Tannin-Based Microbicidal Coatings for Hospital Privacy Curtains
Abstract
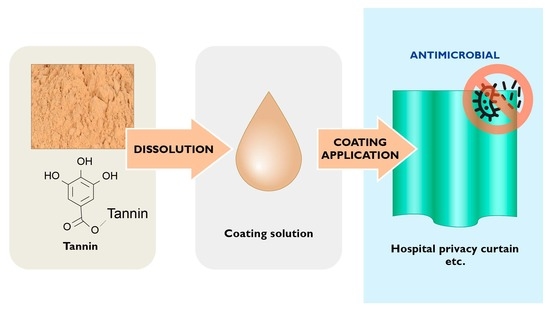
:1. Introduction
2. Materials and Methods
2.1. Tannins
2.2. Characterisation of Tannins
2.3. Preparation and Function of Antimicrobial Curtain Coatings
2.4. Antimicrobial Testing Methods
3. Results and Discussion
3.1. Characterisation of Tannins
3.2. Antibacterial Efficacy of Tannin Powders
3.3. Mechanisms of Action of Tannins
3.4. Laboratory Testing of Tannin Coatings before Hospital Field Study
3.5. Hospital Field Study
3.6. Follow-Up Study
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Das, I.; Lambert, P.; Hill, D.; Noy, M.; Bion, J.; Elliott, T. Carbapenem-resistant Acinetobacter and role of curtains in an outbreak in intensive care units. J. Hosp. Infect. 2002, 50, 110–114. [Google Scholar] [CrossRef]
- Klakus, J.; Vaughan, N.L.; Boswell, T.C. Meticillin-resistant Staphylococcus aureus contamination of hospital curtains. J. Hosp. Infect. 2008, 68, 189–190. [Google Scholar] [CrossRef]
- Trillis III, F.; Eckstein, E.C.; Budavich, R.; Pultz, M.J.; Donskey, C.J. Contamination of hospital curtains with healthcare-associated pathogens. Infect. Control Hosp. Epidemiol. 2008, 29, 1074–1076. [Google Scholar] [CrossRef] [Green Version]
- Ohl, M.; Schweizer, M.; Graham, M.; Heilmann, K.; Boyken, L.; Diekema, D. Hospital privacy curtains are frequently and rapidly contaminated with potentially pathogenic bacteria. Am. J. Infect. Control 2012, 40, 904–906. [Google Scholar] [CrossRef]
- Mahida, N.; Beal, A.; Trigg, D.; Vaughan, N.; Boswell, T. Outbreak of invasive group A streptococcus infection: Contaminated patient curtains and cross-infection on an ear, nose and throat ward. J. Hosp. Infect. 2014, 87, 141–144. [Google Scholar] [CrossRef]
- Shek, K.; Patidar, R.; Kohja, Z.; Liu, S.; Gawaziuk, J.P.; Gawthrop, M.; Kumar, A.; Logsetty, S. Rate of contamination of hospital privacy curtains on a burns and plastic surgery ward: A cross-sectional study. J. Hosp. Infect. 2017, 96, 54–58. [Google Scholar] [CrossRef] [PubMed]
- Woodard, D.R.; Buttner, M.; Cruz, P.; Roeder, J. Microbial contamination of privacy curtains in the emergency department of a metropolitan hospital. J. Hosp. Infect. 2018, 100, e153–e154. [Google Scholar] [CrossRef]
- Cadogan, K.; Bashar, S.; Magnusson, S.; Patidar, R.; Embil, J.; Gawaziuk, J.P.; Gawthrop, M.; Liu, S.; Kumar, A.; Logsetty, S. Assessment of cleaning methods on bacterial burden of hospital privacy curtains: A pilot randomized controlled trial. Sci. Rep. 2021, 11, 21866. [Google Scholar] [CrossRef] [PubMed]
- Brown, L.; Siddiqui, S.; McMullen, A.; Waller, J.; Baer, S. Revisiting the “leading edge” of hospital privacy curtains in the medical intensive care unit. Am. J. Infect. Control 2020, 48, 746–750. [Google Scholar] [CrossRef] [PubMed]
- Al-Tawfiq, J.A.; Bazzi, A.M.; Rabaan, A.A.; Okeahialam, C. The effectiveness of antibacterial curtains in comparison with standard privacy curtains against transmission of microorganisms in a hospital setting. Infez. Med. 2019, 27, 149–154. [Google Scholar] [PubMed]
- Rutala, W.A.; Gergen, M.F.; Sickbert-Bennett, E.E.; Williams, D.A.; Weber, D.J. Effectiveness of improved hydrogen peroxide in decontaminating privacy curtains contaminated with multidrug-resistant pathogens. Am. J. Infect. Control 2014, 42, 426–428. [Google Scholar] [CrossRef] [PubMed]
- Wilson, G.; Jackson, V.; Boyken, L.; Puig-Asensio, M.; Marra, A.R.; Perencevich, E.; Schweizer, M.L.; Diekema, D.; Breheny, P.; Petersen, C. A randomized control trial evaluating efficacy of antimicrobial impregnated hospital privacy curtains in an intensive care setting. Am. J. Infect. Control 2020, 48, 862–868. [Google Scholar] [CrossRef] [PubMed]
- Vickery, K.; Deva, A.; Jacombs, A.; Allan, J.; Valente, P.; Gosbell, I.B. Presence of biofilm containing viable multiresistant organisms despite terminal cleaning on clinical surfaces in an intensive care unit. J. Hosp. Infect. 2012, 80, 52–55. [Google Scholar] [CrossRef] [PubMed]
- Kotsanas, D.; Lovegrove, A.; Sloane, T.L.; Gillespie, E.E. Disposable biocidal cubical curtains: Can they prevent the transfer of bacterial pathogens? Healthc. Infect. 2012, 17, 87–90. [Google Scholar] [CrossRef]
- Schweizer, M.; Graham, M.; Ohl, M.; Heilmann, K.; Boyken, L.; Diekema, D. Novel hospital curtains with antimicrobial properties: A randomized, controlled trial. Infect. Control Hosp. Epidemiol. 2012, 33, 1081–1085. [Google Scholar] [CrossRef] [PubMed]
- Kotsanas, D.; Wijesooriya, W.R.P.L.I.; Sloane, T.; Stuart, R.L.; Gillespie, E.E. The silver lining of disposable sporicidal privacy curtains in an intensive care unit. Am. J. Infect. Control 2014, 42, 366–370. [Google Scholar] [CrossRef]
- Luk, S.; Chow, V.C.Y.; Yu, K.C.H.; Hsu, E.K.; Tsang, N.C.; Chuang, V.W.M.; Lai, C.K.C.; Hui, M.; Lee, R.A.; Lai, W.M.; et al. Effectiveness of antimicrobial hospital curtains on reducing bacterial contamination–A multicenter study. Infect. Control Hosp. Epidemiol. 2019, 40, 164–170. [Google Scholar] [CrossRef]
- Khan, A.S. Trees with Antimicrobial Activities. In Medicinally Important Trees; Springer: Cham, Switzerland, 2017; pp. 85–108. [Google Scholar]
- Pizzi, A. Tannins: Prospectives and actual industrial applications. Biomolecules 2019, 9, 344. [Google Scholar] [CrossRef] [Green Version]
- Scalbert, A. Antimicrobial properties of tannins. Phytochemistry 1991, 30, 3875–3883. [Google Scholar] [CrossRef]
- Ekambaram, S.P.; Perumal, S.S.; Balakrishnan, A. Scope of Hydrolysable Tannins as Possible Antimicrobial Agent. Phyther. Res. 2016, 30, 1035–1045. [Google Scholar] [CrossRef]
- Buzzini, P.; Arapitsas, P.; Goretti, M.; Turchetti, B.; Pinelli, P.; Ieri, F.; Romani, A. Antimicrobial and antiviral activity of hydrolysable tannins. Mini-Rev. Med. Chem. 2008, 8, 1179–1187. [Google Scholar] [CrossRef] [PubMed]
- Rauf, A.; Imran, M.; Abu-Izneid, T.; Iahtisham-Ul-Haq; Patel, S.; Pan, X.; Naz, S.; Sanches Silva, A.; Saeed, F.; Rasul Suleria, H.A. Proanthocyanidins: A comprehensive review. Biomed. Pharmacother. 2019, 116, 108999. [Google Scholar] [CrossRef] [PubMed]
- Farha, A.K.; Yang, Q.-Q.; Kim, G.; Li, H.-B.; Zhu, F.; Liu, H.-Y.; Gan, R.-Y.; Corke, H. Tannins as an alternative to antibiotics. Food Biosci. 2020, 38, 100751. [Google Scholar] [CrossRef]
- Borisova, M.P.; Kataev, A.A.; Sivozhelezov, V.S. Action of tannin on cellular membranes: Novel insights from concerted studies on lipid bilayers and native cells. Biochim. Biophys. Acta Biomembr. 2019, 1861, 1103–1111. [Google Scholar] [CrossRef] [PubMed]
- Villanueva, X.; Zhen, L.; Ares, J.N.; Vackier, T.; Lange, H.; Crestini, C.; Steenackers, H.P. Effect of chemical modifications of tannins on their antimicrobial and antibiofilm effect against Gram-negative and Gram-positive bacteria. Front. Microbiol. 2023, 13, 987164. [Google Scholar] [CrossRef]
- Widsten, P.; Cruz, C.D.; Fletcher, G.C.; Pajak, M.A.; McGhie, T.K. Tannins and extracts of fruit byproducts: Antibacterial activity against foodborne bacteria and antioxidant capacity. J. Agric. Food Chem. 2014, 62, 11146–11156. [Google Scholar] [CrossRef]
- Pizzi, A.; Pasch, H.; Rode, K.; Giovando, S. Polymer structure of commercial hydrolyzable tannins by matrix-assisted laser desorption/ ionization-time-of-flight mass spectrometry. J. Appl. Polym. Sci. 2009, 113, 3847–3859. [Google Scholar] [CrossRef]
- Giovando, S.; Pizzi, A.; Pasch, H.; Pretorius, N. Structure and oligomers distribution of commercial tara (Caesalpina spinosa) hydrolysable tannin. Pro Ligno 2013, 9, 22–31. [Google Scholar]
- Clifford, M.N.; Stoupi, S.; Kuhnert, N. Profiling and characterization by LC-MSn of the galloylquinic acids of green tea, tara tannin, and tannic acid. J. Agric. Food Chem. 2007, 55, 2797–2807. [Google Scholar] [CrossRef]
- Lamb, L.H.; Decusati, O.G. Manufacturing Process for Quaternary Ammonium Tannate, a Vegetable Coagulating/Flocculating Agent. US Patent US6478986B1, 12 November 2002. [Google Scholar]
- Aguilar-Galvez, A.; Noratto, G.; Chambi, F.; Debaste, F.; Campos, D. Potential of tara (Caesalpinia spinosa) gallotannins and hydrolysates as natural antibacterial compounds. Food Chem. 2014, 156, 301–304. [Google Scholar] [CrossRef]
- Granata, A.; Argyropoulos, D.S. 2-Chloro-4,4,5,5-tetramethyl-1,3,2-dioxaphospholane, a Reagent for the Accurate Determination of the Uncondensed and Condensed Phenolic Moieties in Lignins. J. Agric. Food Chem. 1995, 43, 1538–1544. [Google Scholar] [CrossRef]
- Nordlund, E.; Lille, M.; Silventoinen, P.; Nygren, H.; Seppänen-Laakso, T.; Mikkelson, A.; Aura, A.-M.; Heiniö, R.-L.; Nohynek, L.; Puupponen-Pimiä, R.; et al. Plant cells as food–A concept taking shape. Food Res. Int. 2018, 107, 297–305. [Google Scholar] [CrossRef]
- Tenkanen, M.; Siika-Aho, M. An α-glucuronidase of Schizophyllum commune acting on polymeric xylan. J. Biotechnol. 2000, 78, 149–161. [Google Scholar] [CrossRef] [PubMed]
- Strobel, M.; Jones, V.; Lyons, C.S.; Ulsh, M.; Kushner, M.J.; Dorai, R.; Branch, M.C. A Comparison of Corona-Treated and Flame-Treated Polypropylene Films. Plasmas Polym. 2003, 8, 61–95. [Google Scholar] [CrossRef]
- Abdalla, S.; Pizzi, A.; Bahabri, F.; Ganash, A. Analysis of valonia oak (Quercus aegylops) acorn tannin and wood adhesives application. BioResources 2015, 10, 7165–7177. [Google Scholar] [CrossRef] [Green Version]
- Ozgunay, H.; Sari, O.; Tozan, M. Molecular investigation of valonea tannin. J. Am. Leather Chem. Assoc. 2007, 102, 154–157. [Google Scholar]
- Pasch, H.; Pizzi, A. Considerations on the macromolecular structure of chestnut ellagitannins by matrix-assisted laser desorption/ionization-time-of-flight mass spectrometry. J. Appl. Polym. Sci. 2002, 85, 429–437. [Google Scholar] [CrossRef]
- Widsten, P.; Salo, S.; Hakkarainen, T.; Nguyen, T.L.; Borrega, M.; Fearon, O. Antimicrobial and flame-retardant coatings prepared from nano- and microparticles of unmodified and nitrogen-modified polyphenols. Polymers 2023, 15, 992. [Google Scholar] [CrossRef] [PubMed]
- National Committee for Clinical Laboratory Standards (NCCLS). Methods for Dilution Antimicrobial Susceptibility Tests for Bacteria That Grow Aerobically, 3rd ed.; Clinical and Laboratory Standards Institute (CLSI): Villanova, PA, USA, 1993. [Google Scholar]
- Alakomi, H.-L.; Puupponen-Pimiä, R.; Aura, A.-M.; Helander, I.M.; Nohynek, L.; Oksman-Caldentey, K.-M.; Saarela, M. Weakening of Salmonella with selected microbial metabolites of berry-derived phenolic compounds and organic acids. J. Agric. Food Chem. 2007, 55, 3905–3912. [Google Scholar] [CrossRef]
- Alakomi, H.-L.; Paananen, A.; Suihko, M.-L.; Helander, I.M.; Saarela, M. Weakening effect of cell permeabilizers on gram-negative bacteria causing biodeterioration. Appl. Environ. Microbiol. 2006, 72, 4695–4703. [Google Scholar] [CrossRef] [Green Version]
- Virkkunen, M.; Mannila, J.; Niemelä, K.; Salo, S.; Widsten, P.; Jetsu, P.; Jämsén, M.; Alakoski, E.; Mäkelä, J.; Mustonen, P.; et al. Potential of Novel Biobased Materials for the Hospital Uses; Final Report of the Sami&Samu Project; Technical Report VTT-R-00787-21 for VTT Technical Research Centre of Finland: Espoo, Finland, 2021. [Google Scholar]












| Species of Origin | Tree Component | Tannin Type | Main Tannin Subtype |
|---|---|---|---|
| Valonea oak (Quercus ithaburensis) | Acorn cups | HT 1 | Gallo- and ellagitannins [37,38] |
| Tara (Caesalpina spinosa) | Seed pods | HT 1 | Gallotannins including galloquinic and caffeoylquinic acid units) [30,32,39] |
| Chestnut (Castanea sp.) | Bark/wood | HT 1 | Gallo- and ellagitannins [28,39] |
| Mimosa (Acacia mearnsii) | Bark | CT 1 | Prorobinetinidin [27,37]; catechin and gallocatechin di- and oligomers [27] |
| Quebracho (Schinopsis sp.) | Bark | CT 1 | Profisetinidin [37] |
| Mimosa (Acacia mearnsii) | Bark | Cationic CT 1 | Cationised [31] mimosa tannin |
| Tannin | Aliphatic OH, mmol/g | Phenolic OH, mmol/g | COOH, mmol/g | N, % | Carbohydrates, % | Molar Mass, g/mol | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| In Tannin | Total | Ortho-Substitution | Total | Mw | Mn | ||||||
| None | Mono | Di | |||||||||
| Tannic acid | 0.02 | 0.44 | 0.00 | 9.56 | 4.71 | 14.30 | 0.56 | 0.01 | 1.4 | 883 | 732 |
| Chestnut | 0.45 | 4.55 | 0.20 | 4.06 | 2.26 | 7.52 | 0.36 | 0.11 | 12.6 | 1456 | 951 |
| Valonea | 0.51 | 5.15 | 0.10 | 2.39 | 1.83 | 5.08 | 0.40 | 0.44 | 9.1 | 1269 | 869 |
| Tara-E | 0.16 | 4.68 | 0.04 | 7.14 | 3.62 | 10.84 | 0.25 | 0.17 | 5.2 | 925 | 725 |
| Tara-W | 0.19 | 4.97 | 0.02 | 6.37 | 3.25 | 9.66 | 0.25 | 0.42 | 7.1 | 913 | 718 |
| Tara powder | 1.17 | ||||||||||
| Mimosa | 5.30 | 8.52 | 0.32 | 0.16 | 6.7 | 1697 | 1073 | ||||
| Quebracho | 3.78 | 7.69 | 0.42 | 0.57 | 8.7 | 1820 | 1161 | ||||
| TanFloc SG | 7.60 | 4.2 | 2677 | 1197 | |||||||
| TanFloc SH | 6.61 | 3.1 | 3178 | 1273 | |||||||
| Tannin Type | Hydrolysable | Condensed | Cationised Condensed 2 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Tannin | Ampicillin (Control) | Chestnut | Tara 1 | Tara-E | Tara-W | Valonea | Mimosa | Quebracho | TF-SG | TF-SH |
| S. aureus 3 log reduction | 3.8 | 4.2 | 5.0 | 2.1 | 3.6 | 3.1 | 0.5 | 5.0 | 5.0 | |
| E. coli 4 log reduction | 5.0 | 5.0 | 5.0 | 5.0 | 5.0 | 2.1 | 3.0 | 5.0 | 5.0 | |
| S. aureus 3 | 0.25 | 0.83 | 5.7 | 8.0 | 8.0 | 0.58 | 0.58 | 1.67 | 1.44 | >8.0 |
| MIC, mg/mL | ||||||||||
| MRSA 5 | ||||||||||
| MIC, mg/mL | 2.00 | 1.0 | 8.0 | 4.0 | 1.0 | 0.5 | 1.0 | 2.0 | 0.5 | >8.0 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Widsten, P.; Salo, S.; Niemelä, K.; Helin, H.; Salonen, M.; Alakomi, H.-L. Tannin-Based Microbicidal Coatings for Hospital Privacy Curtains. J. Funct. Biomater. 2023, 14, 187. https://doi.org/10.3390/jfb14040187
Widsten P, Salo S, Niemelä K, Helin H, Salonen M, Alakomi H-L. Tannin-Based Microbicidal Coatings for Hospital Privacy Curtains. Journal of Functional Biomaterials. 2023; 14(4):187. https://doi.org/10.3390/jfb14040187
Chicago/Turabian StyleWidsten, Petri, Satu Salo, Klaus Niemelä, Hanna Helin, Minna Salonen, and Hanna-Leena Alakomi. 2023. "Tannin-Based Microbicidal Coatings for Hospital Privacy Curtains" Journal of Functional Biomaterials 14, no. 4: 187. https://doi.org/10.3390/jfb14040187
APA StyleWidsten, P., Salo, S., Niemelä, K., Helin, H., Salonen, M., & Alakomi, H. -L. (2023). Tannin-Based Microbicidal Coatings for Hospital Privacy Curtains. Journal of Functional Biomaterials, 14(4), 187. https://doi.org/10.3390/jfb14040187