Changes in Phonation and Their Relations with Progress of Parkinson’s Disease
Abstract
:1. Introduction
- to identify phonatory acoustic features at baseline that are significantly correlated with changes in various clinical rating scales,
- to investigate relationship between changes in the phonatory acoustic features and the clinical rating scales after the two-year follow-up,
- to establish mathematical models that will estimate the change in clinical rating scales based on the change in acoustic measures,
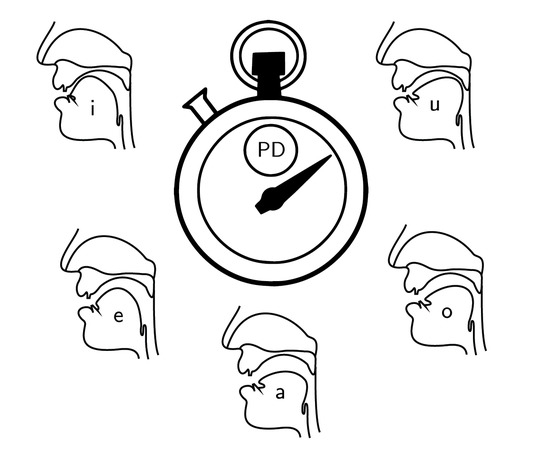
- to compare results based on five vowels: /a/, /e/, /i/, /o/, /u/.
2. Materials and Methods
2.1. Dataset
2.2. Vocal Tasks
2.3. Acoustic Features
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| ACE-R | Addenbrooke’s cognitive examination-revised |
| APQ | amplitude perturbation quotient |
| CV | coefficient of variation |
| EER | estimation error rate |
| ER | energy ratio |
| F0 | fundamental frequency |
| Fi | ith formant |
| FLUF | fraction of locally unvoiced frames |
| FOG | freezing of gait |
| FOG-Q | freezing of gait questionnaire |
| GNE | glottal-to-noise excitation ratio |
| HD | hypokinetic dysarthria |
| HNR | harmonic-to-noise ratio |
| LED | L-dopa equivalent daily dose |
| MAE | mean absolute error |
| NNE | normalized noise energy |
| PD | Parkinson’s disease |
| PPQ | period perturbation quotient |
| Q2 | second quartile (median) |
| RBDSQ | REM sleep behavior disorder screening questionnaire |
| SD | standard deviation |
| TKEO | Teager–Kaiser energy operator |
| UPDRS III | Unified Parkinson’s disease rating scale, part III: evaluation of motor functions |
| UPDRS IV | Unified Parkinson’s disease rating scale, part IV: evaluation of complications of therapy |
References
- Hornykiewicz, O. Biochemical aspects of Parkinson’s disease. Neurology 1998, 51, S2–S9. [Google Scholar] [CrossRef] [PubMed]
- Hoehn, M.M.; Yahr, M.D. Parkinsonism: Onset, Progression, and Mortality. Neurology 1967, 17, 427–442. [Google Scholar] [CrossRef] [PubMed]
- Fahn, S.; Elton, R.L. UPDRS Development Committee (1987) Unified Parkinson’s Disease Rating Scale; Recent Developments in Parkinson’s Disease; Macmillan: Florham Park, NJ, USA, 1987. [Google Scholar]
- Giladi, N.; Shabtai, H.; Simon, E.S.; Biran, S.; Tal, J.; Korczyn, S.D. Construction of freezing of gait questionnaire for patients with Parkinsonism. Parkinsonism Relat. Disord. 2000, 6, 165–170. [Google Scholar] [CrossRef]
- Larner, A.J. Addenbrooke’s cognitive examination-revised (ACE-R) in day-to-day clinical practice. Age Ageing 2007, 36, 685–686. [Google Scholar] [CrossRef] [PubMed]
- Ramaker, C.; Marinus, J.; Stiggelbout, A.M.; Van Hilten, B.J. Systematic evaluation of rating scales for impairment and disability in Parkinson’s disease. Mov. Disord. 2002, 17, 867–876. [Google Scholar] [CrossRef] [PubMed]
- Ramig, L.O.; Fox, C.; Sapir, S. Speech treatment for Parkinson’s disease. Expert Rev. Neurother. 2008, 8, 297–309. [Google Scholar] [CrossRef] [PubMed]
- Darley, F.L.; Aronson, A.E.; Brown, J.R. Differential Diagnostic Patterns of Dysarthria. J. Speech Lang. Hear. Res. 1969, 12, 246–269. [Google Scholar] [CrossRef]
- Brabenec, L.; Mekyska, J.; Galaz, Z.; Rektorova, I. Speech disorders in Parkinson’s disease: Early diagnostics and effects of medication and brain stimulation. J. Neural Transm. 2017, 124, 303–334. [Google Scholar] [CrossRef] [PubMed]
- Eliasova, I.; Mekyska, J.; Kostalova, M.; Marecek, R.; Smekal, Z.; Rektorova, I. Acoustic evaluation of short-term effects of repetitive transcranial magnetic stimulation on motor aspects of speech in Parkinson’s disease. J. Neural Transm. 2013, 120, 597–605. [Google Scholar] [CrossRef] [PubMed]
- Elfmarkova, N.; Gajdos, M.; Mrackova, M.; Mekyska, J.; Mikl, M.; Rektorova, I. Impact of Parkinson’s disease and levodopa on resting state functional connectivity related to speech prosody control. Parkinsonism Relat. Disord. 2016, 22 (Suppl. 1), S52–S55. [Google Scholar] [CrossRef] [PubMed]
- Gómez-Vilda, P.; Mekyska, J.; Ferrández, J.M.; Palacios-Alonso, D.; Gómez-Rodellar, A.; Rodellar-Biarge, V.; Galaz, Z.; Smekal, D.; Rektorova, I.; Eliasova, I.; et al. Parkinson Disease Detection from Speech Articulation Neuromechanics. Front. Neuroinform. 2017, 11, 56. [Google Scholar] [CrossRef] [PubMed]
- Lirani-Silva, C.; Mourão, L.F.; Gobbi, L.T.B. Dysarthria and Quality of Life in neurologically healthy elderly and patients with Parkinson’s disease. CoDAS 2015, 27, 248–254. [Google Scholar] [CrossRef] [PubMed]
- Ho, A.K.; Iansek, R.; Marigliani, C.; Bradshaw, J.L.; Gates, S. Speech Impairment in a Large Sample of Patients with Parkinson’s disease. J. Behav. Neurol. 1999, 11, 131–137. [Google Scholar] [CrossRef]
- Tsanas, A.; Little, M.; McSharry, P.; Ramig, L. Accurate telemonitoring of Parkinson’s Disease progression by noninvasive speech tests. IEEE Trans. Bio-Med. Eng. 2010, 57, 884–893. [Google Scholar] [CrossRef] [PubMed]
- Harel, B.T.; Cannizzaro, M.S.; Cohen, H.; Reilly, N.; Snyder, P.J. Acoustic characteristics of Parkinsonian speech: A potential biomarker of early disease progression and treatment. J. Neurolinguist. 2004, 17, 439–453. [Google Scholar] [CrossRef]
- Rusz, J.; Cmejla, R.; Ruzickova, H.; Klempir, J.; Majerova, V.; Picmausova, J.; Roth, J.; Ruzicka, E. Evaluation of speech impairment in early stages of Parkinson’s disease: A prospective study with the role of pharmacotherapy. J. Neural Transm. 2013, 120, 319–329. [Google Scholar] [CrossRef] [PubMed]
- Skodda, S.; Grönheit, W.; Schlegel, U.; Südmeyer, M.; Schnitzler, A.; Wojtecki, L. Effect of subthalamic stimulation on voice and speech in Parkinson’s disease: For the better or worse? Front. Neurol. 2014, 4, 218. [Google Scholar] [CrossRef] [PubMed]
- Orozco-Arroyave, J.R.; Hönig, F.; Arias-Londoño, J.D.; Vargas-Bonilla, J.F.; Daqrouq, K.; Skodda, S.; Rusz, J.; Nöth, E. Automatic detection of Parkinson’s disease in running speech spoken in three different languages. J. Acoust. Soc. Am. 2016, 139, 481–500. [Google Scholar] [CrossRef] [PubMed]
- Mekyska, J.; Smekal, Z.; Galaz, Z.; Mzourek, Z.; Rektorova, I.; Faundez-Zanuy, M.; López-de Ipiña, K. Perceptual features as markers of Parkinson’s Disease: the issue of clinical interpretability. In Recent Advances in Nonlinear Speech Processing; Springer: New York, NY, USA, 2016; pp. 83–91. [Google Scholar]
- Mekyska, J.; Galaz, Z.; Mzourek, Z.; Smekal, Z.; Rektorova, I.; Eliasova, I.; Kostalova, M.; Mrackova, M.; Berankova, D.; Faundez-Zanuy, M.; et al. Assessing progress of Parkinson’s disease using acoustic analysis of phonation. In Proceedings of the 2015 4th International Work Conference on Bioinspired Intelligence (IWOBI), San Sebastian, Spain, 10–12 June 2015; pp. 111–118. [Google Scholar]
- Arora, S.; Venkataraman, V.; Zhan, A.; Donohue, S.; Biglan, K.; Dorsey, E.; Little, M. Detecting and monitoring the symptoms of Parkinson’s disease using smartphones: A pilot study. Parkinsonism Relat. Disord. 2015, 21, 650–653. [Google Scholar] [CrossRef] [PubMed]
- Villa-Cañas, T.; Orozco-Arroyave, J.; Vargas-Bonilla, J.; Arias-Londoño, J. Modulation spectra for automatic detection of Parkinson’s disease. In Proceedings of the 2014 XIX Symposium on Image, Signal Processing and Artificial Vision (STSIVA), Armenia, Colombia, 17–19 September 2014; pp. 1–5. [Google Scholar]
- Hazan, H.; Hilu, D.; Manevitz, L.; Ramig, L.O.; Sapir, S. Early diagnosis of Parkinson’s disease via machine learning on speech data. In Proceedings of the 2012 IEEE 27th Convention of Electrical & Electronics Engineers in Israel (IEEEI), Eilat, Israel, 14–17 November 2012; pp. 1–4. [Google Scholar]
- Eskidere, Ö.; Ertaş, F.; Hanilçi, C. A comparison of regression methods for remote tracking of Parkinson’s disease progression. Expert Syst. Appl. 2012, 39, 5523–5528. [Google Scholar] [CrossRef]
- Castelli, M.; Vanneschi, L.; Silva, S. Prediction of the Unified Parkinson’s Disease Rating Scale assessment using a genetic programming system with geometric semantic genetic operators. Expert Syst. Appl. 2014, 41, 4608–4616. [Google Scholar] [CrossRef] [Green Version]
- Naranjo, L.; Pérez, C.J.; Martín, J. Addressing voice recording replications for tracking Parkinson’s disease progression. Med. Biol. Eng. Comput. 2017, 55, 365–373. [Google Scholar] [CrossRef] [PubMed]
- Skodda, S.; Rinsche, H.; Schlegel, U. Progression of dysprosody in Parkinson’s disease over time—A longitudinal study. Mov. Disord. 2009, 24, 716–722. [Google Scholar] [CrossRef] [PubMed]
- Skodda, S.; Flasskamp, A.; Schlegel, U. Instability of syllable repetition as a marker of disease progression in Parkinson’s disease: A longitudinal study. Mov. Disord. 2011, 26, 59–64. [Google Scholar] [CrossRef] [PubMed]
- Skodda, S.; Grönheit, W.; Schlegel, U. Impairment of vowel articulation as a possible marker of disease progression in Parkinson’s disease. PLoS ONE 2012, 7, e32132. [Google Scholar] [CrossRef] [PubMed]
- Skodda, S.; Gronheit, W.; Mancinelli, N.; Schlegel, U. Progression of Voice and Speech Impairment in the Course of Parkinson’s Disease: A Longitudinal Study. Parkinson’s Dis. 2013, 2013, 389195. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.Y.; Kim, J.W.; Lee, W.Y.; Kim, J.M.; Ahn, T.B.; Kim, H.J.; Cho, J.; Jeon, B.S. Daily dose of dopaminergic medications in Parkinson’s disease: clinical correlates and a posteriori equation. Neurol. Asia 2010, 15, 137–143. [Google Scholar]
- Stiasny-Kolster, K.; Mayer, G.; Schafer, S.; Muller, J.C.; Heinzel-Gutenbrunner, M.; Oertel, W.H. The REM sleep behavior disorder screening questionnaire—A new diagnostic instrument. Mov. Disord. 2007, 22, 2386–2393. [Google Scholar] [CrossRef] [PubMed]
- Mol, H. Lossfree Twin-Tube Resonator and the Vowel Triangle of Hellwag. J. Acoust. Soc. Am. 1965, 37, 1186. [Google Scholar] [CrossRef] [Green Version]
- Orozco-Arroyave, J.R.; Hönig, F.; Arias-Londoño, J.D.; Vargas-Bonilla, J.; Skodda, S.; Rusz, J.; Nöth, E. Automatic detection of Parkinson’s disease from words uttered in three different languages. In Proceedings of the Fifteenth Annual Conference of the International Speech Communication Association, Singapore, 14–18 September 2014; pp. 1573–1577. [Google Scholar]
- Rusz, J.; Cmejla, R.; Tykalova, T.; Ruzickova, H.; Klempir, J.; Majerova, V.; Picmausova, J.; Roth, J.; Ruzicka, E. Imprecise vowel articulation as a potential early marker of Parkinson’s disease: Effect of speaking task. J. Acoust. Soc. Am. 2013, 134, 2171–2181. [Google Scholar] [CrossRef] [PubMed]
- Rusz, J.; Cmejla, R.; Ruzickova, H.; Ruzicka, E. Quantitative acoustic measurements for characterization of speech and voice disorders in early untreated Parkinson’s disease. J. Acoust. Soc. Am. 2011, 129, 350–367. [Google Scholar] [CrossRef] [PubMed]
- Titze, I.R. Principles of Voice Production; Prentice Hall: Englewood Cliffs, NJ, USA, 1994. [Google Scholar]
- Harar, P.; Alonso-Hernandezy, J.B.; Mekyska, J.; Galaz, Z.; Burget, R.; Smekal, Z. Voice Pathology Detection Using Deep Learning: A Preliminary Study. In Proceedings of the 2017 International Conference and Workshop on Bioinspired Intelligence (IWOBI), Funchal, Portugal, 10–12 July 2017; pp. 45–48. [Google Scholar]
- Harar, P.; Galaz, Z.; Alonso-Hernandez, J.B.; Mekyska, J.; Burget, R.; Smekal, Z. Towards robust voice pathology detection. Neural Comput. Appl. 2018. [Google Scholar] [CrossRef]
- Kostalova, M.; Mrackova, M.; Marecek, R.; Berankova, D.; Eliasova, I.; Janousova, E.; Roubickova, J.; Bednarik, J.; Rektorova, I. The 3F Test Dysarthric Profile—Normative Speach Values in Czech. Ceska Slovenska Neurologie Neurochirurgie 2013, 76, 614–618. [Google Scholar]
- Boersma, P.; Weenink, D. Praat, a system for doing phonetics by computer. Glot Int. 2002, 5, 341–345. [Google Scholar]
- Mekyska, J.; Janousova, E.; Gomez-Vilda, P.; Smekal, Z.; Rektorova, I.; Eliasova, I.; Kostalova, M.; Mrackova, M.; Alonso-Hernandez, J.B.; Faundez-Zanuy, M.; et al. Robust and complex approach of pathological speech signal analysis. Neurocomputing 2015, 167, 94–111. [Google Scholar] [CrossRef]
- Rektorova, I.; Mekyska, J.; Janousova, E.; Kostalova, M.; Eliasova, I.; Mrackova, M.; Berankova, D.; Necasova, T.; Smekal, Z.; Marecek, R. Speech prosody impairment predicts cognitive decline in Parkinson’s disease. Parkinsonism Relat. Disord. 2016, 29, 90–95. [Google Scholar] [CrossRef] [PubMed]
- Arias-Vergara, T.; Vásquez-Correa, J.C.; Orozco-Arroyave, J.R. Parkinson’s Disease and Aging: Analysis of Their Effect in Phonation and Articulation of Speech. Cogn. Comput. 2017, 9, 731–748. [Google Scholar] [CrossRef]
- Rusz, J.; Tykalova, T.; Klempir, J.; Cmejla, R.; Ruzicka, E. Effects of dopaminergic replacement therapy on motor speech disorders in Parkinson’s disease: Longitudinal follow-up study on previously untreated patients. J. Neural Transm. 2016, 123, 379–387. [Google Scholar] [CrossRef] [PubMed]
- Chen, T.; Guestrin, C. Xgboost: A scalable tree boosting system. In Proceedings of the 22nd ACM SIGKDD International Conference on Knowledge Discovery and Data Mining, San Francisco, CA, USA, 13–17 August 2016; pp. 785–794. [Google Scholar]
- Breiman, L.; Friedman, J.H.; Olshen, R.A.; Stone, C.J. Classification and Regression Trees; Wadsworth and Brooks: Monterey, CA, USA, 1984. [Google Scholar]
- Torlay, L.; Perrone-Bertolotti, M.; Thomas, E.; Baciu, M. Machine learning—XGBoost analysis of language networks to classify patients with epilepsy. Brain Inform. 2017, 4, 159. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Wang, X.; Jung, Y.; Abedi, V.; Zand, R.; Bikak, M.; Adibuzzaman, M. Classification of short single lead electrocardiograms (ECGs) for atrial fibrillation detection using piecewise linear spline and XGBoost. Physiol. Meas. 2018, 39, 104006. [Google Scholar] [CrossRef] [PubMed]
- Zhong, J.; Sun, Y.; Peng, W.; Xie, M.; Yang, J.; Tang, X. XGBFEMF: An XGBoost-based Framework for Essential Protein Prediction. IEEE Trans. NanoBiosci. 2018, 17, 243–250. [Google Scholar] [CrossRef] [PubMed]
- Palmer, J.L.; Coats, M.A.; Roe, C.M.; Hanko, S.M.; Xiong, C.; Morris, J.C. Unified Parkinson’s Disease Rating Scale-Motor Exam: Inter-rater reliability of advanced practice nurse and neurologist assessments. J. Adv. Nurs. 2010, 66, 1382–1387. [Google Scholar] [CrossRef] [PubMed]
- Baggio, J.A.O.; Curtarelli, M.B.; Rodrigues, G.R.; Tumas, V. Validity of the Brazilian version of the freezing of gait questionnaire. Arquivos de Neuro-Psiquiatria 2012, 70, 599–603. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Santos, D.G.; Macías, M.A. Inter-rater variability in motor function assessment in Parkinson’s disease between experts in movement disorders and nurses specialising in PD management. Neurologia 2017. [Google Scholar] [CrossRef]
- Jankovic, J. Parkinson’s disease: Clinical features and diagnosis. J. Neurol. Neurosurg. Psychiatry 2008, 79, 368–376. [Google Scholar] [CrossRef] [PubMed]
- Mekyska, J.; Galaz, Z.; Kiska, T.; Zvoncak, V.; Mucha, J.; Smekal, Z.; Eliasova, I.; Kostalova, M.; Mrackova, M.; Fiedorova, D.; et al. Quantitative Analysis of Relationship Between Hypokinetic Dysarthria and the Freezing of Gait in Parkinson’s Disease. Cogn. Comput. 2018. [Google Scholar] [CrossRef]
- Berg, D.; Postuma, R.B.; Adler, C.H.; Bloem, B.R.; Chan, P.; Dubois, B.; Gasser, T.; Goetz, C.G.; Halliday, G.; Joseph, L.; et al. MDS research criteria for prodromal Parkinson’s disease. Mov. Dis. 2015, 30, 1600–1611. [Google Scholar] [CrossRef] [PubMed]


| Scale | Mean ± sd (s1) | Mean ± sd (s2) | Mean ± sd () | p (Wilcoxon) |
|---|---|---|---|---|
| LED | 917.61 ± 544.78 | 1129.92 ± 477.50 | 212.31 ± −67.28 | 0.188 |
| UPDRS III | 22.49 ± 13.47 | 27.45 ± 12.68 | 4.96 ± −0.79 | 0.000 |
| UPDRS IV | 2.82 ± 2.58 | 3.44 ± 2.94 | 0.62 ± 0.36 | 0.632 |
| FOG-Q | 6.57 ± 5.40 | 8.33 ± 5.97 | 1.76 ± 0.57 | 0.000 |
| RBDSQ | 3.98 ± 3.25 | 3.78 ± 2.28 | −0.2 ±−0.98 | 0.522 |
| ACE-R | 87.92 ± 7.62 | 85.89 ± 9.48 | −2.03 ± 1.86 | 0.000 |
| Feature | Mean ± sd (s1) | Mean ± sd (s2) | Mean ± sd () | p (Wilcoxon) |
|---|---|---|---|---|
| vowel /a/ | ||||
| PPQ | 1.31 ± 1.28 | 1.89 ± 2.52 | 0.58 ± 1.24 | 0.069 |
| APQ | 10.69 ± 4.23 | 12.81 ± 6.66 | 2.12 ± 2.42 | 0.063 |
| FLUF | 3.87 ± 5.28 | 4.77 ± 5.61 | 0.90 ± 0.32 | 0.386 |
| HNR (Q2) | 13.35 ± 2.90 | 12.81 ± 3.73 | −0.54 ± 0.83 | 0.390 |
| HNR (SD) | 4.17 ± 0.86 | 4.18 ± 0.89 | 0.02 ± 0.03 | 0.928 |
| F1 (CV) | 0.15 ± 0.06 | 0.18 ± 0.10 | 0.02 ± 0.04 | 0.180 |
| F2 (CV) | 0.22 ± 0.15 | 0.23 ± 0.15 | 0.00 ± 0.00 | 0.913 |
| F3 (CV) | 8.25 ± 40.44 | 4.50 ± 21.67 | −3.75 ± −18.77 | 0.575 |
| ER (Q2) | 6.98 ± 33.97 | 7.40 ± 36.43 | 0.42 ± 2.46 | 0.954 |
| ER (CV) | 0.57 ± 0.26 | 0.57 ± 0.30 | 0.01 ± 0.05 | 0.880 |
| F0 (CV) | 0.30 ± 0.74 | 0.36 ± 1.15 | 0.06 ± 0.41 | 0.763 |
| GNE (Q2) | −0.46 ± 1.85 | −0.46 ± 1.85 | 0.00 ± −0.00 | 0.997 |
| GNE (SD) | 0.23 ± 0.74 | 0.30 ± 0.97 | 0.07 ± 0.23 | 0.679 |
| TEO (CV) | −0.34 ± 1.71 | −0.31 ± 1.75 | 0.03 ± 0.04 | 0.931 |
| NNE (Q2) | −1.45 ± 7.41 | −1.33 ± 7.08 | 0.13 ± −0.34 | 0.932 |
| NNE (SD) | 1.80 ± 0.76 | 1.79 ± 0.78 | −0.01 ± 0.02 | 0.955 |
| vowel /e/ | ||||
| PPQ | 1.31 ± 1.17 | 1.80 ± 3.06 | 0.50 ± 1.89 | 0.269 |
| APQ | 11.21 ± 6.82 | 15.05 ± 9.95 | 3.84 ± 3.13 | 0.036 |
| FLUF | 2.62 ± 3.58 | 5.31 ± 6.02 | 2.69 ± 2.44 | 0.007 |
| HNR (Q2) | 14.36 ± 3.92 | 13.75 ± 4.40 | −0.61 ± 0.48 | 0.394 |
| HNR (SD) | 4.19 ± 0.96 | 4.32 ± 1.18 | 0.13 ± 0.21 | 0.533 |
| F1 (CV) | 0.62 ± 0.23 | 0.56 ± 0.24 | −0.05 ± 0.01 | 0.173 |
| F2 (CV) | 0.19 ± 0.07 | 0.19 ± 0.09 | −0.00 ± 0.02 | 0.965 |
| F3 (CV) | 12.41 ± 86.28 | 7.06 ± 48.94 | −5.36 ± −37.34 | 0.709 |
| ER (Q2) | 3.46 ± 23.30 | 3.39 ± 22.83 | −0.07 ± −0.47 | 0.989 |
| ER (CV) | 0.59 ± 0.28 | 0.61 ± 0.37 | 0.02 ± 0.10 | 0.702 |
| F0 (CV) | 0.42 ± 1.47 | 0.19 ± 0.50 | −0.24 ± −0.97 | 0.293 |
| GNE (Q2) | −0.36 ± 1.77 | −0.17 ± 1.18 | 0.19 ± −0.59 | 0.536 |
| GNE (SD) | 0.08 ± 0.36 | 0.06 ± 0.30 | −0.02 ± −0.07 | 0.726 |
| TEO (CV) | −0.07 ± 0.50 | −0.19 ± 1.31 | −0.11 ± 0.80 | 0.571 |
| NNE (Q2) | −0.19 ± 1.35 | −0.21 ± 1.44 | −0.01 ± 0.10 | 0.961 |
| NNE (SD) | 1.67 ± 0.56 | 1.83 ± 0.61 | 0.17 ± 0.05 | 0.055 |
| vowel /i/ | ||||
| PPQ | 1.26 ± 1.68 | 1.92 ± 3.08 | 0.66 ± 1.40 | 0.196 |
| APQ | 10.49 ± 5.31 | 14.83 ± 9.65 | 4.35 ± 4.34 | 0.005 |
| FLUF | 2.13 ± 3.73 | 4.60 ± 6.89 | 2.46 ± 3.15 | 0.013 |
| HNR (Q2) | 17.16 ± 3.38 | 16.17 ± 5.32 | −0.98 ± 1.95 | 0.212 |
| HNR (SD) | 4.51 ± 1.12 | 4.53 ± 1.40 | 0.02 ± 0.28 | 0.921 |
| F1 (CV) | 0.67 ± 0.48 | 0.58 ± 0.40 | −0.09 ± −0.08 | 0.170 |
| F2 (CV) | 0.14 ± 0.07 | 0.16 ± 0.08 | 0.02 ± 0.00 | 0.088 |
| F3 (CV) | 0.09 ± 0.21 | 38.22 ± 207.82 | 38.14 ± 207.61 | 0.205 |
| ER (Q2) | 0.09 ± 0.08 | 8.35 ± 33.15 | 8.27 ± 33.07 | 0.087 |
| ER (CV) | 0.61 ± 0.37 | 0.56 ± 0.44 | −0.05 ± 0.07 | 0.490 |
| F0 (CV) | 0.36 ± 1.39 | 0.35 ± 1.17 | −0.01 ± −0.22 | 0.961 |
| GNE (Q2) | −0.30 ± 1.49 | −0.30 ± 1.48 | 0.01 ± −0.01 | 0.980 |
| GNE (SD) | 0.07 ± 0.32 | 0.12 ± 0.40 | 0.06 ± 0.08 | 0.449 |
| TEO (CV) | 0.78 ± 0.55 | 0.36 ± 2.47 | −0.42 ± 2.47 | 0.238 |
| NNE (Q2) | −0.01 ± 0.18 | −0.20 ± 11.53 | −0.19 ± 1.15 | 0.228 |
| NNE (SD) | 1.44 ± 0.55 | 1.40 ± 0.70 | −0.05 ± 0.15 | 0.727 |
| vowel /o/ | ||||
| PPQ | 1.14 ± 1.06 | 1.68 ± 2.06 | 0.54 ± 0.99 | 0.047 |
| APQ | 11.09 ± 4.41 | 14.16 ± 9.94 | 3.06 ± 5.53 | 0.051 |
| FLUF | 2.64 ± 4.32 | 5.63 ± 7.24 | 2.99 ± 2.91 | 0.008 |
| HNR (Q2) | 15.49 ± 3.30 | 15.28 ± 4.79 | −0.22 ± 1.49 | 0.773 |
| HNR (SD) | 4.93 ± 1.14 | 4.57 ± 1.36 | −0.36 ± 0.21 | 0.149 |
| F1 (CV) | 0.24 ± 0.19 | 0.31 ± 0.22 | 0.06 ± 0.03 | 0.091 |
| F2 (CV) | 0.14 ± 0.10 | 0.14 ± 0.10 | 0.00 ± 0.01 | 0.867 |
| F3 (CV) | 8.75 ± 35.36 | 23.86 ± 96.34 | 15.11 ± 60.97 | 0.317 |
| ER (Q2) | 8.17 ± 32.52 | 8.07 ± 32.42 | −0.10 ±−0.10 | 0.989 |
| ER (CV) | 0.64 ± 0.39 | 0.61 ± 0.36 | −0.03 ±−0.02 | 0.705 |
| F0 (CV) | 0.40 ± 0.91 | 0.63 ± 1.81 | 0.24 ± 0.89 | 0.434 |
| GNE (Q2) | −0.91 ± 2.72 | −1.25 ± 3.11 | −0.35 ± 0.39 | 0.582 |
| GNE (SD) | 0.30 ± 0.75 | 0.39 ± 0.90 | 0.09 ± 0.15 | 0.580 |
| TEO (CV) | −0.74 ± 3.27 | −0.28 ± 1.30 | 0.46 ± −1.97 | 0.376 |
| NNE (Q2) | −0.19 ± 0.79 | −0.11 ± 0.47 | 0.09 ± −0.31 | 0.530 |
| NNE (SD) | 1.62 ± 0.83 | 1.58 ± 0.91 | −0.04 ± 0.08 | 0.843 |
| vowel /u/ | ||||
| PPQ | 1.35 ± 1.17 | 2.60 ± 3.07 | 1.26 ± 1.90 | 0.009 |
| APQ | 12.66 ± 5.60 | 17.03 ± 9.50 | 4.37 ± 3.91 | 0.007 |
| FLUF | 2.77 ± 5.13 | 8.52 ± 9.83 | 5.75 ± 4.69 | 0.001 |
| HNR (Q2) | 15.28 ± 4.23 | 14.32 ± 5.22 | −0.96 ± 0.99 | 0.270 |
| HNR (SD) | 5.40 ± 1.56 | 5.08 ± 1.46 | −0.32 ±−0.10 | 0.252 |
| F1 (CV) | 0.69 ± 0.44 | 0.71 ± 0.34 | 0.03 ± −0.10 | 0.667 |
| F2 (CV) | 0.17 ± 0.09 | 0.18 ± 0.09 | 0.01 ± −0.00 | 0.468 |
| F3 (CV) | 10.28 ± 52.21 | 15.04 ± 104.80 | 4.76 ± 52.58 | 0.779 |
| ER (Q2) | 8.27 ± 33.82 | 3.63 ± 25.29 | −4.64 ±−8.53 | 0.453 |
| ER (CV) | 0.67 ± 0.39 | 0.74 ± 0.43 | 0.06 ± 0.04 | 0.431 |
| F0 (CV) | 0.23 ± 0.67 | 0.18 ± 0.10 | −0.05 ±−0.57 | 0.586 |
| GNE (Q2) | −0.19 ± 1.31 | 0.00 ± 0.00 | 0.19 ± −1.31 | 0.323 |
| GNE (SD) | 0.09 ± 0.40 | 0.10 ± 0.70 | 0.01 ± 0.30 | 0.966 |
| TEO (CV) | −0.51 ± 2.69 | −0.07 ± 0.51 | 0.43 ± −2.18 | 0.275 |
| NNE (Q2) | −1.27 ± 7.09 | −0.31 ± 2.190 | 0.96 ± −4.91 | 0.373 |
| NNE (SD) | 1.57 ± 0.73 | 1.68 ± 0.49 | 0.11 ± −0.24 | 0.379 |
| Feature | /a/ | /e/ | /i/ | /o/ | /u/ | /a/ | /e/ | /i/ | /o/ | /u/ |
|---|---|---|---|---|---|---|---|---|---|---|
| UPDRS III | UPDRS IV | |||||||||
| PPQ | −0.07 | −0.08 | 0.26 | −0.09 | −0.10 | −0.11 | −0.26 | −0.08 | −0.17 | −0.08 |
| APQ | −0.06 | −0.05 | 0.17 | −0.10 | −0.09 | 0.08 | 0.12 | −0.01 | 0.06 | −0.09 |
| FLUF | 0.10 | 0.08 | 0.11 | 0.10 | 0.16 | −0.23 | −0.47 ** | −0.33 * | −0.34 * | −0.32 * |
| HNR (Q2) | 0.16 | 0.07 | −0.05 | 0.17 | 0.09 | −0.02 | −0.08 | 0.07 | 0.11 | 0.16 |
| HNR (SD) | 0.10 | 0.11 | −0.04 | −0.05 | −0.15 | 0.07 | −0.02 | 0.20 | −0.22 | −0.09 |
| F1 (CV) | 0.04 | 0.10 | −0.17 | −0.02 | 0.19 | −0.27 | −0.07 | 0.08 | −0.32 * | 0.08 |
| F2 (CV) | −0.15 | 0.20 | −0.10 | −0.11 | 0.11 | −0.37 * | −0.11 | −0.12 | −0.23 | 0.04 |
| F3 (CV) | −0.24 | 0.25 | −0.23 | −0.17 | 0.11 | 0.22 | 0.28 | 0.10 | 0.32 * | 0.10 |
| ER (Q2) | −0.25 | 0.25 | −0.14 | −0.17 | 0.17 | 0.16 | 0.28 | 0.12 | 0.34 * | 0.32 * |
| ER (CV) | 0.12 | −0.09 | 0.22 | −0.03 | 0.11 | −0.17 | −0.14 | −0.22 | −0.18 | −0.06 |
| F0 (CV) | 0.28 | −0.12 | 0.04 | −0.08 | 0.17 | 0.33 * | −0.04 | −0.24 | −0.16 | −0.21 |
| GNE (Q2) | −0.14 | 0.11 | −0.15 | 0.06 | −0.17 | −0.35 * | 0.25 | 0.15 | 0.27 | 0.33 * |
| GNE (SD) | −0.16 | −0.08 | −0.12 | −0.22 | 0.24 | 0.30 * | −0.01 | −0.04 | 0.22 | 0.11 |
| TEO (CV) | 0.28 | −0.25 | 0.11 | 0.15 | −0.25 | −0.23 | −0.28 | −0.28 | −0.23 | −0.30 * |
| NNE (Q2) | 0.28 | −0.25 | −0.09 | 0.14 | −0.23 | −0.15 | −0.28 | −0.22 | −0.26 | −0.31 * |
| NNE (SD) | 0.09 | −0.25 | 0.12 | 0.11 | −0.26 | −0.43 ** | −0.17 | −0.28 | −0.12 | −0.12 |
| RBDSQ | FOG-Q | |||||||||
| PPQ | 0.15 | 0.11 | 0.21 | −0.13 | 0.33 * | −0.20 | −0.09 | 0.15 | −0.09 | 0.08 |
| APQ | 0.29 * | 0.27 | 0.21 | 0.27 | 0.20 | −0.18 | −0.14 | −0.16 | −0.16 | −0.12 |
| FLUF | −0.06 | 0.06 | −0.22 | −0.17 | −0.24 | 0.20 | 0.15 | 0.13 | 0.17 | 0.23 |
| HNR (Q2) | −0.20 | −0.17 | −0.19 | −0.27 | −0.20 | 0.09 | 0.03 | −0.03 | 0.09 | −0.05 |
| HNR (SD) | −0.17 | −0.16 | 0.21 | −0.36 * | −0.27 | 0.07 | 0.24 | 0.21 | 0.18 | 0.12 |
| F1 (CV) | 0.08 | −0.02 | 0.24 | 0.09 | 0.11 | 0.16 | −0.22 | 0.33 * | −0.20 | −0.20 |
| F2 (CV) | −0.08 | −0.09 | −0.26 | −0.17 | −0.27 | 0.18 | −0.09 | −0.03 | −0.13 | 0.26 |
| F3 (CV) | −0.10 | −0.04 | −0.11 | 0.07 | −0.08 | 0.03 | 0.22 | 0.14 | 0.08 | −0.11 |
| ER (Q2) | −0.19 | −0.21 | −0.26 | −0.12 | −0.16 | −0.13 | 0.04 | 0.25 | 0.10 | −0.05 |
| ER (CV) | 0.08 | 0.28 | 0.20 | −0.28 | −0.11 | 0.04 | −0.13 | −0.11 | 0.10 | 0.06 |
| F0 (CV) | 0.21 | 0.13 | 0.19 | 0.25 | 0.10 | 0.37 * | 0.20 | −0.03 | −0.10 | 0.19 |
| GNE (Q2) | −0.16 | −0.17 | −0.28 | −0.18 | −0.16 | −0.29 | −0.25 | 0.05 | −0.19 | −0.19 |
| GNE (SD) | −0.05 | −0.09 | −0.25 | 0.09 | −0.20 | 0.08 | 0.14 | −0.05 | 0.12 | 0.15 |
| TEO (CV) | 0.05 | 0.04 | 0.27 | −0.17 | 0.15 | −0.05 | −0.22 | −0.07 | −0.25 | −0.01 |
| NNE (Q2) | 0.24 | 0.28 | 0.18 | 0.20 | 0.21 | −0.04 | 0.21 | 0.17 | 0.16 | 0.20 |
| NNE (SD) | −0.27 | −0.05 | −0.19 | −0.16 | 0.11 | −0.23 | −0.12 | 0.16 | −0.22 ** | 0.05 |
| Feature | /a/ | /e/ | /i/ | /o/ | /u/ | /a/ | /e/ | /i/ | /o/ | /u/ |
|---|---|---|---|---|---|---|---|---|---|---|
| UPDRS III | UPDRS IV | |||||||||
| PPQ | −0.12 | −0.20 | −0.31 * | 0.10 | −0.13 | 0.09 | 0.40 ** | 0.25 | 0.21 | 0.10 |
| APQ | −0.17 | −0.14 | −0.26 | −0.06 | −0.15 | 0.06 | 0.08 | 0.10 | 0.06 | 0.03 |
| FLUF | −0.27 | −0.30 * | −0.15 | −0.40 ** | −0.25 | 0.17 | 0.21 | 0.28 | 0.04 | 0.21 |
| HNR (Q2) | −0.04 | 0.08 | 0.22 | −0.07 | 0.09 | −0.02 | −0.03 | −0.14 | −0.14 | −0.17 |
| HNR (SD) | 0.12 | −0.18 | −0.25 | −0.05 | 0.19 | −0.10 | 0.08 | −0.21 | −0.08 | 0.13 |
| F1 (CV) | −0.35 * | −0.26 | −0.04 | −0.28 | −0.38 ** | 0.05 | −0.04 | −0.07 | −0.02 | −0.11 |
| F2 (CV) | 0.13 | −0.34 * | −0.22 | −0.07 | −0.23 | 0.39 ** | 0.07 | −0.07 | 0.28 | 0.21 |
| F3 (CV) | 0.29 * | −0.19 | 0.22 | 0.24 | −0.09 | −0.16 | −0.12 | −0.21 | −0.21 | −0.10 |
| ER (Q2) | 0.31 * | −0.15 | 0.04 | 0.26 | −0.13 | −0.11 | −0.07 | −0.16 | −0.27 | −0.29 * |
| ER (CV) | −0.23 | −0.05 | −0.16 | −0.17 | 0.05 | −0.08 | −0.33 * | 0.12 | −0.04 | 0.14 |
| F0 (CV) | −0.32 * | 0.18 | 0.21 | −0.19 | −0.30 * | −0.15 | 0.12 | 0.15 | −0.13 | 0.15 |
| GNE (Q2) | 0.27 | −0.22 | −0.22 | 0.20 | 0.17 | 0.17 | −0.18 | −0.15 | 0.11 | −0.27 |
| GNE (SD) | 0.16 | 0.32 * | 0.23 | 0.14 | −0.25 | −0.18 | 0.10 | −0.07 | −0.25 | −0.05 |
| TEO (CV) | −0.23 | −0.18 | −0.11 | −0.13 | 0.23 | 0.29 * | −0.13 | 0.28 | 0.28 | 0.30 * |
| NNE (Q2) | −0.25 | 0.14 | −0.12 | −0.19 | 0.20 | 0.10 | 0.16 | 0.24 | 0.30 * | 0.31 * |
| NNE (SD) | −0.12 | 0.05 | −0.42 ** | −0.06 | 0.11 | 0.29 * | 0.15 | 0.16 | 0.24 | 0.16 |
| RBDSQ | FOG-Q | |||||||||
| PPQ | −0.23 | −0.19 | −0.16 | −0.17 | −0.37 * | 0.15 | −0.17 | −0.18 | 0.12 | −0.10 |
| APQ | −0.28 | −0.37 * | −0.38 ** | −0.29 | −0.32 * | 0.08 | 0.08 | 0.06 | 0.14 | 0.09 |
| FLUF | 0.05 | −0.06 | 0.06 | 0.10 | −0.18 | −0.41 ** | −0.29 * | −0.10 | −0.35 * | −0.40 ** |
| HNR (Q2) | 0.29 * | 0.35 * | 0.31 * | 0.36 * | 0.41 ** | 0.15 | 0.11 | 0.12 | 0.02 | 0.04 |
| HNR (SD) | 0.23 | 0.36 * | 0.10 | 0.40 ** | 0.30 * | −0.06 | 0.07 | −0.18 | −0.20 | 0.01 |
| F1 (CV) | −0.23 | 0.04 | −0.12 | 0.06 | −0.16 | −0.29 | −0.04 | −0.42 ** | 0.12 | 0.13 |
| F2 (CV) | −0.06 | 0.08 | 0.16 | 0.17 | 0.06 | −0.27 | −0.08 | −0.20 | −0.09 | −0.37 * |
| F3 (CV) | 0.07 | 0.15 | −0.25 | −0.40 ** | −0.10 | −0.07 | 0.18 | 0.09 | −0.08 | 0.20 |
| ER (Q2) | 0.17 | 0.23 | −0.27 | −0.27 | 0.09 | 0.12 | 0.26 | −0.06 | −0.21 | 0.17 |
| ER (CV) | −0.10 | −0.46 ** | 0.06 | 0.28 | −0.11 | −0.00 | −0.30 * | −0.34 * | 0.08 | −0.19 |
| F0 (CV) | −0.17 | −0.14 | −0.17 | −0.12 | −0.11 | −0.23 | −0.17 | 0.20 | −0.05 | −0.23 |
| GNE (Q2) | 0.13 | 0.30 * | 0.25 | 0.13 | 0.15 | 0.20 | 0.17 | −0.21 | 0.07 | 0.27 |
| GNE (SD) | 0.04 | 0.40 ** | −0.23 | −0.23 | 0.25 | −0.07 | 0.14 | 0.24 | −0.03 | 0.14 |
| TEO (CV) | −0.06 | −0.25 | 0.24 | 0.25 | −0.18 | 0.06 | −0.37 * | −0.17 | 0.34 * | −0.20 |
| NNE (Q2) | −0.15 | −0.42 ** | 0.24 | 0.27 | −0.23 | −0.20 | −0.28 | −0.05 | 0.25 | −0.13 |
| NNE (SD) | 0.25 | 0.02 | 0.20 | 0.24 | −0.15 | 0.18 | 0.10 | −0.25 | 0.06 ** | −0.15 |
| VT | MAE | EER [%] | MAE | EER [%] | MAE | EER [%] | MAE | EER [%] |
|---|---|---|---|---|---|---|---|---|
| UPDRS III | UPDRS IV | RBDSQ | FOG-Q | |||||
| /a/ | 8.2 ± 2.6 | 29.1 ± 9.2 | 1.9 ± 0.6 | 12.9 ± 4.1 | 2.2 ± 1.0 | 17.6 ± 8.1 | 3.1 ± 0.8 | 14.7 ± 3.8 |
| /e/ | 7.3 ± 2.0 | 25.7 ± 7.0 | 1.8 ± 0.7 | 12.2 ± 4.8 | 2.0 ± 0.8 | 16.4 ± 6.9 | 3.4 ± 1.0 | 16.1 ± 5.0 |
| /i/ | 7.4 ± 2.7 | 26.3 ± 9.4 | 1.9 ± 0.8 | 12.9 ± 5.5 | 2.0 ± 0.7 | 16.3 ± 6.3 | 2.9 ± 0.7 | 13.6 ± 3.6 |
| /o/ | 7.9 ± 2.1 | 28.2 ± 7.7 | 1.7 ± 0.7 | 11.3 ± 4.8 | 2.1 ± 0.8 | 16.8 ± 6.3 | 3.3 ± 0.5 | 15.4 ± 2.6 |
| /u/ | 7.7 ± 2.5 | 27.2 ± 8.8 | 2.0 ± 0.8 | 13.8 ± 5.5 | 2.1 ± 0.9 | 17.3 ± 7.2 | 2.8 ± 0.9 | 13.2 ± 4.5 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Galaz, Z.; Mekyska, J.; Zvoncak, V.; Mucha, J.; Kiska, T.; Smekal, Z.; Eliasova, I.; Mrackova, M.; Kostalova, M.; Rektorova, I.; et al. Changes in Phonation and Their Relations with Progress of Parkinson’s Disease. Appl. Sci. 2018, 8, 2339. https://doi.org/10.3390/app8122339
Galaz Z, Mekyska J, Zvoncak V, Mucha J, Kiska T, Smekal Z, Eliasova I, Mrackova M, Kostalova M, Rektorova I, et al. Changes in Phonation and Their Relations with Progress of Parkinson’s Disease. Applied Sciences. 2018; 8(12):2339. https://doi.org/10.3390/app8122339
Chicago/Turabian StyleGalaz, Zoltan, Jiri Mekyska, Vojtech Zvoncak, Jan Mucha, Tomas Kiska, Zdenek Smekal, Ilona Eliasova, Martina Mrackova, Milena Kostalova, Irena Rektorova, and et al. 2018. "Changes in Phonation and Their Relations with Progress of Parkinson’s Disease" Applied Sciences 8, no. 12: 2339. https://doi.org/10.3390/app8122339
APA StyleGalaz, Z., Mekyska, J., Zvoncak, V., Mucha, J., Kiska, T., Smekal, Z., Eliasova, I., Mrackova, M., Kostalova, M., Rektorova, I., Faundez-Zanuy, M., Alonso-Hernandez, J. B., & Gomez-Vilda, P. (2018). Changes in Phonation and Their Relations with Progress of Parkinson’s Disease. Applied Sciences, 8(12), 2339. https://doi.org/10.3390/app8122339