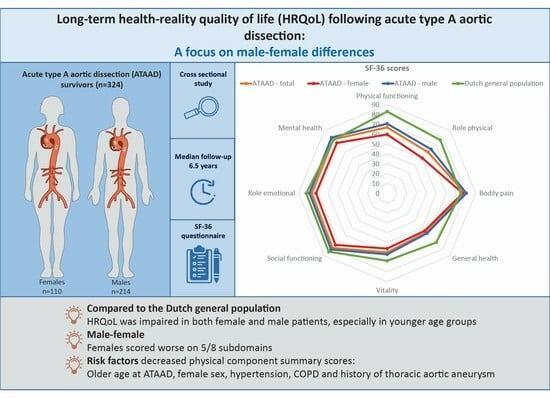
Long-Term Health-Related Quality of Life following Acute Type A Aortic Dissection with a Focus on Male–Female Differences: A Cross Sectional Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Study Population
2.2. Data Collection
2.3. HRQoL Questionnaire
2.4. Statistical Analysis
3. Results
4. Discussion
5. Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- Evangelista, A.; Isselbacher, E.M.; Bossone, E.; Gleason, T.G.; Eusanio, M.D.; Sechtem, U.; Ehrlich, M.P.; Trimarchi, S.; Braverman, A.C.; Myrmel, T.; et al. Insights from the International Registry of Acute Aortic Dissection: A 20-Year Experience of Collaborative Clinical Research. Circulation 2018, 137, 1846–1860. [Google Scholar] [CrossRef] [PubMed]
- Smedberg, C.; Steuer, J.; Leander, K.; Hultgren, R. Sex differences and temporal trends in aortic dissection: A population-based study of incidence, treatment strategies, and outcome in Swedish patients during 15 years. Eur. Heart J. 2020, 41, 2430–2438. [Google Scholar] [CrossRef] [PubMed]
- Hagan, P.G.; Nienaber, C.A.; Isselbacher, E.M.; Bruckman, D.; Karavite, D.J.; Russman, P.L.; Evangelista, A.; Fattori, R.; Suzuki, T.; Oh, J.K.; et al. The International Registry of Acute Aortic Dissection (IRAD): New insights into an old disease. JAMA 2000, 283, 897–903. [Google Scholar] [CrossRef] [PubMed]
- Gariboldi, V.; Grisoli, D.; Kerbaul, F.; Giorgi, R.; Riberi, A.; Metras, D.; Mesana, T.G.; Collart, F. Long-term outcomes after repaired acute type A aortic dissections. Interact. Cardiovasc. Thorac. Surg. 2007, 6, 47–51. [Google Scholar] [CrossRef] [PubMed]
- Carbone, A.; Ranieri, B.; Castaldo, R.; Franzese, M.; Rega, S.; Cittadini, A.; Czerny, M.; Bossone, E. Sex Differences in Type A Acute Aortic Dissection: A Systematic Review and Meta-Analysis. Eur. J. Prev. Cardiol. 2023, 30, 1074–1089. [Google Scholar] [CrossRef] [PubMed]
- Eranki, A.; Wilson-Smith, A.; Williams, M.L.; Saxena, A.; Mejia, R. Quality of life following surgical repair of acute type A aortic dissection: A systematic review. J. Cardiothorac. Surg. 2022, 17, 118. [Google Scholar] [CrossRef] [PubMed]
- Aaronson, N.K.; Muller, M.; Cohen, P.D.; Essink-Bot, M.L.; Fekkes, M.; Sanderman, R.; Sprangers, M.A.; te Velde, A.; Verrips, E. Translation, validation, and norming of the Dutch language version of the SF-36 Health Survey in community and chronic disease populations. J. Clin. Epidemiol. 1998, 51, 1055–1068. [Google Scholar] [CrossRef]
- Thijssen, C.G.E.; Dekker, S.; Bons, L.R.; Gökalp, A.L.; Kauling, R.M.; van den Bosch, A.E.; Cuypers, J.; Utens, E.; van Kimmenade, R.R.L.; Takkenberg, J.J.M.; et al. Health-related quality of life and lived experiences in males and females with thoracic aortic disease and their partners. Open Heart 2020, 7, e001419. [Google Scholar] [CrossRef]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P.; Initiative, S. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for reporting observational studies. Int. J. Surg. 2014, 12, 1495–1499. [Google Scholar] [CrossRef]
- McHorney, C.A.; Ware, J.E., Jr.; Lu, J.F.; Sherbourne, C.D. The MOS 36-item Short-Form Health Survey (SF-36): III. Tests of data quality, scaling assumptions, and reliability across diverse patient groups. Med. Care 1994, 32, 40–66. [Google Scholar] [CrossRef]
- McHorney, C.A.; Ware, J.E., Jr.; Raczek, A.E. The MOS 36-Item Short-Form Health Survey (SF-36): II. Psychometric and clinical tests of validity in measuring physical and mental health constructs. Med. Care 1993, 31, 247–263. [Google Scholar] [CrossRef] [PubMed]
- Ware, J.E., Jr.; Sherbourne, C.D. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med. Care 1992, 30, 473–483. [Google Scholar] [CrossRef] [PubMed]
- Ware, J.E., Jr. SF-36 health survey update. Spine 2000, 25, 3130–3139. [Google Scholar] [CrossRef] [PubMed]
- Adam, U.; Habazettl, H.; Graefe, K.; Kuppe, H.; Wundram, M.; Kurz, S.D. Health-related quality of life of patients after surgery for acute Type A aortic dissection. Interact. Cardiovasc. Thorac. Surg. 2018, 27, 48–53. [Google Scholar] [CrossRef] [PubMed]
- Endlich, M.; Hamiko, M.; Gestrich, C.; Probst, C.; Mellert, F.; Winkler, K.; Welz, A.; Schiller, W. Long-Term Outcome and Quality of Life in Aortic Type A Dissection Survivors. Thorac. Cardiovasc. Surg. 2016, 64, 91–99. [Google Scholar] [PubMed]
- Jussli-Melchers, J.; Panholzer, B.; Friedrich, C.; Broch, O.; Renner, J.; Schöttler, J.; Rahimi, A.; Cremer, J.; Schoeneich, F.; Haneya, A. Long-term outcome and quality of life following emergency surgery for acute aortic dissection type A: A comparison between young and elderly adults. Eur. J. Cardiothorac. Surg. 2017, 51, 465–471. [Google Scholar] [CrossRef] [PubMed]
- Immer, F.F.; Krähenbühl, E.; Immer-Bansi, A.S.; Berdat, P.A.; Kipfer, B.; Eckstein, F.S.; Saner, H.; Carrel, T.P. Quality of life after interventions on the thoracic aorta with deep hypothermic circulatory arrest. Eur. J. Cardiothorac. Surg. 2002, 21, 10–14. [Google Scholar] [CrossRef] [PubMed]
- Santini, F.; Montalbano, G.; Messina, A.; D’Onofrio, A.; Casali, G.; Viscardi, F.; Luciani, G.B.; Mazzucco, A. Survival and quality of life after repair of acute type A aortic dissection in patients aged 75 years and older justify intervention. Eur. J. Cardiothorac. Surg. 2006, 29, 386–391. [Google Scholar] [CrossRef] [PubMed]
- Sbarouni, E.; Georgiadou, P.; Manavi, M.; Analitis, A.; Beletsioti, C.; Niakas, D.; Iliodromitis, E.; Voudris, V. Long-term outcomes and quality of life following acute type A aortic dissection. Hell. J. Cardiol. 2021, 62, 463–465. [Google Scholar] [CrossRef]
- Olsson, C.; Franco-Cereceda, A. Health-Related Quality of Life in Thoracic Aortic Disease: Part II. After Surgery on the Proximal (Root, Ascending, Arch) Aorta. Aorta 2013, 1, 162–170. [Google Scholar] [CrossRef]
- Gjeilo, K.H.; Stenseth, R.; Wahba, A.; Lydersen, S.; Klepstad, P. Long-term health-related quality of life and survival after cardiac surgery: A prospective study. J. Thorac. Cardiovasc. Surg. 2018, 156, 2183–2190.e2182. [Google Scholar] [CrossRef]
- Schachner, T.; Garrido, F.; Bonaros, N.; Krapf, C.; Dumfarth, J.; Grimm, M. Factors limiting physical activity after acute type A aortic dissection. Wien. Klin. Wochenschr. 2019, 131, 174–179. [Google Scholar] [CrossRef] [PubMed]
- Tang, G.H.; Malekan, R.; Yu, C.J.; Kai, M.; Lansman, S.L.; Spielvogel, D. Surgery for acute type A aortic dissection in octogenarians is justified. J. Thorac. Cardiovasc. Surg. 2013, 145 (Suppl. S3), S186–S190. [Google Scholar] [CrossRef] [PubMed]
- Bojko, M.M.; Suhail, M.; Bavaria, J.E.; Bueker, A.; Hu, R.W.; Harmon, J.; Habertheuer, A.; Milewski, R.K.; Szeto, W.Y.; Vallabhajosyula, P. Midterm outcomes of emergency surgery for acute type A aortic dissection in octogenarians. J. Thorac. Cardiovasc. Surg. 2022, 163, 2–12.e7. [Google Scholar] [CrossRef] [PubMed]
- Chaddha, A.; Kline-Rogers, E.; Braverman, A.C.; Erickson, S.R.; Jackson, E.A.; Franklin, B.A.; Woznicki, E.M.; Jabara, J.T.; Montgomery, D.G.; Eagle, K.A. Survivors of Aortic Dissection: Activity, Mental Health, and Sexual Function. Clin. Cardiol. 2015, 38, 652–659. [Google Scholar] [CrossRef] [PubMed]
- Perk, J.; De Backer, G.; Gohlke, H.; Graham, I.; Reiner, Z.; Verschuren, M.; Albus, C.; Benlian, P.; Boysen, G.; Cifkova, R.; et al. European Guidelines on cardiovascular disease prevention in clinical practice (version 2012): The Fifth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of nine societies and by invited experts). Eur. J. Prev. Cardiol. 2012, 19, 585–667. [Google Scholar]
- Smith, J.R.; Thomas, R.J.; Bonikowske, A.R.; Hammer, S.M.; Olson, T.P. Sex Differences in Cardiac Rehabilitation Outcomes. Circ. Res. 2022, 130, 552–565. [Google Scholar] [CrossRef] [PubMed]
- Pelosi, C.; Kauling, R.M.; Cuypers, J.; van den Bosch, A.E.; Helbing, W.A.; Utens, E.; Legerstee, J.S.; Roos-Hesselink, J.W. Daily life and psychosocial functioning of adults with congenital heart disease: A 40–53 years after surgery follow-up study. Clin. Res. Cardiol. 2023, 112, 880–890. [Google Scholar] [CrossRef] [PubMed]
- Pasadyn, S.R.; Roselli, E.E.; Artis, A.S.; Pasadyn, C.L.; Phelan, D.; Hurley, K.; Desai, M.Y.; Blackstone, E.H. From Tear to Fear: Posttraumatic Stress Disorder in Patients with Acute Type A Aortic Dissection. J. Am. Heart Assoc. 2020, 9, e015060. [Google Scholar] [CrossRef]
- Ebert, J.F.; Huibers, L.; Christensen, B.; Christensen, M.B. Paper- or Web-Based Questionnaire Invitations as a Method for Data Collection: Cross-Sectional Comparative Study of Differences in Response Rate, Completeness of Data, and Financial Cost. J. Med. Internet Res. 2018, 20, e24. [Google Scholar] [CrossRef]



| All Patients (n = 324) | Females (n = 110) | Males (n = 214) | p-Value | Missing % | |
|---|---|---|---|---|---|
| Age at questionnaire (median [IQR])—years | 68.0 [61.0–74.0] | 70.5 [64.3–77.0] | 67.0 [60.0–73.0] | 0.001 | 0.3 |
| Follow-up time—years (median [IQR], (range) | 6.5 [4.0–9.4], (1.7–14.2) | 6.2 [3.9–9.3], (1.7–13.9) | 6.6 [4.2–9.4], (1.7–14.2) | 0.386 | 0.0 |
| Patient demographics at ATAAD presentation | |||||
| Age at ATAAD (mean ± SD)—years | 61.0 ± 10.1 | 63.7 ± 10.3 | 59.7 ± 9.7 | 0.001 | 0.3 |
| BSA (mean ± SD)—m2 | 2.0 ± 0.2 | 1.8 ± 0.16 | 2.1 ± 0.2 | <0.001 | 23.5 |
| History of hypertension (%) | 150 (48.9) | 59 (55.7) | 91 (45.3) | 0.107 | 6.2 |
| History of hyperlipidemia (%) | 37 (11.7) | 13 (12.1) | 24 (11.5) | 1.000 | 2.8 |
| Diabetes mellitus (%) | 3 (0.9) | 2 (1.9) | 1 (0.5) | 0.268 i | 2.2 |
| COPD (%) | 14 (4.4) | 7 (6.4) | 7 (3.3) | 0.327 | 0.9 |
| Current or past smoking ≥ 1 pack years | 90 (62.9) | 27 (56.2) | 63 (66.3) | 0.320 | 55.9 |
| History of CVA or TIA (%) | 14 (4.4) | 6 (5.5) | 8 (3.8) | 0.686 | 0.9 |
| History of MI (%) | 7 (2.2) | 3 (2.7) | 4 (1.9) | 0.695 i | 1.2 |
| Chronic kidney disease (%) | 3 (0.9) | 1 (0.9) | 2 (0.9) | 1.000 i | 0.9 |
| Prior TAA (%) | 21 (6.6) | 11 (10.1) | 10 (4.7) | 0.111 | 1.2 |
| Prior aortic surgery (%) | 5 (1.6) | 0 (0.0) | 5 (2.4) | 0.170 i | 1.5 |
| Prior cardiac surgery (%) | 13 (4.1) | 3 (2.7) | 10 (4.8) | 0.554 i | 1.2 |
| Bicuspid aortic valve (%) | 6 (2.1) | 2 (2.0) | 4 (2.2) | 1.000 i | 11.4 |
| Known connective tissue disease (%) * No; no genetic testing performed No; genetic testing performed but not found | 13 (10.7) 67 (55.4) 41 (33.9) | 3 (7.9) 20 (52.6) 15 (39.5) | 10 (12.0) 47 (56.6) 26 (31.3) | 0.602 i | 62.7 |
| Surgical procedures ** | |||||
| Aortic valve surgery Ascending aortic surgery Aortic arch surgery Descending aortic surgery | 210 (66.5) 315 (97.2) 225 (70.8) 2 (0.6) | 75 (70.8) 107 (97.3) 72 (67.9) 0 (0.0) | 135 (64.3) 208 (97.2) 153 (72.2) 2 (0.9) | 0.306 1.000 0.513 0.551 i | 2.5 0.0 1.9 0.6 |
| DHCA (%) | 124 (39.7) | 45 (42.1) | 79 (38.5) | 0.630 | 3.7 |
| All Patients (n = 324) | Females (n = 110) | Males (n = 214) | p-Value | Missing (%) | |
|---|---|---|---|---|---|
| Physical Functioning | 70.0 (53.8–85.0) | 65.0 (42.5–80.0) | 75.0 (60.0–90.0) | <0.001 | 1.2 |
| Role Physical | 75.0 (25.0–100.0) | 50.0 (0.00–100.0) | 75.0 (25.0–100.0) | 0.015 | 2.2 |
| Bodily Pain | 90.0 (67.5–100.0) | 82.5 (57.5–100.0) | 90.0 (67.5–100.0) | 0.142 | 0.3 |
| General Health | 60.0 (40.0–75.0) | 52.5 (36.3–70.0) | 60.0 (40.0–75.0) | 0.103 | 0.0 |
| Vitality | 65.0 (45.0–80.0) | 60.0 (40.0–75.0) | 65.0 (45.0–80.0) | 0.035 | 0.3 |
| Social Functioning | 87.5 (62.5–100.0) | 75.0 (62.5–100.0) | 87.5 (75.0–100.0) | 0.037 | 0.9 |
| Role Emotional | 100.0 (66.7–100.0) | 100.0 (33.3–100.0) | 100.0 (66.7–100.0) | 0.150 | 2.8 |
| Mental Health | 84.0 (68.0–92.0) | 76.0 (64.0–88.0) | 84.0 (72.0–92.0) | 0.006 | 0.6 |
| PCS | 45.7 (36.7–53.5) | 43.3 (35.0–50.3) | 46.5 (39.1–53.8) | 0.008 | 4.0 |
| MCS | 53.2 (44.2–58.2) | 51.4 (41.6–58.0) | 53.6 (45.1–58.3) | 0.184 | 4.0 |
| Responders (n = 324) | Non-Responders (n = 231) | p-Value | Missing % | |
|---|---|---|---|---|
| Patient demographics | ||||
| Female sex (%) | 110 (34.0) | 79 (34.2) | 1.000 | 0.0 |
| Age (median [IQR])—years | 61.0 [54.0–68.0] | 60.0 [51.0–67.8] | 0.126 | 0.2 |
| BSA (mean ± SD)—m2 | 2.00 ± 0.21 | 1.98 ± 0.20 | 0.347 | 30.7 |
| History of hypertension (%) | 150 (48.9) | 104 (47.1) | 0.749 | 6.0 |
| Hyperlipidemia (%) | 37 (11.7) | 20 (8.8) | 0.330 | 4.3 |
| Diabetes mellitus (%) | 3 (0.9) | 6 (2.6) | 0.175 i | 3.3 |
| COPD (%) | 14 (4.4) | 11 (4.8) | 0.979 | 3.0 |
| Current or past smoking ≥ 1 pack years | 90 (62.9) | 89 (82.4) | 0.001 | 58.2 |
| History of CVA or TIA (%) | 14 (4.4) | 9 (4.0) | 0.991 | 3.4 |
| History of MI (%) | 7 (2.2) | 9 (4.0) | 0.338 | 3.3 |
| Chronic kidney disease (%) | 3 (0.9) | 4 (1.7) | 0.458 i | 3.3 |
| Prior TAA (%) | 21 (6.6) | 15 (6.7) | 1.000 | 4.0 |
| Prior aortic surgery (%) | 5 (1.6) | 7 (3.1) | 0.375 | 3.3 |
| Prior cardiac surgery (%) | 13 (4.1) | 8 (3.5) | 0.899 | 2.7 |
| Bicuspid aortic valve (%) | 6 (2.1) | 6 (3.0) | 0.754 | 13.5 |
| Known connective tissue disease (%) * No; no genetic testing performed No; genetic testing performed but not found | 67 (55.4) 41 (33.9) 13 (10.7) | 40 (51.3) 29 (37.2) 9 (11.5) | 0.852 | 65.8 |
| Surgical procedures | ||||
| Aortic valve surgery Ascending aortic surgery Aortic arch surgery Descending aortic surgery | 210 (66.5) 315 (97.2) 225 (70.8) 2 (0.6) | 116 (52.5) 226 (99.6) 148 (67.0) 2 (0.9) | 0.002 0.053 i 0.400 1.000 i | 5.3 2.6 4.7 2.5 |
| DHCA | 124 (39.7) | 79 (37.1) | 0.602 | 8.1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Meccanici, F.; Thijssen, C.G.E.; Gökalp, A.L.; Bom, A.W.; Geuzebroek, G.S.C.; ter Woorst, J.F.; van Kimmenade, R.R.J.; Post, M.C.; Takkenberg, J.J.M.; Roos-Hesselink, J.W. Long-Term Health-Related Quality of Life following Acute Type A Aortic Dissection with a Focus on Male–Female Differences: A Cross Sectional Study. J. Clin. Med. 2024, 13, 2265. https://doi.org/10.3390/jcm13082265
Meccanici F, Thijssen CGE, Gökalp AL, Bom AW, Geuzebroek GSC, ter Woorst JF, van Kimmenade RRJ, Post MC, Takkenberg JJM, Roos-Hesselink JW. Long-Term Health-Related Quality of Life following Acute Type A Aortic Dissection with a Focus on Male–Female Differences: A Cross Sectional Study. Journal of Clinical Medicine. 2024; 13(8):2265. https://doi.org/10.3390/jcm13082265
Chicago/Turabian StyleMeccanici, Frederike, Carlijn G. E. Thijssen, Arjen L. Gökalp, Annemijn W. Bom, Guillaume S. C. Geuzebroek, Joost F. ter Woorst, Roland R. J. van Kimmenade, Marco C. Post, Johanna J. M. Takkenberg, and Jolien W. Roos-Hesselink. 2024. "Long-Term Health-Related Quality of Life following Acute Type A Aortic Dissection with a Focus on Male–Female Differences: A Cross Sectional Study" Journal of Clinical Medicine 13, no. 8: 2265. https://doi.org/10.3390/jcm13082265
APA StyleMeccanici, F., Thijssen, C. G. E., Gökalp, A. L., Bom, A. W., Geuzebroek, G. S. C., ter Woorst, J. F., van Kimmenade, R. R. J., Post, M. C., Takkenberg, J. J. M., & Roos-Hesselink, J. W. (2024). Long-Term Health-Related Quality of Life following Acute Type A Aortic Dissection with a Focus on Male–Female Differences: A Cross Sectional Study. Journal of Clinical Medicine, 13(8), 2265. https://doi.org/10.3390/jcm13082265