Nanomaterials for Cardiac Myocyte Tissue Engineering
Abstract
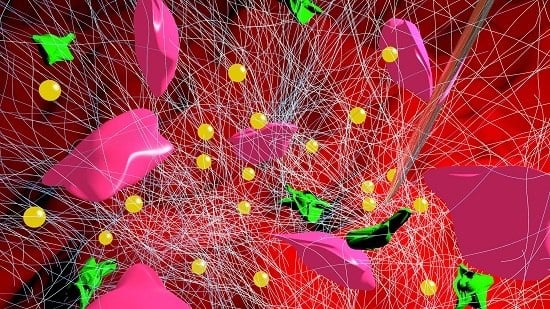
:1. Introduction
2. Scaffolds
2.1. Synthetic Materials
2.2. Natural Materials
2.3. Nanotubes and Nanoparticles
2.4. Electrospun Scaffolds
2.5. Outlook
3. Patches
3.1. Carbon Nanofiber Reinforced Patches
3.2. Gold Nanofiber Reinforced Patches
3.3. Outlook
4. Injectable Scaffolds
5. Miscellaneous Approaches
6. Toxicity
7. Conclusions
Acknowledgments
Conflicts of Interest
Abbreviations
| AU | Gold |
| CBN | Carbon Based Nanomaterials |
| CM | Cardiomyocyte |
| CNF | Carbon Nanofibers |
| CNT | Carbon Nanotube |
| CVD | Cardiovasular Disease |
| Cx43 | Connexin 43 |
| EPR | Enhanced Permeability and Retention |
| FDA | Food and Drug Administration |
| GelMA | Gelatin Methacrylate |
| LSPR | Localized Surface Plasmon Resonance |
| LVAD | Left Ventricular Assist Device |
| mESC | mouse Embryonic Stem Cells |
| MWNT | Multi-walled Carbon Nanotube |
| OPF | Oligo[poly(ethylene glycol) fumarate] |
| PEG | Poly(ethylene glycol) |
| PGA | Poly(glycolic) acid |
| PCL | Poly(caprolactone) |
| PLGA | Poly(lactic-co-glycolic) acid |
| PLA | Polylactic acid |
| PPy | Polypyrrole |
| PG | Poly(glycerol sebecate) and gelatin |
| PGS | Poly(glycerol sebecate) |
| RNT | Rosette Nanotubes |
| SD | Sprague–Dawley |
| SWNT | Single-walled Carbon Nanotube |
References
- Mozaffarian, D.; Benjamin, E.J.; Go, A.S.; Arnett, D.K.; Blaha, M.J.; Cushman, M.; Das, S.R.; de Ferranti, S.; Despres, J.P.; Fullerton, H.J.; et al. Heart Disease and Stroke Statistics-2016 Update: A Report From the American Heart Association. Circulation 2016, 133, e38–e360. [Google Scholar] [CrossRef] [PubMed]
- Thygesen, K.; Alpert, J.S.; White, H.D. Universal definition of myocardial infarction. J. Am. Coll. Cardiol. 2007, 50, 2173–2195. [Google Scholar] [CrossRef] [PubMed]
- Woodcock, E.A.; Matkovich, S.J. Cardiomyocytes structure, function and associated pathologies. Int. J. Biochem. Cell Biol. 2005, 37, 1746–1751. [Google Scholar] [CrossRef] [PubMed]
- Vunjak-Novakovic, G.; Tandon, N.; Godier, A.; Maidhof, R.; Marsano, A.; Martens, T.P.; Radisic, M. Challenges in cardiac tissue engineering. Tissue Eng. Part B Rev. 2009, 16, 169–187. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez, L.E.; Suarez, E.E.; Loebe, M.; Bruckner, B.A. Ventricular assist devices (VAD) therapy: New technology, new hope? Methodist DeBakey Cardiovasc. J. 2013, 9, 32–37. [Google Scholar] [CrossRef] [PubMed]
- Dimmeler, S.; Burchfield, J.; Zeiher, A.M. Cell-based therapy of myocardial infarction. Arterioscler. Thromb. Vasc. Biol. 2008, 28, 208–216. [Google Scholar] [CrossRef] [PubMed]
- Bouten, C.; Dankers, P.; Driessen-Mol, A.; Pedron, S.; Brizard, A.; Baaijens, F. Substrates for cardiovascular tissue engineering. Adv. Drug Deliv. Rev. 2011, 63, 221–241. [Google Scholar] [CrossRef] [PubMed]
- Anversa, P.; Kajstura, J.; Rota, M.; Leri, A. Regenerating new heart with stem cells. J. Clin. Investig. 2013, 123, 62–70. [Google Scholar] [CrossRef] [PubMed]
- Laflamme, M.A.; Murry, C.E. Regenerating the heart. Nat. Biotechnol. 2005, 23, 845–856. [Google Scholar] [CrossRef] [PubMed]
- Passier, R.; van Laake, L.W.; Mummery, C.L. Stem-cell-based therapy and lessons from the heart. Nature 2008, 453, 322–329. [Google Scholar] [CrossRef] [PubMed]
- Ye, Q.; Zünd, G.; Benedikt, P.; Jockenhoevel, S.; Hoerstrup, S.P.; Sakyama, S.; Hubbell, J.A.; Turina, M. Fibrin gel as a three dimensional matrix in cardiovascular tissue engineering. Eur. J. Cardio-Thorac. Surg. 2000, 17, 587–591. [Google Scholar] [CrossRef]
- Leor, J.; Patterson, M.; Quinones, M.J.; Kedes, L.H.; Kloner, R.A. Transplantation of fetal myocardial tissue into the infarcted myocardium of rat: A potential method for repair of infarcted myocardium? Circulation 1996, 94, 332–336. [Google Scholar]
- Zhang, L.; Webster, T.J. Nanotechnology and nanomaterials: Promises for improved tissue regeneration. Nano Today 2009, 4, 66–80. [Google Scholar] [CrossRef]
- Gonsalves, K.; Halberstadt, C.; Laurencin, C.T.; Nair, L. Biomedical Nanostructures; John Wiley and Sons: New York, NY, USA, 2007. [Google Scholar]
- Fahlman, B.D. Semiconducting Materials, Materials Chemistry; Springer Netherlands: Berlin, Germany, 2007; pp. 153–219. [Google Scholar]
- Heydarkhan-Hagvall, S.; Schenke-Layland, K.; Dhanasopon, A.P.; Rofail, F.; Smith, H.; Wu, B.M.; Shemin, R.; Beygui, R.E.; MacLellan, W.R. Three-dimensional electrospun ECM-based hybrid scaffolds for cardiovascular tissue engineering. Biomaterials 2008, 29, 2907–2914. [Google Scholar] [CrossRef] [PubMed]
- Hutmacher, D.W. Scaffold design and fabrication technologies for engineering tissues—State of the art and future perspectives. J. Biomater. Sci. Polym. Ed. 2001, 12, 107–124. [Google Scholar] [CrossRef] [PubMed]
- Chen, Q.Z.; Bismarck, A.; Hansen, U.; Junaid, S.; Tran, M.Q.; Harding, S.E.; Ali, N.N.; Boccaccini, A.R. Characterisation of a soft elastomer poly(glycerol sebacate) designed to match the mechanical properties of myocardial tissue. Biomaterials 2008, 29, 47–57. [Google Scholar] [CrossRef] [PubMed]
- Ciardelli, G.; Chiono, V.; Vozzi, G.; Pracella, M.; Ahluwalia, A.; Barbani, N.; Cristallini, C.; Giusti, P. Blends of poly(ε-caprolactone) and polysaccharides in tissue engineering applications. Biomacromolecules 2005, 6, 1961–1976. [Google Scholar] [CrossRef] [PubMed]
- Alconcel, S.N.; Baas, A.S.; Maynard, H.D. FDA-approved poly(ethylene glycol)—Protein conjugate drugs. Polym. Chem. 2011, 2, 1442–1448. [Google Scholar] [CrossRef]
- Greenwald, R. PEG drugs: An overview. J. Control. Release 2001, 74, 159–171. [Google Scholar] [CrossRef]
- Kim, D.H.; Kim, P.; Song, I.; Cha, J.M.; Lee, S.H.; Kim, B.; Suh, K.Y. Guided three-dimensional growth of functional cardiomyocytes on polyethylene glycol nanostructures. Langmuir 2006, 22, 5419–5426. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.H.; Lipke, E.A.; Kim, P.; Cheong, R.; Thompson, S.; Delannoy, M.; Suh, K.Y.; Tung, L.; Levchenko, A. Nanoscale cues regulate the structure and function of macroscopic cardiac tissue constructs. Proc. Natl. Acad. Sci. USA 2010, 107, 565–570. [Google Scholar] [CrossRef] [PubMed]
- Hurrell, S.; Milroy, G.E.; Cameron, R.E. The degradation of polyglycolide in water and deuterium oxide. Part I: The effect of reaction rate. Polymer 2003, 44, 1421–1424. [Google Scholar] [CrossRef]
- Deng, C.; Yang, X.; Weng, J. Fabrication and in vitro bioactivity of poly(ε-caprolactone) composites filled with silane-modified nano-apatite particles. Int. J. Polym. Mater. 2011, 60, 374–383. [Google Scholar] [CrossRef]
- Griffith, L. Polymeric biomaterials. Acta Mater. 2000, 48, 263–277. [Google Scholar] [CrossRef]
- Aghdam, R.M.; Shakhesi, S.; Najarian, S.; Mohammadi, M.M.; Ahmadi Tafti, S.H.; Mirzadeh, H. Fabrication of a nanofibrous scaffold for the in vitro culture of cardiac progenitor cells for myocardial regeneration. Int. J. Polym. Mater. Polym. Biomaterials 2014, 63, 229–239. [Google Scholar] [CrossRef]
- Makadia, H.K.; Siegel, S.J. Poly lactic-co-glycolic acid (PLGA) as biodegradable controlled drug delivery carrier. Polymers 2011, 3, 1377–1397. [Google Scholar] [CrossRef] [PubMed]
- Simon-Yarza, T.; Rossi, A.; Heffels, K.H.; Prosper, F.; Groll, J.; Blanco-Prieto, M.J. Polymeric electrospun scaffolds: Neuregulin encapsulation and biocompatibility studies in a model of myocardial ischemia. Tissue Eng. Part A 2015, 21, 1654–1661. [Google Scholar] [CrossRef] [PubMed]
- Lakshmanan, R.; Krishnan, U.M.; Sethuraman, S. Living cardiac patch: the elixir for cardiac regeneration. Expert Opin. Biol. Ther. 2012, 12, 1623–1640. [Google Scholar] [CrossRef] [PubMed]
- Kotwal, A.; Schmidt, C.E. Electrical stimulation alters protein adsorption and nerve cell interactions with electrically conducting biomaterials. Biomaterials 2001, 22, 1055–1064. [Google Scholar] [CrossRef]
- Garner, B.; Georgevich, A.; Hodgson, A.; Liu, L.; Wallace, G. Polypyrrole heparin composites as stimulus responsive substrates for endothelial cell growth. J. Biomed. Mater. Res. 1999, 44, 121–129. [Google Scholar] [CrossRef]
- Wang, X.; Gu, X.; Yuan, C.; Chen, S.; Zhang, P.; Zhang, T.; Yao, J.; Chen, F.; Chen, G. Evaluation of biocompatibility of polypyrrole in vitro and in vivo. J. Biomed. Mater. Res. Part A 2004, 68, 411–422. [Google Scholar] [CrossRef] [PubMed]
- Mihardja, S.S.; Sievers, R.E.; Lee, R.J. The effect of polypyrrole on arteriogenesis in an acute rat infarct model. Biomaterials 2008, 29, 4205–4210. [Google Scholar] [CrossRef] [PubMed]
- Kai, D.; Prabhakaran, M.P.; Jin, G.; Ramakrishna, S. Polypyrrole contained electrospun conductive nanofibrous membranes for cardiac tissue engineering. J. Biomed. Mater. Res. Part A 2011, 99, 376–385. [Google Scholar] [CrossRef] [PubMed]
- Li, W.; Danielson, K.G.; Alexander, P.G.; Tuan, R.S. Biological response of chondrocytes cultured in three dimensional nanofibrous poly(ε-caprolactone) scaffolds. J. Biomed. Mater. Res. Part A 2003, 67, 1105–1114. [Google Scholar] [CrossRef] [PubMed]
- Pham, Q.P.; Sharma, U.; Mikos, A.G. Electrospinning of polymeric nanofibers for tissue engineering applications: A review. Tissue Eng. 2006, 12, 1197–1211. [Google Scholar] [CrossRef] [PubMed]
- Pelouch, V.; Dixon, I.M.; Golfman, L.; Beamish, R.E.; Dhalla, N.S. Role of extracellular matrix proteins in heart function. Mol. Cell. Biochem. 1993, 129, 101–120. [Google Scholar] [CrossRef] [PubMed]
- Knowlton, A.A.; Connelly, C.M.; Romo, G.M.; Mamuya, W.; Apstein, C.S.; Brecher, P. Rapid expression of fibronectin in the rabbit heart after myocardial infarction with and without reperfusion. J. Clin. Investig. 1992, 89, 1060–1068. [Google Scholar] [CrossRef] [PubMed]
- Van Den Bulcke, A.I.; Bogdanov, B.; De Rooze, N.; Schacht, E.H.; Cornelissen, M.; Berghmans, H. Structural and rheological properties of methacrylamide modified gelatin hydrogels. Biomacromolecules 2000, 1, 31–38. [Google Scholar] [CrossRef] [PubMed]
- Gasperini, L.; Mano, J.F.; Reis, R.L. Natural polymers for the microencapsulation of cells. J. R. Soc. Interface R. Soc. 2014, 11. [Google Scholar] [CrossRef] [PubMed]
- Ajayan, P.M. Nanotubes from Carbon. Chem. Rev. 1999, 99, 1787–1800. [Google Scholar] [CrossRef] [PubMed]
- Bianco, A.; Kostarelos, K.; Partidos, C.D.; Prato, M. Biomedical applications of functionalised carbon nanotubes. Chem. Commun. 2005. [Google Scholar] [CrossRef] [PubMed]
- Zhou, J.; Chen, J.; Sun, H.; Qiu, X.; Mou, Y.; Liu, Z.; Zhao, Y.; Li, X.; Han, Y.; Duan, C. Engineering the heart: Evaluation of conductive nanomaterials for improving implant integration and cardiac function. Sci. Rep. 2014, 4. [Google Scholar] [CrossRef] [PubMed]
- Martinelli, V.; Cellot, G.; Toma, F.M.; Long, C.S.; Caldwell, J.H.; Zentilin, L.; Giacca, M.; Turco, A.; Prato, M.; Ballerini, L. Carbon nanotubes promote growth and spontaneous electrical activity in cultured cardiac myocytes. Nano Lett. 2012, 12, 1831–1838. [Google Scholar] [CrossRef] [PubMed]
- Shin, S.R.; Jung, S.M.; Zalabany, M.; Kim, K.; Zorlutuna, P.; Kim, S.B.; Nikkhah, M.; Khabiry, M.; Azize, M.; Kong, J. Carbon-nanotube-embedded hydrogel sheets for engineering cardiac constructs and bioactuators. ACS Nano 2013, 7, 2369–2380. [Google Scholar] [CrossRef] [PubMed]
- Jacot, J.G.; McCulloch, A.D.; Omens, J.H. Substrate stiffness affects the functional maturation of neonatal rat ventricular myocytes. Biophys. J. 2008, 95, 3479–3487. [Google Scholar] [CrossRef] [PubMed]
- Fleischer, S.; Shevach, M.; Feiner, R.; Dvir, T. Coiled fiber scaffolds embedded with gold nanoparticles improve the performance of engineered cardiac tissues. Nanoscale 2014, 6, 9410–9414. [Google Scholar] [CrossRef] [PubMed]
- Hanley, P.J.; Young, A.A.; LeGrice, I.J.; Edgar, S.G.; Loiselle, D.S. 3-Dimensional configuration of perimysial collagen fibres in rat cardiac muscle at resting and extended sarcomere lengths. J. Physiol. 1999, 517, 831–837. [Google Scholar] [CrossRef] [PubMed]
- Iyer, R.K.; Chiu, L.L.; Reis, L.A.; Radisic, M. Engineered cardiac tissues. Curr. Opin. Biotechnol. 2011, 22, 706–714. [Google Scholar] [CrossRef] [PubMed]
- Kai, D.; Prabhakaran, M.P.; Jin, G.; Ramakrishna, S. Guided orientation of cardiomyocytes on electrospun aligned nanofibers for cardiac tissue engineering. J. Biomed. Mater. Res. Part B Appl. Biomater. 2011, 98, 379–386. [Google Scholar] [CrossRef] [PubMed]
- Shin, M.; Ishii, O.; Sueda, T.; Vacanti, J. Contractile cardiac grafts using a novel nanofibrous mesh. Biomaterials 2004, 25, 3717–3723. [Google Scholar] [CrossRef] [PubMed]
- Ravichandran, R.; Venugopal, J.R.; Sundarrajan, S.; Mukherjee, S.; Sridhar, R.; Ramakrishna, S. Minimally invasive injectable short nanofibers of poly (glycerol sebacate) for cardiac tissue engineering. Nanotechnology 2012, 23. [Google Scholar] [CrossRef] [PubMed]
- Kofidis, T.; de Bruin, J.L.; Hoyt, G.; Lebl, D.R.; Tanaka, M.; Yamane, T.; Chang, C.P.; Robbins, R.C. Injectable bioartificial myocardial tissue for large-scale intramural cell transfer and functional recovery of injured heart muscle. J. Thorac. Cardiovasc. Surg. 2004, 128, 571–578. [Google Scholar] [CrossRef] [PubMed]
- Tian, B.; Liu, J.; Dvir, T.; Jin, L.; Tsui, J.H.; Qing, Q.; Suo, Z.; Langer, R.; Kohane, D.S.; Lieber, C.M. Macroporous nanowire nanoelectronic scaffolds for synthetic tissues. Nat. Mater. 2012, 11, 986–994. [Google Scholar] [CrossRef] [PubMed]
- Dvir, T.; Timko, B.P.; Brigham, M.D.; Naik, S.R.; Karajanagi, S.S.; Levy, O.; Jin, H.; Parker, K.K.; Langer, R.; Kohane, D.S. Nanowired three-dimensional cardiac patches. Nat. Nanotechnol. 2011, 6, 720–725. [Google Scholar] [CrossRef] [PubMed]
- Stout, D.A.; Yoo, J.; Santiago-Miranda, A.N.; Webster, T.J. Mechanisms of greater cardiomyocyte functions on conductive nanoengineered composites for cardiovascular application. Int. J. Nanomed. 2012, 7, 5653–5669. [Google Scholar]
- Kharaziha, M.; Shin, S.R.; Nikkhah, M.; Topkaya, S.N.; Masoumi, N.; Annabi, N.; Dokmeci, M.R.; Khademhosseini, A. Tough and flexible CNT polymeric hybrid scaffolds for engineering cardiac constructs. Biomaterials 2014, 35, 7346–7354. [Google Scholar] [CrossRef] [PubMed]
- Hu, M.; Chen, J.; Li, Z.Y.; Au, L.; Hartland, G.V.; Li, X.; Marquez, M.; Xia, Y. Gold nanostructures: engineering their plasmonic properties for biomedical applications. Chem. Soc. Rev. 2006, 35, 1084–1094. [Google Scholar] [CrossRef] [PubMed]
- Shevach, M.; Maoz, B.M.; Feiner, R.; Shapira, A.; Dvir, T. Nanoengineering gold particle composite fibers for cardiac tissue engineering. J. Mater. Chem. B 2013, 1, 5210–5217. [Google Scholar] [CrossRef]
- Spector, M.; Lim, T.C. Injectable biomaterials: A perspective on the next wave of injectable therapeutics. Biomed. Mater. 2016, 11. [Google Scholar] [CrossRef] [PubMed]
- Lin, Y.D.; Yeh, M.L.; Yang, Y.J.; Tsai, D.C.; Chu, T.Y.; Shih, Y.Y.; Chang, M.Y.; Liu, Y.W.; Tang, A.C.; Chen, T.Y.; et al. Intramyocardial peptide nanofiber injection improves postinfarction ventricular remodeling and efficacy of bone marrow cell therapy in pigs. Circulation 2010, 122, S132–S141. [Google Scholar] [CrossRef] [PubMed]
- Singelyn, J.M.; DeQuach, J.A.; Seif-Naraghi, S.B.; Littlefield, R.B.; Schup-Magoffin, P.J.; Christman, K.L. Naturally derived myocardial matrix as an injectable scaffold for cardiac tissue engineering. Biomaterials 2009, 30, 5409–5416. [Google Scholar] [CrossRef] [PubMed]
- Park, D.; Wu, W.; Wang, Y. A functionalizable reverse thermal gel based on a polyurethane/PEG block copolymer. Biomaterials 2011, 32, 777–786. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Liu, Z.; Li, D.; Guo, X.; Kasper, F.K.; Duan, C.; Zhou, J.; Mikos, A.G.; Wang, C. Injectable biodegradable hydrogels for embryonic stem cell transplantation: improved cardiac remodelling and function of myocardial infarction. J. Cell. Mol. Med. 2012, 16, 1310–1320. [Google Scholar] [CrossRef] [PubMed]
- Paul, A.; Hasan, A.; Kindi, H.A.; Gaharwar, A.K.; Rao, V.T.; Nikkhah, M.; Shin, S.R.; Krafft, D.; Dokmeci, M.R.; Shum-Tim, D. Injectable graphene oxide/hydrogel-based angiogenic gene delivery system for vasculogenesis and cardiac repair. ACS Nano 2014, 8, 8050–8062. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, M.M.; Gianneschi, N.C.; Christman, K.L. Developing injectable nanomaterials to repair the heart. Curr. Opin. Biotechnol. 2015, 34, 225–231. [Google Scholar] [CrossRef] [PubMed]
- Swyer, T.W.; Strom, J.; Larson, D.F. Nanoparticle oxygen delivery to the ischemic heart. Perfusion 2014, 29, 539–543. [Google Scholar] [CrossRef] [PubMed]
- Dvir, T.; Bauer, M.; Schroeder, A.; Tsui, J.H.; Anderson, D.G.; Langer, R.; Liao, R.; Kohane, D.S. Nanoparticles targeting the infarcted heart. Nano Lett. 2011, 11, 4411–4414. [Google Scholar] [CrossRef] [PubMed]
- Sharifi, S.; Behzadi, S.; Laurent, S.; Forrest, M.L.; Stroeve, P.; Mahmoudi, M. Toxicity of nanomaterials. Chem. Soc. Rev. 2012, 41, 2323–2343. [Google Scholar] [CrossRef] [PubMed]
- Stefano, D.D.; Carnuccio, R.; Maiuri, M.C. Nanomaterials toxicity and cell death modalities. J. Drug Deliv. 2012, 2012. [Google Scholar] [CrossRef] [PubMed]
- Webster, T.J.; Stout, D.A.; Kalmodia, S.; Basu, B. Experimental methods and in vitro cytoxicity and genotoxicity of nanomaterials. Nano LIFE 2013, 3. [Google Scholar] [CrossRef]
- Fischer, H.C.; Chan, W.C. Nanotoxicity: The growing need for in vivo study. Curr. Opin. Biotechnol. 2007, 18, 565–571. [Google Scholar] [CrossRef] [PubMed]
- Buzea, C.; Pacheco, I.I.; Robbie, K. Nanomaterials and nanoparticles: Sources and toxicity. Biointerphases 2007, 2, MR17–MR71. [Google Scholar] [CrossRef] [PubMed]
- Magrez, A.; Kasas, S.; Salicio, V.; Pasquier, N.; Seo, J.W.; Celio, M.; Catsicas, S.; Schwaller, B.; Forró, L. Cellular toxicity of carbon-based nanomaterials. Nano Lett. 2006, 6, 1121–1125. [Google Scholar] [CrossRef] [PubMed]
- Savi, M.; Rossi, S.; Bocchi, L.; Gennaccaro, L.; Cacciani, F.; Perotti, A.; Amidani, D.; Alinovi, R.; Goldoni, M.; Aliatis, I.; et al. Titanium dioxide nanoparticles promote arrhythmias via a direct interaction with rat cardiac tissue. Part. Fibre Toxicol. 2014, 11. [Google Scholar] [CrossRef] [PubMed]





| Nanomaterials for CVD | ||||||
|---|---|---|---|---|---|---|
| Material | Type | Category | Model | Nanofeature | Results | Reference |
| PEG | Synthetic | Scaffold | in vitro | Nanopillars | Enhanced cell binding cites increasing CM adhesion | [22] |
| PGA | Synthetic | Scaffold | in vitro | Nanofibrous | Higher cell viability due to increased hydrophilic properties | [27] |
| PPy/PCL/Gelatin | Synthetic/Natural | Scaffold | in vitro | Nanofibrous | Stronger attachment sites due to conductive PPy | [35] |
| SWNT/Gelatin | Carbon/Natural | Scaffold | SD Rats | Nanotubes | Decreased left ventricular end systole dimension | [44] |
| CNT/GelMA | Carbon/Natural | Scaffold | in vitro | Nanotubes | Biomimetic elastic modulus and decreased impendance increased cell retention | [46] |
| AU/PCL/Gelatin | AU/Synthetic/Natural | Scaffold | in vitro | Nanoparticles | Enhanced functional assembly and increased Cx43 expression | [60] |
| PCL/Gelatin | Synthetic/Natural | Electrospun | in vitro | Nanofibrous | Aligned nanofibers guided cell orientation suggesting CM preference for anisotropic properties | [51] |
| PCL | Synthetic | Electrospun | in vitro | Nanofibrous | Stretched scaffold using a wire ring to promote CM maturity to increased troponin-I expression | [52] |
| Peptides | Natural | Injectable | Porcine | Nanofibrous | Increased interventricular septum thickness and slowed ventricular remodling | [62] |
| Decellularized ECM | Natural | Injectable | Porcine | Nanofibrous | Promoted vascular cell infiltration at the infarct zone | [63] |
| PLGA-CNF | Carbon/Natural | Patch | in vitro | Nanofibrous | Increased mechanical strength, conductivity and enhanced cardiomyocyte growth | [57] |
| CNT/GelMA | Carbon/Natural | Patch | in vitro | Nanofibrous | Improved cell adhesion, organization and cell-cell coupling | [58] |
| AU/Alginate | Gold/Natural | Patch | in vitro | Nanofibrous | Improved electrical communication between cells resulting in enhanced cell adhesion and proliferation | [56] |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Amezcua, R.; Shirolkar, A.; Fraze, C.; Stout, D.A. Nanomaterials for Cardiac Myocyte Tissue Engineering. Nanomaterials 2016, 6, 133. https://doi.org/10.3390/nano6070133
Amezcua R, Shirolkar A, Fraze C, Stout DA. Nanomaterials for Cardiac Myocyte Tissue Engineering. Nanomaterials. 2016; 6(7):133. https://doi.org/10.3390/nano6070133
Chicago/Turabian StyleAmezcua, Rodolfo, Ajay Shirolkar, Carolyn Fraze, and David A. Stout. 2016. "Nanomaterials for Cardiac Myocyte Tissue Engineering" Nanomaterials 6, no. 7: 133. https://doi.org/10.3390/nano6070133
APA StyleAmezcua, R., Shirolkar, A., Fraze, C., & Stout, D. A. (2016). Nanomaterials for Cardiac Myocyte Tissue Engineering. Nanomaterials, 6(7), 133. https://doi.org/10.3390/nano6070133