Ching-Kong Chao, Ching-Chi Hsu, and Meng-Hua Lin. 2022. "Numerical and Experimental Investigations of Humeral Greater Tuberosity Fractures with Plate Fixation under Different Shoulder Rehabilitation Activities" Applied Sciences 12, no. 13: 6802. https://doi.org/10.3390/app12136802
APA StyleMuthusamy, B., Chao, C. -K., Hsu, C. -C., & Lin, M. -H. (2022). Numerical and Experimental Investigations of Humeral Greater Tuberosity Fractures with Plate Fixation under Different Shoulder Rehabilitation Activities. Applied Sciences, 12(13), 6802. https://doi.org/10.3390/app12136802